Abstract
Objective
In diagnosing symptomatic meniscal tear, clinicians often query patients with a “checklist” of symptoms such as “popping” or “catching.” There has been little research on the reliability or diagnostic value of these terms.
Methods
We developed questions to elicit the presence of 11 “checklist” symptoms associated with meniscal tear and administered a survey with both “checklist” and expanded descriptions to study subjects. We examined reliability of checklist and expanded versions of each item. Validity was evaluated in relation to the clinical diagnosis of symptomatic meniscal tear, which consisted of the clinical impression of the treating orthopedic surgeon based upon physical exam, history and MRI. We developed a Meniscal Symptom Index, calculated as the sum of those expanded descriptive items that were independently associated with symptomatic meniscal tear in multivariate logistic regression.
Results
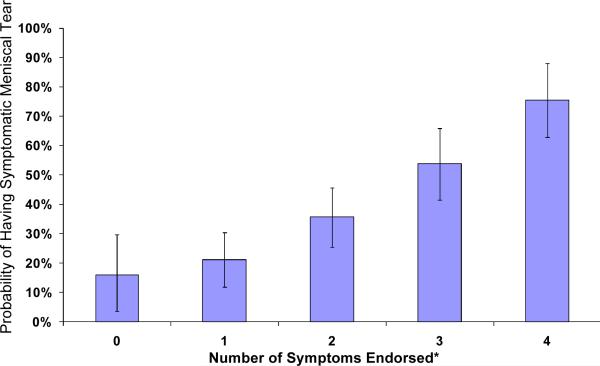
300 individuals (mean age 52 ± 12 years, 66% female) completed the survey. 121 had symptomatic meniscal tear. Test-retest reliability was higher for expanded descriptions than for checklist items. The Meniscal Symptom Index consisted of 4 expanded items: localized pain, clicking, catching, and giving way. Among subjects with none of these symptoms, 16% (95% CI 2 – 30%) had symptomatic meniscal tear, whereas among those with all 4 symptoms, 76% (95% CI 63 – 88%) had symptomatic meniscal tear (p-value for trend = 0.0001).
Conclusion
Clinicians should use expanded symptom definitions when querying patients about meniscal symptoms. A newly-developed Meniscal Symptom Index holds promise as a diagnostic tool and merits further validation.
INTRODUCTION
Meniscal tears are among the most common knee disorders in the US.1 While often asymptomatic,2 meniscal tears can cause considerable disability and pain, prompting substantial resource utilization. In fact, arthroscopic partial meniscectomy (APM) is the most commonly performed orthopedic operation, carried out on one million patients annually in the US.3 Meniscal tears are also risk factors for subsequent development and progression of knee osteoarthritis (OA).4–6
The diagnosis of meniscal tear involves an integration of information from the clinical history, physical examination and ancillary tests. Magnetic resonance imaging (MRI) is also frequently used to visualize meniscal tears. However, as many as one third of asymptomatic adults age 50 and over have a meniscal tear on MRI; this prevalence rises to 51% for those over 70 years. Therefore, imaging alone cannot be used to diagnose symptomatic meniscal tear.2
Thus, the clinical history remains a cornerstone of the diagnosis of symptomatic meniscal tear. Clinicians have traditionally queried symptoms using a checklist of single words or short phrases, such as “clicking” or “giving way” to assess whether the patient's symptoms arise from an intraarticular mechanical lesion (Table 1). Despite the widespread use of these terms, little is known about their reproducibility or the ability of checklist items to distinguish meniscal tears from other disorders such as knee OA. In fact, because symptoms of meniscal tear are often superimposed upon those from knee OA, the identification of meniscal tear is particularly difficult in patients with concomitant OA. Nonetheless, a history of these meniscal symptoms is typically a critical factor in the decision of whether to proceed with APM. Further research on the reliability and validity of strategies for eliciting meniscal symptoms is warranted.
Table 1.
Meniscal symptoms as checklist and expanded descriptions
| Checklist | Expanded Description |
|---|---|
| Clicking | Do you feel a clicking sensation or hear a clicking noise when you move your knee? |
| Catching | Do you feel that sometimes something is caught in your knee that momentarily prevents movement? |
| Giving way | Do you sometimes feel that your knee will give out and not support your weight? |
| Localized pain | Is your knee pain centered to 1 spot on the knee that you can point to with your finger? |
| Episodic pain | Do you have pain that comes and goes with specific movements and activities? |
| Pain with activity | Do you experience pain that is caused by specific activities? |
| Episodic swelling | Do you have swelling in your knee that comes and goes with specific activities? |
| Popping | Do you hear or feel a pop in your knee during movements? |
| Pain with pivoting/twisting | Do you feel pain when you pivot or twist your knee? |
| Change in quality/pattern of pain | Have you had a change in type, location, or frequency of your pain? |
| Locking | Do you feel that your knee sometimes gets stuck temporarily so that you can't move it further? |
The Meniscal Symptom Index is comprised of the first 4 expanded descriptions. Endorsed items are added, without weighting, to yield an index with possible range from 0 to 4.
In this paper, we present the development of expanded descriptions of the checklist of meniscal symptoms. These more fully articulated questions are intended to be easier for patients to understand than the more cryptic symptom checklist. We assess agreement between expanded descriptions and checklist versions of the same symptoms. We then examine the ability of checklist items and expanded symptom descriptions to distinguish patients with symptomatic meniscal tear from those with other sources of knee pain. Finally, we combine those items that best distinguish symptomatic meniscal tear from other diagnoses into a Meniscal Symptom Index, and we assess the diagnostic utility of the Index among patients with knee symptoms.
