Abstract
Prevalence of depression is associated inversely with some indicators of socioeconomic position, and the stress of social disadvantage is hypothesized to mediate this relation. Relative to whites, blacks have a higher burden of most physical health conditions but, unexpectedly, a lower burden of depression. This study evaluated an etiologic model that integrates mental and physical health to account for this counterintuitive patterning. The Baltimore Epidemiologic Catchment Area Study (Maryland, 1993–2004) was used to evaluate the interaction between stress and poor health behaviors (smoking, alcohol use, poor diet, and obesity) and risk of depression 12 years later for 341 blacks and 601 whites. At baseline, blacks engaged in more poor health behaviors and had a lower prevalence of depression compared with whites (5.9% vs. 9.2%). The interaction between health behaviors and stress was nonsignificant for whites (odds ratio (OR = 1.04, 95% confidence interval: 0.98, 1.11); for blacks, the interaction term was significant and negative (β: −0.18, P < 0.014). For blacks, the association between median stress and depression was stronger for those who engaged in zero (OR = 1.34) relative to 1 (OR = 1.12) and ≥2 (OR = 0.94) poor health behaviors. Findings are consistent with the proposed model of mental and physical health disparities.
Keywords: adaptation, psychological; depression; health behavior; health status disparities; minority health; stress, psychological
It is established that socioeconomic position (SEP), whether indexed by wealth, income, or education, is associated with racial categorization in the United States (1–3). These inequalities in socioeconomic resources are associated with widespread disparities in burden of health conditions, including heart disease, cancer, and diabetes (4, 5). The precise mechanisms that produce these pervasive disparities have yet to be established, but social disadvantage, as indexed by black race, SEP, and their confluence, is considered a major factor in the perpetuation of health disparities. Indeed, the literature is replete with studies illustrating that social disadvantage, including marginalization through racial residential segregation and discrimination, is linked to poor physical health (1, 6, 7). Low SEP is associated with greater stress exposure over the life course, including witnessing or being a victim of violence (8) and limited access to health care (9). Consistent with the racial patterning of SEP, blacks live in more disorganized and dangerous neighborhoods and face more traumatic life events and chronic stressors than whites do (10–14). Additionally, health behaviors, both enhancing (e.g., physical activity) (14, 15) and deleterious (e.g., smoking, high-fat diets), are similarly associated with SEP and race (5, 16, 17).
It is expected that blacks would experience higher rates of psychiatric disorders, particularly conditions associated with exposure to stress, such as major depression, given the evidence linking social disadvantage to poor physical health (18). Findings from epidemiologic surveys, however, consistently indicate that, compared with whites, blacks report similar or, in some cases, lower rates of lifetime mental disorders, even after accounting for the effects of SEP (19–21), despite evidence that blacks report higher levels of psychological distress (22). These findings seem counterintuitive, and researchers have sought explanations for why blacks experience lower levels of mental disorders than whites do, despite greater social disadvantage. It has been suggested that this patterning is due to misreporting bias (23); however, validation studies have indicated that survey assessments perform equally well for whites and blacks (23, 24), and the consistency of this patterning across different instruments and study populations calls this argument into question. It has also been suggested that this patterning is due to greater utilization of positive coping strategies (e.g., religiosity, social support) among blacks, but such explanatory models are poorly specified and only weakly supported by empirical research (25).
One of the authors (J. S.) has put forth a testable, theory-derived model that accounts for this counterintuitive patterning of social disadvantage and mental and physical health burden across blacks and whites (26). The model rests on 3 empirical observations: 1) exposure to stressors is associated with risk of both physical and mental health problems through physiologic pathways; 2) when faced with exogenous stressors, individuals engage in coping behaviors to mitigate the psychological stress experience (27); and 3) the specific set of stress-responsive behaviors engaged in is shaped by the characteristics of the environment (28). This model posits that individuals who are exposed to chronic stress and live in poor environments will be more likely to engage in poor health behaviors (PHB), such as smoking, alcohol use, drug use, and overeating, because they are the most environmentally accessible coping strategies for socially disadvantaged groups (26). These behaviors act on common biologic structures and processes associated with pleasure and reward systems (29–32), consistent with the hypothesis that these behaviors alleviate, or interrupt, the physiological and psychological consequences of stress.
Recently, Jackson et al. (33) reported that the relation between stressful events and depression risk was moderated by PHB among blacks, such that, at higher levels of stress, blacks who engaged in more PHB were less likely than those who engaged in fewer PHB to meet Diagnostic and Statistical Manual of Mental Disorders criteria for depression 3 years later. This same interaction between PHB and stress was not significant for whites. These initial results suggest that engaging in PHB can be conceptualized as stress-coping strategies and may explain the counterintuitive patterning of a lower burden of stress-related psychopathology, but a higher burden of behaviorally mediated physical health conditions, among blacks relative to whites.
The purpose of this study was to evaluate the association of race, stress, and PHB with risk of depression and chronic health conditions among whites and blacks over a 12-year period in the Baltimore Epidemiologic Catchment Area Study. Consistent with the etiologic model of the counterintuitive racial disparities in depressive disorders and physical health described above, it is predicted that blacks who engage in more PHB will have a lower risk of depression but a higher risk of physical health disorders at follow-up than those who engage in fewer of these behaviors.
MATERIALS AND METHODS
Sample
The Baltimore Epidemiologic Catchment Area Study is a population-based sample of persons drawn from the East Baltimore, Maryland, area who were originally interviewed in 1981 (N = 3,481) as part of the Epidemiologic Catchment Area Project, described in detail elsewhere (34). The Baltimore sample was followed up in 1982 (n = 2,768), 1993 (n = 1,920), and 2004 (n = 1,071); at each wave, approximately 75% of surviving respondents were successfully interviewed (35). The baseline sample was approximately 63% white and 33% black. This present analysis is limited to 601 white and 341 black respondents who were interviewed at both waves 3 (1993) and 4 (2004) and had complete data on depression, health behaviors, life events, and health conditions (88.0% of the sample interviewed in 2004). At wave 3, the age range of these respondents was 30–86 years. Waves 1 and 2 were not used because data on some key variables (e.g., diet and body mass index) were not available.
Measures
Depression.
Respondents were interviewed in person using the Diagnostic Interview Schedule, a fully structured instrument administered by laypersons and intended to mimic a clinical psychiatric interview (36). The Diagnostic Interview Schedule depression module includes 27 items organized into 9 symptom groups and includes probe items to distinguish plausible psychiatric symptoms from other causes (e.g., fatigue due to illness, poor appetite due to medication). The validity and reliability of the Diagnostic Interview Schedule have been evaluated extensively, including in the Baltimore Epidemiologic Catchment Area specifically (37), and has modest agreement with clinical psychiatric interviews (38). The Diagnostic Interview Schedule performs equally well relative to clinical interviews for whites and blacks (38).
