Abstract
INTRODUCTION
The natural history of a lumbar hernia of the nucleus pulposus (HNP) is not fully known and clear indications for operative intervention cannot be established from the literature. Several studies have shown that the largest discs appear to have the greatest tendency to resolve. The aim of this study was to investigate whether massive prolapsed discs can be safely managed conservatively once clinical improvement has occurred.
PATIENTS AND METHODS
Thirty-seven patients were studied by clinical assessments and serial magnetic resonance imaging (MRI) over 2 years. Patients had severe sciatica at first, but began to show clinical improvement despite the large disc hernia-tions. Clinical assessment included the Lasegue test and neurological appraisal. The Oswestry Disability Index was used to measure function and changes in function. Serial MRI studies allowed measurement of volume changes of the herniated disc material over a period of time.
RESULTS
Initial follow-up at an average of 23.2 months revealed that 83% had a complete and sustained recovery at the initial follow-up. Only four patients required a discectomy. The average Oswestry disability index improved from 58% to 15%. Volumetric analysis of serial MRI scans found an average reduction of 64% in disc size. There was a poor correlation between clinical improvement and the extent of disc resolution.
CONCLUSIONS
A massive disc herniation can pursue a favourable clinical course. If early progress is shown, the long-term prognosis is very good and even massive disc herniations can be treated conservatively.
Keywords: Intervertebral disc displacement, Discectomy, Magnetic resonance imaging, Natural history
The decision to treat any condition depends upon an understanding of the natural history of the disease process. The natural history of a lumbar hernia of the nucleus pulposus (HNP) is not fully known and clear indications for operative intervention cannot be established from the literature. Back surgery rates, however, increase almost linearly with the per capita supply of orthopaedic and neurosurgeons in the country.1
Controversy still exists regarding indications for operating on large, extruded discs. A large extruded disc has been a relative indication for operative treatment in the past.2 However, several papers have demonstrated that these discs have the greatest tendency to decrease in size with conservative management.3–10
Weber11 published the first randomised, prospective trial of the long-term benefit of operative versus non-operative treatment of herniated lumbar discs. He found a statistically better result for operative intervention at 1 year. After 4 years, the operated patients still showed better results, but the difference was marginal and not statistically significant.
By 10 years, the outcomes were similar, but the operated group had fewer exacerbations of symptoms during the 10-year interval. The Weber study occurred before magnetic resonance imaging (MRI) and when computed tomography (CT) was in its infancy and has, therefore, many limitations. The Spine Patient Outcomes Research Trial (SPORT)12 recruited 501 surgical candidates and randomised them into discectomy versus conservative treatment. At 2-year follow-up, both groups had made substantial improvement. There was a tendency towards better outcomes in the operative group but this was not statistically significant. The study was hampered by a large cross-over of patients between the groups. An observational cohort of the SPORT study (743 patients who met the studies eligibility but refused randomisation) reported similar finding with both groups improving and those who had operative intervention reporting greater improvement in the first 2 years.13 However, there has been a paucity of prospective studies which have analysed the long-term outcome of either operative or conservatively treated lumbar disc herniations using modern imaging.
In our clinical experience, patients sometimes present with severe sciatica and incapacity due to intervertebral disc herniation, but by the time MRI scans have been obtained, they may show signs of distinct clinical improvement, despite the MRI evidence of particularly large disc herniations. The surgeon is then faced with the dilemma of intervening in the presence of clinical progress or adopting a conservative policy which, in theory, could prolong the period of suffering, leading to greater nerve damage or even result in cauda equina syndrome.
We defined ‘massive disc herniation’ on MRI scans as cases where extruded disc material occupied 50% or more of the anteroposterior diameter of the spinal canal. Sequestrated discs were included. We then posed the following questions and could not find satisfactory answers in the existing literature:
Is it safe to adopt a ‘wait-and-watch’ policy for cases of massive disc herniation, thus allowing time for the symptoms to resolve spontaneously?
Can cases of massive disc herniation show clinical improvement which is complete and sustained?
Is there a trend for massive disc herniations to cause recurrent clinical crises?
Is there an unacceptable risk of nerve damage or cauda equina syndrome resulting from the conservative approach?
What happens to the large volume of nucleus pulposus lying within the canal? Does it disappear by a process of resorption or does it remain in the canal?
