Abstract
Patients with chronic kidney disease (CKD) are well known to have a higher prevalence of cardiovascular disease from epidemiological studies. Recently, CKD has also been shown to be related to neurological disorders, not only ischemic brain injury but also cognitive impairment. This cerebrorenal connection is considered to involve small vessel disease in both the kidney and brain, based on their hemodynamic similarities. Clinical studies suggest that markers for CKD such as estimated glomerular filtration rate (eGFR), proteinuria, and albuminuria may be helpful to predict brain small vessel disease, white matter lesions (WMLs), silent brain ischemia (SBI), and microhemorrhages. Recently, changes in the vascular system of the brain have been shown to contribute to the onset and progression of cognitive impairment, not only vascular dementia but also Alzheimer's disease. Patients with CKD are also reported to have higher risk of impaired cognitive function in the future compared with non-CKD subjects. These results indicate that CKD markers may be helpful to predict the future risk of neuronal disease.
1. Introduction
Recently, the relation between chronic kidney disease (CKD) and neurological disorders, not only cerebrovascular disease such as ischemic brain injury but also cognitive impairment such as Alzheimer's disease, has been highlighted. This cerebrorenal interaction is considered to be based on small vessel disease. Cerebral and glomerular small vessel disease might have a common soil of pathogenesis, as these organs are closely connected with each other through anatomic and vasoregulatory similarities. Because small vessel disease is a systemic disorder, information about small vessel disease in one organ may provide information on damage in another organ. For the kidney, damage markers are albuminuria/proteinuria and a reduction in estimated glomerular filtration rate (eGFR), which is also a marker of CKD. On the other hand, damage markers in the brain could be magnetic resonance imaging- (MRI-) documented small vessel alterations. Recently, clinical investigations have suggested a relation between these damage markers in the kidney and the brain. Here, we review the cerebrorenal interactions mainly from a clinical view.
2. Clinical Relation between CKD and Cerebrovascular Disease
2.1. Stroke
Recently, the relation between CKD and the onset of stroke has been highlighted. The Northern Manhattan Study (NOMAS), which followed 3298 stroke-free subjects for vascular outcomes with a mean follow-up time of 6.5 years, showed that CKD, which was estimated using serum creatinine and the Cockcroft-Gault formula, between 15 and 59 mL/min is a strong risk factor for stroke (hazard ratio (HR) = 2.65) [1]. In contrast, Bos et al. demonstrated that decreased eGFR (<60 mL/min/1.73 m2) is a strong risk factor for hemorrhagic but not ischemic stroke (HR = 4.10 for hemorrhagic stroke versus 0.87 for ischemic stroke) in the Rotterdam Study [2]. The authors considered two hypotheses for this relation. The first, decreased GFR indicates small vessel disease not only in the kidney but also in the brain. Small vessel disease seems to be the main pathophysiological mechanism in hemorrhage rather than brain infarction; therefore, the authors suggested that GFR may be a marker of cerebral small vessel disease, especially hemorrhage. The second, the authors considered platelet dysfunction to be an inducible factor by CKD. Severe CKD patients show prolonged bleeding time and mucosal oozing [3], indicating that platelet dysfunction may be involved in the relation between eGFR and hemorrhagic stroke. In the relation between microalbuminuria and incident stroke, prospective cohort studies using meta-analysis with 12 prospective cohort studies including 48,596 individuals with more than 1200 stroke events have been very recently published [4]. The presence of microalbuminuria was greatly associated with stroke onset even after adjustment for cardiovascular risk factors (overall HR 1.92), indicating that albuminuria contribute to be a strong predictor for the incidence of stroke. Recently, asymptomatic cerebral small vessel disease has been investigated as a predictor of the risk of future stroke. Oksala et al. demonstrated that cerebral small vessel disease is closely associated with kidney function in patients with acute stroke. Patients with cerebral small vessel disease and impaired kidney function (eGFR < 60 mL/min/1.73 m2) exhibit poor poststroke survival [5]. These results indicate that Representative cerebral small vessel diseases include white matter lesions (WMLs), silent brain infarction (SBI), and microhemorrhages as well as lacunar infarcts and subcortical atrophy.