Respondents were considered depression cases if they met Diagnostic Interview Schedule criteria for a major depressive episode, minor depression, or an episode of bereavement. Major depressive episode criteria include endorsement of 5 or more symptom groups (i.e., dysphoria, anhedonia, appetite/weight disturbances, problems sleeping, fatigue, cognition problems, guilt, psychomotor changes, or suicidal ideation); at least one must be dysphoria or anhedonia, and symptoms must cluster together within the same month and last for at least 2 weeks. Minor depression is indicated by endorsement of at least 2, but fewer than 5, symptom groups (at least 1 must be dysphoria or anhedonia), with the same requirements concerning duration and clustering of symptoms. Bereavement is indicated by a case of major depressive episode or minor depression with onset following the death of a loved one. Previous studies have indicated that the course and prognosis of depression following bereavement are no different from that stemming from other life events (e.g., job loss) (39).
Distress.
A 31-item version of the General Health Questionnaire (40) was used as an indicator of general distress. This questionnaire has been validated in community samples (41) and includes psychological symptoms over the past few weeks such as feeling helpless, hopeful, and nervous. This General Health Questionnaire score was investigated both as a continuous measure (range: 1–50) and dichotomized at the median (score > 14) to indicate high levels of distress.
Life stress.
Respondents were asked about the occurrence of 10 life events: marriage, separation, divorce, widowhood, death of a/another loved one, had/adopted a child, child moved out of the house, retirement, job loss, and occurrence of a serious illness or injury. Respondents were asked the expectedness of each event (Did you have any idea, in the year beforehand, that [event] was going to happen? and, for those who reported that they had some idea beforehand, How sure were you that you were going to have [event]?). Events were placed in time using the Life Chart Interview (42), a standardized instrument designed to reduce recall bias. “Stressful” events were limited to 6 determined a priori to have prolonged effects in multiple domains of life: widowhood, death of a loved one, child moved out, had/adopted a child, job loss, retirement, and serious illness. We hypothesized that unexpected events would be more stressful than expected events, and we assigned weights reflecting this distinction. Events that were “completely unexpected” were given a weight of 5, events that were somewhat expected were assigned a weight between 4 and 2 (indicating “not very sure,” “fairly sure,” and “quite sure,” respectively), and events that were highly expected (respondent was “absolutely sure” event would occur) were given a weight of 1.
The number of stressful life events that occurred between 1981 and 1993, reported in 1993, ranged from zero to 6. After applying the weights to reflect the expectedness of the events, the indicator of “life stress” over this 12-year period ranged from 1 to 25. This index of life stress was then centered on the overall sample median to improve interpretability.
Poor health behaviors.
Four measures of PHB were assessed by self-report: smoking (cigars/cigarettes), alcohol use, and eating behavior, indicated by body mass index and frequency of eating balanced meals. Being a current smoker was determined by self-reported tobacco use within the past 6 months and was indicated by a dummy variable (1 = current smoker). Alcohol use was indexed by the average number of drinks consumed on days when the respondent drank (median = 2, interquartile range: 1–3). Nondrinkers were coded as consuming zero drinks per day. This variable was then dichotomized at the median (1 = >2 drinks per day). Body mass index (weight in kilograms divided by height in meters squared) was calculated from self-reported height and weight and was then dichotomized as obese (body mass index ≥30) or not (1 = obese). Frequency of eating balanced meals was measured using a 5-point scale (always, most of the time, sometimes, rarely, and never) and was collapsed into a binary dummy variable (1 = rarely/never). These 4 variables were summed to create a count of behaviors (mean = 1.30; standard deviation, 1.01), which was collapsed for analysis into 3 categories (zero, 1, and ≥2 behaviors) because of small counts in some of the cells.
Chronic health conditions.
Chronic health disorders were assessed by self-report. For this analysis, 9 conditions common in later life (type 2 diabetes, heart trouble, hypertension, cancer, arthritis, asthma, fracture, stroke, and incontinence) reported at wave 4 were dichotomized as having ever occurred (1 = had condition) and were then summed to create an indicator of overall health burden (median = 2, interquartile range: 1–3). This score was dichotomized at the median to create a binary indicator of high health burden (1 = >2 chronic conditions).
Other covariates.
Three indicators of SEP were assessed at wave 3: education, employment status, and gross household income. Education was assessed by years of schooling completed. Employment status was indexed by a binary variable (1 = employed). Gross household income was indicated by a 5-level categorical variable, with the highest income (≥$70,000 per year) as the reference category. To account for missing data on household income (missing for 103 (10.9%) respondents), income was imputed on the basis of the sequential regression method using IVEWARE (43). As described previously, missing income values were imputed from variables indicating psychopathology, substance use, and cognitive impairment from wave 3, as well as these variables from waves 1 and 2 (35). Covariates for age (in years) and sex (1 = female) were also included.
Analysis
Multiple logistic regression models, stratified by race, were used to estimate the influence of stress and PHB from wave 3 on the relative odds 12 years later of 1) depression syndrome and 2) chronic health conditions at wave 4. All models were adjusted for age, sex, education, employment status, and household income. The models with depression as the outcome were also adjusted for depression at wave 3.
An interaction term was generated between the count of PHB and median-centered life stress to examine whether PHB moderated the influence of stress on risk of depression. To determine whether this interaction term between stress and PHB significantly improved the model fit for whites and blacks, we used the likelihood ratio test to compare nested logistic regression models with and without this term (44). A value of P < 0.05 from the likelihood ratio test would indicate that the interaction between stressful events and PHB significantly improved the fit of the model to the data, consistent with the hypothesis that these behaviors moderate the influence of life stress on risk of depression.
To determine the specificity of the associations to depression as opposed to general distress, we also examined the relation between life stress and PHB on distress as indicated by the General Health Questionnaire. The General Health Questionnaire distress score was investigated both as a continuous variable in linear regression analyses and as a binary variable in logistic regression models.
The Baltimore Epidemiologic Catchment Area Study was approved by the Johns Hopkins Bloomberg School of Public Health Institutional Review Board. All respondents provided informed consent.
RESULTS
Table 1 describes the demographic characteristics, health behaviors, and mental and physical health of the sample. Blacks had lower educational attainment and household income relative to whites. Blacks experienced more life stress compared with whites (a value of 9.0 vs. 8.1, P < 0.002), but they were less likely to meet criteria for depression. Blacks were more likely than whites to engage in 3 of the 4 PHB examined (the exception being alcohol use). Overall, 14.1% of blacks engaged in none of the health behaviors compared with 26.6% of whites (P < 0.001).
Table 1.
