Abstract
Objective
To investigate the ability of the New Jersey Institute of Technology Robot Assisted Virtual Rehabilitation (NJIT-RAVR) system training to elicit changes in upper extremity (UE) function in children with hemiplegia secondary to cerebral palsy.
Methods
Nine children (mean age 9 years, three males) participated in three pilots. Subjects trained 1 hour, 3 days a week for 3 weeks. Two groups performed this protocol as their only intervention. The third group also performed 5–6 hours of constraint-induced movement therapy.
Results
All subjects participated in a short programme of nine, 60-minute training sessions without adverse effects. As a group, subjects demonstrated statistically significant improvements in Melbourne Assessment of Unilateral Upper Limb Function Test, a composite of three timed UE tasks and several measurements of reaching kinematics. Several subjects demonstrated clinically significant improvements in active shoulder abduction and flexion as well as forearm supination.
Conclusion
Three small pilots of NJIT-RAVR training demonstrated measurable benefit with no complications, warranting further examination.
Keywords: cerebral palsy, hemiplegia, upper extremity, rehabilitation, robotics, virtual reality
Introduction
Cerebral palsy (CP) is the most common cause of physical disability in children, with an incidence of two-to-three per 1000 newborn babies diagnosed each year [1]. It produces non-progressive motor dysfunction and multi-joint incoordination in both upper and lower extremities. An impaired upper extremity (UE) significantly affects self-care activities such as eating, dressing and play [2].
‘Massed practice’ interventions based on motor learning theories emphasize the repetitive practice of goal-oriented tasks designed to address impairments. This treatment approach was initially studied in children with CP by Fetters and Kluzick [3], who found that this approach compared favourably to a traditional neuro-developmental approach. Gordon et al. [4] examined a massed practice intervention utilizing both hands to solve movement problems which demonstrated improvements in measurements of assisting hand behaviours and caregiver ratings of bimanual coordination. Constraint-induced therapy is another massed approach, which combines structured practice with a therapist and unstructured completion of daily tasks with the participation of the involved extremity enforced by restraining the less impaired extremity [5].
Several technology-based approaches to massed practice are being developed. Multiple studies have examined virtual reality (VR) interactive computer games with individuals with stroke and children with CP. The overall findings support that VR systems enhance upper limb rehabilitation and habilitation with both of these populations. It is suggested that the use of continual massed practice combined with the motivational features built into the interactive VR games is contributing to this change [6–9]. Sensory presentations and gaming applications specifically designed to appeal to children can offer variety and entertainment value that cannot be achieved in the context of a traditional clinical atmosphere [10]. Other authors cite VR as a method of achieving expanded practice times for children with motor impairments, fulfilling one of the main tenants of massed practice [11–13]. In addition, exploratory work supporting the ability of VR to target specific neural networks may provide for neuroanatomically-based treatment approaches to the rehabilitation of cerebral palsy in the future [10].
The manipulative ability required to interact with VR systems using hand held controls such as a joystick or computer mouse exceeds that of many children with CP. Hand-held controllers can also limit the size of the excursion used to interact with a simulation, making them less effective for shoulder and elbow training tasks. One method of bypassing this challenge is an approach called video capture. These VR systems utilize cameras to collect position information, allowing participants to use larger body movements to interact with virtual environments (VEs), without hand held controllers [14]. One of the limitations to this approach is the inability to shape or assist desired movement patterns because camera-based systems do not allow for physical interactions between the VE and the subject.
Several studies have attempted to expand the group of persons with CP able to access VR by using robotic systems to interface with simple VEs. Robotic interfaces allow multiple methods to shape movement patterns including the physical human–computer interface, haptically rendered obstacles and global forces such as anti-gravity or damping. Recently, Fasoli et al. [15] described a study in which a group of 5–12 year old children with UE hemiplegia secondary to CP performed 16, 60-minute practice sessions in a simple virtual environment with assist as needed robotic facilitation over an 8-week period. Subjects demonstrated average improvements (percentage change from baseline) of 7.49 (13%) in the Quality of Upper Extremity Test and 8 (42%) in the Upper Extremity Fugl-Meyer Assessment scores, along with anecdotal reports of improved real world use by parents. A similar pilot study is described by Frascarelli et al. [16]. Twelve children with upper extremity motor control impairments due to brain lesions performed 18 1-hour sessions of reaching toward simple targets utilizing guided and unguided movements facilitated by the same robotic system used in the previous study by Fasoliet al. [15]. Subjects averaged a 3.33 point (9%) improvement in UEFMA score and a 6.71 point (12%) improvement in Melbourne Assessment of Unilateral Upper Limb Function score. These improvements in clinical tests were accompanied by 63% improvements in smoothness and 40% improvements in speed of the trajectories measured during reaching training [16]. These studies both utilize simple, stereotyped, planar reaching tasks and require no hand interaction with the robot.
A proof of concept study describing the system discussed in this paper was done with two children with moderate hemiplegia secondary to CP by Qiu et al. [17]. The New Jersey Institute of Technology Robot Assisted Virtual Rehabilitation (NJIT-RAVR) system is an admittance-controlled robotic system, designed to augment the motor abilities of children with proximal UE impairments using more complex, three dimensional movements of the shoulder, elbow and forearm. The robotic system provides haptically rendered obstacles and spatial constraints such as floors and walls which allow for force and tactile feedback not available in other forms of VR. The NJIT-RAVR system allows children to interact with engaging, game-like simulations. One of the key features of the simulations utilized in this study is the purposeful nature of each activity. Participants control a moving car, pilot a space ship, produce silly sounds, hammer pegs, transport objects and blow up moving targets. These activities also offer opportunities to practice more complex sensory processing and motor planning compared to other robotic systems designed for the rehabilitation of children because of the three dimensional work space and the inclusion of three modalities of sensory feedback (auditory, tactile and visual). Multiple authors cite complex, purposeful activity as a pre-requisite for effectiveness in therapeutic activities for children with CP [18, 19].
