Abstract
Ilizarov frames provide a versatile fixation system for the management of bony deformities, fractures and their complications. The frames give stability, soft tissue preservation, adjustability and functionality allowing bone to realise its full osteogenic potential. It is important that we have a clear and concise understanding of the Ilizarov principles of deformity correction to best make use of this fixation system. In this review article, the history of Ilizarov frame, the basic sciences behind it, the mechanical principles governing its use and the clinical use of the fixation system are discussed.
Keywords: Ilizarov, Mechanical principles, Deformity correction
History of Ilizarov
Prof. Gavriil Abramovich Ilizarov started his career treating a number of patients in western Siberia, who had returned from World War II having sustained fractures. During the 1950s, Ilizarov began experimenting with external fixation designs; in 1954, he successfully treated his first patient, a factory worker with a tibial non-union. He experienced excellent results, significantly reducing healing time. During this time, he also, by chance, discovered distraction osteogenesis for bone lengthening when he observed callus formation in a patient who had mistakenly distracted his frame instead of compressing it.
In 1968, Valery Brumel, an Olympic champion high jumper at the 1964 games, visited Ilizarov in Kurgan. He had suffered a compound fracture of his distal tibia in 1965 and, despite 20 operations over 3 years, had developed an infected non-union and a significant leg-length discrepancy. His resultant surgery was a widely publicised success and gained Ilizarov recognition within the Soviet Union.
In 1980, Carlo Mauri, a well-known Italian journalist and explorer, was treated in Kurgan. Mauri had suffered a distal tibial fracture 10 years previously during an Alpine accident. Whilst on an Atlantic exploration, his old leg wound re-opened and a Russian team physician advised him to consult Ilizarov in Kurgan. On his return to Italy, the surgeons were amazed by the healing that had occurred in this long-standing non-union and, the following year, arranged for Ilizarov to present his findings at the AO Conference in Bellagio. News of this advance was quick to travel and very soon was being adopted by surgeons both sides of the Atlantic.
Basic science and principles of distraction osteogenesis
Over a 10-year period, a series of experiments were conducted using 65 dogs to understand better the process of distraction osteogenesis.1 These experiments found that ideal conditions included stable fixation, a low energy osteotomy followed by 5-7-day latency, and a distraction rate of 1mm/day in 3 or 4 divided increments.2,3 These findings were mirrored clinically in human studies.4 Prior to these studies, rate and rhythm of distraction were not considered important.5,6
During distraction, regenerate bone arises between the entire cross-sections of each distracted bone surface with a central radiolucent fibrous interzone comprising of type I collagen. New bone trabeculae form directly from this central collagen zone extending to both bone surfaces.7 It is orientated parallel to the distraction force and surrounded by blood vessels. Following distraction, these microcolumns consolidate and rapidly remodel to form a structure similar in composition to that of the host bone, a process called consolidation.
Up to 10% lengthening is well-tolerated by muscle, but substantial histopathological changes occur after lengthening of 30%.8–10 Nerves, arteries and veins had histological evidence of temporary degenerative changes but these disappeared 2 months after lengthening.11,12 Short-term changes in articular cartilage of the knee in tibial lengthening of rabbits showed that the cartilage underwent histopathological changes, including reduced thickness of the hypertrophic and proliferative zones.13
Mechanical principles of the Ilizarov method
Circular fixators are comprised of several components, the most fundamental being rings and connecting rods. Full rings provide the most rigidity; partial rings and arches are particularly helpful when working near joints and allow wound access needed after trauma.
Bony stability is essential for osteogenesis and is dependent on the stability of the external frame. Frame stability is greatly impacted by the ring properties; rings of large diameter are less stable than smaller rings.14 Reducing ring diameter by 2 cm increases axial frame stiffness by 70%;15 therefore, the smallest diameter ring that will fit the extremity should be used. A general guideline is to leave 2-cm space between ring and skin circumferentially to allow for possible limb swelling. Distance between the rings will also affect stability; rings that are far apart and connected with long rods will be less stable. In order to minimise the unsupported length between rings, additional connecting rods or an intermediate free ring secured in the mid-portion of the long rods should be used.
