Abstract
Objectives
To empirically test a multilevel conceptual model of children’s oral health incorporating 22 domains of children’s oral health across four levels: child, family, neighborhood and state.
Data source
The 2003 National Survey of Children’s Health, a module of the State and Local Area Integrated Telephone Survey conducted by the Centers for Disease Control and Prevention’s National Center for Health Statistics, is a nationally representative telephone survey of caregivers of children.
Study design
We examined child-, family-, neighborhood-, and state-level factors influencing parent’s report of children’s oral health using a multilevel logistic regression model, estimated for 26 736 children ages 1–5 years.
Principal findings
Factors operating at all four levels were associated with the likelihood that parents rated their children’s oral health as fair or poor, although most significant correlates are represented at the child or family level. Of 22 domains identified in our conceptual model, 15 domains contained factors significantly associated with young children’s oral health. At the state level, access to fluoridated water was significantly associated with favorable oral health for children.
Conclusions
Our results suggest that efforts to understand or improve children’s oral health should consider a multilevel approach that goes beyond solely child-level factors.
Keywords: children’s oral health, multilevel modeling, multiple imputation
Despite reductions in dental caries rates over the past 25 years resulting from water fluoridation, fluoride toothpaste use, and improvements in oral hygiene and nutrition, dental caries remains the most common chronic childhood disease, overall (1), and the cause of the vast predominance of oral health problems in children. Nationally, 42% of children 2–11 years old have caries experience in their primary teeth, with 23% having untreated caries; among 12–19-year-olds, 59% have caries experience in their permanent teeth with 20% having untreated caries (2). Dental caries accounted for 117 lost school-hours per 100 school-age children in 1989 (3). As overall caries rates decrease, diminishing returns can be expected from applying current individual-based approaches to fight disease.
Population health research has looked beyond the biomedical model to explain disease states, but with the exceptions of water fluoridation and school-based dental sealant programs, population-based approaches have not been implemented extensively in oral health. Health conditions (e.g., diabetes and HIV), health behaviors (e.g., use of alcohol, tobacco, sugary diet, certain drugs, and lack of preventive care), socioeconomic factors (e.g., lower education and income), and minority race/ethnicity are related to poor oral health (4–6). However, few models explain the relationships between the larger contextual, environmental and societal factors and oral health. An individual is exposed to multiple factors at a time and over a lifetime, so focusing primarily on traditional biomedical factors limits our understanding of how these different complex factors operate.
Population health models generally classify health determinants into five broad categories: genetic endowments, social environment, physical environment, health-influencing behaviors, and medical care (7–14). Critically, a multifaceted approach’s determinants do not act independently but complexly interact to impact population health (15, 16). Importantly, these determinants may vary with child age and developmental status (13).
A parallel approach centers on identifying dental and nondental oral health determinants (17–20). Much initial work focused on early childhood caries (21–23), while other efforts have examined the association between oral health and socioeconomic factors over time using a life-course approach (24). These studies proceed from the basic biological model and incorporate additional factors in the social and physical environment, including socioeconomic status, race/ethnicity, culture, stress, health behaviors and the health care system. Reisine et al. (21) found adding social and psychological variables improved predicting dental services utilization over solely biological variables. In related work, they described how dental knowledge and life stress predict decayed, missing, or filled surfaces or teeth (23). Several papers discuss incorporating psychosocial and behavioral indicators for dental health conceptually but few tested these empirically (20, 22, 25, 26).
Theoretical and conceptual work in population epidemiology by Susser and Susser (27), Kaplan (28) and others emphasize the multilevel nature of health determinants. Factors influencing health operate at individual, family, and community levels (28–32). Individual children live in families; families are embedded in communities. A child’s dental disease risk cannot be isolated from family and community disease risk. Hence, any comprehensive children’s oral health model must incorporate a multilevel perspective, as some oral health researchers have begun to do (4, 33, 34).
Over the past 20 years, dental caries rates have dropped dramatically. Fluoridated water is one of the most cost-effective preventive public health strategies, and is one of the few population-based preventive interventions with demonstrated cost-savings (35). Sealants are similarly cost-effective, and even cost-saving when applied to high-risk children (36). Added benefits are also seen from fluoride toothpastes (37).
Despite these gains, there are still wide variations in applying caries-preventing strategies. The percentage of the population with fluoridated water is only 67% in the United States, ranging from a low of 2.3% in Utah to 100% in Washington, DC (38). Sealants similarly are disparately applied, with those at greatest risk being less likely to receive them: rates for black and Mexican-American children are 33% lower than those for white children; children near poverty level are 50% as likely to have sealants as those ≥200% of the Federal Poverty Level (FPL) (2).