This paper will present three small pilot studies with children using the NJIT-RAVR System in order to establish that the combination of robotic facilitation of two and three dimensional movements with complex game-like virtual simulations can accomplish the repetition, attention and ecological validity required for effective massed practice. In addition, this study will attempt to demonstrate that a short programme of RAVR training may contribute to improvements in motor function by measuring changes in grip strength, active range of motion, performance on a standardized measure of reaching and object manipulation as well as measurement of reaching kinematics demonstrated by nine children with UE hemiplegia secondary to CP.
Methods
Hardware
A detailed description of the hardware and software used in this study is presented elsewhere [17]; a brief summary follows. The Haptic Master® (Moog, Nieuw-Vennep, The Netherlands) combined with a ring gimbal is a 6° of freedom admittance-controlled (force-controlled) robot. A three-dimensional (3D) force sensor measures the external force exerted by the user on the robot. End-point position and velocity are measured in 3D in real time by the robot. All three movement parameters (force, position and velocity) were used to generate reactive motion. The ring gimbal, when installed as the end effector, records forearm orientation angles and adds the possibility of perturbing forearm rotation. The Haptic Master was programmed to produce haptic effects, such as springs, dampers and constant global forces.
Positioning and splinting
Subjects’ extremities were supported in volar forearm or hand-based positional splints. The hand-based splints allow for free movement of the digits and wrists for subjects with higher levels of motor control and the forearm-based splints allow free movement of the digits and provide more forearm and wrist support. Splints were chosen for each subject by their therapist in order to allow for the highest degree of freedom of movement while minimizing abnormal movement patterns (Figures 1(a) and (b)). During completion of Haptic Master training subjects were secured in a Leckey chair system (Leckey, Dunmurry, Northern Ireland). The height of the Leckey Chair was oriented in relation to the Haptic Master in order to obtain an initial position of 90° of elbow flexion with humerus resting against the participant’s trunk. Foot supports were provided to optimize pelvic stability in an effort to reduce hypertonicity exacerbated by the subject struggling to maintain postural control [20].
Figure 1.
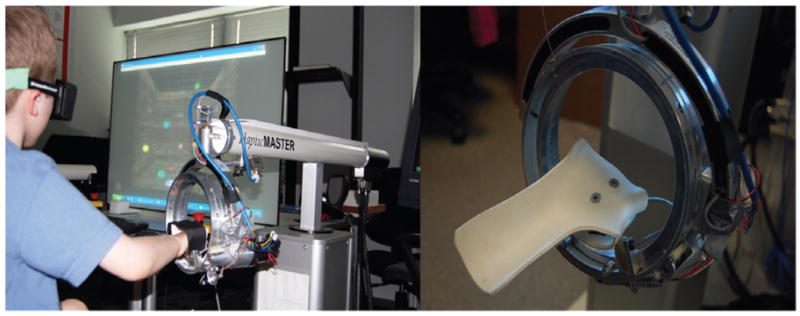
Left panel. Subject seated in chair strapped with chest belt, wearing stereoscopic glasses. Right panel. Volar splint attached to ring gimbal.
Simulations
The Bubble Explosion simulation focuses on improving the speed and accuracy of shoulder and elbow movements during point-to-point reaching movements in 3D space (Figure 2(a)). The participant moves a virtual cursor in order to touch a series of 10 haptically rendered bubbles with 2 cm radii floating in the 3D stereo environment. Stereoscopic glasses are used to enhance depth perception, which increases the sense of immersion and produces more normal UE trajectories. Location of target bubbles are placed in accordance to a pre-defined external configuration file to enable mid-range shoulder flexion/extension, elbow extension/flexion, external and shoulder internal rotation. Target coordinates in the configuration file can be modified based on movement goals.
Figure 2.
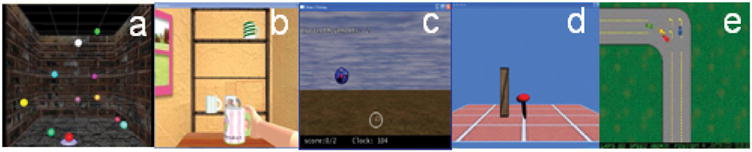
Screen shots from RAVR system simulations: (a) Bubble Explosion, (b) Cup Reach, (c) Falling Objects, (d) Hammer Task, (e) Car Race.
In the Cup Reach simulation the screen displays a 3D room with three haptically rendered shelves and a table (Figure 2(b)). The simulation utilizes a calibration protocol that allows the height, width and distance to the shelves to be adjusted to accommodate the active range of motion of the participant. Haptic obstacles are employed in this simulation to provide feedback, which shapes trajectories performed by the participant. Movements emphasized are similar to those of Bubble Explosion. Resistance supplied by the Haptic Master can be adjusted to simulate a weighted haptic cup, which allows for strengthening. Alternatively, anti-gravity assistance can be supplied by the robot as necessary. A damping effect can be applied by the Haptic Master, which stabilizes the subjects’ movement when issues of tremors or ataxia are a concern.
The purpose of the Falling Objects simulation is to improve UE reaching toward a moving object (Figure 2(c)). Subjects move an avatar to a starting position at the bottom of the screen. A target appears at the top and begins to fall. Subjects are instructed to move the avatar as quickly as possible to touch the target, which explodes on contact. The HammerHM simulation focuses on improving forearm supination (Figure 2(d)). Limited active supination is a common impairment affecting hand function in children with CP [21]. During training, a target (vertically oriented wooden rod) appears in the middle of the screen. With the upper arm stabilized, the subject uses repetitive supination and pronation movements to swing a virtual hammer, driving the target into the ground. The rotation angle required to successfully hammer down the wood is adjustable for different subjects according to their impairment level. The starting rotation angle was often fixed at neutral to enable supination and discourage pronation at the discretion of the supervising therapist. A time bar indicating the time required to complete the task appears at the end of each trial to provide participants with feedback.