PATIENTS AND METHODS
Development of Expanded Standardized Definitions
We asked a convenience sample of orthopedic surgeons, non-orthopedic physicians and physical therapists to describe how they elicit typical meniscal symptom terms (e.g. catching, locking, etc.) from patients. Their input was synthesized into a set of provisional descriptions that we sent to a larger group of clinicians for further comments. The expanded definitions next underwent pilot testing, in which we asked 10 patients to improve the wording. In this fashion, we generated 11 expanded descriptions of meniscal symptoms (Table 1).
Field Testing
Sample Recruitment
We conducted the study in the outpatient clinics of two orthopedic surgeons at Brigham and Women's Hospital, an academic medical center in Boston, MA. These surgeons each see a wide range of knee and other problems and manage patients operatively and non-operatively. Patients who were at least 18 years of age, who could speak English and who did not have prior surgery on their index knee were eligible.
The research coordinator invited eligible patients in the waiting room to participate in the study. Patients who agreed signed a consent letter before filling out the survey. Data collection took place between December 2008 and June 2009.
Data sources and data elements
Survey Instrument
The survey instrument included demographic information, the checklist of one- or several-word descriptions of 11 meniscal symptoms and expanded descriptions of these 11 meniscal symptoms. We varied the ordering of terms in the checklist and the expanded descriptions to reduce the likelihood that patients would match their responses.
For the last 100 patients in the study, we reversed the order of the two diagnostic methods so that the questionnaire presented the expanded symptoms before the checklist. There were no meaningful differences in reliability or validity between the first 200 and the last 100 subjects.
Medical Record Review Form
Research coordinators, blinded to patient survey data, used standardized, explicit abstraction criteria to review the electronic medical records of all subjects to elicit patients' diagnoses. The diagnostic impression of the surgeon, made in the course of routine practice by integrating information from physical exam, imaging studies and clinical history, was recorded with a closed form item that listed frequent diagnoses including knee OA, meniscal tear, patellofemoral syndrome and ligamentous injuries. Each diagnosis was categorized as “definite,” “probable,” “possible,” or “unlikely.” For symptomatic meniscal tear, a classification of “definite” required both MRI documentation of a tear and a positive surgeon's diagnostic impression of meniscal tear. For imaging done at the study center, we confirmed presence of meniscal tear by MRI report. When studies were done at an outside institution (11% of MRIs), we used the impression of the surgeon as documented in the visit note. In both scenarios (radiologist readings and surgeon readings) the radiologist and the surgeon required the lesion to extend to the meniscal surface to qualify as a tear. We assigned the classification of “probable” or “possible” symptomatic meniscal tear if the surgeon's diagnostic impression was symptomatic meniscal tear but MRI was not available at the visit. Patients in the “unlikely” category either had an MRI negative for meniscal tear or were categorized by surgeons as having low probability for meniscal tear. Surgeons made the determination of knee OA based upon symptoms and plain radiographs.
To confirm the accuracy of the surgeons' diagnostic impressions, we compared the diagnoses against criteria established for the classification of knee OA by the American College of Rheumatology.31 Specifically, we took a random sample of 20 patients who the surgeons diagnosed with knee OA and another 20 for whom the diagnostic impression for knee OA was negative. We reviewed the medical records of these 40 patients to determine whether their diagnoses satisfied the ACR classification criteria for knee OA.
Analysis
Reliability
We assessed test-retest reliability of the expanded and checklist items by re-surveying 30 patients one week after their clinic appointment (via mailing the survey to their home). Reliability was assessed at the item level with the Kappa statistic7 and at the index level via the Spearman correlation coefficient9 and paired t-test.
Agreement
Agreement between checklist and standardized descriptions was assessed for each of the 11 symptoms. We calculated the sensitivity, specificity and overall accuracy8 ((number of true positives + number of true negatives)/total number of respondents) of each of the checklist items, with the expanded items serving as the criterion standard. We also examined agreement with the Kappa statistic.10
Validity
We assessed discriminant validity11 at the item level for the checklist and standardized descriptions based on diagnoses ascertained from medical record reviews. We used standardized procedures to divide patients into two groups: symptomatic meniscal tear and no meniscal tear. Patients with symptomatic meniscal tear consisted of the following sub-groups: patients classified as “definite” in medical record review as described above; patients classified as “probable” who never obtained an MRI, and patients classified as “probable,” “possible” or “unlikely” who obtained an MRI that documented a meniscal tear after their appointment date (Electronic appendix, Table 1). Because meniscal tears may be asymptomatic, we performed a sensitivity analysis that categorized patients with MRI showing meniscal tear but whose diagnostic impression of meniscal tear was “unlikely” as not having symptomatic meniscal tear. No meaningful differences in sensitivity, specificity and likelihood ratios of symptoms were found when these patients were re-classified.