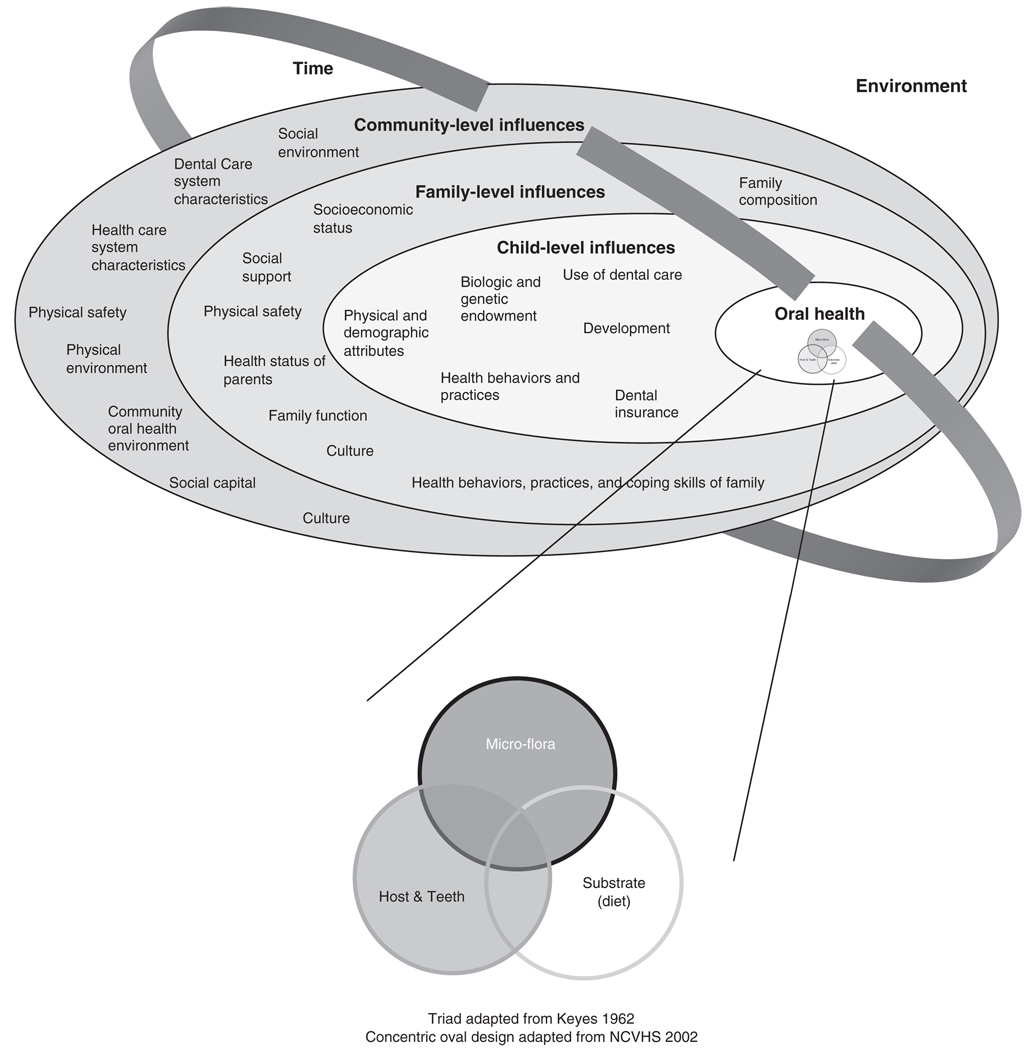
Building on the oral and population health literature, we developed a multilevel conceptual model of children’s oral health (4). That comprehensive review identified 22 oral health domains across three levels – the child, family and community – shown in Fig. 1. This analysis applies our multilevel conceptual model using data from a large, population-based national survey. Because the data are cross-sectional, our analysis is exploratory in nature and intended as an initial step to further understanding the factors that contribute to positive oral health among children. We hope the analysis presented here will provide a basis for the design of more specific studies of interventions to improve children’s oral health.
Fig. 1.
Child, family and community influences on oral health outcomes of children. Reproduced with permission from Pediatrics, Vol. 120 (3), Page e512, copyright © 2007 by the American Academy of Pediatrics.
Methods
Data
Data are from the 2003 National Survey of Children’s Health (NSCH), a module of the State and Local Area Integrated Telephone Survey conducted by the Centers for Disease Control and Prevention (CDC), National Center for Health Statistics (39). The sponsor was the Maternal and Child Health Bureau of the Health Resources and Services Administration (HRSA). The NSCH was conducted from January 2003 to July 2004, using random-digit-dialing to identify households with children. In each household, one child was randomly selected as the subject of an in-depth health interview. The respondent was the adult in the household most knowledgeable about the child’s health. Interviews were completed for 102 353 children in the United States, in English or Spanish (39).
The NSCH included data on the child’s health, health care access and utilization, and health insurance coverage; the child’s family’s functioning; and the child’s neighborhood (39). The NSCH also collected separate data for early childhood (ages 0–5) and middle childhood/adolescence (ages 6–17). The early childhood data included information on the child’s development, childcare, injuries, and breastfeeding. These different data collection components by age fit well with dentition stages; ages 1–5 represent primary dentition and ages 6–17 represent mixed and permanent dentition. Thus, our model of young children’s oral health includes children ages 1–5.
Levels of analysis
Respondents were sampled within states, providing for a natural hierarchy. The NSCH data also included subjective measures at the family and neighborhood levels. However, only one child per household was sampled and households were not geocoded to the neighborhood level, so the family and neighborhood levels were not distinguishable from the child level and could not be modeled statistically. Therefore, our model represents four conceptual levels (child, family, neighborhood, and state) but only two statistical levels (children within states), with our external geographic variables all measured at the state level. State-level variables that we tested were drawn from a variety of sources, including: HRSA’s Area Resource File; CDC’s National Oral Health Surveillance System; CDC’s Behavioral Risk Factor Surveillance System; Statistical Abstract of the United States; the Federal Bureau of Investigation’s Uniform Crime Reports; the Environmental Protection Agency; the Annie E. Casey Foundation’s Kids Count Data Book; and the US Census.
Variable specifications
Most variables in the model are dichotomous indicators where a value of 1 indicates the presence of the attribute described in the variable label (from Table 3) and a value of 0 indicates its absence. Seven variables (age in years, number of adults in household, number of children in household, number of family outings per week, number of residential moves, and the two state-level variables) are continuous measures.
Table 3.