The Race Cars simulation combines a pronation/supination movement with a small shoulder and elbow flexion/extension movement (Figure 2(e)). Forearm rotation is used to steer the car and pushing and pulling is used to control acceleration and deceleration. Track configuration (frequency and radius of turns), the amplitude of movement required to effect car movement and the number and speed of competing cars can be adjusted to scale the challenge of the game.
Subjects and training paradigms
Subjects were selected from a convenience sample of children between the ages of 5–18 years of age who had formerly or were currently receiving occupational therapy at Children’s Specialized Hospital. Criteria for inclusion were (1) Diagnosis of hemiplegia secondary to CP, (2) Residual but impaired active movement of the shoulder, elbow and wrist and (3) The ability to tolerate passive shoulder flexion to shoulder level. The criterion for exclusion was a history of visually evoked seizures. Parental consent and child assent was established for each participating child. Subject recruitment and selection, robotic training, CIMT and testing procedures were approved by the Internal Review Board of NJIT. Provisions of the International Code of Medical Ethics of the World Medical Association were satisfied throughout the study. Nine participants formed three groups which will be identified as Study Group One, Study Group Two and Study Group Three. All groups used the NJIT-RAVR System for 1 hour, 3 days a week for 3 weeks and performed pre-testing 3 days prior to RAVR training and post-testing 3 days after RAVR training.
Study group one
Two boys aged 16 and 10 performed a total of 60 minutes of training in all nine sessions. They performed four sets of 10 reaches utilizing the Bubble Explosion simulation to initiate each session for performance testing purposes. Each boy tried each of the other four simulations at least once over the first two sessions and played a combination of two or three of the other simulations depending on their goals, tolerances and preferences for the remainder of each 60 minute session, without a set time schedule or order, other than Bubble Explosion initiating each session. These subjects started the intervention performing their training without trunk restraint or support and utilized a version of the HammerTaskHM simulation that was configured to have subjects transport the virtual hammer to target pegs using shoulder flexion and elbow extension and swing the virtual hammer using a combination of pronation and supination.
Study group two
Three more children, two boys and a girl (aged 12, 6 and 7, respectively) trained as outpatients, utilizing the same testing and training schedules as Study Group 1. All simulations were applied in a fashion similar to that of Group One, except the HammerTaskHM simulation which was reconfigured to emphasize supination and was performed with the arm secured against the subjects’ body eliminating the need to reach for targets. Subjects in Group Two were also secured in the Leckey Chair via a chest strap.
Study group three
The third group was a similar sample of three girls and one boy (aged 5, 6, 12 and 11, respectively) with UE hemiplegia secondary to CP that performed NJIT-RAVR training 1 hour, 3 days a week for the duration of a 3-week camp as part of an intensive training programme that also incorporated a total of 5 hours of intervention including CIMT and intensive bimanual therapeutic interventions. RAVR training was performed using nine 60 minute sessions following the same treatment and testing configuration as Study Group Two. CIMT consisted of participants wearing a light-weight constraint cast on their non-involved arm for 6 hours a day for 3 weeks except for during individual sessions of 30 or 60 minutes per day and during the NJIT-RAVR training.
Outcome measurements
In an attempt to identify changes elicited using a relatively new treatment modality, an array of clinical evaluations was chosen designed to measure and detect changes in motor function across a variety of domains. Impairment level change was measured at the proximal effectors using active range of motion (AROM) and distal effectors were evaluated using grip and pinch dynamometry. Functional use of the entire extremity was evaluated using a standardized functional assessment and an observational rating scale. Finally, motor control change was assessed using kinematic measurements of one of the reaching simulations performed by subjects during training.
All clinical measurements were performed 1 day prior to training and 1 day after training was completed for subjects from all three groups. The same licensed/registered Occupational Therapist performed both sets of clinical tests using the same equipment for all three groups. Active range of motion was obtained for the effected UE including the shoulder, elbow and forearm using standard procedures [22]. Measurement of active vs passive measurement and the same evaluator for pre- and post-testing were utilized to maximize the reability and validity of these measurements [23]. Improvement in UE AROM of motion is associated with increases in UE function [24]. Grip strength and pinch strength were assessed with hand-held dynamometers using procedures developed by Mathiowetz et al. [25]. This approach to strength measurement has excellent reliability [25] and has literature supporting its validity in predicting disability [26], motor function and disease severity in children with CP [27]. Upper extremity movement quality was measured using the Melbourne Assessment of Unilateral Upper Limb Function (MAUULF), a battery of 16 activities designed for children with upper extremity hemiplegia [28]. Each activity is rated on a 3-, 4- or 5-point scale with all 16 activities summed to achieve a raw score. The raw score is divided by the total possible score to produce a percentage score [28, 29]. Intra-rater reliability of this battery is reported to be high [28]. Higher scores on the MAUULF are correlated with higher scores in several domains of the Pediatric Disability Inventory [29]. Three sub-tests of the Melbourne were timed in order to provide an additional variable that is currently not assessed with this outcome measure and to capture accuracy of movement. The timing of the task was scored by video review. During the video review the timing was initiated at ‘Go’ and was terminated at the completion of the task. Therapists who participated in the study were giving instruction for the timing portion of the test to ensure consistency. Subjects were assigned a score on the Functional Level of Hemiplegia scale, an observational description of hemiplegic UE use in children with CP [30, 31] (see Appendix).