Characteristics of Respondents in the Baltimore Epidemiologic Catchment Area Study, Maryland, 1993–2004a
| Wave 3: Overall (N = 942) | Wave 3 |
P Value | Wave 4 |
P Value | ||||||||
| Whites (n = 601) |
Blacks (n = 341) |
Whites (n = 601) |
Blacks (n = 341) |
|||||||||
| Age, years (mean, SD) | 46.9 | 11.8 | 47.9 | 12.7 | 45.2 | 9.8 | 0.031 | 58.8 | 12.8 | 56.1 | 9.9 | 0.025 |
| Female | 584 | 62.0 | 346 | 57.6 | 238 | 69.8 | <0.001 | 346 | 57.6 | 238 | 69.8 | <0.001 |
| No. of years of education (mean, SD) | 12.5 | 2.6 | 12.6 | 2.6 | 12.2 | 2.7 | 0.035 | 12.7 | 2.7 | 12.4 | 2.7 | 0.067 |
| Employed in the past year | 306 | 32.5 | 185 | 30.8 | 121 | 35.5 | 0.139 | 243 | 40.4 | 141 | 41.4 | 0.783 |
| Gross household income | ||||||||||||
| $≥70,000 | 138 | 14.7 | 110 | 18.3 | 28 | 8.2 | 243 | 40.4 | 69 | 20.2 | ||
| $35,000–$69,999 | 327 | 34.7 | 246 | 40.9 | 81 | 23.8 | 163 | 27.1 | 80 | 23.5 | ||
| $17,500–$34,999 | 223 | 23.7 | 130 | 21.6 | 93 | 27.3 | <0.001 | 88 | 14.6 | 78 | 22.9 | <0.001 |
| $10,000–$17,499 | 137 | 14.5 | 75 | 12.5 | 62 | 18.2 | 82 | 13.6 | 55 | 16.1 | ||
| <$10,000 | 117 | 12.4 | 40 | 6.7 | 77 | 22.6 | 25 | 4.2 | 59 | 17.3 | ||
| No. of negative life events (median, range) | 2 | 1–6 | 2 | 1–5 | 2 | 1–6 | 0.021 | 2 | 0–5 | 2 | 0–5 | 0.019 |
| Life stressb (median, range) | 8 | 1–25 | 7 | 1–25 | 9 | 1–22 | 0.002 | 5 | 1–25 | 6 | 1–25 | 0.002 |
| PHB | ||||||||||||
| Body mass indexc ≥30 kg/m2 | 240 | 28.3 | 131 | 24.3 | 109 | 35.4 | 0.001 | 200 | 36.9 | 162 | 51.9 | <0.001 |
| Rarely/never eat 3 balanced meals/day | 509 | 54.1 | 303 | 50.5 | 206 | 60.4 | 0.003 | 281 | 46.8 | 205 | 60.1 | <0.001 |
| Current smoker | 333 | 35.4 | 186 | 30.9 | 147 | 43.2 | <0.001 | 149 | 24.9 | 121 | 35.5 | <0.001 |
| Drink >2 drinks/dayd on days when drinking alcohol | 197 | 21.1 | 140 | 23.4 | 57 | 16.9 | 0.020 | 89 | 15.1 | 49 | 14.5 | 0.817 |
| Collapsed PHB variable used for analysis | ||||||||||||
| Zero behaviors | 208 | 22.1 | 160 | 26.6 | 48 | 14.1 | 164 | 27.4 | 47 | 13.8 | ||
| 1 behavior | 333 | 35.4 | 206 | 34.3 | 127 | 37.2 | <0.001 | 222 | 37.1 | 109 | 32.1 | <0.001 |
| ≥2 behaviors | 401 | 42.6 | 235 | 39.1 | 166 | 48.7 | 213 | 35.6 | 184 | 54.1 | ||
| Depression and distress indicators | ||||||||||||
| DSM depression syndrome | 148 | 15.7 | 107 | 17.8 | 41 | 12.0 | 0.019 | 106 | 17.6 | 33 | 9.7 | 0.001 |
| GHQ score (mean, SD) | 15.1 | 6.2 | 14.9 | 5.9 | 15.4 | 6.7 | 0.366 | 15.7 | 6.7 | 15.7 | 6.9 | 0.960 |
| High GHQ distress | 430 | 45.7 | 264 | 43.9 | 166 | 46.7 | 0.159 | 263 | 49.3 | 161 | 49.8 | 0.866 |
| Health burden | ||||||||||||
| No. of chronic conditions (median, range) | 1 | 0–7 | 1 | 0–7 | 1 | 0–7 | 0.137 | 2 | 0–7 | 2 | 0–6 | 0.010 |
| High health burden | 143 | 16.0 | 81 | 14.2 | 62 | 19.0 | 0.059 | 157 | 26.1 | 115 | 33.7 | 0.013 |
Abbreviations: DSM, Diagnostic and Statistical Manual of Mental Disorders; GHQ, General Health Questionnaire; PHB, poor health behaviors; SD, standard deviation.
Values are expressed as number and percent unless otherwise noted. P values for chi-squared tests for categorical variables and Mann-Whitney tests for continuous variables comparing whites and blacks within each wave.
Calculated as negative life events weighted by expectedness.
Total number of respondents for body mass index ≥30 = 848.
Total number of respondents for drinks per day = 936.
In bivariate logistic regression models, life stress at wave 3 was associated with higher relative odds of depression at wave 4 for both whites (odds ratio (OR) = 1.06, 95% confidence interval (CI): 1.02, 1.11) and blacks (OR = 1.04, 95% CI: 0.96, 1.12), although the association was statistically significant for whites only. Table 2 shows the results of 3 nested logistic regression models predicting depression at wave 4 by the measures of life stress, health behaviors, and their interaction at wave 3. In model 1, for both whites and blacks, depression at wave 3 was a strong and significant predictor of depression at wave 4. For both groups, higher levels of life stress at wave 3 was modestly, but not significantly, related to depression at wave 4, after accounting for depression at wave 3.
Table 2.