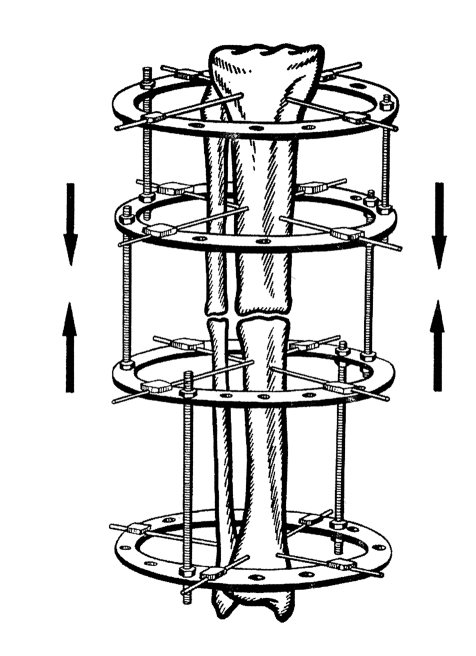
The stability of the ring is further increased by using two rings instead of one for each bone segment, thus controlling both near and far ends of each bone segment. A minimum of four connecting rods between the rings and at least two points of fixation or wires per ring are required (Fig. 1).16 Atrophic non-unions require double ring blocks to increase the stability of the construct. In hypertrophic non-unions, one ring block per segment would be sufficient as long as no deformity correction is needed. Lengthening frames usually gain and sustain additional stability from distraction forces needed to overcome the soft tissue envelope; therefore, one ring per segment with multiple wires in different planes would be used.
Figure 1.
Two ring blocks being compressed together. Note each block consists of two rings with two points of fixation per ring. Threaded rods are parallel to each bone segment, preserving alignment of the entire bone. Although this illustration only depicts two connecting rods, four are needed for adequate stability.16
The ring frame supports and stabilises the underlying bone through the use of transfixion wires and half pins. Frame stability increases with increasing wire diameter and tension, the use of more wires per ring, placing wires on opposite sides of the ring and inserting wires in different planes. Increasing crossing angles of wires to 90° provides maximal stability and crossing angles of less than 60° may allow the bone to slide along the wires requiring the use of opposing olive wires or the addition of a half pin.6 Olive wires provide an important buttress effect in the correction of angular deformity.16
A thorough knowledge of the cross-sectional anatomy of the extremity is necessary to avoid neurovascular injury. If under a general anaesthetic, the patient should not receive paralytic agents as this will mask the important signs of muscle flickering when a motor nerve is irritated. It is important to minimise the heat generated during wire drilling to prevent bone and soft tissue necrosis. Wire ten-sioning greatly enhances the rigidity of the wire and stability of the frame.17 Smooth wires are typically tensioned to 130 Nm as tension beyond 155 Nm will cause stretching and plastic deformity of the wire.18 Wires crossing an angle of less than 60° should be tensioned simultaneously to ensure equal tension across both wires. Studies comparing wire-only frames and combination half-pin frames have shown that the use of half-pins increased the bending and torsion-al stiffness of the frame.19 Hydroxyapatite-coated pins have become increasingly popular, especially in limb lengthening and deformity surgery where the frames stay on for several months. Hydroxyapatite-coated pins have been shown to have increased extraction torque, lower rates of loosening and decreased infection rates.20,21
Deformity correction can be achieved using hinges on the connecting rods but this requires very accurate frame construction (Fig. 2)22 to avoid lengthening, compression or translation. As a consequence, hexapod systems, such as Taylor-spacial frames, have become popular. Readings on six oblique struts and measurements taken from postoperative radiographs are fed into a computer program to provide a protocol for daily adjustments to correct a deformity.
Figure 2.

