Abstract
INTRODUCTION
The concept of using a mesh to repair hernias was introduced over 50 years ago. Mesh repair is now standard in most countries and widely accepted as superior to primary suture repair. As a result, there has been a rapid growth in the variety of meshes available and choosing the appropriate one can be difficult. This article outlines the general properties of meshes and factors to be considered when selecting one.
MATERIALS AND METHODS
We performed a search of the medical literature from 1950 to 1 May 2009, as indexed by Medline, using the PubMed search engine (<http://www.pubmed.gov>). To capture all potentially relevant articles with the highest degree of sensitivity, the search terms were intentionally broad. We used the following terms: ‘mesh, pore size, strength, recurrence, complications, lightweight, properties’. We also hand-searched the bibliographies of relevant articles and product literature to identify additional pertinent reports.
RESULTS AND CONCLUSIONS
The most important properties of meshes were found to be the type of filament, tensile strength and porosity. These determine the weight of the mesh and its biocompatibility. The tensile strength required is much less than originally presumed and light-weight meshes are thought to be superior due to their increased flexibility and reduction in discomfort. Large pores are also associated with a reduced risk of infection and shrinkage. For meshes placed in the peritoneal cavity, consideration should also be given to the risk of adhesion formation. A variety of composite meshes have been promoted to address this, but none appears superior to the others. Finally, biomaterials such as acellular dermis have a place for use in infected fields but have yet to prove their worth in routine hernia repair.
Keywords: Hernia, Mesh, Filament, Tensile strength, Porosity, Acellular dermi
History
Until 1958, abdominal wall hernias were closed with primary suture repair. In 1958, Usher published his technique using a polypropylene mesh. This led to the Lichtenstein repair some 30 years later which popularised mesh for hernia repair. Currently, about one million meshes are used per year world-wide.1 The benefits of meshes were accepted for many years but the need for evidence-based medicine led to several trials designed to quantify their advantages. In 2002, the EU trialist collaboration analysed 58 randomised controlled trials and found that the use of mesh was superior to other techniques. In particular, they noted fewer recurrences and less postoperative pain with mesh repair.2 Although these results are not accepted by all surgeons,3 meshes have now virtually replaced suture repair in the developed world.
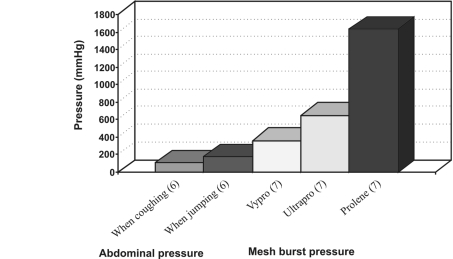
The original logic behind using a mesh was very simple: the mesh was a material which could be used to reinforce the abdominal wall with the formation of scar tissue. It was expected that the best meshes would be those made of very strong material and able to induce the most fibrosis. Unfortunately, this fibrotic reaction led to pain and movement restriction and it soon became clear that this needed to be minimised. In order to do this, the surface area, and therefore strength, of the mesh had to be reduced. Calculations of intra-abdominal pressures proved that this would be possible without compromising mesh function. In fact, the tensile strength of a mesh required to withstand the maximum abdominal pressure is only a tenth of that of most meshes (see Fig. 2). This realisation led to the concept of light-weight meshes.
Figure 2.
Comparison of mesh strength with abdominal wall pressures.
Light-weight meshes were first introduced in 1998 (Vypro) and their superiority over the heavy-weight meshes is now widely accepted. These meshes have large pores (normally 3–5 mm) and a small surface area. They stimulate a reduced inflammatory reaction and, therefore, have greater elasticity and flexibility.4 They also shrink less and have been shown to decrease pain after Lichtenstein inguinal hernia repair. Unfortunately, despite these improvements, they continue to have complications such as recurrence, infection and adhesion formation. Thus, the search for an ideal mesh continues.