Reaching movement duration was measured and averaged daily, using data collected by the robot during the Bubble Explosion activity. This simulation was chosen for kinematic measurement because it is performed in a three dimensional space, providing for more effective generalization of these measurements to real world reaching performance. Smoothness of end-point trajectory during performance of the same activity was evaluated by integrating the third derivative of the trajectory length. This numerically describes the ability to produce smooth, coordinated, gross reaching movements vs disjointed collections of sub-movements [32, 33]. The average length of the trajectory utilized to perform the 10 reaching movements was recorded each day as well. Ronnqvist and Rosblad [34] found longer reaching path lengths in children with hemiplegic CP than typically-developing children. Reaching trajectory length, smoothness and duration were described as sensitive to changes in impairment achieved secondary to a programme of reaching activities in children with CP [35].
Subjects’ responses were evaluated via therapist report each session. Therapists determined if a subject showed fatigue during a simulation. An observation checklist with guidelines for fatigue and attention were completed by the observing therapists during each session. The attention to the task was noted as the amount of time that the child was actively engaged in the activity. Breaks in attention were recorded if the child offered complaints about the activity, a desire to do something else or demonstrated intermittent participation in the activity. Fatigue was described as verbal report by the child, physical signs of fatigue, discontinuing the activity, fidgeting in the chair, noted decreased ability or effort to continue the task or requiring more verbal cuing to continue the task. Time to fatigue and time to break in attention demonstrated verbally or non-verbally as described were recorded.
Statistical analyses
Preliminary inspection of the results confirmed normal distribution of the Melbourne test scores and of the kinematic data collected by the robot. Statistical significance for pre- to post-training changes in Melbourne scores were evaluated using paired, two tailed t-tests. Analysis of variance (ANOVA) with repeated measures factors Time (Pre-, Post-) and Item (Forward Reach, Sideways Reach and Hand to Mouth and Down) was calculated for the three timed sub-tests of the Melbourne. Statistical significance for pre- to post-test changes were evaluated using paired, two tailed t-tests. Results were considered statistically significant at p <0.05.
Results
Study group one
The attending Occupational Therapists noted that subjects were utilizing compensatory movements of the trunk to complete shoulder and elbow movements during training. This is consistent with experimental observations made by Levin et al. [36]. A harness system (Leckey Seating System) was applied to decrease trunk rotation and lateral flexion, resulting in an increase in shoulder and elbow movement [37]. The HammerHM simulation configured to train pronation/supination movements in the context of unsupported, three dimensional reaching proved to be extremely difficult for both subjects and did not elicit the supination movements which were the primary goal of this simulation. Therapists and engineers programmed the RAVR system to limit pronation and eliminate elbow flexion and extension, utilizing only supination movements to interact with the simulation. In addition, a forearm-based splint that controlled wrist flexion and extension as well as radial and ulnar deviation was attached to the robot gimbal to emphasize supination movements as well.
Clinical tests
Table I summarizes Melbourne data which are scored and reported as percentages of the maximum possible score, for the nine subjects. The children from Group Three demonstrated similar mean improvement on the Melbourne score compared to the Group Two subjects (6.5 and 6.2, respectively). Two children making changes in Melbourne score that exceed the minimal detectable change established for this instrument (>8.9%) [38] were in Group Three and one in Group Two. The two subjects from Group One did not show a substantial improvement.
Table I.
Melbourne scores.
| MAUULF (%) |
Forward reach time (s) |
Reach sideways time (s) |
Hand to mouth time (s) |
Composite time (s) |
|||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Pre | Post | Diff | Pre | Post | Diff | Pre | Post | Diff | Pre | Post | Diff | Pre | Post | Diff | |
| Group 1 S1 | 40.2 | 42.6 | 2.4 | 1.9 | 1.2 | −0.7 | u | 1.4 | na | u | u | 1.9 | 1.2 | −0.7 | |
| Group 1 S2 | 74.6 | 75.4 | 0.8 | 3.6 | 2.9 | −0.7 | 3.7 | 2.3 | −1.4 | 15.1 | 10.7 | −4.4 | 22.4 | 15.9 | −6.5 |
| Group 1 Mean | 57.4 | 59.0 | 1.6 | 2.8 | 2.1 | −0.7 | 3.7 | 1.9 | −1.9 | 15.1 | 10.7 | −4.4 | 12.2 | 8.6 | −3.6 |
| Group 2 S3 | 59.8 | 67.2 | 7.4 | 2.9 | 1.5 | −1.4 | 2.2 | 0.8 | −1.4 | 5.4 | 4.6 | −0.8 | 10.5 | 6.9 | −3.6 |
| Group 2 S4 | 76.2 | 77.1 | 0.9 | 4.5 | 1.5 | −3.0 | 2.4 | 1.8 | −0.6 | 2.2 | 1.6 | −0.6 | 9.1 | 4.9 | −4.2 |
| Group 2 S5 | 68.2 | 78.6 | 10.4 | 1.2 | 0.5 | −0.7 | 1.3 | 0.5 | −0.8 | 7.3 | 2.9 | −4.4 | 9.8 | 3.8 | −6.0 |
| Group 2 Mean | 68.1 | 74.3 | 6.2 | 2.9 | 1.2 | −1.7 | 2.0 | 1.0 | −0.9 | 5.0 | 3.0 | −1.9 | 9.8 | 5.2 | −4.6 |
| Group 3 S6 | 53.4 | 50.8 | −2.6 | 2.0 | 1.8 | −0.2 | 1.7 | 1.8 | 0.1 | 4.7 | 1.7 | −3.0 | 8.4 | 5.3 | −3.1 |
| Group 3 S7 | 41.8 | 54.1 | 12.3 | 3.2 | 3.9 | 0.7 | 3.6 | 1.6 | −2.0 | 6.6 | 1.5 | −5.1 | 13.4 | 7.0 | −6.4 |
| Group 3 S8 | 52.5 | 61.5 | 9.0 | 3.0 | 1.6 | −1.4 | 4.3 | 3.1 | −1.2 | 3.4 | 5.5 | 2.1 | 10.7 | 10.2 | −0.5 |
| Group 3 S9 | 79.5 | 86.9 | 7.4 | 1.7 | 1.2 | −0.5 | 1.7 | 1.1 | −0.6 | 2.8 | 1.8 | −1.0 | 6.2 | 4.1 | −2.1 |
| Group 3 Mean | 56.8 | 63.3 | 6.5 | 2.5 | 2.1 | −0.4 | 2.8 | 1.9 | −0.9 | 4.4 | 2.6 | −1.7 | 9.7 | 6.7 | −3.0 |
| Grand Mean | 60.7 | 66.0 | 5.3** | 2.7 | 1.8 | −0.9* | 2.6 | 1.6 | −1.0** | 5.9 | 3.8 | −2.2* | 10.3 | 6.6 | −3.7** |
| Grand SD | 14.8 | 14.8 | 5.1 | 1.1 | 1.0 | 1.0 | 1.1 | 0.8 | 0.6 | 4.1 | 3.2 | 2.5 | 5.6 | 4.3 | 2.3 |
p <0.05;
p <0.001.