By placing the hinge on the bisector line and off the cortex correcting the deformity will cause distraction at the bone ends (A). Positioning the hinge off the bisector will cause a translational deformity (B).16
Clinical use of Ilizarov external fixators
Deformity assessment requires a thorough knowledge of normal anatomical alignment and rotation. Usually, the contralateral limb can be used as a reference, and radiographs are a routine part of deformity and leg-length discrepancy investigation. A full-length, standing, anteroposte-rior radiograph of both lower limbs, using blocks under the short leg to level the pelvis, are taken. Anteroposterior and lateral radiographs will guide management and provide a template for pre-operative planning.
To correct the leg-length discrepancy, a corticotomy is performed, the bone is exposed and the periosteum incised and elevated paying careful attention to preserve its integrity. Using a 4.8-mm drill, holes are made circumferentially through the cortex and the corticotomy is completed using an osteotome. For tibial lengthening, the suggested site of corticotomy is at the junction between proximal metaphysis and diaphysis, distal to the tibial tuberosity. Femoral lengthening corticotomies are usually just distal to the lesser tro chanter.
To correct angular deformity, an awareness of the normal mechanical axis is required. This represents a line drawn from the centre of the femoral head to the centre of the ankle mortice. The location of this line in relation to the knee joint defines the mechanical axis deviation, normally 0-8 mm medial to the centre of the knee. Figure 3 shows that deviations from this value denote varus or valgus deformities.16 The site of the deformity must be identified and mid-diaphyseal lines can be drawn on a radiograph on either side of a deformity. The point at which these lines bisect is the centre of rotation and angulation (CORA), and the angle between these lines is the magnitude of the deformity (Fig. 4).16 A corrective osteotomy at this site will allow angular correction without translation. In cases where there is length discrepancy and angular deformity, correction can be made at one level, the CORA, if bone regeneration potential is good. Alternatively, a double level osteotomy may be performed, one at CORA for deformity correction and one at the advised level for lengthening.
Figure 3.
Due to the tibial deformity, the mechanical axis deviation has been moved medially, and as a result a varus deformity is present.22
Figure 4.
CORA is present at the bisection of the mid-diaphyseal lines, the angle between the two lines denotes the magnitude of deformity.22
Gradual correction and lengthening uses the principle of ‘distraction osteogenesis'. Bone and soft tissue are gradually distracted at a rate of 1 mm per day in four divided increments. Bone growth in the distraction gap is called regenerate. The interval between osteotomy and lengthening is called the latency phase and is usually 7-10 days. The correction and lengthening is called the distraction phase. The time from the end of distraction until bony union is called the consolidation phase. Methods of bone separation that disrupt the periosteum, such as widely displaced corticotomies or osteotomies, can result in decreased osteogenesis.23
The optimum way to treat hypertrophic non-unions is via gradual distraction to achieve normal alignment. Only modest lengthening of 1.5 cm can be achieved through the non-union. If additional lengthening is required, a further corticotomy will need to be performed. In atrophic non-unions, the treatment needs to be directed to improve the biology and mechanical environment of the union site. Atrophic non-unions should be exposed and bone ends contoured so there is healthy bleeding bone on both sides with good contact. Acute correction of deformity should be followed by bone grafting and stable fixation with compression.
In infected non-unions, the non-union must be exposed and all infected bone removed by opening of intramedullary canals with thorough washout. Bone should be excised back to bleeding surfaces and apposed with good contact and correction of deformity. The patient should ideally have not been receiving antibiotics for several weeks and multiple intra-operative specimens for culture and pathology should be sent. Bone graft should not be used in the primary surgery, if there is a gap between the two bone ends antibiotic beads can be used for dead-space management. Several weeks later, the antibiotic beads can be removed and the non-union can be bone grafted.24
Complications
Immediate complications involve direct damage to neu-rovascular structures. Early complications are pain, bleeding that can result in haematoma or compartment syndrome, deep vein thrombosis and pulmonary embolism, and nerve injury as a result of stretching. Infection, especially of the pin sites, has been reported to be as high as 95%; however, with local pin care, with or without oral administration of antibiotics for 5 days, 97% of these resolved.25 Soft tissue contractures, subluxation and contra cture of the joint are more serious complications. They can, however, be minimised with pre-operative planning, including protection against subluxation by spanning of the joint with the fixator and with intensive therapy and splinting during the fixation period.26 Late complications include chronic recurrent pin-site infections, osteomyelitis, premature union if distraction is too slow or delayed or non-union, hardware failure, reflex sympathetic dystrophy, late bowing and fracture.