The difficulty of finding a single, ‘ideal’ mesh was acknowledged by the development of composite meshes. These combine more than one material and are the basis of most new mesh designs. The main advantage of the composite meshes is that they can be used in the intraperitoneal space with minimal adhesion formation. Despite the vast selection of brands available, nearly all these meshes continue to use one or other of three basic materials – Polypropylene, Polyester and ePTFE. These are used in combination with each other or with a range of additional materials such as titanium, omega 3, monocryl, PVDF and hyaluronate. Contrary to the manufacturers' literature, it appears that none of these synthetic materials is without disadvantages.5
The problems encountered with synthetic materials led to the development of biomaterials and it is appropriate that the history of meshes should conclude with the most physiologically based implants. These consist of an acellular collagen matrix derived from human dermis (Aderm) or porcine small intestine submucosa (Surgisis). The matrix allows soft tissue to infiltrate the mesh which eventually becomes integrated into the body by a process of remodelling. Unfortunately, this process also appears to lead to a rapid reduction in their mechanical strength, and concerns regarding this have restricted their use to infected environments (where one would normally use an absorbable synthetic material such as Vicryl).
It is clear that the evolution of meshes is not yet complete and the ideal mesh has yet to be found. As no such mesh exists, this article outlines the properties to be considered when choosing a suitable implant from the many available.
Materials and Methods
We performed a search of the medical literature from 1950 to 1 May 2009, as indexed by Medline, using the PubMed search engine (<http://www.pubmed.gov>). To capture all potentially relevant articles with the highest degree of sensitivity, the search terms were intentionally broad. We used: ‘mesh, pore size, strength, recurrence, complications, lightweight, properties’. We also hand-searched the bibliographies of relevant articles and product literature to identify additional pertinent reports.
Mesh properties
TENSILE STRENGTH
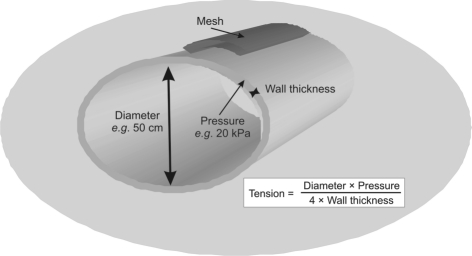
The tension placed on the abdominal wall can be calculated by the law of Laplace which states that (Fig. 1): ‘in an elastic spherical vessel (abdomen), the tension, pressure, wall thickness and diameter are related by: Tension = (Diameter × Pressure)/(4 × Wall thickness)’.
Figure 1.
The tension placed on the abdominal wall as calculated by the law of Laplace.
The maximum intra-abdominal pressures generated in healthy adults occur whilst coughing and jumping (Fig. 2). These are estimated to be about 170 mmHg.6 Meshes used to repair large hernias, therefore need to withstand at least 180 mmHg before bursting (tensile strength up to 32 N/cm). This is easily achieved as even the lightest meshes will withstand twice this pressure without bursting (for example, burst pressure of Vypro = 360 mmHg7). This illustrates that the tensile strengths of 100 N/cm of the original meshes were vastly overestimated.
PORE SIZE
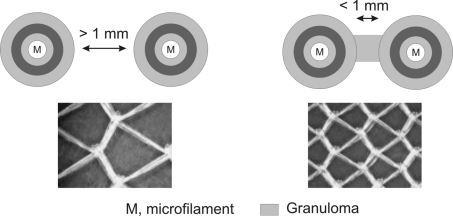
Porosity is the main determinant of tissue reaction. Pores must be more than 75 μm in order to allow infiltration by macrophages, fibroblasts, blood vessels and collagen. Meshes with larger pores allow increased soft tissue in-growth and are more flexible because of the avoidance of granuloma bridging. Granulomas normally form around individual mesh fibres as part of the foreign body reaction. Bridging describes the process whereby individual granulomas become confluent with each other and encapsulate the entire mesh (Fig. 3). This leads to a stiff scar plate and reduced flexibility. It occurs in meshes with small pores of less than 800 μm.
Figure 3.
Granulomas forming around individual mesh fibres and bridging where individual granulomas become confluent with each other and encapsulate the entire mesh.
WEIGHT
The weight of the mesh depends on both the weight of the polymer and the amount of material used (pore size).9
Heavy-weight meshes use thick polymers, have small pore sizes and high tensile strength. These meshes typically weigh 100 g/m2 (1.5 g for 10 × 15 cm mesh). The strength is derived from a large mass of material, which activates a profound tissue reaction and dense scarring.
