Abstract
To investigate the roles of mutations in enhancer II (Enh II) and basal core promoter (BCP) of hepatitis B virus (HBV) in hepatocellular carcinoma (HCC), we determined the sequence of Enh II/BCP in 152 HCC and 136 non-HCC patients from a high-incidence area of East China. A longitudinal study was conducted on 21 cases in which serial plasma samples were available before HCC. In total, six point mutations, including T1653, V1753, T1762, A1764, T1766 and A1768, were found to occur more frequently in HCC patients. Multivariate analysis showed that the T1653 [odds ratio (OR), 2.07; 95% confidence interval (CI), 1.114–3.845] and V1753 (OR, 3.099; 95% CI, 1.520–6.317) were independent factors that were associated with HCC. Although a T1762/A1764 double mutation was found in 73.0% of the HCC patients and 66.9% of the non-HCC patients, if the combined pattern with other adjacent mutations was not taken into account, it alone showed a lower frequency in HCC patients compared with non-HCC patients (19.7 versus 34.6%, P = 0.005). Interestingly, while the OR of HCC patients with a double mutation was only 0.393 (95% CI, 0.234–0.660), it increased to 1.861 (95% CI, 1.161–2.984) with a triple mutation and to 4.434 (95% CI, 1.630–12.063) with a quadruple mutation. The longitudinal study demonstrated that the mutations in Enh II/BCP accumulated during the development of HCC. In conclusion, the T1653 and V1753 mutations were independent risk factors for HCC in East China. The T1762/A1764 double mutation was necessary but not sufficient to produce an association between Enh II/BCP mutations and HCC.
Introduction
Hepatocellular carcinoma (HCC) is the fifth most common cancer worldwide and the third most common cause of cancer mortality (1). Hepatitis B virus (HBV) infection causes 75–80% of the cases of this type of cancer. Recently, several virological factors have been identified that are associated with a high risk of HCC development. These include HBV DNA levels, HBV genotypes, pre-S deletions and mutations in the pre-S2 start codon, core promoter (CP) and precore regions (2).
HBV is a partially double-stranded DNA virus with four overlapping open reading frames that are under the control of four different promoters. The CP and enhancer II (Enh II) are located in the region that overlaps with the HBV X gene. The CP is composed of the upper regulatory region (nt.1613–1742) and the basal core promoter (BCP, nt.1742–1849) and directs transcription of both pregenomic messenger RNA and precore messenger RNA (3). Enh II is located in nt.1636–1741 and is composed of the boxes α (nt.1646–1668) and β (nt.1704–1715). It stimulates the transcriptional activity of surface, core and X gene promoters (4,5). The most common naturally occurring mutations in BCP are an A to T mutation at 1762 and a G to A mutation at 1764. The T1762/A1764 double mutation was reported to be associated with the severity of hepatitis and the development of HCC (6–13), although this association has not been consistently confirmed by others (14–16). Recently, T1766, A1768 and V1753 in BCP and T1653 in box α of Enh II were found to occur more frequently in HCC patients than in non-HCC patients in Asia (7,17–19). Although the mechanisms whereby Enh II/BCP mutations lead to HCC remain unknown, their association with the increased risk of HCC has been confirmed by a recent meta-analysis (19).
HBV is classified into eight genotypes, A–H, which can be further segregated into subgenotypes based on a >4% (but <8%) difference in the entire nucleotide sequence with distinct ethnic or geographic origin (20). In Asia, genotype C is associated with an increased risk of HCC compared with genotype B (12,14), although these findings have not been supported by other studies (7,21). HBV subgenotypes also seem to influence the outcome of liver diseases (22,23). Because HBV genotype C is more prone to the T1762/A1764 mutation than genotype B (7,9,12), whether the association between genotype C and increased HCC risk is genuine or merely due to the high percentage of BCP mutations in patients with genotype C is an interesting issue. Studies in Hong Kong populations suggest that the BCP double mutant, as opposed to HBV genotype C, is the primary risk factor for HCC (6,7). However, studies in Taiwanese populations indicate that both genotype C and the T1762/A1764 double mutation status are independent risk factors for the development of HCC (12). These controversial results reflect the complex interplay between HBV genotypes and BCP mutations. Thus, a predictive model for HCC that is based on the HBV sequence should be constructed in the context of geographic regions or ethnic groups.
China has one of the world’s highest rates of HCC (24). In some areas, the incidence of HCC can be as high as 70–80 per 100 000 people (25). The high incidence of HCC is usually observed in the eastern and southern coasts of China, where HBV infection has been documented in >90% of HCC cases (26). However, the relationship between Enh II/BCP mutations and HCC risk is largely uncharacterized, especially with regard to the T1653 and V1753 mutations. Thus, we performed a cross-sectional study of 152 HCC patients and 136 non-HCC patients from Shanghai and Qidong (both of which are coastal cities in East China). Furthermore, a longitudinal study was conducted on 21 HCC cases in which plasma samples were serially obtained before and after the occurrence of HCC. We aimed to assess the mutation or mutation profiles which can serve as predictive markers for HCC in East China, where chronic hepatitis and HCC are hyperendemic.