The rate of complications decreases substantially as the experience of the surgeon increases. In one study, major complications followed 69% Ilizarov lengthenings performed in the first 6-month period of experience, but only 35% in the third 6-month period.27 The rate of minor complications remained constant independent of the experience of the surgeon and type of fixator.
Summary
Ilizarov frames provide a versatile fixation system that gives stability, soft tissue preservation, adjustability and functionality. All these factors are vital for bone to realise its full osteogenic potential. A pre-operative plan is essential with careful selection of patients who will be able to adhere to the strict postoperative regimen of lengthening and angular correction to avoid late complications.
References
- 1.Ilizarov GA, Ledyasev VI, Shitin VP. Experimental studies of bone lengthening. Eksp Khir Anesteziol. 1969;14:3. [PubMed] [Google Scholar]
- 2.Ilizarov GA. The tension-stress effect on the genesis and growth of tissues: Part I. The influence of stability of fixation and sort tissue preservation. Clin Orthop. 1989;238:249–81. [PubMed] [Google Scholar]
- 3.Ilizarov GA. The tension-stress effect on the genesis and growth of tissues: Part II. The influence of the rate and frequency of distraction. Clin Orthop. 1989;239:263–85. [PubMed] [Google Scholar]
- 4.Ilizarov GA. Clinical application of the tension-stress effect for limb lengthening. Clin Orthop. 1990;250:8–26. [PubMed] [Google Scholar]
- 5.Codivilla A. On the means of lengthening in the lower limbs, the muscles and tissues which are shortened through deformity. Am J Orthop Surg. 1905;2:353–69. [Google Scholar]
- 6.Wagner H. Operative lengthening of the femur. Clin Orthop. 1978;136:125–42. [PubMed] [Google Scholar]
- 7.Vauhkonen M, Peltonen J, Karaharju E, Aalto K, Alitalo I. Collagen synthesis and mineralization in the early phase of distraction bone healing. Bone Miner. 1990;10:171–81. doi: 10.1016/0169-6009(90)90260-m. [DOI] [PubMed] [Google Scholar]
- 8.Kaljumae U, Martson A, Haviko T, Hanninen O. The effect of lengthening of the femur on the extensors of the knee. An electromyographic study. J Bone Joint Surg Am. 1995;77:247–50. doi: 10.2106/00004623-199502000-00011. [DOI] [PubMed] [Google Scholar]
- 9.Paley D. Problems, obstacles and complications of limb lengthening by the Ilizarov technique. Clin Orthop. 1990;250:81–104. [PubMed] [Google Scholar]
- 10.Lee DY, Choi IH, Chung CY Chung PH, Chi JG, Suh YL. Effect of tibial length ening on the gastrocnemius muscle. A histopathologic and morphometric study in rabbits. Acta Orthop Scand. 1993;64:688–92. doi: 10.3109/17453679308994599. [DOI] [PubMed] [Google Scholar]
- 11.Ippolito E, Peretti G, Bellocci M, Farsetti P, Tudisco C, et al. Histology and ultrastructure of arteries, veins and peripheral nerves during limb lengthening. Clin Orthop. 1994;308:54–62. [PubMed] [Google Scholar]
- 12.Galardi G, Comi G, Lozza L, Marchettini P, Novarina M, et al. Peripheral nerve damage during limb lengthening. Neurophysiology in five cases of bilateral tibial lengthening. J Bone Joint Surg Br. 1990;72:121–4. doi: 10.1302/0301-620X.72B1.2298769. [DOI] [PubMed] [Google Scholar]