2.2. White Matter Lesions
WMLs are detected as hyperintense areas on T2-weighted MRI in areas that are bilaterally and symmetrically sited in the hemispheric white matter. The prevalence of WMLs is significantly related to the risk of stroke, cognitive decline, and dementia [6–8]. The NOMAS demonstrated that white matter hyperintensity volume is associated with moderate-to-severe CKD, which was estimated using serum creatinine and the Cockcroft-Gault formula, between 15 and 59 mL/min [9]. Wada et al. demonstrated that subjects with lower eGFR (less than 60 mL/min/1.73 m2) tended to have more lacunar infarcts and higher grade of WMLs; moreover, mean grade of WMLs and the mean number of lacunar infarcts in subjects with albuminuria were greater than those in subjects without albuminuria [10]. Furthermore, they also reported that urinary albumin level was associated with cerebral small vessel disease, independently of traditional cerebrovascular risk factors, in community-based elderly [11]. Similarly, Ikram et al. investigated the relation between kidney function evaluated by eGFR and cerebral small vessel disease via MRI analysis. They clearly showed that decreased eGFR was related to subclinical markers of cerebral small vessel disease such as deep white matter volume and WNLs independent of cardiovascular risk factors such as age, sex, blood pressure, and diabetes [12]. Interestingly, they also demonstrated that persons with lower eGFR had a smaller brain volume, indicating that CKD may relate to brain atrophy.
2.3. Silent Brain Infarction
On the other hand, SBI is defined as a cerebral infarction detected by brain imaging without clinical symptoms. Kobayashi et al. also reported that there is an independent association between SBI and eGFR [13]. The prevalence of SBI and the number of SBIs increased markedly as eGFR decreased. The presence of SBI is reported to predict clinical overt stroke [14, 15] or cognitive impairment. Therefore, patients with CKD should be assessed for SBI by MRI during the follow-up period. In contrast, Uzu et al. followed 608 patients with type 2 diabetes for 7.5 years and very recently reported that SBI may predict the progression of kidney disease in these patients [16]. The risk of end-stage renal disease (ESRD) or death was significantly higher in patients with SBI than in those without (HR 2.44). The estimated eGFR declined more in patients with SBI than in those without; however, the presence of SBI did not increase the risk of progression of albuminuria.
2.4. Microhemorrhages
Microhemorrhages are discrete or isolated punctate hypointense lesions smaller than 5 mm on T2*-weighted MRI. They are considered to be clinically silent but are strongly associated with advanced small vessel or microvascular ischemic disease [17, 18] and to be a marker for increased risk of future intracranial hemorrhage [19, 20]. Interestingly, Cho et al. showed that lower eGFR is associated with the presence of cerebral microhemorrhages [21]. Moreover, proteinuria is also strongly associated with both the frequency and number of cerebral microhemorrhages in patients with recent cerebral ischemia [22]. Therefore, CKD may increase the risk of hemorrhagic microangiopathy in the brain.
2.5. Hypertensive Nephroangiosclerosis
Hypertensive nephroangiosclerosis was observed in 25% of patients with ESRD in the United States [23]. Because nephroangiosclerosis is also mostly clinically silent, its prevalence in stroke patients is not well known. A recent autopsy data bank clearly demonstrated that nephroangiosclerosis is common in patients with fatal stroke. Indeed, nephroangiosclerosis is independently associated with the prevalence or history of hypertension in stroke patients (39.8% of patients with stroke versus 9.0% of patients with other neurologic diseases) [24]. These results suggest that senile kidney change is also commonly observed in patients with cerebrovascular disease and a true relation between kidney dysfunction and cerebral small vessel disease; however, the factors connecting kidney dysfunction and cerebrovascular disease remain under discussion.