In an attempt to answer these questions, we initiated a prospective study of the clinical outcome of a cohort of patients with sciatica who initially appeared to require dis-cectomy, but subsequently showed spontaneous improvement, despite MRI evidence of a massive disc prolapse. The study ran for 2 years during which time clinical progress was monitored. Second scans were performed after the initial scan in order to study volumetric changes of the herni-ated disc material with time, and its relationship with the clinical outcome. We aimed to ascertain the natural history of a conservatively treated massive lumbar disc herniation. Five years later, we contacted the patients to detect the late consequences of our conservative treatment policy.
Patients and Methods
Initial study – clinical and serial MRI
Between 1995 and 1998, patients referred to our orthopaedic clinic who demonstrated a clinical syndrome of severe sciatica for more than 6 weeks, an MRI-proven massive disc prolapse (disc material occupying > 50% of the spinal canal) and evidence of any improvement in their symptoms since onset were consecutively recruited into this study. Patients with spinal stenosis or a previous spinal operation were excluded.
All patients underwent a full clinical assessment and MRI on presentation. They were then offered a follow-up clinical examination and a repeat MRI between 6 months and 2 years after the original scans. Patients were assessed by independent orthopaedic surgeons who were blinded to the MRI results. Clinical assessment included the Lasegue test and neurological appraisal. The Oswestry Disability Index (the Oswestry Disability Score expressed as a percentage) was used as a subjective measure.
The MRI scans were done on an IGE 0.5 Tesla Vectra machine. The protocol used was T1-weighted sagittal and axial scans with a gradient echo of 100° and repetition and echo times (TR/TE) of 250/15. The parameters of the T2-weighted sagittal and axial images were FSE 4200TR 110TE. Volumes were measured using specific tissue volume measurement software in the sagittal plane. The scans were assessed by a consultant radiologist who was blinded to the clinical outcome. Statistical analysis was undertaken using Pearson's correlation coefficients and regression lines were drawn. Mean and standard deviations or range are given. Significance was set at P < 0.05.
Late assessment – telephone enquiry
Symptoms were assessed at 7 years by a structured telephone enquiry. All patients were questioned about any further back complaints, persistent weakness or numbness following their massive disc prolapse. Patients were asked to grade their original symptoms as: (i) resolved; (ii) continued providing occasional discomfort; (iii) continued providing frequent discomfort limiting activities; or (iv) resolved and returned. Patients also graded their satisfaction with the treatment they received as: (i) satisfied; (ii) uncertain; or (iii) not satisfied. The Fisher exact test was used to analyse outcomes at 7 years. Significance was set at P < 0.05.
Results
Thirty-seven patients who satisfied the inclusion and exclusion criteria were recruited to the study. Two refused repeat scans because of claustrophobia and were thus excluded from the analysis and initial follow-up leaving 35 remaining. Initial follow-up period was 23.2 months mean (range, 6–45 months). Average age was 40.4 years (range, 25–62 years). The distribution of involved levels by gender is shown in Table 1.
Table 1.
Distribution of prolapsed disc level by gender
| Male | Female | Total | |
|---|---|---|---|
| L4/5 | 5 | 7 | 12 |
| L5/S | 1 | 17 | 6 |
| All | 22 | 13 | 35 |
Early follow-up
OSWESTRY DISABILITY INDEX
The index showed a general improvement over time. The initial mean index was 58% (range, 32–94%). The mean of the final index was 15% (range, 0–68%). The mean percentage reduction in indices (i.e. Initial index – Final index/Initial index × 100) was 72%. There were no statistical differences between the sexes.
CLINICAL OUTCOME
Four patients underwent microdiscectomy for persistent or recurrent symptoms at an average of 33 months after symptom onset (range, 18–60 months). Two other patients had recurrent episodes of sciatica but no operations. Thus, 29 (83%) had a complete and sustained recovery at the initial follow-up.
Ten patients (29%) complained of occasional or intermittent back pain. Five patients (14%) had occasional or intermittent leg pain. Only one patient had a persistently positive straight leg raise test and was one of the patients who underwent a discectomy. Four patients (11%) had sensory loss, but none had permanent motor loss.