Patients without symptomatic meniscal tear were further stratified into two sub-groups: primary diagnosis of knee OA and/or patellofemoral syndrome; and primary diagnosis of ligamentous injuries and/or knee sprain. We recognize that mechanical symptoms may reflect anatomic abnormalities in the knee arising from internal derangements. We anticipated that ligamentous injury (e.g. ACL, PCL) would also be associated with these symptoms. Thus, we excluded patients with diagnoses of ligamentous injuries and/or knee sprain from our principal analyses of item level discriminant validity in order to focus on the most clinically cogent distinction – between meniscal tear and other chronic conditions (generally OA and patellofemoral syndrome). Using the responses to the expanded descriptions, we calculated sensitivity, specificity and likelihood ratios (sensitivity / 1 – specificity)12 to ascertain which individual symptoms best discriminated patients with symptomatic meniscal tear from patients with a primary diagnosis of OA and/or patellofemoral syndrome.
Development and preliminary validation of the Meniscal Symptom Index
We entered into a logistic regression model those items that distinguished (with likelihood ratio > 1.25) symptomatic meniscal tear from OA and/or patellofemoral syndrome. Symptomatic meniscal tear served as the dependent variable. Those independent variables with p-values < 0.05 and/or odds ratios > 1.5 in the logistic regression model were included in the final index. The index was calculated as the unweighted sum of these items. For each possible index score, we calculated the proportion of patients with that score who had a symptomatic meniscal tear.
Sensitivity Analysis
We performed three additional sensitivity analyses. First, we evaluated how concomitant meniscal tear and knee OA and/or patellofemoral syndrome affected the prevalence of symptoms. For this analysis, we compared the average number of symptoms endorsed between patients with meniscal tear and OA and/or patellofemoral syndrome versus patients with meniscal tear who did not have these conditions.
Our second sensitivity analysis evaluated whether meniscal symptoms were specific for meniscal tear or rather accompanied knee derangements in general. For this analysis, we included a third group of patients with ligamentous injury and compared the average number of symptoms endorsed among this group, the meniscal tear group, and the OA and/or patellofemoral syndrome group.
A third sensitivity analysis evaluated whether meniscal tears present differently in the setting of knee OA. For this analysis, we divided all patients into having or not having knee OA and calculated the likelihood ratios for all 11 symptoms in the expanded form.
All study activities were approved by the Brigham and Women's Hospital IRB.
RESULTS
Study sample
346 patients were identified during preliminary screening of electronic records as potentially eligible for the study. Of these patients, 23 had prior surgery on the index knee, 6 did not present with knee pain and 1 could not understand English, resulting in 316 eligible individuals. 300 patients (95%) agreed to participate in the study and completed the survey. Their demographic features are summarized in Table 2. Based on medical record reviews, 121 patients met the case definition of symptomatic meniscal tear and 28 (23%) went on to receive APM. The 121 patients included 108 with tear documented on MRI and 13 classified by their surgeons as “probable” for having a tear without MRI. Of the 179 without symptomatic meniscal tear, 146 had either OA or patellofemoral syndrome and 33 had various ligamentous injuries. Of the 20 patients diagnosed with knee OA, 20 (100%) had radiographic evidence of OA and 18 (90%) satisfied the ACR criteria for the diagnosis of knee OA. Of the 20 patients who were not diagnosed with knee OA, none had radiographic evidence of OA and 17 (85%) met the ACR criteria for diagnosis of knee OA.
Table 2.
Demographics of study participants
| Variable | Mean (St Dev) |
|---|---|
| Age | 52.3 (12.4) |
| Category | Count (%) | |
|---|---|---|
| Sex | Female | 200 (66.6) |
| Male | 100 (33.3) | |
| Race | White | 217 (72.3) |
| Black | 48 (16.0) | |
| Hispanic | 23 (7.7) | |
| Asian | 6 (2.0) | |
| Other | 2 (1.0) | |
| No response | 4 (1.0) | |
| Education | Did not graduate from high school | 10 (3.3) |
| Graduated from high school; no further education | 38 (12.7) | |
| Attended technical college, professional school or college, but did not graduate | 40 (13.3) | |
| Graduated from technical college or professional school | 31 (10.3) | |
| Graduated from college | 169 (56.3) | |
| No response | 12 (4.0) | |
| Knee | Right | 124 (41.3) |
| Left | 129 (43.0) | |
| Both | 46 (15.3) | |
| No response | 1 (0.0) | |
| Diagnosis | Meniscal Tear | 121 (40.3) |
| Osteoarthritis (OA) | 146 (48.7) | |
| Ligamentous injuries | 33 (11.0) |
Sixty-eight participants were sent the test-retest questionnaire and 30 (44%) returned it. The age, gender, race, and diagnosis of the test-retest responders did not substantially differ from those of the non-responders nor those who were not mailed the test-retest questionnaire.
Reliability
Test-retest reliability showed item-level Kappas in the range of 0 to 0.75 (median across all items = 0.55) for the checklist and 0.52 to 1.00 (median = 0.77) for the expanded descriptions (Table 3). The overall recall accuracies ranged from 0.62 to 0.97 (median = 0.85) for the checklist and 0.83 – 1.00 (median = 0.90) for the expanded terms. Kappa values for all symptoms, except pain with pivoting/twisting, were higher with expanded descriptions than checklist items. Overall accuracies for eight of eleven symptoms were also higher for expanded descriptions.
Table 3.