3. Clinical Relation between CKD and Cognitive Impairment
Dementia and cognitive decline impair the quality of life and are associated with a profound disease burden, morbidity, and mortality, not only in patients but also in caregivers. Although an earlier approach to prevent cognitive dysfunction has been expected, there are few markers for evaluating the future risk of cognitive decline in subjects. Recently, impaired kidney function was reported to be associated with dementia and cognitive impairment. The REasons for Geographic and Racial Differences in Stroke (REGARDS) Study with 23,405 participants showed that reduced kidney function is associated with a higher prevalence of cognitive impairment [25]. In patients with CKD, each 10 mL/min/1.73 m2 decrease in eGFR below 60 mL/min/1.73 m2 was associated with an 11% increased prevalence of cognitive impairment (HR = 1.11). Yaffe et al. conducted a chronic renal insufficiency cohort cognitive study in 825 adults aged 55 and older with CKD [26]. Participants with advanced CKD (eGFR < 30 mL/min/1.73 m2) were more likely to have clinically significant impairment of global cognition than those with mild-to-moderate CKD (eGFR 45–59 mL/min/1.73 m2) (HR = 2.0). Moreover, Buchman et al. reported a prospective, observational cohort study in 886 elderly without dementia [27]. Impaired kidney function (eGFR < 60 mL/min/1.73 m2) at baseline was associated with a more rapidly decline in cognitive, especially in semantic memory, episodic memory, and working memory. In contrast, Jassal et al. very recently demonstrated that baseline albuminuria, but not eGFR, was associated with reduced cognitive function only in men [28]. They indicated that albuminuria was a simple predictor of future cognitive decline. Although there is sex difference in the relation between albuminuria and cognitive impairment, kidney function may provide an important window on future cognitive impairment. Recently, changes in the vascular system in the brain have been shown to contribute to the onset and progression of dementia [29]. The so-called “central nervous system (CNS) neurovascular unit” is linked to many common human CNS pathological conditions including dementia. Although multiple mechanisms are involved in cognitive impairment and dementia associated with CKD, small vessel disease in the kidney and brain is also considered to have a key role in this connection.
4. Hemodynamic Similarities of Vascular Beds between Kidney and Brain
Unlike most organs, both the kidney and brain are low resistance end-organs that are exposed to high-volume blood flow throughout the cardiac cycle. These hemodynamic similarities are observed in the vascular beds in the kidney and the brain [30]; therefore, small vessel disease in the kidney may let us know of the presence of small vessel disease in the brain. Ito et al. proposed the very interesting “strain vessel hypothesis” as a possible mechanism for cerebro-cardio-renal connections [31]. Based on the similarity of the juxtamedullary afferent arterioles in the kidney to the perforating arteries in the brain, they are thought to be evolutionally developed to maintain the perfusion of vital tissues such as nephrons and the brainstem directly from large arteries to deliver blood to the tissue. These “strain vessels” are exposed to very high pressure and maintain a high vascular tone. Vascular damage induced by high arterial blood pressure and diabetes mellitus occurs in these similar strain vessels; therefore, microalbuminuria may be an indicator of vascular damage not only in the kidney but also in the brain. One of the common molecular components of small-vessel physiology that may also mediate microvascular dysfunction or injury is nitric oxide. Many papers have reported that nitric oxide deficiency could occur in renal disease, and this subject was been well reviewed by Baylis [32]. Nitric oxide regulates the microcirculation and the blood brain barrier [33], both of which are implicated in the development of WMLs and other manifestations of small vessel disease in the brain. Moreover, patients with impaired cognitive function show increased levels of endogenous inhibitors of nitric oxide synthesis and decreased nitric oxide metabolites [34]. Therefore, decreased nitric oxide may be one of the key factors in the cerebrorenal connection.