Relative Odds of Depression Syndrome at Wave 4 Predicted by Life Stress and Poor Health Behaviors at Wave 3, the Baltimore Epidemiologic Catchment Area Study, Maryland, 1993–2004
| Model 1 |
Model 2 |
Model 3 |
||||||||||
| Whites |
Blacks |
Whites |
Blacks |
Whites |
Blacks |
|||||||
| OR | 95% CI | OR | 95% CI | OR | 95% CI | OR | 95% CI | OR | 95% CI | OR | 95% CI | |
| Depression syndrome at wave 3 (referent, no depression) | 7.63 | 4.63, 12.56 | 12.57 | 5.21, 30.34 | 7.75 | 4.69, 12.80 | 13.95 | 5.52, 32.24 | 7.80 | 4.71, 12.91 | 15.94 | 6.11, 41.59 |
| Sex (referent, male) | 3.07 | 1.79, 5.27 | 0.99 | 0.39, 2.52 | 2.97 | 1.72, 5.14 | 1.02 | 0.39, 2.67 | 2.89 | 1.67, 5.01 | 1.09 | 0.41, 2.93 |
| Age, years | 0.99 | 0.96, 1.01 | 0.93 | 0.88, 0.99 | 0.99 | 0.96, 1.01 | 0.94 | 0.89, 1.00 | 0.99 | 0.96, 1.01 | 0.95 | 0.89, 1.00 |
| Education, years | 1.05 | 0.94, 1.17 | 1.10 | 0.91, 1.34 | 1.05 | 0.94, 1.17 | 1.15 | 0.94, 1.40 | 1.04 | 0.94, 1.17 | 1.18 | 0.95, 1.46 |
| Currently employed (referent, no) | 0.60 | 0.32, 1.12 | 4.14 | 1.54, 11.16 | 0.59 | 0.32, 1.10 | 5.11 | 1.84, 14.20 | 0.60 | 0.32, 1.11 | 5.90 | 2.05, 16.99 |
| Income (referent, ≥$70,000) | 1.01 | 0.79, 1.30 | 0.67 | 0.44, 1.00 | 1.03 | 0.80, 1.32 | 0.59 | 0.38, 0.90 | 1.03 | 0.80, 1.32 | 0.57 | 0.37, 0.88 |
| Life events, median centered | 1.04 | 0.99, 1.10 | 1.01 | 0.93, 1.11 | 1.05 | 0.99, 1.10 | 1.01 | 0.93, 1.11 | 1.00 | 0.91, 1.09 | 1.34 | 1.06, 1.71 |
| PHB (referent, none) | 0.90 | 0.65, 1.23 | 2.65 | 1.29, 5.43 | 0.88 | 0.64, 1.22 | 4.38 | 1.76, 10.88 | ||||
| Life events × PHB (referent, median events and zero PHB) | 1.04 | 0.98, 1.11 | 0.83 | 0.72, 0.96 | ||||||||
| No. of participants | 601 | 341 | 601 | 341 | 601 | 341 | ||||||
| Log-likelihood | −226.99 | −84.31 | −226.77 | −80.10 | −226.02 | −77.00 | ||||||
| Likelihood ratio test | Referent | Referent | 0.43a | 8.42a | 1.51b | 6.20b | ||||||
| Chi-squared P value | 0.510 | 0.004 | 0.220 | 0.013 | ||||||||
Abbreviations: CI, confidence interval; OR, odds ratio; PHB, poor health behaviors.
Model 2 vs. model 1.
Model 3 vs. model 2.
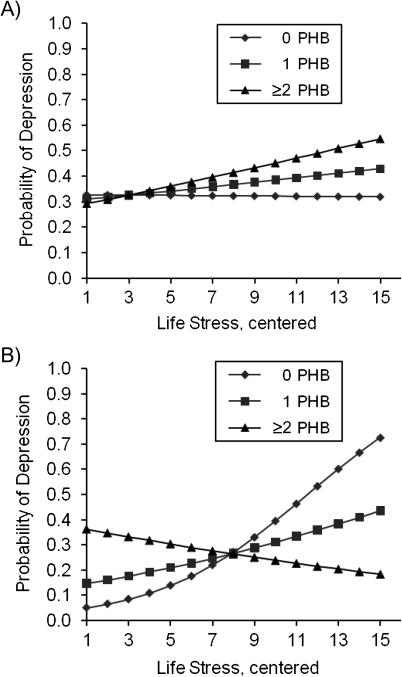
Addition of the count of PHB to the model significantly improved model fit for blacks (likelihood ratio test χ2 = 8.42, P < 0.004) but not whites (χ2 = 0.43, P = 0.510). Adding the interaction between life stress and PHB in model 3 significantly improved model fit for blacks (χ2 = 6.20, P < 0.013) but not whites (χ2 = 1.51, P = 0.220). The interaction term was null for whites (OR = 1.04, P = 0.221) but less than 1 for blacks (OR = 0.83, 95% CI: 0.72, 0.96, P < 0.014), indicating that, as the number of PHB increased, the association between life stress and depression decreased. For blacks, the association between median life stress and depression was stronger for those who engaged in zero PHB (OR = 1.34, 95% CI: 1.06, 1.71) relative to 1 (OR = 1.12, 95% CI: 0.99, 1.27) and 2 or more (OR = 0.94, 95% CI: 0.83, 1.05) behaviors. This result is consistent with the hypothesis that PHB moderate the relation between life stress and depression for blacks. Figure 1 illustrates this interaction between life stress and PHB for both groups.
Figure 1.
Predicted probability of depression at wave 4 by race, number of poor health behaviors (PHB), and life stress at wave 3 for A) whites and B) blacks, the Baltimore Epidemiologic Catchment Area Study, Maryland, 1993–2004.
Table 3 shows the relation between life stress and PHB at wave 3 predicting chronic health conditions 12 years later. Life stress was associated with a modest, but statistically significant increase in the relative odds of chronic health problems for both whites and blacks, even after accounting for PHB (model 1). As expected, PHB at wave 3 were also significantly predictive of chronic conditions. In contrast to the depression analysis, the interaction term between life stress and PHB was close to null and was not statistically significant for either whites or blacks. The likelihood ratio test indicated that adding this term did not significantly improve model fit for either group.
Table 3.