Light-weight meshes are composed of thinner filaments and have larger pores (> 1 mm). Their weight is typically 33 g/m2 (0.5 g for 10 × 15 cm mesh). They initiate a less pronounced foreign body reaction and are more elastic. Despite a reduced tensile strength, they can still withstand pressures above the maximum abdominal pressure of 170 mmHg (minimum tensile strength 16 N/cm).
A new generation of even lighter meshes include the titanium/propylene composite meshes. These have been shown to be associated with a more rapid recovery in a recent, randomised controlled trial (RCT).8 The lightest of these (Extralight TiMesh) may have insufficient tensile strength in some situations (maximum tensile strength 12 N/cm).
REACTIVITY/BIOCOMPATIBILITY
Modern biomaterials are physically and chemically inert. They are generally stable, non-immunogenic and non-toxic. Despite this, they are not biologically inert.7 A foreign body reaction is triggered by their presence. This involves inflammation, fibrosis, calcification, thrombosis and formation of granulomas. It is very different from the physiological wound healing of suture repair.9
The foreign body reaction is fairly uniform regardless of the type of foreign material, but the extent of the reaction is affected by the amount of material present. Thus pore size is once again the determining factor for meshes. As described above, meshes with small pores develop stiff scar plates which are avoided in meshes with larger pores where there is a gap between the granulomas.
Meshes also appear to alter collagen composition. During normal scar healing, the initial, immature, type III collagen is rapidly replaced by stronger, type I collagen. This process is delayed in the presence of a foreign body such as a mesh. The result is a much lower ratio of type I/III collagen, leading to reduced mechanical stability.7,9,10 This effect occurs regardless of the type of mesh used, although the amount of collagen laid down is higher in microporous meshes.
ELASTICITY
The natural elasticity of abdominal wall at 32 N/cm is about 38%. Light-weight meshes have an elasticity of about 20–35% elasticity at 16 N/cm.7 Heavy-weight meshes have only half this elasticity (4–16% at 16 N/cm) and can restrict abdominal distension.
CONSTITUTION
Mesh fibres can be monofilament, multifilament (braided), or patches (for example, ePTFE). Multifilament fibres have a higher risk of infection.
SHRINKAGE
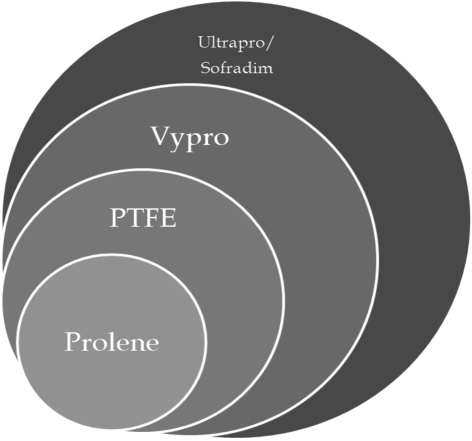
Shrinkage occurs due to contraction of the scar tissue formed around the mesh. Scar tissue shrinks to about 60% of the former surface area of the wound.7 The smaller pores of heavy-weight meshes lead to more shrinkage due to the formation of a scar plate (Fig. 4).
Figure 4.
Shrinkage properties of different meshes. Prolene shrinks 75–94%, PTFE shrinks 40–50%, Vypro II shrinks 29%, Ultrapro shrinks < 5%, and Sofradim shrinks < 5%.
Complications of meshes
Most complications are merely a reflection of the properties already described. Thus, when choosing a mesh, the surgeon must decide which properties are the most important for the specific situation. For example, materials such as ePTFE have a good profile for adhesion risk but a high risk of infection. Incontrast, Polypropylene meshes are durable and have a low infection risk but they have little flexibility and a high adhesion risk. The main factors to consider in relation to complications are outlined below.
INFECTION RISK
Mesh infection is feared because it is difficult to eradicate without removing the mesh and can become clinically apparent many years after implantation.11 Mesh infection remains about 0.1–3%,12,13 although this is obviously higher in the infected fields, for example, in parastomal hernia repair.