Test-Retest reliability of meniscal symptoms
| Kappa Value | Overall Accuracy | |||
|---|---|---|---|---|
| Symptom | Checklist (95% CI) | Expanded (95% CI) | Checklist (95% CI) | Expanded (95% CI) |
| Clicking | 0.66 (0.40–0.93) | 0.80 (0.58–1.00) | 0.83 (0.66–0.93) | 0.90 (0.74–0.97) |
| Giving way | 0.68 (0.40–0.97) | 0.80 (0.58–1.00) | 0.85 (0.66–0.94) | 0.90 (0.74–0.97) |
| Episodic pain | −0.06 (−0.16–0.04) | 1.00 (1.00–1.00) | 0.82 (0.64–0.92) | 1.00 (0.89–1.00) |
| Catching | 0.53 (0.20–0.85) | 0.65 (0.37–0.93) | 0.78 (0.59–0.89) | 0.83 (0.64–0.93) |
| Pain with activity | 0.00 (0.00–0.00) | 0.63 (0.17–1.00) | 0.97 (0.83–0.99) | 0.93 (0.77–0.98) |
| Episodic swelling | 0.75 (0.49–1.00) | 0.70 (0.43–0.97) | 0.90 (0.74–0.97) | 0.87 (0.70–0.95) |
| Popping | 0.55 (0.24–0.86) | 0.86 (0.67–1.00) | 0.78 (0.59–0.89) | 0.93 (0.78–0.98) |
| Pain with pivoting/twisting | 0.52 (0.12–0.93) | 0.52 (0.12–0.93) | 0.87 (0.70–0.95) | 0.87 (0.70–0.95) |
| Localized pain | 0.63 (0.17–1.00) | 0.84 (0.63–1.00) | 0.93 (0.78–0.98) | 0.93 (0.79–0.98) |
| Change in quality/pattern of pain | 0.19 (−0.12–0.51) | 0.78 (0.55–1.00) | 0.62 (0.44–0.77) | 0.90 (0.74–0.96) |
| Locking | 0.60 (0.29–0.91) | 0.77 (0.52–1.00) | 0.82 (0.66–0.92) | 0.90 (0.74–0.97) |
Agreement between checklist and expanded versions of symptom items
The data in Table 4 document considerable variation in sensitivity and specificity of checklist items, as compared with expanded versions of the same items. For example, checklist versions of catching,” and “change in quality/pattern of pain” had sensitivities <0.70, meaning that > 30% of patients who reported the symptom on the expanded version did not endorse it in the checklist. On the other hand, the specificities the checklist versions of “pain with activity,” “localized pain,” and “locking” were < 0.70, meaning that at least 30% of patients who did not report the symptom on the expanded version did endorse it on the checklist. Because few symptoms were both sensitive and specific, overall agreement between the two versions of most symptoms was modest (median overall agreement across all items = 0.79, range 0.65 to 0.95,). The Kappa values (Table 4) also indicate considerable disagreement between checklist and expanded versions of some items. For example, the Kappa values for localized pain and clicking were 0.17 and 0.82, respectively.
Table 4.
Measures of agreement between meniscal symptoms expressed as checklist and expanded descriptions
| Symptom | Sensitivity (95% CI) | Specificity (95% CI) | Overall Accuracy (95% CI) | Kappa Value (95% CI) |
|---|---|---|---|---|
| Clicking | 0.90 (0.84–0.94) | 0.93 (0.87–0.96) | 0.91 (0.87–0.94) | 0.82 (0.76–0.89) |
| Giving way | 0.73 (0.65–0.80) | 0.82 (0.75–0.88) | 0.77 (0.72–0.81) | 0.54 (0.44–0.63) |
| Episodic pain | 0.80 (0.75–0.85) | 0.70 (0.48–0.86) | 0.79 (0.74–0.84) | 0.24 (0.12–0.37) |
| Catching | 0.55 (0.46–0.64) | 0.85 (0.79–0.90) | 0.74 (0.68–0.78) | 0.42 (0.30–0.52) |
| Pain with activity | 0.98 (0.95–0.99) | 0.28 (0.17–0.44) | 0.88 (0.84–0.92) | 0.34 (0.17–0.50) |
| Episodic swelling | 0.91 (0.86–0.95) | 0.82 (0.73–0.88) | 0.88 (0.83–0.91) | 0.74 (0.65–0.82) |
| Popping | 0.86 (0.78–0.91) | 0.91 (0.86–0.95) | 0.89 (0.85–0.92) | 0.78 (0.70–0.85) |
| Pain with pivoting/twisting | 0.97 (0.94–0.99) | 0.83 (0.71–0.91) | 0.95 (0.91–0.97) | 0.82 (0.73–0.90) |
| Localized pain | 0.90 (0.85–0.94) | 0.25 (0.18–0.34) | 0.65 (0.59–0.70) | 0.17 (0.07–0.27) |
| Change in quality/pattern of pain | 0.83 (0.76–0.88) | 0.49 (0.41–0.57) | 0.67 (0.62–0.72) | 0.33 (0.22–0.43) |
| Locking | 0.61 (0.51–0.70) | 0.87 (0.82–0.91) | 0.78 (0.73–0.82) | 0.50 (0.39–0.60) |
Sensitivity and specificity calculated using the expanded descriptions as the criterion standard.
Validity
We examined the capacity of the checklist items and the expanded items to distinguish symptomatic meniscal tear from a primary diagnosis of OA and/or patellofemoral syndrome. Table 5 shows the sensitivity, specificity and likelihood ratios of each of the terms based on symptomatic meniscal tear diagnosis ascertained from medical record reviews. The likelihood ratios of all 11 symptoms were higher when expressed as an expanded description than as a checklist item.