5. Prevention and Future Perspectives
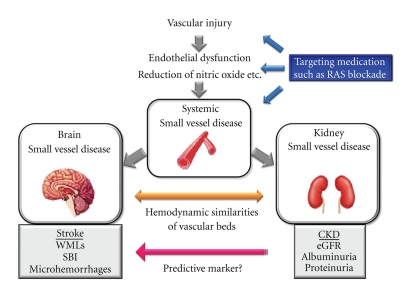
These reports above strongly suggest that a brain and kidney connection exists and that systematic treatment targeting small vessel disease is therapeutically effective on not only the apparent damaged organ but also on the silently damaged organs (Figure 1). According to their unique shared susceptibility to vascular injury from central aortic pressure as a strain vessel, a logical preventive approach to cerebrorenal-related dysfunction is to achieve a reduction of central pulse pressure. A reduction of the central pulse pressure involves a reduction of the wave reflection by dilation of conduit arteries, since drugs do not directly affect the aorta and large arteries. Therefore, antihypertensive drugs should be selected to reduce the central pulse pressure, such as renin-angiotensin system (RAS) blockers and calcium-channel antagonists (CCB). For the kidney, there is good evidence from large clinical studies that blockade of RAS is highly effective to prevent renal damage compared with other antihypertensive drugs. In the brain, recent large clinical trials indicate that RAS blockade with angiotensin receptor blockers (ARBs) is effective to prevent a first or recurrent stroke beyond their blood pressure-lowering effect [35–37]. Moreover, a very recent paper clearly demonstrated that patients treated with ARBs have less severe deficit after stroke [38]. These results suggest that treatment with ARBs may be effective not only to reduce blood pressure but also to protect both the kidney and brain via preventing small vessel disease. However, the Blood Pressure Lowering Treatment Trialists' Collaboration (BPLTTC) demonstrates that all of the blood pressure-lowering regimens have broadly similar protection against stroke [39]. Moreover, there are not any large clinical studies that demonstrate the effect of ARBs on dementia or cognitive impairment. Therefore, there is few evidence of the preventive effect of RAS blockade in the brain compared with that in the kidney. On the other hand, CCBs are proved to have preventive effect on dementia in the Systolic Hypertension in Europe (Syst-Eur) study [40]. CCB, nitrendipine was found to be effective to reduce the incidence of dementia. This is the only large clinical study that shows the effect of anti-hypertensive drug on dementia. Although several CCBs are reported to have renoprotective effects, generally CCBs do not have a remarkable effect on CKD prevention compared with RAS blockade due to the preferentially dilate afferent arteriole. Therefore, preventive effect of CCBs on cerebrorenal connection is also still under investigation. Furthermore, although hypertension may be involved in each pathological change in brain and kidney, it can be result of high blood pressure “in parallel,” indicating that direct evidence of common mechanistic factors in hypertension-induced cerebrorenal damage is still under investigation.
Figure 1.
Schematic representation of cerebrorenal connection. RAS: renin-angiotensin system, CKD: chronic kidney disease, eGFR: estimated glomerular filtration rate, WMLs: white matter lesions, and SBI: silent brain infarction.
6. Conclusion
A cerebro-renal connection exists clinically. CKD markers may be helpful to evaluate the future risk of neuronal disease (Figure 1). Further investigation of the brain-kidney connection may contribute to prevention of impaired quality of life from multiple organ dysfunction due to small vessel disease. Furthermore, protection of the damaged organ will shift to protection of multiple hidden damaged organs, focusing on systemic small vessel disease.