Although widely practiced, there is no evidence that routine prophylaxis with antibiotics confers any protection against infection. In contrast there is some evidence that the infection risk can be lowered by impregnating meshes with antiseptics.14
The risk of infection is mainly determined by the type of filament used and pore size. Microporous meshes (for example, ePTFE) are at higher risk of infection because macrophages and neutrophils are unable to enter small pores (< 10 μm). This allows bacteria (< 1 μm) to survive unchallenged within the pores. A similar problem applies to multifilament meshes. The meshes at lowest risk of infection are, therefore, those made with monofilament and containing pores greater than 75 μm. Eradication of infection in such meshes can be achieved without their removal.15
ADHESION RISK
The popularisation of laparoscopic intraperitoneal mesh placement has led to increasing concern regarding mesh-related adhesions. Adhesions result from the fibrin exudates that follow any kind of trauma. These exudates form temporary adhesions until the fibrinolytic system absorbs the fibrin. Absorption is delayed in the presence ischaemia, inflammation or foreign bodies (for example, meshes). In these situations, they mature into tissue adhesions.
All meshes produce adhesions when placed adjacent to bowel, but their extent is determined by pore size, filament structure and surface area. Heavy-weight meshes induce an intense fibrotic reaction which ensures strong adherence to the abdominal wall but also causes dense adhesions. In contrast, microporous ePTFE does not allow tissue in-growth. It has a very low risk of adhesion formation, but is unable to adhere strongly to the abdominal wall.
These two extremes illustrate the difficulty of producing a mesh which will adhere well to the abdominal wall but not to the bowel. Composite meshes aim to do this by providing an additional surface which can be safely placed in contact with bowel whilst peritoneal mesothelial cells grow over the mesh. It takes up to 7 days to regenerate peritoneum; however, once formed, it should prevent adhesion formation to the mesh. Until recently, the standard composite mesh was a PP/ePTFE mix, but there are now a large variety of substances available, including PVDF, cellulose and omega-3 fatty acids. Unfortunately, there is evidence to suggest that most of these only prevent adhesion formation in the short term and the effect is diminished after 30 days.16 In some types, it is also possible for the layers to separate and become adherent to bowel.17
RECURRENCE
The use of meshes is thought to reduce dramatically the incidence of hernia recurrence. Quoted rates vary greatly between studies, but most describe a reduction in the rate of recurrence by at least half when using a mesh (for example, for incisional hernias this is reduced from 17–67% to 1–32%).18–23 In nearly all cases, recurrent herniation occurs at the edges of meshes. This is commonly due to inadequate fixation, or underestimation of shrinkage of the mesh, at the original operation. There is little evidence that recurrence is related to the type of mesh used,5 although it has been proposed that light-weight meshes have a higher risk due to their increased flexibility and movement.7 Other known risk factors include postoperative infection, seroma and haematoma.
Two-thirds of recurrences occur after 3 years (median, 26 months).24 This suggests that a technical error is unlikely to be the only cause of recurrence and defective collagen synthesis may be equally important. All meshes cause a foreign body reaction which has an effect on the ratio of Type I and III collagen synthesised.7,9 Changes in this ratio affect both tensile strength and mechanical stability and may increase the risk of recurrence. Altered ratios of collagen can be seen within fibroblasts located at the edges of recurrent hernias.7,9,22 It is not clear if the type of mesh used has any effect on this.
PAIN
Meshes are associated with a reduced risk of chronic pain compared to suture repair. This is thought to be related to the ability to use tension-free technique rather than the mesh itself.19 However, pain remains a serious complication of mesh repair and can occur for a variety of reasons. With regards to acute postoperative pain, there is little difference in the type of mesh used. Chronic pain following hernia repair has gained increased recognition, with a quoted risk of over 50%.25,26 When it starts in the immediate postoperative period, it is usually due to nerve damage at the time of operation. In contrast, pain due to foreign body reaction (FBR) typically presents after 1 year. Explants removed for chronic pain are found to have nerve fibres and fascicles around the foreign body granulomata within the mesh. Neuromas can also be found at the interface of mesh and host tissue suggesting mechanical destruction of nerves by mesh. It follows that meshes with small pores and greater FBR, will cause higher rates of chronic pain. This is supported by most studies,27,28 although disputed by some.29,30 Some authors have also suggested that absorbable meshes may have a role in reducing chronic pain.26
MESH DEGRADATION
Degradation of meshes is rare and mainly seen in polyester meshes.31 Degradation may be due to hydrolysis, resulting in brittleness and loss of mechanical strength. Calcification can also occur but has only been documented in meshes with small pores.32
SEROMA
Seromas develop with any mesh type but those with larger pores may be less likely to do so.33
Which mesh should surgeons use?