Relative Odds of High Health Burden at Wave 4 Predicted by Life Stress and Poor Health Behaviors at Wave 3, the Baltimore Epidemiologic Catchment Area Study, Maryland, 1993–2004
| Model 1 |
Model 2 |
Model 3 |
||||||||||
| Whites |
Blacks |
Whites |
Blacks | Whites |
Blacks |
|||||||
| OR | 95% CI | OR | 95% CI | OR | 95% CI | OR | 95% CI | OR | 95% CI | OR | 95% CI | |
| Sex (referent, male) | 1.73 | 1.14, 1.08 | 1.51 | 0.86, 2.65 | 1.93 | 1.05, 1.09 | 1.53 | 0.86, 2.72 | 1.91 | 1.24, 2.95 | 1.56 | 0.88, 2.78 |
| Age, years | 1.06 | 1.04, 1.08 | 1.07 | 1.04, 1.10 | 1.07 | 1.05, 1.09 | 1.08 | 1.05, 1.11 | 1.07 | 1.05, 1.09 | 1.07 | 1.04, 1.11 |
| Education, years | 0.98 | 0.90, 1.06 | 0.99 | 0.89, 1.10 | 0.99 | 0.91, 1.08 | 1.00 | 0.90, 1.11 | 0.99 | 0.91, 1.08 | 0.99 | 0.89, 1.11 |
| Currently employed (referent, no) | 0.71 | 0.43, 1.20 | 0.89 | 0.50, 1.60 | 0.74 | 0.44, 1.26 | 0.95 | 0.52, 1.72 | 0.74 | 0.44, 1.26 | 0.95 | 0.52, 1.73 |
| Income (referent, ≥$70,000) | 1.12 | 0.90, 1.38 | 1.31 | 1.03, 1.67 | 1.08 | 0.87, 1.34 | 1.26 | 0.99, 1.61 | 1.08 | 0.87, 1.34 | 1.25 | 0.97, 1.59 |
| Life events, median centered | 1.07 | 1.03, 1.12 | 1.06 | 1.01, 1.12 | 1.07 | 1.02, 1.12 | 1.06 | 1.01, 1.12 | 1.05 | 0.97, 1.14 | 0.98 | 0.85, 1.11 |
| PHB (referent, none) | 1.55 | 1.18, 2.04 | 1.67 | 1.16, 2.41 | 1.55 | 1.18, 2.03 | 1.62 | 1.12, 2.34 | ||||
| Life events × PHB (referent, median events and zero PHB) | 1.01 | 0.96, 1.07 | 1.06 | 0.98, 1.15 | ||||||||
| No. of participants | 601 | 341 | 601 | 341 | 601 | 341 | ||||||
| Log-likelihood | −307.93 | −196.12 | −302.67 | −192.07 | −302.56 | −191.05 | ||||||
| Likelihood ratio test | Referent | Referent | 10.53a | 8.06a | 0.22b | 2.04b | ||||||
| Chi-squared P value | 0.001 | 0.005 | 0.642 | 0.153 | ||||||||
Abbreviations: CI, confidence interval; OR, odds ratio; PHB, poor health behaviors.
Model 2 vs. model 1.
Model 3 vs. model 2.
To assess whether the results from the depression analyses were specific to this clinical psychiatric syndrome, as opposed to general distress, we repeated these analyses for the outcome of distress indicated by the General Health Questionnaire (Table 4). Neither life stress nor PHB were significantly associated with high distress at wave 4 after accounting for General Health Questionnaire score at wave 3, and adding the interaction term between life stress and PHB did not significantly improve model fit for either group. When General Health Questionnaire distress was examined as a continuous variable, the results were similar (Appendix Table 1).
Table 4.
Relative Odds of High Distress at Wave 4 Predicted by Life Stress and Poor Health Behaviors at Wave 3, the Baltimore Epidemiologic Catchment Area Study, Maryland, 1993–2004
| Model 1 |
Model 2 |
Model 3 |
||||||||||
| Whites |
Blacks |
Whites |
Blacks |
Whites |
Blacks |
|||||||
| OR | 95% CI | OR | 95% CI | OR | 95% CI | OR | 95% CI | OR | 95% CI | OR | 95% CI | |
| High distress at wave 3 (referent, low distress) | 2.33 | 1.63, 3.34 | 2.28 | 1.44, 3.63 | 2.33 | 1.63, 3.33 | 2.21 | 1.39, 3.53 | 2.33 | 1.62, 3.33 | 2.22 | 1.39, 3.53 |
| Sex (referent, male) | 1.29 | 0.89, 1.86 | 1.17 | 0.69, 1.96 | 1.27 | 0.88, 1.85 | 1.18 | 0.70, 2.00 | 1.25 | 0.86, 1.82 | 1.20 | 0.71, 1.06 |
| Age, years | 0.99 | 0.37, 1.01 | 1.03 | 1.00, 1.06 | 0.99 | 0.97, 1.01 | 1.03 | 1.01, 1.06 | 0.99 | 0.97, 1.01 | 1.03 | 1.00, 1.06 |
| Education, years | 0.94 | 0.87, 1.02 | 0.94 | 0.85, 1.04 | 0.94 | 0.87, 1.02 | 0.94 | 0.85, 1.05 | 0.94 | 0.87, 1.02 | 0.94 | 0.85, 1.04 |
| Currently employed (referent, no) | 1.09 | 0.67, 1.77 | 1.12 | 0.64, 1.96 | 1.08 | 0.67, 1.76 | 1.15 | 0.65, 2.03 | 1.08 | 0.66, 1.75 | 1.15 | 0.65, 2.04 |
| Income (referent, ≥$70,000) | 1.10 | 0.91, 1.34 | 0.96 | 0.77, 1.21 | 1.11 | 0.91, 1.35 | 0.95 | 0.75, 1.19 | 1.11 | 0.91, 1.35 | 0.94 | 0.75, 1.19 |
| Life events, median centered | 0.97 | 0.93, 1.01 | 1.02 | 0.97, 1.07 | 0.97 | 0.93, 1.01 | 1.02 | 0.97, 1.07 | 0.92 | 0.86, 0.99 | 0.98 | 0.88, 1.10 |
| PHB (referent, none) | 0.96 | 0.77, 1.21 | 1.21 | 0.87, 1.69 | 0.97 | 0.77, 1.22 | 1.19 | 0.85, 1.67 | ||||
| Life events × PHB (referent, median events and zero PHB) | 1.05 | 0.99, 1.10 | 1.03 | 0.96, 1.11 | ||||||||
| No. of participants | 534 | 322 | 534 | 322 | 534 | 322 | ||||||
| Log-likelihood | −352.40 | −211.38 | −352.35 | −210.74 | −350.74 | −210.42 | ||||||
| Likelihood ratio test | Referent | Referent | 0.10a | 1.28a | 3.24b | 0.64b | ||||||
| Chi-squared P value | 0.752 | 0.258 | 0.072 | 0.424 | ||||||||
Abbreviations: CI, confidence interval; OR, odds ratio; PHB, poor health behaviors.
Model 2 vs. model 1.
Model 3 vs. model 2.
We conducted a series of post-hoc analyses to assess the robustness of our findings. We repeated our analysis using a body mass index of >25 (indicating overweight/obese) as the proxy indicator of overeating behavior; findings were consistent. There was no evidence that marital status or life stress experienced between wave 3 and wave 4 confounded the results. Finally, additional adjustment for chronic conditions at wave 3 did not substantially change the findings regarding risk of high health burden.