Materials and methods
Patients and samples
We recruited 152 HCC patients and 136 non-HCC patients with HBV infections for the cross-sectional study. Plasma samples were collected at the Qidong Liver Cancer Institute/Qidong Tumor Hospital (110 HCC and 100 non-HCC cases) and at the Shanghai Dahua Hospital (42 HCC and 36 non-HCC cases) between 1990 and 2007. Informed consent was obtained from all patients and the study protocol was approved by the local institution review boards at Shanghai Cancer Institute, Qidong Liver Cancer Institute and Shanghai Dahua Hospital. All of the patients were positive for hepatitis B surface antigen and HBV DNA. The diagnoses of HCC were based on either histological findings or elevated serum contents of α-fetal protein (>400 μg/l), combined with at least one positive image on sonography, computerized tomography and/or nuclear magnetic resonance. According to the current Chinese diagnostic criterion (27), there were 125 chronic hepatitis B patients and 11 inactive carriers in the non-HCC group. Patients with hepatitis C virus infection or cirrhosis were excluded from the study. For the longitudinal study, 21 HCC patients who did or did not have the Enh II/BCP mutations were obtained from a prospective cohort that was started in 1992, which included 852 hepatitis B surface antigen-positive individuals and 786 hepatitis B surface antigen-negative individuals residing in Qidong, Jiangsu Province, China. The plasma samples of each individual were collected annually. For each of the 21 cases, at least one polymerase chain reaction (PCR)-amplifiable DNA sample was available from before the patient was diagnosed with HCC.
Amplification of Enh II/BCP sequence
The HBV DNA was extracted from 100 μl of plasma using a QIAamp DNA blood mini kit (QIAGEN, Hilden, Germany) or from 50 μl of plasma by boiling in 5 μl DNA of extraction buffer (PG Biotech Co., Shenzhen, China) for 10 min. The HBV DNA sequence from nt.1261 to 1796 was amplified by semi-nested PCR using the HB1 [5′-GCCAAGTGTTTGCTGACGC-3′ (nt.1177–1195), forward] and HBV 1796R [5′-CAATTTATGCCTACAGCCTCC-3′ (nt.1796–1776), reverse] primers as first round primers and the HBxF2 [5′-CCGATCCATACTGCGGAACT-3′(nt.1261–1280), forward] and HBV 1796R primers as second round primers. The amplification was carried out in a 50 μl reaction mixture containing 5 μl of 10× buffer, 4 μl of 2.5 mM deoxyribonucleoside triphosphates, 2 μl of 10 μM forward and reverse primers and 1 U Pyrobest DNA polymerase (TaKaRa Bio, Dalian, China). The PCR products were gel-purified and used as the templates for sequencing using the BigDye terminator cycle-sequencing reaction kit and the Prism 3700 DNA analyzer (Applied Biosystems, Foster City, CA). The sequences were compared using the Clustal W program.
HBV genotyping
The HBV genotypes were determined by comparing the sequence of the X gene to standard sequences from the GenBank database. The phylogenetic tree was constructed using MEGA4.1 software.
Quantification of HBV DNA
The HBV DNA copies in plasma samples were quantified by real-time PCR using a commercial kit (PG Biotech Co., Shenzhen, China) according to the manufacturer’s instructions. The detection limit of the kit was 5.0 × 102 copies/ml.
Statistical analysis
The statistical analyses were performed using the chi-square test or the Fisher’s exact test for categorical variables. The Student’s t-test and nonparametric test were used for continuous variables where they were appropriate. Multivariate analyses with logistic regression were used to determine the independent factors that correlated with HCC. All of the tests were two tailed, and a P value of <0.05 was considered to be statistically significant. SPSS (SPSS, Chicago, IL) version 12.0 was used for statistical analysis.
Results
Demographics
The demographic data of the 152 HCC patients and 136 non-HCC patients are listed in Table I. There were no differences in age or male to female ratio between the HCC and non-HCC groups (47.9 ± 11.9 years versus 45.6 ± 11.4 years, P = 0.155 for age; 130:22 versus 122:14, P = 0.284 for male to female ratio). The patients with HCC had significantly higher Hepatitis B e antigen (HBeAg) positivity and fewer copies of HBV DNA than the control patients (P < 0.001). Genotype C was the major type of HBV, accounting for 86.8% of HCC cases and 90.4% of non-HCC cases. There was no difference in genotype distribution between the HCC and non-HCC groups (P > 0.05). All of the genotype C strains isolated from Qidong and Shanghai were of the subgenotype C2, and all of the genotype B strains were of the subgenotype B2.
Table I.
Clinical and virological characteristics of HCC and non-HCC patients
| Characteristic | HCC (n = 152) | Non-HCC (n = 136) | P value |
| Age, mean ± SD | 47.9 ± 11.9 | 45.6 ± 11.4 | Matched |
| Sex, male (%) | 130 (85.5) | 122 (89.7) | Matched |
| ALT (U/L), mean ± SD | 59.9 ± 29.5 | 70.4 ± 66.2 | 0.075 |
| HBeAg positive (%) | 49 (32.2) | 28 (20.6) | 0.026 |
| HBV DNA (log copies/ml), mean ± SD | 3.7 ± 1.0 | 4.4 ± 1.0 | <0.001 |
| Genotype (%) | |||
| B | 17 (11.2) | 9 (6.6) | 0.177 |
| C | 132 (86.8) | 123 (90.4) | 0.338 |
| Others | 3 (2.0) | 4 (2.9) | 0.595 |
| Mutation in box α | |||
| T1653 (%) | 53 (34.9) | 34 (25.0) | 0.069 |
| Mutations in basal core promoter (%) | |||
| V (not T) 1753 | 43 (28.3) | 20 (14.7) | 0.005 |
| T1762 | 114 (75.0) | 92 (67.6) | 0.167 |
| A1764 | 131 (86.2) | 110 (80.9) | 0.224 |
| T1762/A1764 | 111 (73.0) | 91 (66.9) | 0.258 |
| T1766 | 29 (19.1) | 19 (14.0) | 0.246 |
| A1768 | 21 (13.8) | 11 (8.1) | 0.123 |
ALT, alanine aminotransferase.