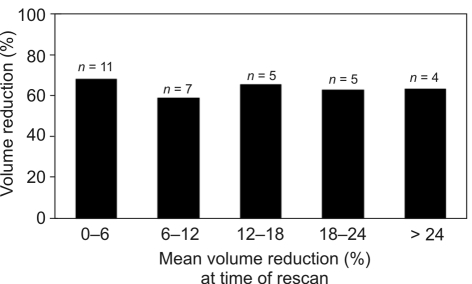
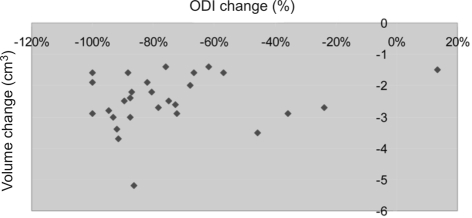
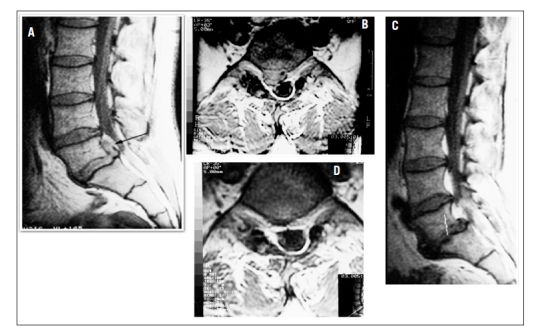
VOLUMETRIC ANALYSIS
Three patients were excluded from this analysis due to the quality of their scans; therefore, 32 patients’ scans were analysed. The average time between scans was 13.2 months (range, 3–42 months). All discs were non-contained and showed a reduction in size on their second scan (Figs 1 and 2).
Figure 1.
(A–D) Sagittal and axial MR images of a massive disc prolapse at L5/S1 that demonstrated a 74% reduction in size over 12 months.
Figure 2.
(A–D) Sagittal and axial MR images of a non-contained large disc prolapse at L5/S1.
The mean disc volume reduction (the percentage of shrinkage of the disc prolapse) was 64% (range, 31–78%). The mean volume reduction at the time of re-scan is shown in Figure 3. Fourteen patients (44%) had a percentage reduction of greater than 70%. A further 14 had a percentage reduction of 50–70%. Four patients had a reduction of less than 50%. The patients who underwent an operation had an average volume reduction of 47% (range, 31–62%). There were no significant differences in volume reduction between the involved levels and sexes (Table 2).
Figure 3.
The mean percentage volume reduction of disc prolapses with time.
Table 2.
Mean volume measurements by gender and disc level
| Volume of initial scan (cm3) | Volume of repeat scan (cm3) | Percentage change | |
|---|---|---|---|
| Males | 3.8 ± 0.9 | 1.4 ± 0.6 | −62.7 |
| Females | 3.6 ± 1.3 | 1.3 ± 0.4 | −65.2 |
| L4/5 | 4.1 ± 0.4 | 1.5 ± 0.7 | −63.5 |
| L5/S1 | 3.4 ± 0.9 | 1.2 ± 0.5 | −64.9 |
| All | 3.7 ± 1.1 | 1.4 ± 0.5 | −64.0 |
Values are mean ± SD.
VOLUME CHANGES AND CLINICAL OUTCOME
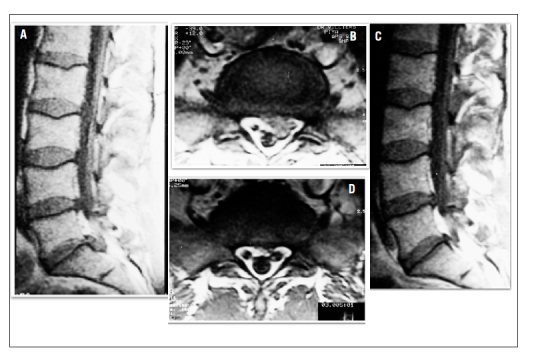
When the patients who underwent surgical intervention were excluded, there was a poor correlation between the volume changes and the percentage change in Oswestry Disability Score (r = 0.19; P = 0.35; Fig. 4).
Figure 4.
Percentage change of Oswestry Disability Index and volume change of the disc between initial and follow-up MRI in the non-operative patients.
There was no correlation between the initial disc volume and the Oswestry Disability Index, and between the initial or subsequent disc volume and the percentage change in the Oswestry Disability Index.