DISCUSSION
The primary finding of our study is that PHB moderate the positive association between life stress and risk of depression for blacks but not for whites. These results are consistent with the proposed etiologic model linking social disadvantage, exposure to stress, coping via PHB, and mental and physical health disparities (17, 26). These findings replicate the initial results from Jackson et al. (33) and have the advantages of examining these associations over a longer time period and the specificity of the association to depression syndrome as opposed to general distress. This finding indicates that transient psychological distress may not capture the same pathophysiological state indicated by psychiatric conditions, at least concerning the relation between stress and coping. Overall, this study demonstrates that mental and physical health must be considered jointly when investigating the causes of disparities across racial groups and calls into question implicit assumptions about the associations between social disadvantage, health behaviors, and mental health.
The theoretical model we evaluated offers a comprehensive explanation for the seemingly counterintuitive patterning of racial disparities in mental and physical health, and it has implications for efforts to reduce disparities in health. These findings suggest that interventions need to consider not only how disadvantaged environments can be a source of stress but also how material and psychological coping strategies are shaped by environments constrained by poor infrastructure and limited access to healthy foods and recreational activities (45–47). For those living under chronically stressful conditions, it may not be sufficient to promote the prevention or reduction of PHB alone (48). Thus, interventions among low-SEP and marginalized populations require a combined effort to reduce both PHB and the sources of stress that make engaging in such behaviors more likely (49).
The observed difference in the association of stress and PHB with depression risk for blacks and whites begs the question. We think that part of this difference is due to our impoverished measures of social disadvantage and that race may be effectively capturing the unmeasured aspects of differences in cumulative living conditions, including race-based stressors, unsafe living conditions, and financial strain, that are more often experienced over the life course by blacks. If we more comprehensively accounted for this difference in accumulative burden, we think that this ostensible “racial” group difference would be substantially reduced. We will explicitly evaluate this hypothesis in future work.
Limitations and strengths
The results of this study should be interpreted in light of study limitations. First, assessment of some variables was suboptimal. For example, body mass index is influenced by factors other than food intake (e.g., exercise, genetic liability) and is thus only a rough proxy for overeating. Although the measure of life stress reflected major events in multiple domains and accounted for expectedness of the events, the study would have benefited from direct measures of perceived stress severity and indicators of daily hassles and contextual stressors. This analysis did not examine the role that positive coping strategies, such as social support and religiosity, may play in this association. Finally, the relatively long time period between assessments resulted in a subsequent lack of information regarding the dynamic interrelationships of stress and coping between interviews.
This study also has a number of strengths, primarily the use of a population-based sample, which minimizes selection bias. It is prospective, which reduces recall bias and enabled examination of the longer-term consequences of engaging in PHB for physical health outcomes. Depression was measured using a validated, diagnostic interview, which resulted in a more homogenous and clinically relevant assessment of depression relative to checklist measures (37).
Conclusion
This study explored an epidemiologic paradox that challenges existing notions of the nature of the associations between mental and physical health. Future research should focus on identifying the interaction between negative and positive coping behaviors and the development and persistence of disparities in mental and physical health. Researchers should also examine whether the associations we identified extend to other marginalized groups (e.g., some Latino groups), whose health status is also characterized by counterintuitive epidemiologic patterning (50).
Acknowledgments
Author affiliations: Department of Epidemiology and Community Health, Virginia Commonwealth University, Richmond, Virginia (Briana Mezuk); Institute for Social Research, University of Michigan, Ann Arbor, Michigan (Jane A. Rafferty, James S. Jackson); Department of Epidemiology, University of Michigan, Ann Arbor, Michigan (Kiarri N. Kershaw, Cleopatra M. Abdou, Hedwig Lee); Center for Social Disparities in Health, University of California–San Francisco, San Francisco, California (Darrell Hudson); and Department of Mental Health, Johns Hopkins Bloomberg School of Public Health. Baltimore, Maryland (William W. Eaton).
This work was supported by the National Institute of Mental Health (U01-MH57716), with supplemental support from the Office of Behavioral and Social Science Research, the National Institute on Aging (5 R01 AG020282-04), the National Institute on Drug Abuse, the National Center for Minority Health Disparities (1 P60 MD002249-01), and the University of Michigan. Preparation of this paper was also aided by the National Institute of Mental Health (1P01 MH58565 and 1T32 MH67555). The Baltimore Epidemiologic Catchment Area Study is funded by the National Institute on Drug Abuse (R01 DA026652). Additional support was provided by the Robert Wood Johnson Health and Society Scholars Program and the Center for Integrative Approaches to Health Disparities at the University of Michigan.
Conflict of interest: none declared.
Glossary
Abbreviations
- CI
confidence interval
- OR
odds ratio
- PHB
poor health behaviors
- SEP
socioeconomic position
Appendix Table 1.
Expected Change (β (SE)) in GHQ Score at Wave 4 Predicted by Coping Behaviors at Wave 3, Baltimore Epidemiologic Catchment Area, Maryland, 1994/1996–2004/2005
| Model 1 |
Model 2 |
Model 3 |
||||
| Whites | Blacks | Whites | Blacks | Whites | Blacks | |
| GHQ at wave 3 | 0.31 (0.21 to 0.40) | 0.36 (0.25 to 0.47) | 0.31 (0.22 to 0.40) | 0.35 (0.24 to 0.46) | 0.30 (0.21 to 0.40) | 0.35 (0.24 to 0.46) |
| Sex (referent, male) | 0.69 (−0.43 to 1.82) | 0.95 (−0.65 to 2.56) | 0.56 (−0.58 to 1.69) | 1.01 (−0.59 to 2.61) | 0.50 (−0.63 to 1.63) | 1.01 (−0.60 to 2.61) |
| Age, years | −0.05 (−1.11 to −0.002) | 0.01 (−0.07 to 0.08) | −0.06 (−0.12 to −0.01) | 0.01 (−0.07 to 0.09) | −0.06 (−0.12 to −0.01) | 0.01 (−0.07 to 0.09) |
| Education, years | −0.27 (−0.50 to −0.03) | −0.14 (−0.46 to 0.19) | −0.29 (−0.53 to −0.05) | −0.13 (−0.45 to 0.20) | −0.29 (−0.52 to −0.05) | −0.13 (−0.45 to 0.20) |
| Currently employed (referent, no) | 1.27 (−0.21 to 2.74) | 0.53 (−1.29 to 2.36) | 1.21 (−0.27 to 2.69) | 0.65 (−1.18 to 2.48) | 1.20 (−0.28 to 2.67) | 0.65 (−1.19 to 2.48) |
| Income (referent, ≥$70,000) | 0.55 (−0.08 to 1.18) | 0.12 (−0.67 to 0.91) | 0.60 (−0.03 to 1.23) | 0.06 (−0.74 to 0.85) | 0.61 (−0.02 to 1.25) | 0.06 (−0.74 to 0.86) |
| Life events (median centered) | −0.13 (−0.25 to −0.01) | 0.09 (−0.06 to 0.25) | −0.12 (−0.24 to 0.001) | 0.09 (−0.06 to 0.25) | −0.27 (−0.49 to −0.06) | 0.10 (−0.23 to 0.44) |
| PHB (referent, none) | −0.56 (−1.26 to 0.13) | 0.69 (−0.34 to 1.72) | −0.56 (−1.25 to 0.14) | 0.69 (−0.34 to 1.73) | ||
| Life events × PHB (referent, median events and zero PHB) | 0.12 (−0.02 to 0.27) | −0.01 (−0.23 to 0.21) | ||||
| No. of participants | 534 | 322 | 534 | 322 | 534 | 322 |
| R2 | 0.13 | 0.15 | 0.13 | 0.15 | 0.13 | 0.15 |
Abbreviations: GHQ, General Health Questionnaire; PHB, poor health behaviors; SE, standard error.