Relationship between Enh II/BCP mutations and HCC
As listed in Table I, six point mutations in the HBV Enh II/BCP region occurred more frequently in HCC patients, although univariate analysis showed no statistically significant difference in five of them. The V1753 mutation was the only mutation in the Enh II/BCP region that was present at a significantly higher rate in HCC patients than in non-HCC patients (28.3 versus 14.7%, P = 0.005). Most of the V1753 mutations had a T-to-C transition at 1753; in four cases, there were V1753 T-to-A or T-to-G transversions. The T1762/A1764 double mutation was highly prevalent and was present in 70.1% of all of the study subjects. However, there was no correlation between the T1762/A1764 double mutation and clinical manifestations (73.0% in HCC and 66.9% in non-HCC, P > 0.05). In box α, the T1653 mutation was present at a higher frequency in HCC patients compared with non-HCC patients (34.9 versus 25.0%, P = 0.069). Multivariate analysis indicated that the T1653 (OR, 2.07; 95% CI, 1.114–3.845; P = 0.021) and V1753 (OR, 3.099; 95% CI, 1.520–6.317; P = 0.002) mutations were independent factors that were associated with HCC (Table II).
Table II.
Multivariate analysis of variables with independent predictive values for HCC
| Factor | OR (95% CI) | P value |
| Agea | ||
| <46 | 1 | |
| ≥46 | 1.173 (0.678–2.032) | NS |
| Sex | ||
| Female | 1 | |
| Male | 0.898 (0.392–2.054) | NS |
| HBeAg | ||
| Negative | 1 | |
| Positive | 2.565(1.360–4.837) | 0.004 |
| HBV DNA (log copies/ml)a | ||
| <4.0 | 1 | |
| ≥4.0 | 0.273 (0.155–0.482) | < 0.001 |
| HBV genotype | ||
| B | 1 | |
| C | 0.611 (0.297–1.257) | NS |
| T1653 mutation | ||
| Absence | 1 | |
| Presence | 2.07 (1.114–3.845) | 0.021 |
| V (not T)1753 mutation | ||
| Absence | 1 | |
| Presence | 3.099 (1.520–6.317) | 0.002 |
| T1762/A1764 mutation | ||
| Absence | 1 | |
| Presence | 1.475 (0.694–3.135) | NS |
| T1766 mutation | ||
| Absence | 1 | |
| Presence | 1.622 (0.610–4.314) | NS |
| A1768 mutation | ||
| Absence | 1 | |
| Presence | 1.691 (0.615–4.653) | NS |
NS, not significant.
Two groups were divided by each median value.
Complex mutations in the Enh II/BCP region increased the risk of HCC
We previously showed that combined mutations in BCP were associated with the development of HCC (17). In this study, the cumulative effects of Enh II and BCP mutations, including the T1653 and V1753 mutations, on HCC were explored. Double or triple mutations were highly prevalent and were found in 30.2 and 44.8% of the study subjects, respectively. Quadruple mutations were relatively rare and only occurred in 9.4% of the patients. Quintuple or sextuple mutations were not found in any cases. The different patterns of CP mutations are presented in Table III. Surprisingly, without the additional adjacent mutation, the T1762/A1764 double mutation alone was present at a lower frequency in HCC patients compared with non-HCC patients (19.7 versus 34.6%, P = 0.005). On the contrary, the triple and quadruple mutations were more frequent in the HCC group than in the non-HCC group (52.0 versus 36.8%, P = 0.01 for triple mutations and 14.5 versus 3.7%, P = 0.002 for quadruple mutations). The OR of HCC with double, triple or quadruple mutations were 0.393 (95% CI, 0.234–0.660), 1.861 (95% CI, 1.161–2.984) and 4.434 (95% CI, 1.630–12.063), respectively. These data indicate that the number of mutations in Enh II/BCP may be a useful predictive factor for HCC.
Table III.