Table 5.
Discriminant validity of meniscal symptoms based on medical record review
| Symptom | Sensitivity | Specificity | Likelihood Ratio | |||
|---|---|---|---|---|---|---|
| Checklist (95% CI) | Expanded Description (95% CI) | Checklist (95% CI) | Expanded Description (95% CI) | Checklist (95% CI) | Expanded Description (95% CI) | |
| Clicking | 0.61 (0.52–0.70) | 0.65 (0.56–0.73) | 0.52 (0.45–0.59) | 0.50 (0.43–0.58) | 1.28 (1.04–1.58) | 1.31 (1.08–1.60) |
| Giving way | 0.47 (0.39–0.56) | 0.69 (0.60–0.77) | 0.51 (0.43–0.58) | 0.53 (0.45–0.60) | 0.96 (0.75–1.22) | 1.46 (1.20–1.77) |
| Episodic pain | 0.80 (0.72–0.86) | 0.98 (0.93–0.99) | 0.26 (0.20–0.33) | 0.11 (0.07–0.16) | 1.08 (0.95–1.22) | 1.09 (1.03–1.16) |
| Catching | 0.29 (0.22–0.38) | 0.59 (0.50–0.67) | 0.69 (0.61–0.75) | 0.75 (0.68–0.80) | 0.94 (0.65–1.35) | 2.31 (1.72–3.01) |
| Pain with activity | 0.97 (0.92–0.99) | 0.89 (0.82–0.94) | 0.07 (0.04–0.12) | 0.16 (0.11–0.22) | 1.04 (0.99–1.10) | 1.06 (0.97–1.16) |
| Episodic swelling | 0.68 (0.59 – 0.75) | 0.71 (0.62–0.78) | 0.38 (0.31–0.45) | 0.42 (0.35–0.49) | 1.09 (0.92–1.29) | 1.22 (1.03–1.45) |
| Popping | 0.44 (0.36–0.53) | 0.49 (0.40–0.58) | 0.61 (0.53–0.68) | 0.63 (0.58–0.71) | 1.14 (0.86–1.50) | 1.33 (1.07–1.83) |
| Pain with pivoting/twisting | 0.84 (0.76–0.90) | 0.87 (0.79–0.92) | 0.20 (0.15–0.26) | 0.21 (0.16–0.28) | 1.05 (0.94–1.17) | 1.10 (0.99–1.22) |
| Localized pain | 0.89 (0.82–0.93) | 0.74 (0.65–0.81) | 0.18 (0.13–0.25) | 0.49 (0.31–0.56) | 1.09 (0.99–1.20) | 1.43 (1.20–1.71) |
| Change in quality/pattern of pain | 0.68 (0.59–0.76) | 0.55 (0.46–0.63) | 0.32 (0.26–0.39) | 0.50 (0.43–0.57) | 1.00 (0.86–1.18) | 1.09 (0.88–1.36) |
| Locking | 0.33 (0.25–0.42) | 0.47 (0.38–0.56) | 0.73 (0.66–0.79) | 0.74 (0.67–0.80) | 1.23 (0.87–1.74) | 1.78 (1.31–2.43) |
Sensitivity and specificity calculated using the physician's impression, supported by MRI, as the criterion standard (see text and Electronic Index, Table 1).
Development and preliminary validation of the Meniscal Symptom Index
To develop the Meniscal Symptom Index we took all symptoms with likelihood ratios > 1.25 on bivariate analyses and entered them into a logistic regression analysis with meniscal tear as the dependent variable. The model adjusted for age and sex. None of the checklist items met these criteria. The expanded descriptions of “clicking,” “localized pain,” “giving way,” and “catching” had p-values < 0.05 and/or odds ratios > 1.5 in the logistic regression model. These four expanded items were included in the Meniscal Symptom Index. Patients were assigned a score between 0 (none of these four expanded symptoms present) to 4 (all 4 present).
We examined the test-retest reliability of the Meniscal Symptom Index. At the item level, the Kappa values were 0.65 for catching, 0.80 for clicking, 0.80 for giving way and 0.84 for localized pain. At the index level, the Spearman coefficient assessing correlation between the two administration times was 0.80. The mean scores at time 1 and time 2 were 2.10 (sd = 1.21) and 2.07 (sd = 1.20), respectively (p-value for paired t-test = 0.8).
To evaluate the validity of the Meniscal Symptom Index, we examined the association between Meniscal Symptom Index score and diagnosis of symptomatic meniscal tear (Figure 1). The probability of having a meniscal tear increased from 16% (95% CI 2 – 30%) for patients with an index score of 0 to 76% (95% CI 63 – 88%) for those with an index score of 4 (p value for trend = 0.0001).
Figure 1. Probability of having symptomatic meniscal tear given number of symptoms endorsed in meniscal symptom index.
The bars show the percent of patients with symptomatic meniscal tear, stratified by the number of symptoms endorsed in the meniscal symptom index. This index is comprised of the following four symptoms, expressed as expanded descriptions: clicking (Do you feel a clicking sensation or hear a clicking noise when you move your knee?), catching (Do you feel that sometimes something is caught in your knee that momentarily prevents movement?), giving way (Do you sometimes feel that your knee will give out and not support your weight?) and localized pain (Is your knee pain centered to 1 spot on the knee that you can point to with your finger?). Endorsed items are added, without weighting, to yield an index with possible range from 0 to 4. The error bars represent the 95% confidence intervals.