References
- 1.Nickolas TL, Khatri M, Boden-Albala B, et al. The association between kidney disease and cardiovascular risk in a multiethnic cohort: findings from the Northern Manhattan Study (NOMAS) Stroke. 2008;39(10):2876–2879. doi: 10.1161/STROKEAHA.107.513713. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bos MJ, Koudstaal PJ, Hofman A, Breteler MMB. Decreased glomerular filtration rate is a risk factor for hemorrhagic but not for ischemic stroke: the Rotterdam Study. Stroke. 2007;38(12):3127–3132. doi: 10.1161/STROKEAHA.107.489807. [DOI] [PubMed] [Google Scholar]
- 3.Noris M, Remuzzi G. Uremic bleeding: closing the circle after 30 years of controversies? Blood. 1999;94(8):2569–2574. [PubMed] [Google Scholar]
- 4.Lee M, Saver JL, Chang K-H, Liao H-W, Chang S-C, Ovbiagele B. Impact of microalbuminuria on incident stroke: a meta-analysis. Stroke. 2010;41(11):2625–2631. doi: 10.1161/STROKEAHA.110.581215. [DOI] [PubMed] [Google Scholar]
- 5.Oksala NKJ, Salonen T, Strandberg T, et al. Cerebral small vessel disease and kidney function predict long-term survival in patients with acute stroke. Stroke. 2010;41(9):1914–1920. doi: 10.1161/STROKEAHA.110.587352. [DOI] [PubMed] [Google Scholar]
- 6.Vermeer SE, Hollander M, Van Dijk EJ, Hofman A, Koudstaal PJ, Breteler MMB. Silent brain infarcts and white matter lesions increase stroke risk in the general population: the Rotterdam Scan Study. Stroke. 2003;34(5):1126–1129. doi: 10.1161/01.STR.0000068408.82115.D2. [DOI] [PubMed] [Google Scholar]
- 7.Prins ND, Van Dijk EJ, Den Heijer T, et al. Cerebral white matter lesions and the risk of dementia. Archives of Neurology. 2004;61(10):1531–1534. doi: 10.1001/archneur.61.10.1531. [DOI] [PubMed] [Google Scholar]
- 8.Au R, Massaro JM, Wolf PA, et al. Association of white matter hyperintensity volume with decreased cognitive functioning: the Framingham Heart Study. Archives of Neurology. 2006;63(2):246–250. doi: 10.1001/archneur.63.2.246. [DOI] [PubMed] [Google Scholar]
- 9.Khatri M, Wright CB, Nickolas TL, et al. Chronic kidney disease is associated with white matter hyperintensity volume: the Northern Manhattan Study (NOMAS) Stroke. 2007;38(12):3121–3126. doi: 10.1161/STROKEAHA.107.493593. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Wada M, Nagasawa H, Iseki C, et al. Cerebral small vessel disease and chronic kidney disease (CKD): results of a cross-sectional study in community-based Japanese elderly. Journal of the Neurological Sciences. 2008;272(1-2):36–42. doi: 10.1016/j.jns.2008.04.029. [DOI] [PubMed] [Google Scholar]
- 11.Wada M, Nagasawa H, Kurita K, et al. Microalbuminuria is a risk factor for cerebral small vessel disease in community-based elderly subjects. Journal of the Neurological Sciences. 2007;255(1-2):27–34. doi: 10.1016/j.jns.2007.01.066. [DOI] [PubMed] [Google Scholar]
- 12.Ikram MA, Vernooij MW, Hofman A, Niessen WJ, Van Der Lugt A, Breteler MMB. Kidney function is related to cerebral small vessel disease. Stroke. 2008;39(1):55–61. doi: 10.1161/STROKEAHA.107.493494. [DOI] [PubMed] [Google Scholar]
- 13.Kobayashi M, Hirawa N, Yatsu K, et al. Relationship between silent brain infarction and chronic kidney disease. Nephrology Dialysis Transplantation. 2009;24(1):201–207. doi: 10.1093/ndt/gfn419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Howard G, Wagenknecht LE, Cai J, Cooper L, Kraut MA, Toole JF. Cigarette smoking and other risk factors for silent cerebral infarction in the general population. Stroke. 1998;29(5):913–917. doi: 10.1161/01.str.29.5.913. [DOI] [PubMed] [Google Scholar]