Mutation patterns of Enh II/BCP in HCC and non-HCC patients
| Type | Pattern |
Total (n = 288), n (%) | HCC (n = 152), n (%) | Non-HCC (n = 136), n (%) | P value | OR (95% CI) | |||||
| T1653 | V1753 | T1762 | A1764 | T1766 | A1768 | ||||||
| Wild type | − | − | − | − | − | − | 37 (12.8) | 17 (11.2) | 20 (14.7) | NS | |
| Single mutation | 8 (2.8) | 2 (1.3) | 6 (4.4) | NS | |||||||
| + | − | – | − | − | − | 6 (2.1) | 1 (0.7) | 5 (3.7) | |||
| − | − | + | − | − | − | 1 (0.3) | 0 (0) | 1 (0.7) | |||
| − | − | − | + | − | − | 1 (0.3) | 1 (0.7) | 0 (0) | |||
| Double mutations | 87 (30.2) | 32 (21.1) | 55 (40.4) | 0.000 | 0.393 (0.234–0.660) | ||||||
| − | − | + | + | − | − | 77 (26.7) | 30 (19.7) | 47 (34.6) | |||
| − | − | − | + | + | − | 10 (3.5) | 2 (1.3) | 8 (5.9) | |||
| Triple mutations | 129 (44.8) | 79 (52.0) | 50 (36.8) | 0.01 | 1.861 (1.161–2.984) | ||||||
| + | − | + | + | − | − | 55 (19.1) | 31 (20.4) | 24 (17.6) | |||
| − | + | + | + | − | − | 47 (16.3) | 30 (19.7) | 17 (12.5) | |||
| + | – | − | + | + | − | 7 (2.4) | 5 (3.3) | 2 (1.5) | |||
| − | + | − | + | + | − | 1 (0.3) | 0 (0) | 1 (0.7) | |||
| − | – | + | + | + | − | 2 (0.7) | 2 (1.3) | 0 (0) | |||
| − | − | + | + | − | + | 4 (1.4) | 3 (2.0) | 1 (0.7) | |||
| − | − | − | + | + | + | 13 (4.5) | 8 (5.3) | 5 (3.7) | |||
| Quadruple mutations | 27 (9.4) | 22 (14.5) | 5 (3.7) | 0.002 | 4.434 (1.630–12.063) | ||||||
| + | + | + | + | − | − | 8 (2.8) | 8 (5.3) | 0 (0) | |||
| + | − | + | + | + | − | 3 (1.0) | 3 (2.0) | 0 (0) | |||
| − | + | + | + | + | − | 1 (0.3) | 1 (0.7) | 0 (0) | |||
| + | − | + | + | − | + | 3 (1.0) | 1 (0.7) | 2 (1.5) | |||
| – | + | + | + | − | + | 1 (0.3) | 1 (0.7) | 0 (0) | |||
| + | − | + | − | + | + | 1 (0.3) | 1 (0.7) | 0 (0) | |||
| − | + | + | − | + | + | 2 (0.7%) | 2 (1.3%) | 0 (0%) | |||
| + | – | – | + | + | + | 4 (1.4) | 3 (2.0) | 1 (0.7) | |||
| − | + | – | + | + | + | 3 (1.0) | 1 (0.7) | 2 (1.5) | |||
| − | − | + | + | + | + | 1 (0.3) | 1 (0.7) | 0 (0) | |||
NS, not significant.
Longitudinal observation of Enh II/BCP mutations during HCC development
We used serial plasma samples that were collected from the prospective cohorts in Qidong to assess the evolution of the Enh II/BCP sequence during the progression of liver disease. Twenty-one cases that harbored either zero, triple or quadruple mutations at the time of HCC diagnosis were included in the longitudinal study. The plasma samples that were collected 2–3 or 5–6 years before HCC diagnosis were retrieved and tested for mutations in Enh II/BCP. There was no sequence information for three cases (487, 405 and 124) at 5–6 years pre-HCC because the plasma samples were not present before the cohort was started. With the progression of liver disease, all of the patients (except patients 049 and 655) showed a gradual accumulation of mutations in Enh II/BCP (Table IV). Patients 049 and 655 did not exhibit any mutations with disease progression. Reverse mutation did occur but only in three cases (405, 527 and 960) at nt.1762 or 1766. Interestingly, the total number of Enh II/BCP mutations never decreased in these three cases due to new mutation events in neighboring mutation hot spots.
Table IV.
Longitudinal observation of HBV Enh II/BCP mutations in patients with HCC
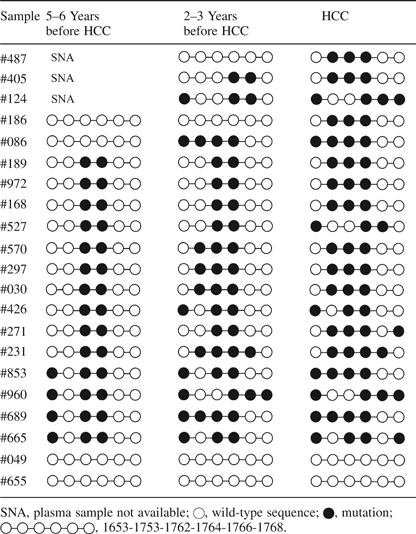 |
The T1762, A1764 and T1653 mutations were detected in the plasma samples that were collected 5–6 years before the diagnosis of HCC. However, the V1753, T1766 and A1768 mutations appeared at 2–3 years before HCC diagnosis. The V1753, T1766 and A1768 mutations occurred after T1762, A1764 or T1653. These data indicate that mutations in Enh II/BCP not only accumulate but also that they accumulate in a certain order: T1762/A1764 mutations appear first, followed by the T1653 mutation and finally, the V1753, T1766 or A1768 mutations, at which point, the patients enter a stage of high risk for HCC development.