*symptoms included: clicking, catching, giving way and localized pain
Sensitivity Analyses
In our sample, 69 of 121 patients with meniscal tear had co-existent OA and/or patellofemoral syndrome. These patients endorsed a mean of 2.93 out of the 4 symptoms in our meniscal symptom index. Those without OA and/or patellofemoral syndrome endorsed a mean of 2.27 out of 4 symptoms.
Patients with a primary diagnosis of ligamentous injury endorsed a mean of 1.94 symptoms, falling between those with meniscal tear (mean = 2.64) and those with a primary diagnosis of OA and/or patellofemoral syndrome (mean = 1.69).
All 11 symptoms in the expanded form, except for change in quality/pattern of pain and pain with activity had higher likelihood ratios for patients with OA than for those without OA.
DISCUSSION
We developed a set of expanded descriptions for 11 symptoms in the commonly used meniscal symptom “checklist.” The checklist and expanded items were administered to patients seeing orthopedic surgeons for knee pain. Test-retest reliability was higher for expanded descriptions than for the corresponding checklist version of each item and the expanded descriptions better discriminated patients with symptomatic meniscal tear from those with other disorders. We created a Meniscal Symptom Index that included items associated with symptomatic meniscal tear with likelihood ratios > 1.25. The index comprised the symptoms “clicking,” “catching,” “giving way,” and “localized pain,” expressed as expanded descriptions. We provide preliminary validation of the Meniscal Symptom Index.
To the best of our knowledge, this is the first study to examine the validity and reliability of the clinical history relevant to meniscal tear. Prior studies on the diagnosis of meniscal tear have focused on physical exam13–18 or MRI.14, 17–21 These studies suggest that no single test can definitively diagnose symptomatic meniscal tear.
Our study extends this concept to the clinical history. We have shown that asking patients about symptoms in expanded form is more informative than querying the same symptoms via checklist. Yet our results also demonstrate that physicians should not rely on clinical history alone to diagnose meniscal tear. The Meniscal Symptom Index stratified a population with an overall prevalence of symptomatic meniscal tear of 40% into a low risk group with 16% prevalence of symptomatic meniscal tear and a high risk group with 76% prevalence. These risks are neither low enough in the low risk group nor high enough in the high risk group for the index to be considered an adequate stand-alone test. However, if the Meniscal Symptom Index is validated in other populations, physicians may consider using it to refine their estimate of the likelihood of symptomatic meniscal tear.
Several findings from our study deserve emphasis. First, the level of agreement between patients' responses in the checklist and the questionnaire is strikingly low for certain symptoms. This finding shows that patients and clinicians do not share the same understanding of certain commonly used terms. Since a patient's symptoms are regarded as critical factors in the decision of whether to order an MRI, and ultimately, whether to proceed with APM, this finding is particularly concerning. The broader implication is that physicians and patients must understand each other to collaborate effectively in decision making.
Second, Kappa values for several terms in the checklist and expanded descriptions were low, despite high overall accuracy. For example, in test-retest analyses, the symptoms “pain with activity” and “pain with pivoting/twisting” had Kappa values ≤ 0.65 and overall accuracies ≥ 0.85 in both the checklist and expanded format. The phenomenon of high agreement but low Kappa is well recognized25, 26 and occurs most often when chance agreement is high and a symptom is especially common or rare. Thus, our Kappa values must be interpreted cautiously.
It is noteworthy that none of the checklist items and just 6 of the 11 expanded descriptions had likelihood ratios >1.25 based on diagnoses obtained from medical records. This finding demonstrates that certain pieces of the history that have been used traditionally to identify meniscal tear may not be informative. The history used to elicit meniscal symptoms should focus on the few discriminating items.
One strength of this study is that both the surgeon who assigned the diagnosis and the research associate who abstracted the diagnoses were blinded to the patient's response to the questionnaire. The fact that these three streams of information were completely independent eliminates the possibility of observer bias.
The generalizability of study results may be limited because all patients were recruited at a single academic center by two orthopedic surgeons. Thus, our cohort of patients may not be representative of the population of individuals with knee disorders. Further, it is conceivable that the surgeons in our study differed in the criteria and thresholds they used to arrive at diagnostic impressions. However, our medical record review revealed a high level of agreement between the diagnostic impression for knee OA and ACR criteria for the classification of knee OA, suggesting that the diagnoses of the surgeons are valid. In addition, the study design creates the risk of incorporation bias in which the test items are incorporated into the diagnosis. However, the goal of our analysis is to deconstruct the diagnostic impression of an expert clinician and specifically to determine whether individual items of the history have independent diagnostic value when presented to patients in the form of a questionnaire. It is also conceivable that the diagnoses assigned by surgeons were conflated by patients' surgical candidacy. However, the low proportion of patients diagnosed with meniscal tear who went on to receive APM (23%) suggests it is unlikely that the diagnosis of meniscal tear was influenced by the eventual decision to operate.
We found that the number of symptoms in the meniscal symptom checklist endorsed by patients with a primary diagnosis of ligamentous injury fell between those with a primary diagnosis of meniscal tear and OA and/or patellofemoral syndrome, suggesting that some of the symptoms may not be specific for meniscal tear but rather may accompany internal derangements in general. However, our group of patients with ligamentous injury was small.