Multilevel model of fair/poor parent-reported oral health among children 1–5 years of age
| 95% confidence interval |
||||||
|---|---|---|---|---|---|---|
| Level | Domain | Variable | Unadjusted odds ratio |
Adjusted odds ratio |
Lower limit |
Upper limit |
| Race/ethnicity | ||||||
| Child | Physical Attributes | Hispanic | 4.753*** | 1.512*** | 1.237 | 1.848 |
| Child | Physical Attributes | Non-Hispanic White (referent) | 1.00 | 1.00 | – | – |
| Child | Physical Attributes | Non-Hispanic Black | 2.419*** | 1.527*** | 1.225 | 1.904 |
| Child | Physical Attributes | Non-Hispanic Other | 2.003*** | 1.422*** | 1.155 | 1.751 |
| Child | Physical Attributes | Gender is male | 1.173** | 1.168** | 1.056 | 1.291 |
| Child | Development | Age in years | 1.420*** | 1.271*** | 1.215 | 1.328 |
| Child | Development | Child was ever breastfed | 0.729*** | 0.871* | 0.778 | 0.974 |
| Child | Dental Insurance | Child has no dental insurance | 1.346*** | 1.199** | 1.062 | 1.354 |
| Child | Use of Dental Care | Last dental visit was >1 year ago or never | 0.419*** | 0.439*** | 0.388 | 0.495 |
| Child/Family | Biological & Genetic Endowment/ | Either parent’s physical health is fair/poor | 3.236*** | 2.051*** | 1.774 | 2.372 |
| Child/Family | Health Status of Parents | Either parent’s mental health is fair/poor | 1.777*** | 1.353*** | 1.152 | 1.589 |
| Family Structure | ||||||
| Family | Family Composition | Two-parent biological/adoptive (referent) | 1.00 | 1.00 | – | – |
| Family | Family Composition | Step-family | 1.529** | 0.968 | 0.733 | 1.279 |
| Family | Family Composition | Single-mother family | 1.807*** | 1.049 | 0.898 | 1.225 |
| Family | Family Composition | Other family structure | 2.177*** | 1.770*** | 1.328 | 2.358 |
| Family | Family Composition | Number of adults in household | 1.213*** | 1.115*** | 1.061 | 1.171 |
| Family | Family Composition | Number of children in household | 1.224*** | 1.079** | 1.032 | 1.129 |
| Family | Family Function | Number of family outings per week | 0.891*** | 0.978* | 0.957 | 0.998 |
| Highest Education of any member in Household | ||||||
| Family | Socioeconomic Status | Less than High School/GED | 1.959*** | 1.457*** | 1.261 | 1.682 |
| Family | Socioeconomic Status | High School/GED (referent) | 1.00 | 1.00 | – | – |
| Family | Socioeconomic Status | More than High School/GED | 0.539*** | 0.662*** | 0.570 | 0.769 |
| Household Income relative to Federal Poverty Level | ||||||
| Family | Socioeconomic Status | Less than 50% of Federal Poverty Level (FPL) | 4.173** | 1.934 | 0.887 | 4.215 |
| Family | Socioeconomic Status | 50% to less than 100% of FPL | 3.390* | 1.687 | 0.841 | 3.382 |
| Family | Socioeconomic Status | 100% to less than 133% of FPL | 3.519* | 1.958* | 1.057 | 3.626 |
| Family | Socioeconomic Status | 133% to less than 150% of FPL | 2.141 | 1.333 | 0.574 | 3.097 |
| Family | Socioeconomic Status | 150% to less than 185% of FPL | 2.939* | 1.713 | 0.847 | 3.462 |
| Family | Socioeconomic Status | 185% to less than 200% of FPL | 2.727 | 1.821 | 0.825 | 4.019 |
| Family | Socioeconomic Status | 200% to less than 300% of FPL | 2.497 | 1.880* | 1.056 | 3.349 |
| Family | Socioeconomic Status | 300% to less than 400% of FPL | 1.578** | 1.253 | 0.955 | 1.645 |
| Family | Socioeconomic Status | 400% of FPL or higher (referent) | 1.00 | 1.00 | – | – |
| Family | Health Behaviors/Practices/Coping | Either parent does not regularly exercise | 1.488*** | 1.337*** | 1.202 | 1.487 |
| Family | Health Behaviors/Practices/Coping | Either parent has no health insurance | 2.306*** | 1.369*** | 1.186 | 1.581 |
| Family | Health Behaviors/Practices/Coping | Index, how well parent is coping with raising child | 0.403*** | 0.601*** | 0.538 | 0.672 |
| Family | Social Support | Number of times child has ever moved residence | 1.194*** | 1.038 | 0.997 | 1.081 |
| Family | Culture | Primary language spoken at home is not English | 3.804*** | 1.517*** | 1.273 | 1.806 |
| Family | Culture | Child was born outside of the United States | 1.884*** | 1.563** | 1.202 | 2.033 |
| Neighborhood | Social Capital | Presence of bad neighborhood influences on children | 1.161* | 1.198** | 1.073 | 1.337 |
| Neighborhood | Social Capital/Physical Safety | Index, whether parent feels neighbors help, watch out for, count on or trust each other, neighborhood is safe | 0.476*** | 0.756*** | 0.674 | 0.848 |
| Metropolitan Statistical Area (MSA) Status | ||||||
| Neighborhood | Social Environment | In an MSA, in central city | 1.032 | 0.807** | 0.691 | 0.943 |
| Neighborhood | Social Environment | In an MSA, not in central city | 0.717*** | 0.807** | 0.688 | 0.945 |
| Neighborhood | Social Environment | Not in an MSA (referent) | 1.00 | 1.00 | – | – |
| State | Social Environment | Gini Index of income inequality (US Census) | 1.009 | 0.954* | 0.916 | 0.993 |
| State | Physical Environment | Percent of population with access to fluoridated water (NOHSS) | 0.993*** | 0.995** | 0.991 | 0.998 |
P < 0.05;
P < 0.01;
P < 0.001.
Note: Sample size = 26 736; Unadjusted odds ratios are from single-domain models run on imputed data. Data Source = National Survey of Children’s Health 2003; US Census 2000; CDC National Oral Health Surveillance System 2000 (NOHSS).
Two variables require more explanation. In both cases, maximum-likelihood factor analysis and Cronbach’s alpha indicated that a group of variables was highly correlated and may have been measuring the same underlying construct (results available upon request).