When choosing a mesh (Tables 1–3), the surgeon must consider the context in which it is to be used. In most situations, one should look for a light-weight mesh, with large pores and minimal surface area. Ideally, it should consist of a monofilament. A polypropylene or polyester mesh is, therefore, usually suitable (for example, Paritiene Light, Optilene, Mersilene). These meshes will be more comfortable and have a lower risk of infection. If the mesh is to be placed inside the peritoneal cavity, an attempt should be made to minimise adhesions by choosing a hybrid mesh with an absorbable surface. Despite manufacturers' claims, the differences between the various types of these are unproven and it is currently difficult to recommend a single material. In infected wounds, an absorbable mesh is preferred, for example, polyglactin (Vicryl) or polyglycolic (Dexon). Biomaterials may also be useful in this situation if the additional cost can be justified. Finally, the surgeon should not forget that the way the mesh is placed is as important as the type of mesh used. If a mesh is too small or fixed under tension, there will be complications whatever its material. Despite the new implants available, surgical skill still has a role in preventing hernia recurrence!
Table 1.
Types of mesh: Multi, mulifilament and monofilament, foil
| Type of mesh | Pore size | Absorbable | Weight | Comments | |
|---|---|---|---|---|---|
| Multi | |||||
| Vicryl (Ethicon) | Polyglactin | Small 0.4 mm | Yes, fully (60–90 days) | Medium weight 56 g/m2 | Absorbable meshes primarily used in infected fields |
| Dexon (Syneture) | Polyglycolic | Medium 0.75mm | Yes, fully (60–90 days) | ||
| Safil (B-Baun) | |||||
| Multifilament and monofilament | |||||
| Marlex (BARD) | Polypropylene | Small to medium 0.8 mm | No | Heavy-weight average 80–100 g/m2 | Traditional heavy meshes with small pores and little stretch. Not used in extraperitoneal spaces as they produce dense adhesions. Low infection risk |
| 3D Max (BARD) | |||||
| Polysoft (BARD) | |||||
| Prolene (Ethicon) | |||||
| Surgipro (Autosuture) | |||||
| Prolite (Atrium) | |||||
| Trelex (Meadox) | |||||
| Atrium (Atrium) | |||||
| Premilene (B-Braun) | |||||
| Serapren (smooth) | |||||
| Parietene (Covidien) | |||||
| Parietene Light (Covidien) | Large 1.0–3.6 mm | Light/medium weight 36–48g/m2 | Traditional meshes but lighter, with larger pores | ||
| Optilene (B-Baun) | |||||
| Multi | |||||
| Mersilene (Ethicon) | Polyester | Large 1–2 mm | No | Medium weight ∼40 g/m2 | Low infection risk and ?less inflammatory response than PP. Long-term degradation may be a problem30 |
| Foil | |||||
| Goretex (Gore) | ePTFE | Very small 3 μm | No | Heavyweight | Smooth and strong. Not a true mesh but multilaminar patch. Microporous. High infection risk |
Table 3.