Discussion
In this study, we investigated the potential association of mutations in the Enh II/BCP region of the HBV with the development of HCC in patients in East China who are primarily infected with the HBV genotype C2. To our knowledge, this is the largest investigation from mainland China that focuses on the effects of both individual and combined mutations in Enh II/BCP on HCC prognosis. Our results showed that although several mutations, including T1762/A1764, were present at higher frequencies in HCC patients than in non-HCC patients, only the V1753 mutation showed a statistically significant difference (P = 0.005) and only the T1653 mutation exhibited a borderline difference (P = 0.069) by univariate analysis. Multivariate analysis confirmed that the presences of T1653 and V1753 mutations were independent factors that were associated with HCC (OR, 2.07; 95% CI, 1.114–3.845 and OR, 3.099; 95% CI, 1.520–6.317), whereas the T1762/A1764 double mutation was not an independent predictor of HCC.
The clinical implications of the T1653 and V1753 mutations were initially reported in Japanese patients who were infected with genotype C. Takahashi et al. (18) showed that the frequencies of T1653 and/or V1753 mutations were strikingly increased in chronic hepatitis patients (18%) compared with liver cirrhosis and/or HCC patients (82%) in cases where HBeAg was detectable. The higher frequency of T1653 in HCC patients was subsequently confirmed by other investigators in eastern Asia (7,11,28). However, the association between V1753 and HCC was not consistent, according to the data from populations in Japan, Hong Kong and Korea (7,28,29). Compared with the hot spot T1762/A1764 double mutation, the effects of the T1653 and V1753 mutations on the progression of liver disease are less well defined. Thus far, there have only been two studies from mainland China that implicated T1653 and V1753 mutations in HCC development. However, these findings were hampered by small sample sizes. Wang et al. (30) compared the sequences from 47 HCC patients and 132 patients with chronic hepatitis from Guangdong province in southern China and found that both the T1653 and V1753 mutations were independent predictive markers for HCC (P < 0.001). In a study carried out in the same area, Yuan et al. (31) reported that the frequency of the V1753 mutation was increased in eight HCC patients compared with that in 28 patients with chronic hepatitis (62.5 versus 28.6%, respectively). The present case–control study confirmed the observation that the less common T1653 and V1753 mutations, either independently or in combination with the T1762/A1764 double mutation, may serve as predictive factors for HCC.
An interesting novel finding from this study is that, without the complement of other mutations in Enh II/BCP, the T1762/A1764 double mutation itself was less frequent in HCC patients than it was in non-HCC patients (19.7 versus 34.6%, P = 0.005). In contrast to other analyses, our study stratified the Enh II/BCP mutations into a T1762/A1764 alone group and a T1762/A1764 combination group, thus allowing us to demonstrate that the T1762/A1764 double mutation indeed occurred less frequently in HCC patients than it did in non-HCC patients. This does not mean that the mutations at the nucleotide positions 1762 and 1764 had the inhibitory effects on HCC. If all of the complex mutation types were taken into account, the overall frequency of mutations at nt.1762 and 1764 was even slightly higher in the HCC group compared with the non-HCC group (73.0 versus 66.9%, P = 0.258, Table I). The low frequency (19.7%) of the T1762/A1764 double mutation in the HCC group was due to the fact that more HCC cases harbored triple (52.0%) or quadruple (14.5%) mutations on the basis of T1762/A1764. In contrast, the non-HCC group only displayed triple and quadruple mutation rates of 36.8 and 3.7, respectively. These results led us to speculate that the oncogenicity of the T1762/A1764 double mutation itself might not be sufficient to initiate malignancy. However, when one or more mutations were added on top of the double mutation, the risk of HCC significantly increased. The cross-sectional study revealed that while the OR of HCC patients that had double mutations (including T1762/A1764 and A1764/T1766) was only 0.393 (95% CI, 0.234–0.660), it increased to 1.861 (95% CI, 1.161–2.984) with triple mutations and to 4.434 (95% CI, 1.630–12.063) with quadruple mutations. These data are consistent with previous reports that showed that the addition of the T1653 mutation to the existing T1762/A1764 double mutation could significantly increase the risk of HCC (28,29). The cumulative effect of viral mutations on HCC development has also been observed in HBV that contains complex mutations in the pre-S and BCP sequences (32).
The biological impact of the T1762/A1764 double mutation on the life cycle of HBV has been extensively studied. It was generally believed that the T1762/A1764 double mutation could enhance the replication of the viral genome and reduce HBeAg expression (33,34). However, in a recent study, the T1762/A1764 double mutation was not shown to exert an appreciable effect on the replication capacity of the virus, although mutations at positions 1766/1768, 1762/1764/1766 and 1753/1762/1764 exhibited increased replication phenotypes (35). In another independent study, a V1753/T1762/A1764/T1766 mutation was shown to confer a significantly higher rate of viral replication and lower HBeAg expression than the T1762/A1764 mutation alone (36). Thus, CP mutations, in addition to those at positions 1762 and 1764, might have major impacts on viral DNA replication and HBeAg expression. How altered viral replication potentials and HBeAg levels modify the oncogenic properties of HBV is poorly understood. Indeed, unlike the data gathered from cell transfection studies, patients who were infected with triple or quadruple mutant viruses showed a lower viremia level in their blood (data not shown). Similar results were reported previously by Parekh et al. (36). It is well established that the level of viremia declines over the course of HBV infection, especially during the period of cirrhosis and HCC. Whether this is attributable to the accumulation of Enh II/BCP mutations is an interesting issue. Because Enh II/BCP overlaps with the HBV X gene, and the T1653, V1753, T1762, A1764 and A1768 mutations are missense mutations that result in amino acid changes in HBx (H94Y, I127T/N/S, K130M, V131I and F132Y), one cannot rule out the possibility that HBV mutations enhance hepatocarcinogenesis via altered HBx function. HBx is a non-structural protein that has pleiotropic functions in regulating cell death, cell proliferation and transformation. We found that the T1762/A1764/A1768 triple mutation abrogates (∼50%) the colony-inhibitory activity of wild-type HBx (17). Taken together, our data indicate that the accumulation of mutations in Enh II/BCP is likely to have pathological significance and is not an epiphenomenon.