First, we constructed a parental coping index averaging values of five variables that assessed how often parents felt that: they were not coping well with parenting demands; their child was harder to care for than other children; the child did things that really bothered the parent; they were giving up too much to meet the child’s needs; and they felt angry with the child. Second, we constructed a dichotomous variable that indicated whether parents usually or always felt their child was safe in the neighborhood and agreed that people in the neighborhood help each other, watch out for each other’s children, can be counted on, and can be trusted to help the child (if any condition was not met, the indicator was coded to 0).
Operationalizing the complex social constructs included in our conceptual model – such as ethnicity, language and culture – required use of proxy variables from the NSCH and other sources. Table 1 shows how each construct was specified in our empirical model.
Table 1.
Child-, family-, and community-level influences on young children’s oral health
| Child-level domains | Family-level domains | Community-level domains (neighborhood or state) |
|---|---|---|
| Physical Attributes | Family Composition | Culture |
| Race/ethnicity | Family structure | Percent of population non-English |
| Sex | Household size | speakingc,d |
| Biologic/Genetic Endowment | Family Function | Social Capital |
| Physical health of parents | Religiositya | Whether neighbors help/watch out |
| Mental health of parents | Family time readingb | for/count on/trust each other |
| Birth ordera | Family outings | Presence of bad influences on child |
| Development | Eating meals togetherb | Percent of housing owner-occupiedc,d |
| Age | Socioeconomic Status | Percent of population in same |
| Breastfeeding | Highest education in household | residence 1995–2000c,d |
| Health Behaviors & Practices | Family income | Social Environment |
| Special health care needsb | Parental unemploymenta | Metropolitan statistical area status |
| Dental Insurance | Health Status of Parents | Percent of population in urban areasc,d |
| Dental insurance coverage | Physical health of parents | Percent of population in povertyc,d |
| Use of Dental Care | Mental health of parents | Unemployment ratec,d |
| Dental visit in last year | Health Behaviors, Practices & Coping | Percent of children with unemployed |
| Skills of Family | parentsc,d | |
| Parental exercise patterns | Income inequalityc | |
| Parental health insurance coverage | Percent of families female-headedc,e | |
| Parental coping with child raising | Percent of 8th-graders below basic | |
| Handling family disagreements by | reading levelc,d | |
| Keeping opinions to selfa | Physical Environment | |
| Discussing calmlyb | Population density per square milec,d | |
| Arguinga | Percent of housing with standard | |
| Hitting/throwing thingsb | plumbingc,d | |
| Social Support | Percent of population with access to | |
| Frequency of residential moves | fluoridated waterc | |
| Physical Safety | Percent of population ages 12–17 who | |
| Perceptions of child’s safety at | smokec,d | |
| homea | Percent of population ages 18–25 | |
| Culture | who smokec,d | |
| Language spoken at home | Percent of children in crowded housingc,d | |
| Child born in the United States | Percent of population affected by | |
| Parents born in the U.S.a | health-based violations in water | |
| supply c,d | ||
| Percent of children with elevated blood | ||
| lead level c,d | ||
| Physical Safety | ||
| Perceptions of child safety in | ||
| neighborhood | ||
| Crime ratec,d | ||
| Community Oral Health Environment | ||
| Percent of adults with teeth cleaning, | ||
| previous yearc,d | ||
| Percent with no dental visit in last 2 yearsc,d | ||
| Dental Care System Characteristics | ||
| Supply of dentistsc,d | ||
| Health Care System Characteristics | ||
| Supply of doctorsc,d | ||
| Percent of population uninsuredc | ||
| Percent of children uninsuredc | ||
| Medicaid/SCHIP funding per capitac,d | ||
| Vaccination coveragec,d | ||
| Age-adjusted mortality ratec,d | ||
| Low-birth-weight ratec,e |
Nonsignificant at 0.10 level in single-domain model.
Significant in single-domain model but not significant at 0.10 level in full model.
State-level characteristic.
Nonsignificant at 0.10 level in mixed models with 1 state characteristic.
Reduced to nonsignificance (at 0.10 level) in mixed models with multiple state characteristics.
Imputation
Many factors were considered for inclusion in our model of children’s oral health. The cumulative effect across many variables of discarding observations with missing data could potentially bias our results, if a substantial proportion of the sample were excluded from the analysis. Our full model with unimputed data discards 20% of the sample due to missing values on various covariates. To overcome this limitation, we used IVEware, a multivariate sequential regression imputation software package designed for complex data structures (40). With IVEware, we used all our analysis variables to impute a range of plausible values for missing cases on each explanatory variable, generating a set of five imputed databases. Multiple imputation allows for variation across the five data sets to reflect the uncertainty of imputed data, and research indicates that five is a sufficient number of data sets for this purpose (41).
These datasets were analyzed using ordinary sas procedures (described below) along with the sas procedure mianalyze to aggregate results to obtain proper standard errors accounting for additional variation across imputed data sets (42). The variable requiring the most imputation (9.2% of children) was household income relative to the FPL. The variable indicating whether people in the neighborhood might be a bad influence on children required 4.9% imputation; the variable indicating how often the respondent felt the child was safe in the neighborhood required 4.2% imputation; and the child dental insurance variable required 3.1% imputation. No other variable needed more than 2% imputation.
Statistical analyses
Our dependent variable is a dichotomous indicator coded from the question: “How would you describe the condition of (child)’s teeth? (excellent, very good, good, fair or poor)” Our model compares excellent, very good or good oral health to fair or poor oral health. We excluded children with no teeth or under age 1 from our analysis, resulting in a sample size of 26 736 children ages 1–5. The unweighted percentage of sample children ages 1–5 whose teeth were rated as fair/poor was 5.1% (the weighted population estimate of fair/poor oral health was 6.7%).