- 15.Kobayashi S, Okada K, Koide H, Bokura H, Yamaguchi S. Subcortical silent brain infarction as a risk factor for clinical stroke. Stroke. 1997;28(10):1932–1939. doi: 10.1161/01.str.28.10.1932. [DOI] [PubMed] [Google Scholar]
- 16.Uzu T, Kida Y, Shirahashi N, et al. Cerebral microvascular disease predicts renal failure in type 2 diabetes. Journal of the American Society of Nephrology. 2010;21(3):520–526. doi: 10.1681/ASN.2009050558. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kwa VIH, Franke CL, Verbeeten Jr. B, Stam J. Silent intracerebral microhemorrhages in patients with ischemic stroke. Amsterdam Vascular Medicine Group. Annals of Neurology. 1998;44(3):372–377. doi: 10.1002/ana.410440313. [DOI] [PubMed] [Google Scholar]
- 18.Kato H, Izumiyama M, Izumiyama K, Takahashi A, Itoyama Y. Silent cerebral microbleeds on T2∗-weighted MRI: correlation with stroke subtype, stroke recurrence, and leukoaraiosis. Stroke. 2002;33(6):1536–1540. doi: 10.1161/01.str.0000018012.65108.86. [DOI] [PubMed] [Google Scholar]
- 19.Roob G, Lechner A, Schmidt R, Flooh E, Hartung HP, Fazekas F. Frequency and location of microbleeds in patients with primary intracerebral hemorrhage. Stroke. 2000;31(11):2665–2669. doi: 10.1161/01.str.31.11.2665. [DOI] [PubMed] [Google Scholar]
- 20.Nighoghossian N, Hermier M, Adeleine P, et al. Old microbleeds are a potential risk factor for cerebral bleeding after ischemic stroke: a gradient-echo T2∗-weighted brain MRI study. Stroke. 2002;33(3):735–742. doi: 10.1161/hs0302.104615. [DOI] [PubMed] [Google Scholar]
- 21.Cho AH, Lee SB, Han SJ, Shon YM, Yang DW, Kim BS. Impaired kidney function and cerebral microbleeds in patients with acute ischemic stroke. Neurology. 2009;73(20):1645–1648. doi: 10.1212/WNL.0b013e3181c1defa. [DOI] [PubMed] [Google Scholar]
- 22.Ovbiagele B, Liebeskind DS, Pineda S, Saver JL. Strong independent correlation of proteinuria with cerebral microbleeds in patients with stroke and transient ischemic attack. Archives of Neurology. 2010;67(1):45–50. doi: 10.1001/archneurol.2009.310. [DOI] [PubMed] [Google Scholar]
- 23.Foley RN, Collins AJ. End-stage renal disease in the United States: an update from the United States Renal Data System. Journal of the American Society of Nephrology. 2007;18(10):2644–2648. doi: 10.1681/ASN.2007020220. [DOI] [PubMed] [Google Scholar]
- 24.Abboud H, Labreuche J, Duyckaerts C, Hauw JJ, Amarenco P. Prevalence of nephroangiosclerosis in patients with fatal stroke. Neurology. 2009;72(10):899–904. doi: 10.1212/01.wnl.0000344165.77496.05. [DOI] [PubMed] [Google Scholar]
- 25.Kurella Tamura M, Wadley V, Yaffe K, et al. Kidney function and cognitive impairment in US adults: the Reasons for Geographic and Racial Differences in Stroke (REGARDS) Study. American Journal of Kidney Diseases. 2008;52(2):227–234. doi: 10.1053/j.ajkd.2008.05.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Yaffe K, Ackerson L, Tamura MK, et al. Chronic kidney disease and cognitive function in older adults: findings from the chronic renal insufficiency cohort cognitive study. Journal of the American Geriatrics Society. 2010;58(2):338–345. doi: 10.1111/j.1532-5415.2009.02670.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Buchman AS, Tanne D, Boyle PA, Shah RC, Leurgans SE, Bennett DA. Kidney function is associated with the rate of cognitive decline in the elderly. Neurology. 