Composite meshes (for intraperitoneal use)
| Type of mesh | Pore size | Absorbable | Weight | Comments | |
|---|---|---|---|---|---|
| Multi | |||||
| Vypro, Vypro II (Ethicon) | Prolypropylene/PG910 | Large > 3 mmm | Partially (42 days) | Light-weight 25 & 30 g/m2 | First light-weight meshes with large pores. Vypro not strong enough for incisional hernias (use Vypro II) |
| Gortex Dual Mesh & Dual Mesh Plus (Gore) | ePTFE | Very small 3/22 μm | No | Heavy-weight | Different sized pores for each side. Dual Mesh Plus is impregnated with antiseptic to minimise infection |
| Parietex (Covidien) | Polyester/collagen | Large > 3 mm | Partially (20 days) | Medium weight 75 g/m2 | Bovine collagen coating and anti-adhesion film of polyethylene glycol and glycerol. ?Only short-term benefit for anti-adhesional property16 |
| Mono | |||||
| Composix EX Dulex (BARD) | Polypropylene/ePTFE | Medium 0.8 mm | No | Light-weight | Two distinct surfaces, overlap of ePTFE stops adhesions at the edges |
| Proceed (Ethicon) | Polypropylene/cellulose (ORC) | Large | Partially (< 30 days) | Light-weight 45 g/m2 | 3-layer laminate with PP; oxidised cellulose (absorbable) and polydioxanone film (not absorbed) |
| Dynamesh IPOM (FEG Textiltechnik) | Prolypropylene/PVDF | Large 1–2 mm | Partially | Medium weight 60 g/m2 | PVDF causes minimal foreign body reaction |
| Sepramesh (Genzyme) | Prolypropylene/sodium | Large 1–2 mm | Partially (< 30 days) | Heavy-weight 102 g/m2 | Seprafilm turns to gel in 48 h and remains on mesh for 1 week to allow re-epithelisation. ?Only short-term benefit for anti-adhesional property hyaluronate16 |
| Ultrapro (Ethicon) | Polypropylene/polyglecaprone (Monocryl) | Large > 3 mm | Partially (< 140 days) | Light-weight 28 g/m2 | Monocryl has a combination of polymers; e-caprolactone, which is malleable and polyglycolide, which is strong. Less inflammatory response than Vicryl |
| Ti-mesh (GfE) | Polypropylene/titanium | Large > 1 mm | No | Light-weight and extra-light 16 & 35 g/m2 | Possibly has a reduced inflammatory response compared to other meshes (?biologically inert)34 |
| C-Qur (Atrium) | Polypropylene/omega 3 | Large > 1 mm | Partially (∼120 days) | Medium-weight 50 g/m2 | Omega 3 from fish oils ?Only short-term benefit for anti-adhesional property16 |
Table 2.
Types of mesh: Biomateria
| Type of mesh | Comments | |
|---|---|---|
| Surgisis (Cook) | Porcine (small intestine submucosa) | Readily colonised by host and forms scaffold for repair and remodelling of ECM. Strong at first but loss of strength with remodelling. Can be used in contaminated wounds |
| Fortagen (Organogenesis) | ||
| Alloderm (Lifecell) | Human acellular dermis | |
| Flex HD (J&J) | ||
| AlloMax (Davol) | ||
| Collamend (Davol) | Xenogenic acellular dermis (porcine/bovine) | |
| Strattice (LifeCell) | ||
| Permacol (TSL) | ||
| XenMatriX (Brennen) | ||
| SurgiMend (TEI) | ||
References
- 1.Klinge U, Klosterhalfen B, Birkenhauer V, Junge K, Conze J, Schumpelick V. Impact of polymer pore size on the interface scar formation in a rat model. J Surg Res. 2002;103:208–14. doi: 10.1006/jsre.2002.6358. [DOI] [PubMed] [Google Scholar]
- 2.The EU Hernia Trialists Collaboration. Repair of groin hernia with synthetic mesh: meta-analysis of RCT. Ann Surg. 2002;235:322–32. doi: 10.1097/00000658-200203000-00003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Nixon SJ, Jawaid H. Recurrence after inguinal hernia repair at ten years by open darn, open mesh and TEP – no advantage with mesh. Surgeon. 2009;7:71–4. doi: 10.1016/s1479-666x(09)80018-8. [DOI] [PubMed] [Google Scholar]