All 11 symptoms except for change in quality/pattern of pain and pain with activity had higher likelihood ratios for the group of patients with OA. This suggests that having OA does not compromise the performance of most symptoms, including all four of the meniscal symptom checklist. The discrepancy in likelihood ratios for the groups with and without knee OA also suggests that meniscal tears may present differently in the setting of knee OA. Our study represents a beginning research step in differentiating between symptoms caused by the two conditions.
The ideal gold standard for clinical syndromes, such as meniscal tear, is elusive. Our use of the clinician's overall impression augments specificity by avoiding the notorious problem of false positive imaging studies. This approach is consistent with other diagnostic testing studies in clinical syndromes. For example, the classification criteria for systemic lupus erythematosus (SLE),27 rheumatoid arthritis,28 and lumbar spinal stenosis,29 among other conditions, were validated against expert clinical opinion. Thus, for conditions in which no universally accepted gold standard exists, the impression of expert clinicians has been used as a method of establishing a clinical diagnosis, and diagnostic tests for these conditions were validated against this expert opinion.30 We used a similar strategy to assess the validity and reliability of the Meniscal Symptom Index.
Our study provides preliminary evidence of discriminant validity of a newly developed Meniscal Symptom Index, an aggregation of four symptoms (clicking, giving way, catching and localized pain) expressed as expanded descriptions. Although further validation is needed, we suggest that clinicians consider using this index of expanded clinical history items, rather than the traditional “checklist” of short-term symptoms, when eliciting clinical history relevant to symptomatic meniscal tear. On a more general level, our study demonstrates that the way physicians ask questions is important and that time-honored features of the clinical history methods deserve critical scrutiny.
Acknowledgments
Supported by: NIH R01 AR 055557, P60 AR 47782, R01 AR053112, K24 AR 02123 (Dr. Katz), 1K24AR057827 (Dr. Losina), and an Innovative Research Grant from the Arthritis Foundation (Dr. Losina)
Electronic Appendix
Table 1.
Case definition of meniscal tear
| MRI results | |||
|---|---|---|---|
| Positive for meniscal tear | Negative for meniscal tear | MRI not available | |
| Physician's Impression | |||
| Definite | +* | N/A*** | N/A |
| Probable | + | − ** | + |
| Possible | + | − | − |
| Unlikely | +**** | − | − |
patients in “+” boxes were classified as having symptomatic meniscal tear
patients in “−” boxes were classified as not having symptomatic meniscal tear
all patients classified by their physician as “definite” for having meniscal tear had obtained an MRI that was positive for meniscal tear
In sensitivity analyses patients with positive MRI but whose physicians' impression' of meniscal tear was “unlikely” were recategorized as not having meniscal tear.
References
- 1.McDermott ID, Amis AA. The consequences of meniscectomy. J Bone Joint Surg Br. 2006;88:1549–56. doi: 10.1302/0301-620X.88B12.18140. [DOI] [PubMed] [Google Scholar]
- 2.Englund M, Guermazi A, Gale D, et al. Incidental meniscal findings on knee MRI in middle-aged and elderly persons. N Engl J Med. 2008;359:1108–15. doi: 10.1056/NEJMoa0800777. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Cullen K, Golosinskiy A. National health statistics reports. National Center for Health Statistics; 2009. Ambulatory Surgery in the United States, 2006. [PubMed] [Google Scholar]
- 4.Biswal S, Hastie T, Andriacchi TP, Bergman GA, Dillingham MF, Lang P. Risk factors for progressive cartilage loss in the knee: a longitudinal magnetic resonance imaging study in forty-three patients. Arthritis Rheum. 2002;46:2884–92. doi: 10.1002/art.10573. [DOI] [PubMed] [Google Scholar]
- 5.Englund M. The role of the meniscus in osteoarthritis genesis. Med Clin North Am. 2009;93:37–43. x. doi: 10.1016/j.mcna.2008.08.005. [DOI] [PubMed] [Google Scholar]
- 6.Katz JN, Martin SD. Meniscus--friend or foe: epidemiologic observations and surgical implications. Arthritis Rheum. 2009;60:633–5. doi: 10.1002/art.24363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Sim J, Wright CC. The kappa statistic in reliability studies: use, interpretation, and sample size requirements. Phys Ther. 2005;85:257–68. [PubMed] [Google Scholar]
- 8.Alberg AJ, Park JW, Hager BW, Brock MV, Diener-West M. The use of “overall accuracy” to evaluate the validity of screening or diagnostic tests. J Gen Intern Med. 2004;19:460–5. doi: 10.1111/j.1525-1497.2004.30091.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Spearman C. The proof and measurement of association between two things. By C. Spearman, 1904. Am J Psychol. 1987;100:441–71. [PubMed] [Google Scholar]