We used the model-based approach to analyzing sample surveys (43–45) in sas procedure glimmix to fit mixed models for dichotomous dependent variables with random state effects. We included variables used to create the NSCH sampling weights as covariates. The NSCH sampling weights were adjusted to account for noncoverage of households without landline telephones (nontelephone or wireless-only households), so our results represent all children ages 1–5 in United States households (39).
Table 1 lists the indicators chosen to represent each domain and analysis level, based on an extensive literature assessment and development of our comprehensive conceptual model (4), shown in Fig. 1. Our data set included too many candidate variables for one model and multiple possible indicators for some domains. This necessitated a modeling approach reducing the number of factors for the final model. Although guided by our conceptual model and literature review, the modeling approach is necessarily exploratory in nature.
We began the modeling process by fitting single-domain models with unimputed data at the individual level. That is, for each domain, we fitted a model including all individual-level characteristics from that domain (as listed in Table 1). We then constructed a full model that included all characteristics that were found to be significant at the 0.10 level in any single-domain model. We then re-fitted the full model using imputed data and examined the effects for robustness across unimputed and imputed models (no substantial differences were found). We next sequentially trimmed the model variables that were not significant at the 0.10 level in the full model. Finally, we tested each state-level characteristic in the model, keeping those with significant effects at the 0.10 level. Preliminary model results are available upon request from the authors.
We took multiple steps to reduce multicollinearity during the modeling process, including checking for high correlations between independent variables prior to inclusion in the models, developing scales of similar measures using factor analysis, and examining changes in the coefficients and standard errors. The model was assessed for multicollinearity problems using criteria of 2.5 for the variance inflation factor and 0.4 for tolerance (46). The model was not affected by multicollinearity based on these criteria.
We present odds ratios and associated 95% confidence intervals for the model variables. For discrete variables, the odds ratio represents the odds of having fair/poor oral health for children in a particular category, relative to the omitted (referent) category. For continuous variables, the odds ratio represents the incremental increase/decrease in the odds of having fair/poor oral health for each incremental increase in the continuous variable value. Hence, comparisons of the sizes of odds ratios for continuous and dichotomous variables are not appropriate.
Table 1 indicates factors that were (i) not significant at the 0.10 level in single-domain models; (ii) significant in single-domain models but not significant at the 0.10 level in the full model; (iii) state-level factors that were not significant at the 0.10 level in mixed models with one state characteristic; or (iv) state-level factors that were significant at the 0.10 level in single-characteristic mixed models but were reduced to nonsignificance at the 0.10 level when other state-level characteristics were added to the model. Variables meeting any of these criteria were excluded from the final model. Variables with no annotation in Table 1 are included in the final model.
Assessing model fit is complicated in sas proc glimmix, which does not provide likelihood values for likelihood ratio tests. The fit statistics produced in glimmix are pseudo-likelihoods that should not be compared across models to determine model fit (SAS Institute, 2006). We used theory and prior knowledge to construct our model, and used decision rules regarding the significance of covariates to guide what remained in the model.
Results
Model fit
The estimate of residual variance for the null model is 0.9835 and for the full model, 0.8978, indicating an 8.7% reduction in residual variance when our covariates are included in the model (Table 2). The ratio of the generalized chi-square statistic and its degrees of freedom in the full model is 0.90 (close to 1), indicating that there is little residual over-dispersion and the variance in the data has been modeled appropriately.
Table 2.
Random effects and model fit for the null and full models of fair/poor parent-reported oral health among children 1–5 years of age
| Covariance parameter estimates | Model fit statistic | ||
|---|---|---|---|
| Model | Parameter | Estimate (SE) | Generalized chi-square/DF |
| Null Model | Intercept | 0.1007 (0.000827) | 0.98 |
| Residual | 0.9835 (0.000073) | ||
| Full Model | Intercept | 0.0438 (0.0178) | 0.90 |
| Residual | 0.8978 (0.0082) | ||
Data Source = National Survey of Children’s Health 2003; US Census 2000; CDC. National Oral Health Surveillance System 2000.
Results by domain
Table 3 presents the multilevel model, based on imputed data, for parent-reported fair/poor oral health for children 1–5 years old. Five of six child-level domains and seven of eight family-level domains listed in Table 1 are represented in Table 3 (although family level social support is not significant at the 0.05 level in the final model). Four community-level domains (at either neighborhood- or state-level) showed statistically significant effects at the 0.05 level for young children: social environment, social capital, physical safety, and physical environment.
Of the 22 domains listed in Table 1, only seven were not significantly related at the 0.05 level to children’s oral health in the final model: child-level health behaviors and practices; family-level social support and physical safety; and four community-level domains: oral health environment, dental care system characteristics, health care system characteristics, and community-level culture (although family-level culture was significant).
Results by level
Our generalized linear mixed model produces parameter estimates for two statistical levels: child and state. However, many characteristics measured at the child level measure aspects of the family or neighborhood in which the child lives, resulting in four conceptual levels: child, family, neighborhood, and state. By conceptual level, the child, family, neighborhood and state levels were all found to include significant effects at the 0.05 level (Table 3).
Social environment was significant at both neighborhood and state levels. Children who live in Metropolitan Statistical Areas are less likely to be rated fair/poor than children in nonmetro areas, and children who live in states with higher income inequality were less likely to be rated fair or poor.
Results by variable
Oral health was less likely to be rated fair/poor in young children if they were non-Hispanic white or female, were ever breastfed, last saw a dentist more than a year ago or never, were born in the US, spoke English at home, lived in the city or suburbs, or if both parents were in good physical and mental health, exercised regularly and had health insurance. The likelihood of having fair/poor oral health decreased for younger children and those who went on family outings more often, and for children in households with fewer children, fewer adults, or higher education. Oral health was more likely to be rated fair/poor for children with no dental insurance, if the parents did not report coping well with raising children, if there were bad influences in the neighborhood, or the neighborhood was unsafe. Children in states with greater income inequality were less likely to be rated fair/poor. An increase in the percent of the state’s population with access to fluoridated water of 10% points was associated with a 4% decrease in a young child’s odds of having fair/poor oral health.