Diff =Difference; u =unable.
Table I also summarizes performance on the three timed items of the Melbourne. Only one subject in Group One could perform the timed Sideways Reach and Hand to Mouth tests. This boy demonstrated large improvements (1.4 and 4.4 seconds, respectively) when compared to the average changes accomplished by Group Two (1.9 and 0.9 seconds) and Group Three (1.7 and 0.9 seconds) for these items. Group Two achieved the largest improvements in the timed Forward Reach item as well as the composite of the three scores, with average changes of 1.7 and 4.6 seconds, respectively, as compared to Group Two (0.7 and 3.6 seconds) and Group Three (0.4 and 3.0 seconds).
Table II describes changes in active range of motion from pre- to post-testing for the three Group Two subjects and the four Group Three subjects. S3 and S5 made modest improvements in shoulder flexion AROM and S5 made the largest magnitude change in supination AROM. Interestingly, S3 made the largest improvements in grip and pinch strength during the study despite the absence of a distal training component for Study Group 2’s intervention. Subjects S6, S7 and S8 from Group Three made substantial improvements in shoulder, elbow and forearm AROM but smaller improvements in wrist extension AROM, grip and pinch dynamometry. Table II also describes changes in the Functional Levels of Hemiplegia test. All three Group Two subjects improved one level. Two of the Group Three children also improved, one a single level and one made a three level improvement.
Table II.
Active range of motion (in degrees), grip dynamometry (kg) and functional levels of hemiplegia measurements pre- and post-training.
| Subject | Shoulder Abd |
Shoulder Flex |
Elbow Ext |
Supination |
Wrist Ext |
Grip |
Pinch |
FLH |
||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Pre | Post | Diff | Pre | Post | Diff | Pre | Post | Diff | Pre | Post | Diff | Pre | Post | Diff | Pre | Post | Diff | Pre | Post | Diff | Pre | Post | Diff | |
| Group 2 S1 | 150 | 150 | 0 | 130 | 145 | 15 | wnl | wnl | na | 75 | 65 | −10 | 45 | 55 | 10 | 6 | 14 | 8 | 3 | 7 | 4 | 6 | 7 | 1 |
| Group 2 S2 | 150 | 155 | 5 | 150 | 145 | −5 | wnl | wnl | na | −60 | −10 | 50 | 60 | 65 | 5 | 3 | 3 | 0 | 3 | 4 | 1 | 4 | 5 | 1 |
| Group 2 S3 | 96 | 100 | 4 | 94 | 110 | 16 | wnl | wnl | na | 66 | 76 | 10 | 8 | 12 | 4 | nt | nt | nt | nt | nt | nt | 5 | 6 | 1 |
| Group 2 Mean | 3 | 9 | na | 17 | 6 | 4 | 3 | 1 | ||||||||||||||||
| Group 3 S4 | 135 | 135 | 0 | 135 | 140 | 5 | wnl | wnl | na | 75 | 60 | −15 | 0 | 49 | 49 | 5 | 8 | 3 | 3.6 | 4 | 0.4 | 5 | 5 | 0 |
| Group 3 S5 | 110 | 125 | 5 | 105 | 135 | 30 | −25 | −20 | 5 | 10 | 35 | 25 | 0 | 0 | 0 | 12 | 14 | 2 | 0 | 0 | 0 | 3 | 2 | 1 |
| Group 3 S6 | 105 | 160 | 5 | 120 | 135 | 15 | −20 | −10 | 10 | 45 | 55 | 10 | 0 | 0 | 0 | 4.3 | 4.6 | 0.3 | 2.6 | 1.6 | −1 | 1 | 4 | 3 |
| Group 3 S7 | 145 | 150 | 5 | 140 | 135 | −5 | −20 | −15 | 5 | 65 | 70 | 10 | 50 | 50 | 0 | 27 | 35 | 0.3 | 10 | 11 | −1 | 7 | 7 | 0 |
| Group 3 Mean | 19 | 11 | 7 | 8 | 12 | 1 | 0 | 1 | ||||||||||||||||
| Grand Mean | 12 | 10** | 7 | 11 | 10 | 2** | 1 | 1 | ||||||||||||||||
| Grand SD | 20 | 13 | 3 | 22 | 18 | 3 | 2 | 1 | ||||||||||||||||
p <0.05;
p <0.001.
Abd =Abduction, Flex =Flexion, Ext =Extension, FLH =Functional Level of Hemiplegia, wnl =within normal limits, nt =not tested, Diff =Difference.