- 4.Klinge U. Mesh for hernia repair. Br J Surg. 2008;95:539–40. doi: 10.1002/bjs.6159. [DOI] [PubMed] [Google Scholar]
- 5.O'Dwyer, Kingsworth AN, Molloy RG, Small PK, Lammers B, Horeyseck G. Randomized clinical trial assessing impact of a lightweight or heavyweight mesh on chronic pain after inguinal hernia repair. Br J Surg. 2005;92:166–70. doi: 10.1002/bjs.4833. [DOI] [PubMed] [Google Scholar]
- 6.Cobb WS, Burns JM, Kercher KW, Matthews BD, James Norton H, Todd Heniford B. Normal intraabdominal pressure in healthy adults. J Surg Res. 2005;129:231–5. doi: 10.1016/j.jss.2005.06.015. [DOI] [PubMed] [Google Scholar]
- 7.Klosterhalfen B, Junge K, Klinge U. The lightweight and large porous mesh concept for hernia repair. Expert Rev Med Devices. 2005;2:103–17. doi: 10.1586/17434440.2.1.103. [DOI] [PubMed] [Google Scholar]
- 8.Koch A, Bringman S, Myrelid P, Kald A. Randomised clinical trial of groin hernia repair with titanium-coated lightweight mesh compared with standard polypropylene mesh. Br J Surg. 2008;95:1226–31. doi: 10.1002/bjs.6325. [DOI] [PubMed] [Google Scholar]
- 9.Klosterhalfen B, Hermanns B, Rosch R. Biological response to mesh. Eur Surg. 2003;35:16–20. [Google Scholar]
- 10.Junge K, Klinge U, Rosch R, Mertens PR, Kirch J, et al. Decreased collagen type I/III ration in patients with recurring hernia after implantation of alloplastic prosthesis. Langenbecks Arch Surg. 2004;389:17–22. doi: 10.1007/s00423-003-0429-8. [DOI] [PubMed] [Google Scholar]
- 11.Klinge U, Junge K, Spellerberg B, Piroth C, Klosterhalfen B, Schumpelick V. Do multifilament alloplastic meshes increase the infection rate? J Biomed Mater Res. 2002;63:765–71. doi: 10.1002/jbm.10449. [DOI] [PubMed] [Google Scholar]
- 12.Kumar S. Chronic groin sepsis following tension-free inguinal hernioplasty. Br J Surg. 1999;86:1482. [PubMed] [Google Scholar]
- 13.Avtan L, Avci C, Bulut T, Fourtanier G. Mesh infections after laparoscopic inguinal her nia repair. Surg Laparosc Endosc. 1997;7:192–5. [PubMed] [Google Scholar]
- 14.Carbonell AM, Mathews BD, Dreau D, Foster M, Austin CE, et al. The sus ceptibility of prosthetic materials to infection. Surg Endosc. 2005;19:430–5. doi: 10.1007/s00464-004-8810-4. [DOI] [PubMed] [Google Scholar]
- 15.Amid PK, Lichtenstein IL, Shulman AG. Biomaterials for tension-free hernioplasties and principles of their applications. Minerva Chir. 1995;50:821–6. [PubMed] [Google Scholar]
- 16.Schreinemacher MHF, Emans PJ, Gijbels MJ, Greve JW, Beets GL, Bouvy ND. Degradation of mesh coatings and intraperitoneal adhesion formation in an experimen tal model. Br J Surg. 2009;96:305–313. doi: 10.1002/bjs.6446. [DOI] [PubMed] [Google Scholar]
- 17.Bohmer RD, Byrne PD, Maddern GJ. A peeling mesh. Hernia. 2002;6:86–7. doi: 10.1007/s10029-002-0061-5. [DOI] [PubMed] [Google Scholar]
- 18.Schumpelick V, Klinge U. Prosthetic implants for hernia repair. Br J Surg. 2003;90:1457–8. doi: 10.1002/bjs.4385. [DOI] [PubMed] [Google Scholar]
- 19.Burger JWA, Luijendijk RW, Hop WCJ, Halm JA, Verdaasdonk EGG, Jeekel J. Long-term follow-up of RCT of suture versus mesh repair of incisional hernia. Ann Surg. 2004;240:578–85. doi: 10.1097/01.sla.0000141193.08524.e7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Finan KR, Kilgore ML, Hawn MT. Open suture versus mesh repair of primary incisional hernias a cost-utility analysis. Hernia. 2009;13:173–82. doi: 10.1007/s10029-008-0462-1. [DOI] [PubMed] [Google Scholar]