HBV genotypes have been shown to influence the mutation rate of the T1762/A1764 mutation. Patients who were infected with genotype C are more likely to develop the BCP double mutation than those who are infected with genotype B (7,9,12). In the present study, >90% of the patients were infected with genotype C2. Thus, even in non-HCC patients, the T1762/A1764 double mutation rate was as high as 66.9%. Although HCC patients showed a slightly higher incidence of the double mutation (73.0%), there was no statistically significant difference between the groups (P = 0.258). The T1762/A1764 double mutation seemed to have more significant clinical implications in genotype B-infected patients than it did in genotype C-infected patients. Chen et al. (32) reported that the T1762/A1764 mutation was significantly associated with a higher risk of HCC in patients who were infected with genotype B (OR, 3.22; 95% CI, 1.53–6.79; P = 0.002), whereas it was not an independent risk factor in genotype C-infected patients. This genotype-dependent association was also observed by Yuen et al. (6). In the present study, the double mutation had a tendency to be associated with HCC in genotype B-infected patients. In 17 HCC patients who were infected with genotype B virus, 6 (35.3%) contained the T1762/A1764 mutation, whereas in non-HCC patients with genotype B infection, only one (11.1%, P = 0.357) had these mutations (data not shown). The limited number of genotype B cases in this study may obscure the real effect of the double mutation on HCC. It is worth noting that in Taiwan, where genotype B is the predominant type of HBV, the T1762/A1764 double mutation has consistently been reported to be significantly associated with HCC development (9,10,12). However, in areas where genotype C is dominant, the association between the double mutation and HCC is still being debated (14,28,37). The high prevalence of genotype C in our study might explain, at least in part, the weaker association of the double mutation with HCC.
Although the association between the double mutation and HCC was not seen in our study, this does not rule out a role for the T1762/A1764 double mutation in the development of HCC. The results from both the cross-sectional and longitudinal studies reveal that the V1753, T1766 and A1768 mutations did not occur unless the T1762 and A1764 mutations were already present. Although the T1653 mutation could also be an early event during the course of HBV infection (as exhibited in the longitudinal study) the cross-sectional study demonstrated that only 6 of 288 cases (2.1%) had the T1653 mutation in the absence of the T1762 and/or A1764 mutations. Kuang et al. (13) reported that the T1762/A1764 mutation was detectable in patients up to 8 years before the diagnosis of HCC. In another case–control study, a substantially increased risk of HCC development, based on the presence of the double mutation, could already be detected ≥9 years before the diagnosis of HCC (38). These data suggest that the T1762/A1764 mutation might be an early step during HCC development when the less common mutations are absent.
Most of earlier studies that focused on the relationship between BCP mutations and HCC were either cross-sectional studies that were conducted at the time of HCC diagnosis or longitudinal studies that used samples that were taken at the baseline of the cohort. These studies provide little information regarding the evolution of the BCP sequence and the cumulative effects of mutations during the long course of HCC development. Because HBV mutations are usually acquired during the course of chronic infection as opposed to the initial infection, it is critical to know when or at which stage of liver disease, the BCP mutations occurred. This study was made possible by the availability of prospectively collected plasma samples from Qidong, China. The serial samples that were collected before HCC development allowed us to observe, for the first time, the temporal order of Enh II/BCP sequence variations. Apart from the well-known T1762/A1764 mutation, the T1653 mutation in box α of Enh II was also detected in the plasma long before HCC development. Hence, the T1653, T1762 and A1764 mutations may be early predictive markers for HCC, whereas the V1753, T1766 and A1768 mutations seem to be late or immediate markers of HCC development. These two types of mutations may play different roles during different steps of liver carcinogenesis.
Taken together, the T1653 and V1753 mutations were independent risk factors for HCC in patients in East China. This study highlights the importance of studying the cumulative effects of Enh II/BCP mutations on HCC development. It also reveals, for the first time, the temporal order of mutations in Enh II/BCP. A combined examination of these and other mutations might help to predict the progression of liver disease more precisely, thus helping those who are at high-risk of HCC to benefit from early diagnoses and interventions.
Funding
Chinese state key project specialized for infectious diseases (2008ZX10002-015 to H.T.); National Institute of Environmental Health Sciences grant PO I (ES06052 to J.D.G).
Acknowledgments
Conflict of Interest Statement: None declared.