Movement kinematics
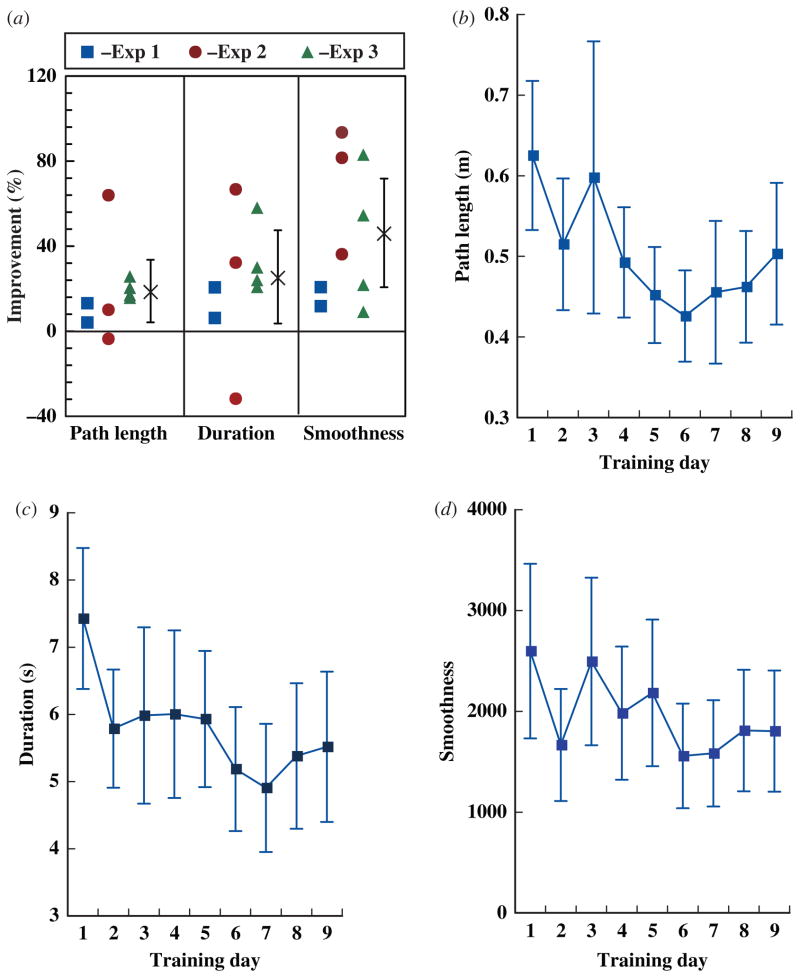
Figure 3 summarizes improvements in robotically collected kinematics during the performance of Bubble Explosion. The percentage changes described in Figure 3 compare the means of hundreds of measurements collected for each subject during training on the first and last days of training, justifying the reporting of percentages in this situation despite the small sample sizes. The three study groups are presented separately in Figure 3(a) and as a nine subject group in the balance of Figure 3. This simulation was applied in a similar fashion for all three groups, justifying group reporting. All subjects improved in movement speed, trajectory smoothness and efficiency. Subjects S4 and S5 from Group Two made the largest improvements in all three measures, with more moderate changes demonstrated by Group Three subjects and minimal changes demonstrated by Group One subjects. Movement time decreased for the nine subject group by 26%. This change was statistically significant (t =2.69, p =0.028). The improvement in hand trajectory smoothness by 46% was not significant (t =4.2, p =0.067). This change was skewed by a single negative score for one subject who had considerable difficulty on her last training day secondary to a change in her schedule. This analysis reached statistical significance (t =3.06, p =0.016) using the next to last training day’s data for this subject. Path length decreased significantly by 19% (t =2.96, p =0.003). The other three panels in this figure show the daily averages for each of these measurements. All three measurements demonstrate trends toward improvement with some day-to-day fluctuations.
Figure 3.
(a) Percentage improvements from baseline in trajectory length, duration and smoothness for four sets of 10 reaching movements performed using the Bubble Explosion simulation on the first and final training days. Squares denote subjects from the Group 1 study, circles from Group 2, triangles from Group 3 and crosses the mean for all nine subjects. Error bars show the 95% confidence interval. (b) Average length of path; required to complete a set of 10 targets during performance of the Bubble Explosion simulation for each training day. (c) Average time to complete a set of 10 targets; (d) Average smoothness of hand trajectory; Error bars indicate standard error.
Response to simulations
As a nine subject group, the children averaged a total of 24 minutes of time on task during the 60-minute training sessions. Table III summarizes the average time subjects participated in each simulation when it was utilized and reports the relative frequencies of decreased attention or signs of fatigue demonstrated by subjects during training. There was no consistent correlation between training time and fatigue or attention issues.
Table III.
Participation time, attention and fatigue issue frequencies.
| Falling objects | Bubble explosion | Car race | Hammer | Placing cups | |
|---|---|---|---|---|---|
| Time (SD), s | 6.62 (3.2) | 8.49 (3.48) | 5.88 (3.37) | 3.93 (2.44) | 5.47 (2.42) |
| Attention* | 11/56 | 8/81 | 0/70 | 8/18 | 0/27 |
| Fatigue* | 18/56 | 29/81 | 22/70 | 18/18 | 14/27 |
issue noted during performance of simulation/total number of performances of simulation.
Discussion
This paper describes the first system combining complex, haptically rendered, three dimensional virtual environments and robotics to train the UE of children with CP. All of the subjects in this study utilized the NJIT-RAVR system without adverse reactions or complications. No seizure activity or symptoms associated with cyber sickness were noted [39]. This system, which was initially designed to accommodate persons with strokes [40, 41], was easily re-fitted and modified to allow for interaction with children. During the first pilot study, a need was identified to increase emphasis on active supination. This was accomplished by decreasing the complexity of the HammerHM simulation and using longer splints to interface between robot and participants. This resulted in significant increases in active supination, achieved by these subjects during training, which carried over into improvements in active range of motion during post-testing.