- 10.Landis JR, Koch GG. The measurement of observer agreement for categorical data. Biometrics. 1977;33:159–74. [PubMed] [Google Scholar]
- 11.Campbell DT, Fiske DW. Convergent and discriminant validation by the multitrait-multimethod matrix. Psychol Bull. 1959;56:81–105. [PubMed] [Google Scholar]
- 12.Radack KL, Rouan G, Hedges J. The likelihood ratio. An improved measure for reporting and evaluating diagnostic test results. Arch Pathol Lab Med. 1986;110:689–93. [PubMed] [Google Scholar]
- 13.Dervin GF, Stiell IG, Wells GA, Rody K, Grabowski J. Physicians' accuracy and interrator reliability for the diagnosis of unstable meniscal tears in patients having osteoarthritis of the knee. Can J Surg. 2001;44:267–74. [PMC free article] [PubMed] [Google Scholar]
- 14.Kocabey Y, Tetik O, Isbell WM, Atay OA, Johnson DL. The value of clinical examination versus magnetic resonance imaging in the diagnosis of meniscal tears and anterior cruciate ligament rupture. Arthroscopy. 2004;20:696–700. doi: 10.1016/j.arthro.2004.06.008. [DOI] [PubMed] [Google Scholar]
- 15.Kurosaka M, Yagi M, Yoshiya S, Muratsu H, Mizuno K. Efficacy of the axially loaded pivot shift test for the diagnosis of a meniscal tear. Int Orthop. 1999;23:271–4. doi: 10.1007/s002640050369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Mohan BR, Gosal HS. Reliability of clinical diagnosis in meniscal tears. Int Orthop. 2007;31:57–60. doi: 10.1007/s00264-006-0131-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Munk B, Madsen F, Lundorf E, et al. Clinical magnetic resonance imaging and arthroscopic findings in knees: a comparative prospective study of meniscus anterior cruciate ligament and cartilage lesions. Arthroscopy. 1998;14:171–5. doi: 10.1016/s0749-8063(98)70036-2. [DOI] [PubMed] [Google Scholar]
- 18.Rose NE, Gold SM. A comparison of accuracy between clinical examination and magnetic resonance imaging in the diagnosis of meniscal and anterior cruciate ligament tears. Arthroscopy. 1996;12:398–405. doi: 10.1016/s0749-8063(96)90032-8. [DOI] [PubMed] [Google Scholar]
- 19.Boden SD, Labropoulos PA, Vailas JC. MR scanning of the acutely injured knee: sensitive, but is it cost effective? Arthroscopy. 1990;6:306–10. doi: 10.1016/0749-8063(90)90061-h. [DOI] [PubMed] [Google Scholar]
- 20.Glashow JL, Katz R, Schneider M, Scott WN. Double-blind assessment of the value of magnetic resonance imaging in the diagnosis of anterior cruciate and meniscal lesions. J Bone Joint Surg Am. 1989;71:113–9. [PubMed] [Google Scholar]
- 21.Mink JH, Levy T, Crues JV., 3rd Tears of the anterior cruciate ligament and menisci of the knee: MR imaging evaluation. Radiology. 1988;167:769–74. doi: 10.1148/radiology.167.3.3363138. [DOI] [PubMed] [Google Scholar]
- 22.Fowler PJ, Lubliner JA. The predictive value of five clinical signs in the evaluation of meniscal pathology. Arthroscopy. 1989;5:184–6. doi: 10.1016/0749-8063(89)90168-0. [DOI] [PubMed] [Google Scholar]
- 23.Noble J, Erat K. In defence of the meniscus. A prospective study of 200 meniscectomy patients. J Bone Joint Surg Br. 1980;62-B:7–11. doi: 10.1302/0301-620X.62B1.7351438. [DOI] [PubMed] [Google Scholar]
- 24.Evans PJ, Bell GD, Frank C. Prospective evaluation of the McMurray test. Am J Sports Med. 1993;21:604–8. doi: 10.1177/036354659302100420. [DOI] [PubMed] [Google Scholar]
- 25.Cicchetti DV, Feinstein AR. High agreement but low kappa: II. Resolving the paradoxes. J Clin Epidemiol. 1990;43:551–8. doi: 10.1016/0895-4356(90)90159-m. [DOI] [PubMed] [Google Scholar]
- 26.Feinstein AR, Cicchetti DV. High agreement but low kappa: I. The problems of two paradoxes. J Clin Epidemiol. 1990;43:543–9. doi: 10.1016/0895-4356(90)90158-l. [DOI] [PubMed] [Google Scholar]
- 27.Tan EM, Cohen AS, Fries JF, et al. The 1982 revised criteria for the classification of systemic lupus erythematosus. Arthritis Rheum. 1982;25:1271–7. doi: 10.1002/art.1780251101. [DOI] [PubMed] [Google Scholar]
- 28.Arnett FC, Edworthy SM, Bloch DA, et al. The American Rheumatism Association 1987 revised criteria for the classification of rheumatoid arthritis. Arthritis Rheum. 1988;31:315–24. doi: 10.1002/art.1780310302. [DOI] [PubMed] [Google Scholar]
- 29.Katz JN, Dalgas M, Stucki G, et al. Degenerative lumbar spinal stenosis. Diagnostic value of the history and physical examination. Arthritis Rheum. 1995;38:1236–41. doi: 10.1002/art.1780380910. [DOI] [PubMed] [Google Scholar]
- 30.Feinstein A. Clinical Epidemiology: The Architecture of Clinical Research. WB Saunders; Philadelphia: 1985. [Google Scholar]
- 31.Altman R, Asch E, Bloch D, et al. Development of criteria for the classification and reporting of osteoarthritis, classification of osteoarthritis of the knee. Arthritis Rheum. 1986;29:1039. doi: 10.1002/art.1780290816. [DOI] [PubMed] [Google Scholar]