2009;73(12):920–927. doi: 10.1212/WNL.0b013e3181b72629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Jassal SK, Kritz-Silverstein D, Barrett-Connor E. A prospective study of albuminuria and cognitive function in older adults. American Journal of Epidemiology. 2010;171(3):277–286. doi: 10.1093/aje/kwp426. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Zlokovic BV. New therapeutic targets in the neurovascular pathway in Alzheimer’s disease. Neurotherapeutics. 2008;5(3):409–414. doi: 10.1016/j.nurt.2008.05.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.O’Rourke MF, Safar ME. Relationship between aortic stiffening and microvascular disease in brain and kidney: cause and logic of therapy. Hypertension. 2005;46(1):200–204. doi: 10.1161/01.HYP.0000168052.00426.65. [DOI] [PubMed] [Google Scholar]
- 31.Ito S, Nagasawa T, Abe M, Mori T. Strain vessel hypothesis: a viewpoint for linkage of albuminuria and cerebro-cardiovascular risk. Hypertension Research. 2009;32(2):115–121. doi: 10.1038/hr.2008.27. [DOI] [PubMed] [Google Scholar]
- 32.Baylis C. Nitric oxide deficiency in chronic kidney disease. American Journal of Physiology. 2008;294(1):F1–F9. doi: 10.1152/ajprenal.00424.2007. [DOI] [PubMed] [Google Scholar]
- 33.Iadecola C. Neurovascular regulation in the normal brain and in Alzheimer’s disease. Nature Reviews Neuroscience. 2004;5(5):347–360. doi: 10.1038/nrn1387. [DOI] [PubMed] [Google Scholar]
- 34.Kielstein JT, Böger RH, Bode-Böger SM, et al. Marked increase of asymmetric dimethylarginine in patients with incipient primary chronic renal disease. Journal of the American Society of Nephrology. 2002;13(1):170–176. doi: 10.1681/ASN.V131170. [DOI] [PubMed] [Google Scholar]
- 35.Schrader J, Lüders S, Kulschewski A, et al. Morbidity and mortality after stroke, eprosartan compared with nitrendipine for secondary prevention: principal results of a prospective randomized controlled study (MOSES) Stroke. 2005;36(6):1218–1224. doi: 10.1161/01.STR.0000166048.35740.a9. [DOI] [PubMed] [Google Scholar]
- 36.Mochizuki S, Dahlöf B, Shimizu M, et al. Valsartan in a Japanese population with hypertension and other cardiovascular disease (Jikei Heart Study): a randomised, open-label, blinded endpoint morbidity-mortality study. Lancet. 2007;369(9571):1431–1439. doi: 10.1016/S0140-6736(07)60669-2. [DOI] [PubMed] [Google Scholar]
- 37.Sawada T, Yamada H, Dahlöf B, Matsubara H. Effects of valsartan on morbidity and mortality in uncontrolled hypertensive patients with high cardiovascular risks: KYOTO heart study. European Heart Journal. 2009;30(20):2461–2469. doi: 10.1093/eurheartj/ehp363. [DOI] [PubMed] [Google Scholar]
- 38.Fuentes B, Fernández-Domínguez J, Ortega-Casarrubios MÁ, Sanjosé B, Martínez-Sánchez P, Díez-Tejedor E. Treatment with angiotensin receptor blockers before stroke could exert a favourable effect in acute cerebral infarction. Journal of Hypertension. 2010;28(3):575–581. doi: 10.1097/HJH.0b013e3283350f50. [DOI] [PubMed] [Google Scholar]
- 39.Turnbull F, Woodward M, Neal B, et al. Do men and women respond differently to blood pressure-lowering treatment? Results of prospectively designed overviews of randomized trials. European Heart Journal. 2008;29(21):2669–2680. doi: 10.1093/eurheartj/ehn427. [DOI] [PubMed] [Google Scholar]
- 40.Forette F, Seux ML, Staessen JA, et al. The prevention of dementia with antihypertensive treatment: new evidence from the systolic hypertension in Europe (syst-eur) study. Archives of Internal Medicine. 2002;162(18):2046–2052. doi: 10.1001/archinte.162.18.2046. [DOI] [PubMed] [Google Scholar]