The Melbourne Assessment of Unilateral Upper Limb Function Test, the main functional outcome measure used in this study, utilizes observational ratings of motor performance and motor control. This is common to other standardized measurements of UE function for children. This study has attempted to extend the observational approach by timing three activities from the Melbourne. When pooling these times, as is done to interpret other batteries designed for adults, the group of nine subjects demonstrated statistically significant improvements. It is felt that development of a more comprehensive battery of timed, standardized UE movements would significantly contribute to the paediatric rehabilitation literature.
To test for improvements in distal function, two tests of finger strength, grip and pinch dynamometry were incorporated. As would be expected, Group Three made the largest improvements in grip and pinch strength, most likely due to the extensive distal effector interactions involved in the CIMT portion of the Group Three protocol. Interestingly, Group One and Group Two also made positive changes. Similar improvements of smaller magnitude in distal function in response to proximal UE robotic training have been described in the adult stroke literature [42].
Analyses of robotically collected kinematics revealed that all subjects made the largest magnitude improvement from day 1 to day 2 which is similar to the pattern demonstrated in response to robotic UE training by the adult subjects with hemiparesis due to stroke [40]. These analyses show improvements in performance combined with decreased variance in performance, trends consistent with improvements in motor control [43]. Fluctuations could be related in part to the small sample size and day-to-day variations in attention and motivation, which are typical in young children.
Average time on task for the 60 minute sessions was ~24 minutes as measured by the computer system, for the children participating in this study. The 24 minutes described exceeds the time on task reported in the adult stroke literature for treatments of comparable length [44]. A similar study quantifying participation intensities during traditional out-patient or inpatient rehabilitation activities in a population of children with CP is indicated to establish the effectiveness of technologies designed to enhance rehabilitation experiences.
Limitations of this study which reduce one’s ability to generalize the results to a broader population include the small sample size and the lack of measurements of out of the clinic function. Over the next few years the authors plan to examine this training approach in a larger group of children using an expanded battery of timed tasks, a validated activities of daily living scale and 24-hour upper extremity activity monitoring.
Two specific aspects of training support the RAVR systems ability to affect improvements in motor function. It is interesting to note that two children with significantly impaired active supination range of motion, a common impairment for children with hemiplegia secondary to CP [21], made large improvements in this construct. The NJIT-RAVR is unique as a robotic system specifically designed to train this movement in persons with hemiplegia. Arm elevation accomplished with shoulder and elbow musculature was another construct stressed during the RAVR training trials described. The children participating in this trial demonstrated improved performance by these effectors across measurements of AROM, UE motor function, reaching kinematics and motor control. While subjects’ responses to the games varied, they performed each simulation while maintaining attention sufficient to improve in both robotic task performance and measures of motor function. It is felt that this approach to training has demonstrated measurable benefit with minimal complications, warranting further examination and discussion.
Appendix.
Functional levels of hemiplegia
| Class | Ability | |
|---|---|---|
| 0 | Does not use | Does not use |
| 1 | Poor Passive Assist | Uses as stabilizing weight only |
| 2 | Fair Passive Assist | Can hold objects placed in hand |
| 3 | Good Passive Assist | Can hold object and stabilize for use in other hand |
| 4 | Poor Active Assist | Can actively grasp object and hold it weakly |
| 5 | Fair Active Assist | Can actively grasp object and stabilize well |
| 6 | Good Active Assist | Can actively grasp object and manipulate it against other hand |
| 7 | Incomplete Spontaneous | Can perform bimanual activities easily and occasionally uses the hand spontaneously |
| 8 | Spontaneous Use-Complete | Uses the hand completely independently |
Acknowledgments
We would like to thank Janelle Lenzo-Werner, MOT, OTR, Regina Freeman, OTR, Susan M. Shannon, MSOT, OTR, Nichole M. Turmelle, OTR, and George Fuller and the administration, staff and participants at Children’s Specialized Hospital.
Footnotes
Declaration of interest: Supported in part by the Rehabilitation Engineering Research Center grant # H133E050011 from the National Institute on Disability and Rehabilitation Research, and by grant HD58301 from the National Institute of Child Health and Human Development. The authors report no conflicts of interest. The authors alone are responsible for the content and writing of the paper.