Long-term follow-up
All of the initial 37 patients were sought for the long-term follow-up. Unfortunately, three patients were untraceable (two of these had moved abroad). Therefore, 34 patients were followed up by telephone enquiry at mean 7 years 6 months (range, 76–109 months). The conservatively treated group recorded a 90% satisfaction rate compared with 50% in the operated group. This was not statistically significant. The patients’ clinical outcome at 7 years is shown in Table 3. There was statistical significance between the groups.
Table 3.
Results of 7-year clinical outcome and satisfaction rating
| Symptomatic outcome | Conservative treatment (n = 30) | Operative treatment (n = 4) | P-value |
|---|---|---|---|
| Resolved | 17 | 0 | 0.028 |
| Occasional symptoms | 10 | 2 | |
| Frequent symptoms | 1 | 1 | |
| Late recurrence | 2 | 1 | |
| Overall satisfaction | 27 (90%) | 2 (50%) | 0.09 |
P-values calculated using Fisher's exact test.
Discussion
Spontaneous regression of herniated nucleus pulposus was first documented by Guinto et al.14 in 1984. Treplick and Haskin15 then reported 11 patients in whom there was unequivocal regression or disappearance of a herniated lumbar disc on follow-up CT scan. Since then, many studies have demonstrated large reductions in the size of herniated discs with conservative treatment.6–10,16
Bush et al.17 studied 165 patients with sciatica thought to be due to lumbosacral nerve root compromise. They were treated with serial epidurals. Of the study cohort, 14% underwent surgical decompression and the rest made satisfactory clinical recovery. They were surprised to find on follow-up CT scanning that 64 of the 84 herniated/sequestered intervertebral discs showed partial or complete resolution at 1 year, whereas only 7 of the 27 bulging discs showed any resolution at 1 year. This was statistically significant.
Several studies using CT and MRI have demonstrated that the largest lumbar intervertebral disc herniations have the greatest ability to regress over time.
Maigne et al.18 examined 48 patients with acute sciatica treated by conservative measures. Using an initial CT scan, they classified the herniations by size – 13 small, 20 medium and 15 large. Comparison with follow-up CT showed that nine of the herniations had decreased by at least 25%, eight decreased between 50–75% and 31 decreased between 75–100%. The largest herniations were those which had the greatest tendency to decrease in size. Modic et al.8 studied 25 patients with acute lumbar radiculopathy using MRI. Eighteen patients had HNP. Further MRI assessment was used at 6 weeks and 6 months. Among the HNPs larger than 6 mm, substantial reduction in size was noted in 36% at 6 weeks and in more than 60% at 6 months after presentation. Cribb et al.10 studied 15 massive disc prolapses treated non-operatively and found, on repeat MRI after a mean of 24 months, a dramatic resolution of the herniation in 14 with a mean reduction of size of 80% (range, 68–100%). Similar findings have been demonstrated in the cervical spine.19,20
In our study, all the analysed discs demonstrated a reduction in volume. We found 87% had a reduction of 50% or more. Our results are in keeping with the findings from other studies. Saal et al.9 reported 82% and Maigne et al.18 found 81% reduction of 50% or more on CT within 2 years. Bozzao et al.4 showed 48% had a reduction of 70% or more on MRI while our study demonstrated 44% of cases with this degree of resolution.
The mechanism by which herniated discs are resorbed is not fully understood. It is generally thought that an immune response develops to the disc tissue and inflammation helps to remove the invading tissue.21 Evidence suggests macrophages22–24 and neovascularisation24,25 play central roles in the resorption of discs following prolapse. Macrophages which infiltrate the herniated disc express high levels of matrix metalloproteinases, and these have an important role in the natural resorption process.26,27 The new blood vessels have an important role as a passage into the degenerate matrix.25
Both radiological and histological studies support the fact that massive discs have the greatest potential to resolve naturally. Ahn et al.3 studied 36 patients with symptomatic disc herniations who were treated conservatively. They found that transligamentous extension of the herniated disc materials through the ruptured posterior longitudinal ligament was more important to the disc reduction in size than its initial size. Matsui et al.28 found more granulation tissue and macrophages in transligamentous herniations than in subligamentous herniations. They found no granulation tissue in the protrusion specimens. Neovascularisation is most pronounced at the outermost hernia tissue25 and when the posterior longitudinal ligament is ruptured.29 It is likely that these vessels originate from the epidural venous plexus. Massive discs appear to have a greater inflammatory response and, therefore, a better capacity for resorption.