- 13.Lee DY, Chung CY, Choi IH. Longitudinal growth of the rabbit tibia after callotasis. J Bone Joint Surg Br. 1993;75:898–903. doi: 10.1302/0301-620X.75B6.8245079. [DOI] [PubMed] [Google Scholar]
- 14.Cross AR, Lewis DD, Murphy ST. Effects of ring diameter and wire tension on the axial biomechanics of four ring circular external fixator constructs. Am J Vet Res. 2001;62:1025–30. doi: 10.2460/ajvr.2001.62.1025. [DOI] [PubMed] [Google Scholar]
- 15.Gasser B, Boman B, Wyder D. Stiffness characteristics of the circular Ilizarov device as opposed to conventional external fixators. J Biomech Eng. 1990;112:15–21. doi: 10.1115/1.2891120. [DOI] [PubMed] [Google Scholar]
- 16.Rozbruch SR, Ilizarov S. Limb Lengthening and Reconstruction Surgery. New York: Informa Healthcare; 2007. [Google Scholar]
- 17.Podolsky A, Chao EY. Mechanical performance of Ilizarov circular frame exter nal fixators in comparison with other external fixators. Clin Orthop. 1993;293:61–70. [PubMed] [Google Scholar]
- 18.Ilizarov GA, Emilyanova HS, Lebedev BE. Perosseus compression and distraction osteosynthesis. Traumatology and Orthopaedics. Kurgan: 1972. Some experimental studies. Mechanical characteristics of Kirschner wires; pp. 34–47. l. [Google Scholar]
- 19.Calhoun JH, Li F, Bauford WL. Rigidity of half pins for the Ilizarov external fixator. Bull Hosp J Dis. 1992;52:21–6. [PubMed] [Google Scholar]
- 20.Piza G, Caja VL, Gonzalez-Viejo MA. Hydroxyapatite-coated external-fixation pins. The effect on pin loosening and pin-tract infection in lengthening for short stature. J Bone Joint Surg Br. 2004;86:892–7. doi: 10.1302/0301-620x.86b6.13875. [DOI] [PubMed] [Google Scholar]
- 21.Pommer A, Muhr G, David A. Hydroxyapatite-coated Schantz pins in external fixators for distraction osteogenesis: a randomised, controlled trial. J Bone Joint Surg Am. 2002;84:1162–6. doi: 10.2106/00004623-200207000-00011. [DOI] [PubMed] [Google Scholar]
- 22.Paley D. Principles of Deformity Correction. Berlin: Springer; 2001. [Google Scholar]
- 23.Frierson M, Ibrahim K, Boles M, Bote H, Ganey T. Distraction osteogenesis. A comparison of corticotomy techniques. Clin Orthop. 1994;301:19–24. [PubMed] [Google Scholar]
- 24.McKee MD, Wild LM, Schemitsch EH, Waddell JP. The use of antibiotic-impregnated, osteoconductive, bioabsorbable bone substitute in the treatment of infected long bone defects: Early results of a prospective trial. J Orthop Trauma. 2002;16:622–7. doi: 10.1097/00005131-200210000-00002. [DOI] [PubMed] [Google Scholar]
- 25.Aronson J. Experimental and clinical experience with distraction osteogenesis. Cleft Palate Craniofac J. 1994;31:473–81. doi: 10.1597/1545-1569_1994_031_0473_eacewd_2.3.co_2. [DOI] [PubMed] [Google Scholar]
- 26.Coglianese DB, Herzenberg JE, Goulet JA. Physical therapy management of patients undergoing limb lengthening by distraction osteogenesis. J Orthop Sports Phys Ther. 1993;17:124–32. doi: 10.2519/jospt.1993.17.3.124. [DOI] [PubMed] [Google Scholar]
- 27.Velazquez RJ, Bell DF, Armstrong PF, Babyn P, Tibshirani R. Complications of use of the Ilizarov technique in the correction of limb deformities in children. J Bone Joint Surg Am. 1993;75:1148–56. doi: 10.2106/00004623-199308000-00004. [DOI] [PubMed] [Google Scholar]