References
- 1.Williams DR, Collins C. US socioeconomic and racial differences in health: patterns and explanations. Ann Rev Sociol. 1995;21:349–386. [Google Scholar]
- 2.Geronimus AT. To mitigate, resist, or undo: addressing structural influences on the health of urban populations. Am J Public Health. 2000;90(6):867–872. doi: 10.2105/ajph.90.6.867. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.DeNavas-Walt C, Proctor BD, Smith JC. Income, Poverty, and Health Insurance Coverage in the United States: 2008. US Census Bureau, Current Population Reports, P60-236. Washington, DC: US Government Printing Office; 2009. [Google Scholar]
- 4.Mensah GA, Mokdad AH, Ford ES, et al. State of disparities in cardiovascular health in the United States. Circulation. 2005;111(10):1233–1241. doi: 10.1161/01.CIR.0000158136.76824.04. [DOI] [PubMed] [Google Scholar]
- 5.Lantz PM, Lynch JW, House JS, et al. Socioeconomic disparities in health change in a longitudinal study of US adults: the role of health-risk behaviors. Soc Sci Med. 2001;53(1):29–40. doi: 10.1016/s0277-9536(00)00319-1. [DOI] [PubMed] [Google Scholar]
- 6.Geronimus AT, Bound J, Waidmann TA, et al. Excess mortality among blacks and whites in the United States. N Engl J Med. 1996;335(21):1552–1558. doi: 10.1056/NEJM199611213352102. [DOI] [PubMed] [Google Scholar]
- 7.Kaufman JS, Long AE, Liao Y, et al. The relation between income and mortality in U.S. blacks and whites. Epidemiology. 1998;9(2):147–155. [PubMed] [Google Scholar]
- 8.Karlsen S, Nazroo JY. Relation between racial discrimination, social class, and health among ethnic minority groups. Am J Public Health. 2002;92(4):624–631. doi: 10.2105/ajph.92.4.624. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Adler NE, Newman K. Socioeconomic disparities in health: pathways and policies. Health Aff (Millwood) 2002;21(2):60–76. doi: 10.1377/hlthaff.21.2.60. [DOI] [PubMed] [Google Scholar]
- 10.Williams DR, Collins C. Racial residential segregation: a fundamental cause of racial disparities in health. Public Health Rep. 2001;116(5):404–416. doi: 10.1093/phr/116.5.404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Diez Roux AV. Residential environments and cardiovascular risk. J Urban Health. 2003;80(4):569–589. doi: 10.1093/jurban/jtg065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Turner RJ, Lloyd DA. The stress process and the social distribution of depression. J Health Soc Behav. 1999;40(4):374–404. [PubMed] [Google Scholar]
- 13.Turner RJ, Avison WR. Status variations in stress exposure: implications for the interpretation of research on race, socioeconomic status, and gender. J Health Soc Behav. 2003;44(4):488–505. [PubMed] [Google Scholar]
- 14.Turner RJ, Lloyd DA. Stress burden and the lifetime incidence of psychiatric disorder in young adults: racial and ethnic contrasts. Arch Gen Psychiatry. 2004;61(5):481–488. doi: 10.1001/archpsyc.61.5.481. [DOI] [PubMed] [Google Scholar]
- 15.Baltrus PT, Lynch JW, Everson-Rose S, et al. Race/ethnicity, life-course socioeconomic position, and body weight trajectories over 34 years: the Alameda County Study. Am J Public Health. 2005;95(9):1595–1601. doi: 10.2105/AJPH.2004.046292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Galea S, Nandi A, Vlahov D. The social epidemiology of substance use. Epidemiol Rev. 2004;26:36–52. doi: 10.1093/epirev/mxh007. [DOI] [PubMed] [Google Scholar]
- 17.Krueger PM, Chang VW. Being poor and coping with stress: health behaviors and the risk of death. Am J Public Health. 2008;98(5):889–896. doi: 10.2105/AJPH.2007.114454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Dohrenwend BP, Levav I, Shrout PE, et al. Socioeconomic status and psychiatric disorders: the causation-selection issue. Science. 1992;255(5047):946–952. doi: 10.1126/science.1546291. [DOI] [PubMed] [Google Scholar]
- 19.Riolo SA, Nguyen TA, Greden JF, et al. Prevalence of depression by race/ethnicity: findings from the National Health and Nutrition Examination Survey III. Am J Public Health. 2005;95(6):998–1000. doi: 10.2105/AJPH.2004.047225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kessler RC, Berglund P, Demler O, et al. Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the National Comorbidity Survey Replication. Arch Gen Psychiatry. 2005;62(6):593–602. doi: 10.1001/archpsyc.62.6.593. [DOI] [PubMed] [Google Scholar]
- 21.Breslau J, Aguilar-Gaxiola S, Kendler KS, et al. Specifying race-ethnic differences in risk for psychiatric disorder in a USA national sample. Psychol Med. 2006;36(1):57–68. doi: 10.1017/S0033291705006161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Jackson JS. Health and mental health disparities among Black Americans. In: Hager M, editor. Modern Psychiatry: Challenges in Educating Health Professionals to Meet New Needs. New York, NY: Josiah Macy Jr Foundation; 2002. pp. 246–254. [Google Scholar]
- 23.Breslau J, Javaras KN, Blacker D, et al. Differential item functioning between ethnic groups in the epidemiological assessment of depression. J Nerv Ment Dis. 2008;196(4):297–306. doi: 10.1097/NMD.0b013e31816a490e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Williams DR, González HM, Neighbors H, et al. Prevalence and distribution of major depressive disorder in African Americans, Caribbean blacks, and non-Hispanic whites: results from the National Survey of American Life. Arch Gen Psychiatry. 2007;64(3):305–315. doi: 10.1001/archpsyc.64.3.305. [DOI] [PubMed] [Google Scholar]
- 25.Schwartz S, Meyer IH. Mental health disparities research: the impact of within and between group analyses tests of social stress hypotheses. Soc Sci Med. 2010;70(8):1111–1118. doi: 10.1016/j.socscimed.2009.11.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Jackson JS, Knight KM. Race and self-regulatory health behaviors: the role of the stress response and the HPA axis in physical and mental health disparities. In: Schaie KW, Cartensen L, editors. Social Structures, Aging, and Self-Regulation in the Elderly. New York, NY: Springer; 2006. pp. 189–207. [Google Scholar]