- 21.Mahmoud Uslu HY, Erkek AB, Cakmak A, Sozener U, Soylu L, et al. Incisional hernia treatment with polypropylene graft: results of 10 years. Hernia. 2006;10:380–4. doi: 10.1007/s10029-006-0107-1. [DOI] [PubMed] [Google Scholar]
- 22.Sauerland S, Schmedt CG, Lein S, Leibl BJ, Bittner R. Primary incisional hernia repair with or without polypropylene mesh: a report on 384 patients with 5-year follow-up. Langenbecks Arch Surg. 2005;390:408–12. doi: 10.1007/s00423-005-0567-2. [DOI] [PubMed] [Google Scholar]
- 23.Anthony T, Bergen PC, Kim LT, Henderson M, Fahey T, et al. Factors affecting recurrence following incisional herniorrhaphy. World J Surg. 2000;24:95–100. doi: 10.1007/s002689910018. [DOI] [PubMed] [Google Scholar]
- 24.Schumpelick V, Nylus L. Meshes: benefits and risks. Berlin: Springer; 2003. [Google Scholar]
- 25.Poobalan AS, Bruce J, Smith WC, King PM, Krukowski ZH, Chambers WA. A review of chronic pain after inguinal herniorrhaphy. Clin J Pain. 2003;19:48–54. doi: 10.1097/00002508-200301000-00006. [DOI] [PubMed] [Google Scholar]
- 26.Courtney CA, Duffy K, Serpell MG, O'Dwyer PJ. Outcome of patients with severe chron ic pain following repair of groin hernia. Br J Surg. 2002;89:1310–4. doi: 10.1046/j.1365-2168.2002.02206.x. [DOI] [PubMed] [Google Scholar]
- 27.Horstmann R, Hellwig M, Classen C, Röttgermann S, Palmes D. Impact of polypropy lene amount on functional outcome and quality of life after inguinal hernia repair by the TAPP procedure using pure, mixed, and titanium-coated meshes. World J Surg. 2006;30:1742–9. doi: 10.1007/s00268-005-0242-3. [DOI] [PubMed] [Google Scholar]
- 28.Agarwal BB, Agarwal KA, Mahajan KC. Prospective double-blind randomized controlled study comparing heavy- and lightweight polypropylene mesh in totally extraperitoneal repair of inguinal hernia: early results. Surg Endosc. 2009;23:242–7. doi: 10.1007/s00464-008-0188-2. [DOI] [PubMed] [Google Scholar]
- 29.Bringman S, Wollert S, Osterberg J. One year results of a randomised controlled multi-centre study comparing Prolene and Vypro II-mesh in Lichtenstein hernioplasty. Hernia. 2005;9:223–7. doi: 10.1007/s10029-005-0324-z. [DOI] [PubMed] [Google Scholar]
- 30.Langenbach MR, Schmidt J, Ubrig B. Sixty-month follow-up after endoscopic inguinal hernia repair with three types of mesh: a prospective randomized trial. Surg Endosc. 2008;22:1790–7. doi: 10.1007/s00464-008-9863-6. [DOI] [PubMed] [Google Scholar]
- 31.Klosterhalfen B, Klinge U, Schumpelick V. Polymers in hernia repair-common polyester vs. polypropylene surgical meshes. J Mat Sci. 2000;35:4769–76. [Google Scholar]
- 32.Zieren J, Neuss H, Paul M, Müller J. Introduction of polyethylene terephthalate mesh (KoSa hochfest) for abdominal hernia repair: an animal experimental study. Biom Mat Eng. 2004;2:127–32. [PubMed] [Google Scholar]
- 33.Schumpelick V, Klosterhalfen B, Müller M. Minimized polypropylene mesh for preperitoneal net plasty (PNP) of incisional hernias. Chirurg. 1999;70:422–30. doi: 10.1007/s001040050666. [DOI] [PubMed] [Google Scholar]
- 34.Scheidbach H, Tannapfel A, Schmidt U, Lippert H, Köckerling F. Influence of titanium coating on the biocompatibility of a heavyweight polypropylene mesh. Eur Surg Res. 2004;36:313–7. doi: 10.1159/000079917. [DOI] [PubMed] [Google Scholar]