Discussion
This analysis is the first to empirically consider a range of correlates for children’s oral health based on a comprehensive conceptual model with nationally representative data. It is intended to provide researchers, advocates and dental professionals with information on factors associated with children’s oral health as reported by their parents. Although our results are provisional, they represent an important step forward since they are based on a comprehensive conceptual model and encompass biological, environmental, social and behavioral correlates that have not been studied together previously. As we discuss below, our findings can be used as a basis for future investigations of specific interventions to improve the oral health of children.
Our goal was to identify factors associated with oral health operating at the child, family, neighborhood and state levels. Several important findings emerged from our analysis. First, we found relatively few significant correlates of oral health at the state level. This is not to say that factors acting at the state level are not important. We found that state-level access to fluoridated water was associated with better oral health for young children. But, for the most part, significant effects were found for variables measured at child, family and neighborhood levels.
Second, we found evidence that most domains in our conceptual model are associated with oral health outcomes for children. Measures of biologic and genetic endowment, physical attributes, development, dental insurance, use of dental care, family composition, family function, socioeconomic status, health behaviors and coping skills, culture, social environment, social capital and physical environment were significant correlates of oral health. Our analysis showed that domain effects were significant at the child, family and community levels. However, we did not evaluate the relative importance of different domains, so further research with multifactorial approaches is encouraged. Such studies can help inform policymakers concerning the domains and levels where interventions would be most efficacious.
Some surprising exceptions to the general finding that most domains mattered were the lack of significant effects of community oral health environment and health care and dental care system characteristics, which would seem to be directly relevant. These domains may be important for older children, an avenue for further research. Another surprise was the direction of the use of dental care effect: compared with children whose last dental visit occurred during the previous year, young children whose last dental visit was more than a year ago or who had never had a dental visit had better perceived oral health. This is likely due to very young children being more likely to be taken to the dentist only if they exhibit recognizable problems with their teeth or specific complaints, and less likely if primary teeth were considered to be temporary or unimportant. Not recognizing that the child’s teeth are in poor condition could result in (i) not taking the child to the dentist and (ii) not rating the oral health as fair or poor.
Primary language spoken at home was an important correlate of children’s oral health. Results indicate children in households where the primary language was not English had about 1.5 times the odds of being in fair/poor oral health as children in English-speaking households. This is particularly striking since the model controls for household income and education and child race/ethnicity, nativity, dental insurance, and use of dental care. If other studies confirm this finding, additional health education and health promotion efforts in culturally appropriate languages may be needed to reach nonEnglish speakers.
Interestingly, we found that children in states with greater income inequality were less likely to have fair/poor oral health, while family income measured at the individual-level was inversely related to worse oral health in our model. Other surveys have also documented that individual-level income is inversely related to poor health in the general population (1), but no studies have reported the converse association we found at the state level. The state may be too large of a geographic unit for this kind of measure to have much meaning. Alternately, the Gini Index may be acting as a proxy for other factor(s) operating at the state-level not included in our model. Given these interpretational issues, this finding merits further investigation with other data sets.
Dentists traditionally focus on child-level factors (i.e., those pertaining to the patient). Our results suggest that family and neighborhood characteristics may play an important role in relation to children’s oral health outcomes. One avenue for further research is to examine cross-level interaction effects, which were beyond the scope of this study. Further research taking a broader perspective on the domains associated with oral health could ultimately contribute to improved dental health outcomes for children.
Limitations
This investigation has several limitations. While these limitations necessarily qualify the conclusions that can be drawn from this study, they can also serve to inform future research on the determinants of children’s oral health. An important limitation follows from the cross-sectional design of the NSCH which precludes causal inferences. Consequently, our findings should be viewed as provisional and subject to verification using other data sources. Development of population-based longitudinal surveys of children’s oral health that permit identification of causal relationships, while expensive and difficult undertakings, should be explored to address this issue. At present, no large-scale longitudinal surveys of children’s oral health exist at the national level. If properly implemented, such surveys could provide a basis for improving our understanding of the determinants of children’s oral health.
Our dependent variable is a subjective measure of parent’s report of the condition of the child’s teeth. Although these reports were not validated using dental exams, evidence from other studies suggests that subjective reports of oral health are reasonably valid indicators for many oral health issues, including root canals, fillings, and prostheses, while the evidence is somewhat mixed for caries (47). More generally, our outcome variable should be viewed as a global health measure that captures parental assessment of multiple aspects of oral health - such as toothaches or swelling, decayed or missing teeth, restorations from past disease, dental esthetics, and functional aspects like chewing ability. It is possible that other sets of explanatory factors would be significant in models predicting different specific oral health problems. The next iteration of the NSCH questionnaire was revised to identify specific oral health problems, such as toothaches, broken teeth, bleeding gums, and decayed teeth or cavities, providing researchers a unique opportunity to assess the factors that may contribute differentially to a variety of important oral health outcomes.
More generally, our study findings are derived from a sample survey, which is subject to various forms of nonrandom error, including nonresponse bias. Survey error is present in any population survey and the NSCH has several methodologies built-in to minimize such biases. These include random selection, assurances of confidentiality for respondents, selecting respondents who were most knowledgeable about the sample child’s health, testing of questionnaire items through focus groups and cognitive interviewing, and incentives to increase response rates.
Finally, although we were able to examine a large number of explanatory factors in our models, there were variables that were identified in our conceptual model (4) for which data were unavailable. Some domains could only be measured by proxy, including family-level social support and child-level health behaviors and practices. Given the potential importance of these factors, we recommend that future survey questionnaires incorporate more direct measures of these variables. Similarly, our indicators of biological and genetic endowment are also indicators of parental health status, and the two domains could not be disentangled without access to more direct measures of biological and genetic endowment, such as indicators of siblings’ or parents’ oral health status. Here again, questionnaire modifications could fruitfully address these issues.