We noted a poor correlation between the volume changes of the disc and the percentage change in Oswestry Disability Score. The correlation of disc resorption and symptom improvement is still controversial. Some authors have noted only symptom improvement accompanying disc regression,9,17 while others have found correlation between them.6,30 Many studies have shown patients with marked symptomatic improvements with little or no changes on MRI.9 The fact that some discs are unchanged at follow-up scan, yet the patient has undergone symptomatic improvement, indicates that compression is not the only explanation for the symptoms. Other explanations include the release of inflammatory chemicals from the diseased disc31 and the composition of the herniated disc itself.32
Several authors have highlighted the lack of knowledge regarding long-term outcomes of sciatica caused by lumbar disc herniation.33,34 The strength of our study lies in the long duration of follow-up. We believe this is the first long-term follow-up study looking at massive disc prolapses. We found that, at long-term follow up, the conservatively treated group had very good outcomes and no evidence of significant complications from this approach. The 5-year outcomes from the Maine et al.33 study found that the advantages of surgery were greatest early in follow-up and narrowed over the 5 years. This is similar to the findings of Weber11 but he found no difference between the groups at 4 years. Postacchini2 noted that the results of surgery appear to deteriorate in the long and very long term.
Our study has several potential weaknesses. The software used for analysing the size of the disc has not been validated. However, the technique was used consistently throughout the study by a single radiologist, who was blinded to the clinical status of the patients. Due to the uncertainty of the rate of resorption of the disc, we did not use fixed repeat scan intervals. We did not re-scan before 6 months, but chose a number of different time intervals in an effort to observe the natural history of a PID over a 2-year period. Although the patients had clinical assessments initially and at 2 years, the final 7-year follow-up was carried out by telephone consultation.
Patients with sciatica should be encouraged to be patient and submit to conservative treatment methods initially. In the presence of clinical progress, even very large disc herniations can be left to resolve naturally. Early access to surgeons and diagnostic imaging may result in unnecessary operative treatment.
Conclusions
We can answer the questions that were posed at the outset of our study:
It is safe to adopt a ‘wait-and-watch’ policy for cases of massive disc herniation if there is any early sign of clinical improvement.
Where clinical progress is evident, 83% of cases of massive disc herniation will have sustained improvement.
Only 17% of cases will have recurring crises of back pain and sciatica.
If there is evidence of clinical improvement, massive disc prolapses do not appear to carry a risk of major nerve damage or cauda equina syndrome.
Massive disc herniations usually reduce in volume and by 6 months most are only a third of their original size.
Acknowledgments
The authors would like to thank Judith Wood for her help in the study.
References
- 1.Cherkin DC, Deyo RA, Loeser JD, Bush T, Waddell G. An international comparison of back surgery rates. Spine. 1994;19:1201–6. doi: 10.1097/00007632-199405310-00001. [DOI] [PubMed] [Google Scholar]
- 2.Postacchini F. Results of surgery compared with conservative management for lumbar disc herniations. Spine. 1996;21:1383–7. doi: 10.1097/00007632-199606010-00023. [DOI] [PubMed] [Google Scholar]