- 27.Taylor SE, Aspinwall LG. Mediating and moderating processes in psychosocial stress: appraisal, coping, resistance, and vulnerability. In: Kaplan HB, editor. Psychosocial Stress: Perspectives on Structure, Theory, Life Course and Methods. San Diego, CA: Academic Press; 1996. pp. 71–100. [Google Scholar]
- 28.Gibson JJ. The theory of affordances. In: Shaw R, Bransford J, editors. Perceiving, Acting and Knowing. Hillsdale, NJ: Lawrence Erlbaum Associates; 1977. pp. 67–82. [Google Scholar]
- 29.Avena NM, Rada P, Hoebel BG. Evidence for sugar addiction: behavioral and neurochemical effects of intermittent, excessive sugar intake. Neurosci Biobehav Rev. 2008;32(1):20–39. doi: 10.1016/j.neubiorev.2007.04.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Avena NM. Examining the addictive-like properties of binge eating using an animal model of sugar dependence. Exp Clin Psychopharmacol. 2007;15(5):481–491. doi: 10.1037/1064-1297.15.5.481. [DOI] [PubMed] [Google Scholar]
- 31.Adam TC, Epel ES. Stress, eating and the reward system. Physiol Behav. 2007;91(4):449–458. doi: 10.1016/j.physbeh.2007.04.011. [DOI] [PubMed] [Google Scholar]
- 32.Cottone P, Sabino V, Roberto M, et al. CRP system recruitment mediates dark side of compulsive eating. Proc Natl Acad Sci U S A. 2009;106:20016–20020. doi: 10.1073/pnas.0908789106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Jackson JS, Knight KM, Rafferty JA. Race and unhealthy behaviors: chronic stress, the HPA axis, and physical and mental health disparities over the life course. Am J Public Health. 2010;100(5):933–939. doi: 10.2105/AJPH.2008.143446. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Regier DA, Myers JK, Kramer M, et al. The NIMH Epidemiologic Catchment Area program. Historical context, major objectives, and study population characteristics. Arch Gen Psychiatry. 1984;41(10):934–941. doi: 10.1001/archpsyc.1984.01790210016003. [DOI] [PubMed] [Google Scholar]
- 35.Eaton WW, Kalaydjian A, Scharfstein DO, et al. Prevalence and incidence of depressive disorder: the Baltimore ECA follow-up, 1981-2004. Acta Psychiatr Scand. 2007;116(3):182–188. doi: 10.1111/j.1600-0447.2007.01017.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Helzer JE, Robins LN. The diagnostic interview schedule: its development, evolution, and use. Soc Psychiatry Psychiatr Epidemiol. 1988;23(1):6–16. doi: 10.1007/BF01788437. [DOI] [PubMed] [Google Scholar]
- 37.Eaton WW, Hall AL, MacDonald R, et al. Case identification in psychiatric epidemiology: a review. Int Rev Psychiatry. 2007;19(5):497–507. doi: 10.1080/09540260701564906. [DOI] [PubMed] [Google Scholar]
- 38.Eaton WW, Neufeld K, Chen LS, et al. A comparison of self-report and clinical diagnostic interviews for depression: diagnostic interview schedule and schedules for clinical assessment in neuropsychiatry in the Baltimore epidemiologic catchment area follow-up. Arch Gen Psychiatry. 2000;57(3):217–222. doi: 10.1001/archpsyc.57.3.217. [DOI] [PubMed] [Google Scholar]
- 39.Kendler KS, Myers J, Zisook S. Does bereavement-related major depression differ from major depression associated with other stressful life events? Am J Psychiatry. 2008;165(11):1449–1455. doi: 10.1176/appi.ajp.2008.07111757. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Goldberg DP, Hillier VF. A scaled version of the General Health Questionnaire. Psychol Med. 1979;9(1):139–145. doi: 10.1017/s0033291700021644. [DOI] [PubMed] [Google Scholar]
- 41.Makowska Z, Merecz D, Mościcka A, et al. The validity of general health questionnaires, GHQ-12 and GHQ-28, in mental health studies of working people. Int J Occup Med Environ Health. 2002;15(4):353–362. [PubMed] [Google Scholar]
- 42.Lyketsos CG, Nestadt G, Cwi J, et al. The life chart interview: a standardized method to describe the course of psychopathology. Int J Methods Psychiatr Res. 1994;4:143–155. [Google Scholar]
- 43.Raghunathan TE, Lepkowski JM, VanHoewyk J, et al. A multivariate technique for multiply imputing missing values using a sequence of regression models. Surv Methodol. 2001;27:85–95. [Google Scholar]
- 44.Selvin S. Statistical Analysis of Epidemiologic Data. 3rd ed. New York, NY: Oxford University Press; 2004. [Google Scholar]
- 45.LaVeist TA, Wallace JM., Jr. Health risk and inequitable distribution of liquor stores in African American neighborhood. Soc Sci Med. 2000;51(4):613–617. doi: 10.1016/s0277-9536(00)00004-6. [DOI] [PubMed] [Google Scholar]
- 46.Hackbarth DP, Silvestri B, Cosper W. Tobacco and alcohol billboards in 50 Chicago neighborhoods: market segmentation to sell dangerous products to the poor. J Public Health Policy. 1995;16(2):213–230. [PubMed] [Google Scholar]
- 47.Auchincloss AH, Diez Roux AV, Brown DG, et al. Neighborhood resources of physical activity and healthy foods and their association with insulin resistance. Epidemiology. 2008;19(1):146–157. doi: 10.1097/EDE.0b013e31815c480. [DOI] [PubMed] [Google Scholar]
- 48.Winkleby MA, Cubbin C, Ahn DK, et al. Pathways by which SES and ethnicity influence cardiovascular disease risk factors. Ann N Y Acad Sci. 1999;896:191–209. doi: 10.1111/j.1749-6632.1999.tb08116.x. [DOI] [PubMed] [Google Scholar]
- 49.Williams DR. Socioeconomic differentials in health: a review and redirection. Soc Psychol Q. 1990;53(2):81–99. [Google Scholar]
- 50.Markides KS, Coreil J. The health of Hispanics in the southwestern United States: an epidemiologic paradox. Public Health Rep. 1986;101(3):253–265. [PMC free article] [PubMed] [Google Scholar]