Conclusions
This study is the first empirical investigation of the social determinants of children’s oral health using large-scale, population-based data and multilevel modeling. Although our analysis has many strengths, the limitations suggest important avenues for future research on children’s oral health outcomes. These include using longitudinal data and collecting data on more proximate indicators for some domains, such as genetic endowment. In the meantime, our results can help us to begin identifying characteristics of the child, family and community worthy of further exploration and, ultimately, facilitate the design of interventions to improve oral health. Some variables we found as significant correlates, such as age and ethnicity, are immutable. However, we found a number of significant correlates that are amenable to public health interventions, including access to fluoridated water, family and neighborhood cohesiveness, and positive health behaviors of parents.
Acknowledgements
This study was supported by US DHHS National Institutes of Health/National Institute of Dental and Craniofacial Research grants R03 DE165701 and U54 DE014251.
References
- 1.US Department of Health anD Human Services, Oral Health in America. A Report of the Surgeon General. Rockville, MD: US DHHS, NIDCR, NIH; 2000. [Google Scholar]
- 2.Dye BA, Tan S, Smith V, Lewis BG, Barker LK, Thornton-Evans G, et al. Trends in oral health status: United States, 1988–1994 and 1999–2004. Vital Health Stat. 2007;11:1–92. [PubMed] [Google Scholar]
- 3.Gift HC, Reisine ST, Larach DC. The social impact of dental problems and visits. Am J Public Health. 1992;82:1663–1668. doi: 10.2105/ajph.82.12.1663. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Fisher-Owens SA, Gansky SA, Platt LJ, Weintraub JA, Soobader MJ, Bramlett MD, et al. Influences on children's oral health: a conceptual model. Pediatrics. 2007;120:e510–e520. doi: 10.1542/peds.2006-3084. [DOI] [PubMed] [Google Scholar]
- 5.Ismail AI, Sohn W. The impact of universal access to dental care on disparities in caries experience in children. J Am Dent Assoc. 2001;132:295–303. doi: 10.14219/jada.archive.2001.0172. [DOI] [PubMed] [Google Scholar]
- 6.Mouradian WE, Huebner CE, Ramos-Gomez F, Slavkin HC. Beyond access: the role of family and community in children’s oral health. J Dent Educ. 2007;71:619–631. [PubMed] [Google Scholar]
- 7.Black D, Whitehead M. Inequalities in health: the black report and the health divide. In: Townsend P, Davidson N, Whitehead JA, editors. Inequalities in Health: the Black Report and the Health Divide. London: Penguin Books; 1990. [Google Scholar]
- 8.Cassel J. The contribution of the social environment to host resistance: the Fourth Wade Hampton Frost Lecture. Am J Epidemiol. 1976;104:107–123. doi: 10.1093/oxfordjournals.aje.a112281. [DOI] [PubMed] [Google Scholar]
- 9.Evans RG, Barer ML, Marmor TR. The determinants of health of populations. New York: Aldine de Gruyter; 1994. Why are some people healthy and others not? [Google Scholar]
- 10.Kindig D, Stoddart G. What is population health? Am J Public Health. 2003;93:380–383. doi: 10.2105/ajph.93.3.380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Marmot MG, Wilkinson RG. Social determinants of health. xii. New York: Oxford University Press; 1999. p. 291. [Google Scholar]
- 12.McGinnis MJ, Williams-Russo P, Knickman JR. The case for more active policy attention to health promotion. To succeed, we need leadership that informs and motivates, economic incentives that encourage change, and science that moves the frontiers. Health Aff. 2002;21:78–93. doi: 10.1377/hlthaff.21.2.78. [DOI] [PubMed] [Google Scholar]
- 13.National Academy Press. Committee on evaluation of children’s health, children’s health, the nation’s wealth: assessing and improving child health. Washington, DC: National Academy Press; 2004. [Google Scholar]
- 14.Link B, Phelan J. Social conditions as fundamental causes of disease. J Health Social Behav. 1995;(Special issue):80–94. [PubMed] [Google Scholar]
- 15.Stansfeld S. Social support and social cohesion. In: Marmot M, Wilkinson RG, editors. Social determinants of health. New York: Oxford University Press; 1999. pp. 155–174. [Google Scholar]
- 16.Susser M. Causal thinking in the health sciences; concepts and strategies of epidemiology. xviii. New York: Oxford University Press; 1973. p. 181. [Google Scholar]
- 17.Gift HC, Atchison KA. Oral health, health, and health-related quality of life. Med Care. 1995;33(11 Suppl):NS57–NS77. doi: 10.1097/00005650-199511001-00008. [DOI] [PubMed] [Google Scholar]
- 18.Fejerskov O. Changing paradigms in concepts on dental caries: consequences for oral health care. Caries Res. 2004;38:182–191. doi: 10.1159/000077753. [DOI] [PubMed] [Google Scholar]
- 19.Demers M, Brodeur JM, Simard PL, Mouton C, Veilleux G, Fréchette S. Caries predictors suitable for mass-screenings in children: a literature review. Commun Dental Health. 1990;7:11–21. [PubMed] [Google Scholar]
- 20.Hausen H. Caries prediction – state of the art. Commun Dentistry Oral Epidemiol. 1997;25:87–96. doi: 10.1111/j.1600-0528.1997.tb00904.x. [DOI] [PubMed] [Google Scholar]
- 21.Reisine S, Litt M, Tinanoff N. A biopsychosocial model to predict caries in preschool children. Pediatr Dent. 1994;16:413–418. [PubMed] [Google Scholar]