- 3.Ahn SH, Ahn MW, Byun WM. Effect of the transligamentous extension of lumbar disc herniations on their regression and the clinical outcome of sciatica. Spine. 2000;25:475–80. doi: 10.1097/00007632-200002150-00014. [DOI] [PubMed] [Google Scholar]
- 4.Bozzao A, Gallucci M, Masciocchi C, Aprile I, Barile A, Passariello R. Lumbar disk herniation: MR imaging assessment of natural history in patients treated without surgery. Radiology. 1992;185:135–41. doi: 10.1148/radiology.185.1.1523297. [DOI] [PubMed] [Google Scholar]
- 5.Delauche-Cavallier MC, Budet C, Laredo JD, Debie B, Wybier M, et al. Lumbar disc herniation. Computed tomography scan changes after conservative treatment of nerve root compression. Spine. 1992;17:927–33. [PubMed] [Google Scholar]
- 6.Komori H, Shinomiya K, Nakai O, Yamaura I, Takeda S, Furuya K. The natural history of herniated nucleus pulposus with radiculopathy. Spine. 1996;21:225–9. doi: 10.1097/00007632-199601150-00013. [DOI] [PubMed] [Google Scholar]
- 7.Matsubara Y, Kato F, Mimatsu K, Kajino G, Nakamura S, Nitta H. Serial changes on MRI in lumbar disc herniations treated conservatively. Neuroradiology. 1995;37:378–83. doi: 10.1007/BF00588017. [DOI] [PubMed] [Google Scholar]
- 8.Modic MT, Ross JS, Obuchowski NA, Browning KH, Cianflocco AJ, Mazanec DJ. Contrast-enhanced MR imaging in acute lumbar radiculopathy: a pilot study of the natural history. Radiology. 1995;195:429–35. doi: 10.1148/radiology.195.2.7724762. [DOI] [PubMed] [Google Scholar]
- 9.Saal JA, Saal JS, Herzog RJ. The natural history of lumbar intervertebral disc extrusions treated nonoperatively. Spine. 1990;15:683–6. doi: 10.1097/00007632-199007000-00013. [DOI] [PubMed] [Google Scholar]
- 10.Cribb GL, Jaffray DC, Cassar-Pullicino VN. Observations on the natural history of massive lumbar disc herniation. J Bone Joint Surg Br. 2007;89:782–4. doi: 10.1302/0301-620X.89B6.18712. [DOI] [PubMed] [Google Scholar]
- 11.Weber H. Lumbar disc herniation. A controlled, prospective study with ten years of observation. Spine. 1983;8:131–40. [PubMed] [Google Scholar]
- 12.Weinstein JN, Tosteson TD, Lurie JD, Tosteson AN, Hanscom B, et al. Surgical vs nonoperative treatment for lumbar disk herniation: the Spine Patient Outcomes Research Trial (SPORT): a randomized trial. JAMA. 2006;296:2441–50. doi: 10.1001/jama.296.20.2441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Weinstein JN, Lurie JD, Tosteson TD, Skinner JS, Hanscom B, et al. Surgical vs nonoperative treatment for lumbar disk herniation: the Spine Patient Outcomes Research Trial (SPORT) observational cohort. JAMA. 2006;296:2451–9. doi: 10.1001/jama.296.20.2451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Guinto FC, Jr, Hashim H, Stumer M. CT demonstration of disk regression after conservative therapy. AJNR Am J Neuroradiol. 1984;5:632–3. [PMC free article] [PubMed] [Google Scholar]
- 15.Teplick JG, Haskin ME. Spontaneous regression of herniated nucleus pulposus. AJR Am J Roentgenol. 1985;145:371–5. doi: 10.2214/ajr.145.2.371. [DOI] [PubMed] [Google Scholar]
- 16.Masui T, Yukawa Y, Nakamura S, Kajino G, Matsubara Y, et al. Natural history of patients with lumbar disc herniation observed by magnetic resonance imaging for minimum 7 years. J Spinal Disord Tech. 2005;18:121–6. doi: 10.1097/01.bsd.0000154452.13579.b2. [DOI] [PubMed] [Google Scholar]
- 17.Bush K, Cowan N, Katz DE, Gishen P. The natural history of sciatica associated with disc pathology. A prospective study with clinical and independent radiologic follow-up. Spine. 1992;17:1205–12. doi: 10.1097/00007632-199210000-00013. [DOI] [PubMed] [Google Scholar]
- 18.Maigne JY, Rime B, Deligne B. Computed tomographic follow-up study of fortyeight cases of nonoperatively treated lumbar intervertebral disc herniation. Spine. 1992;17:1071–4. doi: 10.1097/00007632-199209000-00010. [DOI] [PubMed] [Google Scholar]