Glossary
Abbreviations
- BCP
basal core promoter
- CI
confidence interval
- CP
core promoter
- Enh II
enhancer II
- HBeAg
hepatitis B e antigen
- HBV
hepatitis B virus
- HCC
hepatocellular carcinoma
- OR
odds ratio
- PCR
polymerase chain reaction
References
- 1.Parkin DM. Global cancer statistics in the year 2000. Lancet Oncol. 2001;2:533–543. doi: 10.1016/S1470-2045(01)00486-7. [DOI] [PubMed] [Google Scholar]
- 2.Lin CL, et al. Hepatitis B viral factors and clinical outcomes of chronic hepatitis B. J. Biomed. Sci. 2008;15:137–145. doi: 10.1007/s11373-007-9225-8. [DOI] [PubMed] [Google Scholar]
- 3.Kramvis A, et al. The core promoter of hepatitis B virus. J. Viral Hepat. 1999;6:415–427. doi: 10.1046/j.1365-2893.1999.00189.x. [DOI] [PubMed] [Google Scholar]
- 4.Yuh CH, et al. The genome of hepatitis B virus contains a second enhancer: cooperation of two elements within this enhancer is required for its function. J. Virol. 1990;64:4281–4287. doi: 10.1128/jvi.64.9.4281-4287.1990. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Yuh CH, et al. Differentiated liver cell specificity of the second enhancer of hepatitis B virus. J. Virol. 1993;67:142–149. doi: 10.1128/jvi.67.1.142-149.1993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Yuen MF, et al. Role of hepatitis B virus genotypes Ba and C, core promoter and precore mutations on hepatocellular carcinoma: a case control study. Carcinogenesis. 2004;25:1593–1598. doi: 10.1093/carcin/bgh172. [DOI] [PubMed] [Google Scholar]
- 7.Yuen MF, et al. Risk for hepatocellular carcinoma with respect to hepatitis B virus genotypes B/C, specific mutations of enhancer II/core promoter/precore regions and HBV DNA levels. Gut. 2008;57:98–102. doi: 10.1136/gut.2007.119859. [DOI] [PubMed] [Google Scholar]
- 8.Baptista M, et al. High prevalence of 1762(T) 1764(A) mutations in the basic core promoter of hepatitis B virus isolated from black Africans with hepatocellular carcinoma compared with asymptomatic carriers. Hepatology. 1999;29:946–953. doi: 10.1002/hep.510290336. [DOI] [PubMed] [Google Scholar]
- 9.Kao JH, et al. Basal core promoter mutations of hepatitis B virus increase the risk of hepatocellular carcinoma in hepatitis B carriers. Gastroenterology. 2003;124:327–334. doi: 10.1053/gast.2003.50053. [DOI] [PubMed] [Google Scholar]
- 10.Liu CJ, et al. Role of hepatitis B virus precore/core promoter mutations and serum viral load on noncirrhotic hepatocellular carcinoma: a case-control study. J. Infect. Dis. 2006;194:594–599. doi: 10.1086/505883. [DOI] [PubMed] [Google Scholar]
- 11.Tanaka Y, et al. Specific mutations in enhancer II/core promoter of hepatitis B virus subgenotypes C1/C2 increase the risk of hepatocellular carcinoma. J. Hepatol. 2006;45:646–653. doi: 10.1016/j.jhep.2006.06.018. [DOI] [PubMed] [Google Scholar]
- 12.Yang HI, et al. Associations between hepatitis B virus genotype and mutants and the risk of hepatocellular carcinoma. J. Natl Cancer Inst. 2008;100:1134–1143. doi: 10.1093/jnci/djn243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kuang SY, et al. Specific mutations of hepatitis B virus in plasma predict liver cancer development. Proc. Natl Acad. Sci. USA. 2004;101:3575–3580. doi: 10.1073/pnas.0308232100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Chan HL, et al. Genotype C hepatitis B virus infection is associated with an increased risk of hepatocellular carcinoma. Gut. 2004;53:1494–1498. doi: 10.1136/gut.2003.033324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Chun YK, et al. No significant correlation exists between core promoter mutations, viral replication, and liver damage in chronic hepatitis B infection. Hepatology. 2000;32:1154–1162. doi: 10.1053/jhep.2000.19623. [DOI] [PubMed] [Google Scholar]
- 16.Chan HL, et al. Hepatitis B e antigen-negative chronic hepatitis B in Hong Kong. Hepatology. 2000;31:763–768. doi: 10.1002/hep.510310330. [DOI] [PubMed] [Google Scholar]
- 17.Guo X, et al. Sequential accumulation of the mutations in core promoter of hepatitis B virus is associated with the development of hepatocellular carcinoma in Qidong, China. J. Hepatol. 2008;49:718–725. doi: 10.1016/j.jhep.2008.06.026. [DOI] [PubMed] [Google Scholar]
- 18.Takahashi K, et al. Clinical implications of mutations C-to-T1653 and T-to-C/A/G1753 of hepatitis B virus genotype C genome in chronic liver disease. Arch. Virol. 1999;144:1299–1308. doi: 10.1007/s007050050588. [DOI] [PubMed] [Google Scholar]