- 22.Reisine S, Douglass JM. Psychosocial and behaveioral issues in early childhood caries. Commun Dentistry Oral Epidemiol. 1998;26 Suppl 1:32–44. doi: 10.1111/j.1600-0528.1998.tb02092.x. [DOI] [PubMed] [Google Scholar]
- 23.Litt MD, Reisine S, Tinanoff N. Multidimensional causal model of dental caries development in low-income preschool children. Public Health Rep. 1995;110:607–617. [PMC free article] [PubMed] [Google Scholar]
- 24.Thomson WM, Poulton R, Milne BJ, Caspi A, Broughton JR, Ayers KM. Socioeconomic inequalities in oral health in childhood and adulthood in a birth cohort. Commun Dentistry Oral Epidemiol. 2004;32:345–353. doi: 10.1111/j.1600-0528.2004.00173.x. [DOI] [PubMed] [Google Scholar]
- 25.Grembowski D, Andersen RM, Chen M. A public health model of the dental care process. Med Care Rev. 1989;46:439–496. doi: 10.1177/107755878904600405. [DOI] [PubMed] [Google Scholar]
- 26.Strippel H. Sociodental indicators in children and adolescents. Gesundheitswesen. 2001;63:93–97. doi: 10.1055/s-2001-10959. [DOI] [PubMed] [Google Scholar]
- 27.Susser M, Susser E. Choosing a future for epidemiology: II. From black box to Chinese boxes and eco-epidemiology. Am J Public Health. 1996;86:674–677. doi: 10.2105/ajph.86.5.674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Kaplan GA. Searching for simplicity in a complex world (Presidential Address). Society of Epidemiologic Research 37th Annual Meeting; Salt Lake City, UT: 2004. [Google Scholar]
- 29.Diez-Roux A. Multilevel analysis in public health research. Ann Rev Public Health. 2000;21:171–192. doi: 10.1146/annurev.publhealth.21.1.171. [DOI] [PubMed] [Google Scholar]
- 30.National Committee on Vital and Health Statistics. Shaping a Health Statistics Vision for the 21st Century. Washington, DC: National Center for Health Statistics; Department of Health and Human Services Data Council, Centers for Disease Control and Prevention. 2002
- 31.Newacheck PW, Rising JP, Kim SE. Children at risk for special health care needs. Pediatrics. 2006;118:334–342. doi: 10.1542/peds.2005-2238. [DOI] [PubMed] [Google Scholar]
- 32.Patrick D, Lee RS, Nucci M, Grembowski D, Jolles CZ, Milgrom P. Reducing oral health disparities: a focus on social and cultural determinants. BMC Oral Health. 2006;6 Suppl 1:S4. doi: 10.1186/1472-6831-6-S1-S4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Gansky SA, Cheng N, Pollick HF. Predicting early childhood caries with individual, family and neighborhood factors. J Dent Res. 2005;84(Spec Iss A) #0012. [Google Scholar]
- 34.Tellez M, Sohn W, Burt BA, Ismail AI. Assessment of the relationship between neighborhood characteristics and dental caries severity among low-income African-Americans: a multilevel approach. J Public Health Dent. 2006;66:30–36. doi: 10.1111/j.1752-7325.2006.tb02548.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Griffin SO, Jones K, Tomar SL. An economic evaluation of community water fluoridation. J Public Health Dent. 2001;61:78–86. doi: 10.1111/j.1752-7325.2001.tb03370.x. [DOI] [PubMed] [Google Scholar]
- 36.Weintraub JA, Stearns SC, Rozier RG, Huang CC. Treatment outcomes and costs of dental sealants among children enrolled in Medicaid. Am J Public Health. 2001;91:1877–1881. doi: 10.2105/ajph.91.11.1877. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Marinho VC, Higgins JP, Sheiham A, Logan S. Fluoride toothpastes for preventing dental caries in children and adolescents. Cochrane Database Syst Rev. 2003 doi: 10.1002/14651858.CD002278. CD002278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.CDC–NOHSS. CDC Water Fluoridation Reporting System (WFRS) National Oral Health Surveillance System: Fluoridation Status; [cited 2006];2004 July 1; Available from: http://www2.cdc.gov/nohss/FluoridationV.asp.
- 39.Blumberg SJ, Olson L, Frankel MR, Osborn L, Srinath KP, Giambo P. Design and operation of the National Survey of Children’s Health, 2003. Vital Health Stat. 2005;1:131. [PubMed] [Google Scholar]
- 40.Raghunathan TE, Lepkowski JM, Van Hoewyk J, Solenberger P. A multivariate technique for multiply imputing missing values using a sequence of regression models. Surv Methodol. 2001;27:85–95. [Google Scholar]
- 41.Rubin DB. Appl Probab Stat. xxix. New York: Wiley; 1987. Multiple imputation for nonresponse in surveys. Wiley series in probability and mathematical statistics; p. 258. [Google Scholar]
- 42.Yuan YC. Multiple imputation for missing values: concepts and new development. 2000; SUGI Proceedings; Cary, NC: SAS Institute Inc.; [last accessed 2 July 2009]. Available at: http://support.sas.com/rnd/app/papers/multipleimputation.pdf. [Google Scholar]
- 43.Särndal CE, Swenson B, Wretman J. Model assisted survey sampling. New York: Springer-Verlag; 1992. [Google Scholar]
- 44.Korn EL, Graubard BI. Epidemiologic studies utilizing surveys: accounting for the sampling design. Am J Public Health. 1991;81:1166–1173. doi: 10.2105/ajph.81.9.1166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Korn EL, Graubard BI. Examples of differing weighted and unweighted estimates from a sample survey. Am Sta. 1995;49:291–295. [Google Scholar]
- 46.Allison P. Logistic regression using the SAS system: theory and application. Cary, NC: SAS Institute; 1999. [Google Scholar]
- 47.Pitiphat W, Garcia RI, Douglass CW, Joshipura KJ. Validation of self-reported oral health measures. J Public Health Dent. 2002;62:122–128. doi: 10.1111/j.1752-7325.2002.tb03432.x. [DOI] [PubMed] [Google Scholar]