- 19.Maigne JY, Deligne L. Computed tomographic follow-up study of 21 cases of nonoperatively treated cervical intervertebral soft disc herniation. Spine. 1994;19:189–91. doi: 10.1097/00007632-199401001-00013. [DOI] [PubMed] [Google Scholar]
- 20.Mochida K, Komori H, Okawa A, Muneta T, Haro H, Shinomiya K. Regression of cervical disc herniation observed on magnetic resonance images. Spine. 1998;23:990–5. doi: 10.1097/00007632-199805010-00005. discussion 6–7. [DOI] [PubMed] [Google Scholar]
- 21.Satoh K, Konno S, Nishiyama K, Olmarker K, Kikuchi S. Presence and distribution of antigen-antibody complexes in the herniated nucleus pulposus. Spine. 1999;24:1980–4. doi: 10.1097/00007632-199910010-00003. [DOI] [PubMed] [Google Scholar]
- 22.Gronblad M, Virri J, Seitsalo S, Habtemariam A, Karaharju E. Inflammatory cells, motor weakness, and straight leg raising in transligamentous disc herniations. Spine. 2000;25:2803–7. doi: 10.1097/00007632-200011010-00013. [DOI] [PubMed] [Google Scholar]
- 23.Gronblad M, Virri J, Tolonen J, Seitsalo S, Kaapa E, et al. A controlled immunohistochemical study of inflammatory cells in disc herniation tissue. Spine. 1994;19:2744–51. doi: 10.1097/00007632-199412150-00002. [DOI] [PubMed] [Google Scholar]
- 24.Ito T, Yamada M, Ikuta F, Fukuda T, Hoshi SI, et al. Histologic evidence of absorption of sequestration-type herniated disc. Spine. 1996;21:230–4. doi: 10.1097/00007632-199601150-00014. [DOI] [PubMed] [Google Scholar]
- 25.Koike Y, Uzuki M, Kokubun S, Sawai T. Angiogenesis and inflammatory cell infiltration in lumbar disc herniation. Spine. 2003;28:1928–33. doi: 10.1097/01.BRS.0000083324.65405.AE. [DOI] [PubMed] [Google Scholar]
- 26.Haro H, Komori H, Kato T, Hara Y, Tagawa M, et al. Experimental studies on the effects of recombinant human matrix metalloproteinases on herniated disc tissues – how to facilitate the natural resorption process of herniated discs. J Orthop Res. 2005;23:412–9. doi: 10.1016/j.orthres.2004.08.020. [DOI] [PubMed] [Google Scholar]
- 27.Haro H, Crawford HC, Fingleton B, MacDougall JR, Shinomiya K, et al. Matrix metalloproteinase-3-dependent generation of a macrophage chemoattractant in a model of herniated disc resorption. J Clin Invest. 2000;105:133–41. doi: 10.1172/JCI7090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Matsui Y, Maeda M, Nakagami W, Iwata H. The involvement of matrix metalloproteinases and inflammation in lumbar disc herniation. Spine. 1998;23:863–8. doi: 10.1097/00007632-199804150-00005. discussion 8–9. [DOI] [PubMed] [Google Scholar]
- 29.Ozaki S, Muro T, Ito S, Mizushima M. Neovascularization of the outermost area of herniated lumbar intervertebral discs. J Orthop Sci. 1999;4:286–92. doi: 10.1007/s007760050105. [DOI] [PubMed] [Google Scholar]
- 30.Takada E, Takahashi M, Shimada K. Natural history of lumbar disc hernia with radicular leg paspontaneous MRI changes of the herniated mass and correlation with clinical outcome. J Orthop Surg (Hong Kong) 2001;9:1–7. doi: 10.1177/230949900100900102. [DOI] [PubMed] [Google Scholar]
- 31.Siddall PJ, Cousins MJ. Spinal pain mechanisms. Spine. 1997;22:98–104. doi: 10.1097/00007632-199701010-00016. [DOI] [PubMed] [Google Scholar]
- 32.Willburger RE, Ehiosun UK, Kuhnen C, Kramer J, Schmid G. Clinical symptoms in lumbar disc herniations and their correlation to the histological composition of the extruded disc material. Spine. 2004;29:1655–61. doi: 10.1097/01.brs.0000133645.94159.64. [DOI] [PubMed] [Google Scholar]
- 33.Atlas SJ, Keller RB, Chang Y, Deyo RA, Singer DE. Surgical and nonsurgical management of sciatica secondary to a lumbar disc herniation: five-year outcomes from the Maine Lumbar Spine Study. Spine. 2001;26:1179–87. doi: 10.1097/00007632-200105150-00017. [DOI] [PubMed] [Google Scholar]
- 34.Miller S, Casden AM. Spontaneous regression of a herniated disk. A case report with a four year follow-up. Bull Hosp Jt Dis. 1998;57:99–101. [PubMed] [Google Scholar]