- 19.Liu S, et al. Associations between hepatitis B virus mutations and the risk of hepatocellular carcinoma: a meta-analysis. J. Natl Cancer Inst. 2009;101:1066–1082. doi: 10.1093/jnci/djp180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Pujol FH, et al. Worldwide genetic diversity of HBV genotypes and risk of hepatocellular carcinoma. Cancer Lett. 2009;286:80–88. doi: 10.1016/j.canlet.2009.07.013. [DOI] [PubMed] [Google Scholar]
- 21.Sumi H, et al. Influence of hepatitis B virus genotypes on the progression of chronic type B liver disease. Hepatology. 2003;37:19–26. doi: 10.1053/jhep.2003.50036. [DOI] [PubMed] [Google Scholar]
- 22.Orito E, et al. Differences of hepatocellular carcinoma patients with hepatitis B virus genotypes of Ba, Bj or C in Japan. Intervirology. 2005;48:239–245. doi: 10.1159/000084601. [DOI] [PubMed] [Google Scholar]
- 23.Kao JH, et al. Hepatitis B genotypes correlate with clinical outcomes in patients with chronic hepatitis B. Gastroenterology. 2000;118:554–559. doi: 10.1016/s0016-5085(00)70261-7. [DOI] [PubMed] [Google Scholar]
- 24.Yuen MF, et al. Hepatocellular carcinoma in the Asia pacific region. J. Gastroenterol. Hepatol. 2009;24:346–353. doi: 10.1111/j.1440-1746.2009.05784.x. [DOI] [PubMed] [Google Scholar]
- 25.Chen JG, et al. Trends in the incidence of cancer in Qidong, China, 1978-2002. Int. J. Cancer. 2006;119:1447–1454. doi: 10.1002/ijc.21952. [DOI] [PubMed] [Google Scholar]
- 26.Ming L, et al. Dominant role of hepatitis B virus and cofactor role of aflatoxin in hepatocarcinogenesis in Qidong, China. Hepatology. 2002;36:1214–1220. doi: 10.1053/jhep.2002.36366. [DOI] [PubMed] [Google Scholar]
- 27.Chinese Society of Hepatology, Chinese Medical Association; Chinese Society of Infectious Diseases, Chinese Medical Association (2007) Guideline on prevention and treatment of chronic hepatitis B in China (2005) Chin. Med. J. (Engl.) 2007;120:2159–2173. [PubMed] [Google Scholar]
- 28.Ito K, et al. T1653 mutation in the box alpha increases the risk of hepatocellular carcinoma in patients with chronic hepatitis B virus genotype C infection. Clin. Infect. Dis. 2006;42:1–7. doi: 10.1086/498522. [DOI] [PubMed] [Google Scholar]
- 29.Kim JK, et al. Specific mutations in the enhancer II/core promoter/precore regions of hepatitis B virus subgenotype C2 in Korean patients with hepatocellular carcinoma. J. Med. Virol. 2009;81:1002–1008. doi: 10.1002/jmv.21501. [DOI] [PubMed] [Google Scholar]
- 30.Wang Z, et al. Clinical and virological characteristics of hepatitis B virus subgenotypes Ba, C1, and C2 in China. J. Clin. Microbiol. 2007;45:1491–1496. doi: 10.1128/JCM.02157-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Yuan J, et al. Hepatitis B virus (HBV) genotypes/subgenotypes in China: mutations in core promoter and precore/core and their clinical implications. J. Clin. Virol. 2007;39:87–93. doi: 10.1016/j.jcv.2007.03.005. [DOI] [PubMed] [Google Scholar]
- 32.Chen CH, et al. Combined mutations in pre-s/surface and core promoter/precore regions of hepatitis B virus increase the risk of hepatocellular carcinoma: a case-control study. J. Infect. Dis. 2008;198:1634–1642. doi: 10.1086/592990. [DOI] [PubMed] [Google Scholar]
- 33.Buckwold VE, et al. Effects of a naturally occurring mutation in the hepatitis B virus basal core promoter on precore gene expression and viral replication. J. Virol. 1996;70:5845–5851. doi: 10.1128/jvi.70.9.5845-5851.1996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Moriyama K, et al. Reduced precore transcription and enhanced core-pregenome transcription of hepatitis B virus DNA after replacement of the precore-core promoter with sequences associated with e antigen-seronegative persistent infections. Virology. 1996;226:269–280. doi: 10.1006/viro.1996.0655. [DOI] [PubMed] [Google Scholar]
- 35.Jammeh S, et al. Effect of basal core promoter and pre-core mutations on hepatitis B virus replication. J. Gen. Virol. 2008;89:901–909. doi: 10.1099/vir.0.83468-0. [DOI] [PubMed] [Google Scholar]
- 36.Parekh S, et al. Genome replication, virion secretion, and e antigen expression of naturally occurring hepatitis B virus core promoter mutants. J. Virol. 2003;77:6601–6612. doi: 10.1128/JVI.77.12.6601-6612.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Muroyama R, et al. Nucleotide change of codon 38 in the X gene of hepatitis B virus genotype C is associated with an increased risk of hepatocellular carcinoma. J. Hepatol. 2006;45:805–812. doi: 10.1016/j.jhep.2006.07.025. [DOI] [PubMed] [Google Scholar]
- 38.Chou YC, et al. Temporal relationship between hepatitis B virus enhancer II/basal core promoter sequence variation and risk of hepatocellular carcinoma. Gut. 2008;57:91–97. doi: 10.1136/gut.2006.114066. [DOI] [PubMed] [Google Scholar]