References
- 1.Morris C. Definition and classification of cerebral palsy: A historical perspective. Developmental Medicine and Child Neurology Supplement. 2007;109:3–7. doi: 10.1111/j.1469-8749.2007.tb12609.x. [DOI] [PubMed] [Google Scholar]
- 2.Reid D. The influence of virtual reality on playfulness in children with cerebral palsy: A pilot study. Occupational Therapy International. 2004;11:131–144. doi: 10.1002/oti.202. [DOI] [PubMed] [Google Scholar]
- 3.Fetters L, Kluzik J. The effects of neurodevelopmental treatment versus practice on the reaching of children with spastic cerebral palsy. Physical Therapy. 1996;76:346–358. doi: 10.1093/ptj/76.4.346. [DOI] [PubMed] [Google Scholar]
- 4.Gordon AM, Schneider JA, Chinnan A, Charles JR. Efficacy of a hand-arm bimanual intensive therapy (HABIT) in children with hemiplegic cerebral palsy: A randomized control trial. Developmental Medicine and Child Neurology. 2007;49:830–838. doi: 10.1111/j.1469-8749.2007.00830.x. [DOI] [PubMed] [Google Scholar]
- 5.Hoare BJ, Wasiak J, Imms C, Carey L. Constraint-induced movement therapy in the treatment of the upper limb in children with hemiplegic cerebral palsy. Cochrane Database of Systematic Reviews. 2007;2:CD004149. doi: 10.1002/14651858.CD004149.pub2. [DOI] [PubMed] [Google Scholar]
- 6.Wille D, Eng K, Holper L, Chevrier E, Hauser Y, Kiper D, Pyk P, Schlegel S, Meyer-Heim A. Virtual reality-based paediatric interactive therapy system (PITS) for improvement of arm and hand function in children with motor impairment–a pilot study. Developmental Neurorehabilitation. 2009;12:44–52. doi: 10.1080/17518420902773117. [DOI] [PubMed] [Google Scholar]
- 7.Chen YP, Kang LJ, Chuang TY, Doong JL, Lee SJ, Tsai MW, Jeng SF, Sung WH. Use of virtual reality to improve upper-extremity control in children with cerebral palsy: A single-subject design. Physical Therapy. 2007;87:1441–1457. doi: 10.2522/ptj.20060062. [DOI] [PubMed] [Google Scholar]
- 8.Sveistrup H. Motor rehabilitation using virtual reality. Journal of Neuroengineering and Rehabilitation. 2004;1:10. doi: 10.1186/1743-0003-1-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Snider L, Majnemer A, Darsaklis V. Virtual reality as a therapeutic modality for children with cerebral palsy. Developmental Neurorehabilitation. 2010;13:120–128. doi: 10.3109/17518420903357753. [DOI] [PubMed] [Google Scholar]
- 10.Adamovich SV, Fluet GG, Tunik E, Merians AS. Sensorimotor training in virtual reality: A review. NeuroRehabilitation. 2009;25:29–44. doi: 10.3233/NRE-2009-0497. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Rizzo A, Kim G. A SWOT analysis of the field of virtual reality rehabilitation and therapy. Presence. 2005;14:1–28. [Google Scholar]
- 12.Reid DT. Benefits of a virtual play rehabilitation environment for children with cerebral palsy on perceptions of self-efficacy: A pilot study. Pediatric Rehabilitation. 2002;5:141–148. doi: 10.1080/1363849021000039344. [DOI] [PubMed] [Google Scholar]
- 13.Parsons TD, Rizzo AA, Rogers S, York P. Virtual reality in paediatric rehabilitation: A review. Developmental Neurorehabilitation. 2009;12:224–238. doi: 10.1080/17518420902991719. [DOI] [PubMed] [Google Scholar]
- 14.Weiss PL, Rand D, Katz N, Kizony R. Video capture virtual reality as a flexible and effective rehabilitation tool. Journal of Neuroengineering and Rehabilitation. 2004;1:12. doi: 10.1186/1743-0003-1-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Fasoli SE, Fragala-Pinkham M, Hughes R, Krebs HI, Hogan N, Stein J. Robotic therapy and botulinum toxin type A: A novel intervention approach for cerebral palsy. American Journal of Physical Medicine and Rehabilitation. 2008;7:89–97. doi: 10.1097/PHM.0b013e31817fb346. [DOI] [PubMed] [Google Scholar]
- 16.Frascarelli F, Masia L, Di Rosa G, Cappa P, Petrarca M, Castelli E, Krebs HI. The impact of robotic rehabilitation in children with acquired or congenital movement disorders. European Journal of Physical and Rehabilitation Medicine. 2009;45:135–141. [PubMed] [Google Scholar]
- 17.Qiu Q, Ramirez DA, Saleh S, Fluet GG, Parikh HD, Kelly D, Adamovich SV. The New Jersey Institute of Technology Robot-Assisted Virtual Rehabilitation (NJIT-RAVR) system for children with cerebral palsy: A feasibility study. Journal of Neuroengineering and Rehabilitation. 2009;6:40. doi: 10.1186/1743-0003-6-40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Valvano J. Activity-focused motor interventions for children with neurological conditions. Physical and Occupational Therapy in Pediatrics. 2004;24:79–107. doi: 10.1300/j006v24n01_04. [DOI] [PubMed] [Google Scholar]
- 19.Volman MJ, Wijnroks A, Vermeer A. Effect of task context on reaching performance in children with spastic hemiparesis. Clinical Rehabilitation. 2002;16:684–692. doi: 10.1191/0269215502cr540oa. [DOI] [PubMed] [Google Scholar]
- 20.Trefler E, Taylor SJ. Prescription and positioning: Evaluating the physically disabled individual for wheelchair seating. Prosthetics and Orthotics International. 1991;15:217–224. doi: 10.3109/03093649109164291. [DOI] [PubMed] [Google Scholar]
- 21.Sakellarides HT, Mital MA, Lenzi WD. Treatment of prona-tion contractures of the forearm in cerebral palsy by changing the insertion of the pronator radii teres. Journal of Bone and Joint Surgery American. 1981;63:645–652. [PubMed] [Google Scholar]
- 22.Norkin CC, White DJ. Measurement of joint motion: a guide to goniometry. Philadelphia, PA: F A Davis Company; 2003. [Google Scholar]
- 23.Gajdosik RL, Bohannon RW. Clinical measurement of range of motion. Review of goniometry emphasizing reliability and validity. Physical Therapy. 1987;67:1867–1872. doi: 10.1093/ptj/67.12.1867. [DOI] [PubMed] [Google Scholar]
- 24.Bartlett DJ, Palisano RJ. Physical therapists’ perceptions of factors influencing the acquisition of motor abilities of children with cerebral palsy: Implications for clinical reasoning. Physical Therapy. 2002;82:237–248. [PubMed] [Google Scholar]
- 25.Mathiowetz V, Weber K, Volland G, Kashman N. Reliability and validity of grip and pinch strength evaluations. Journal of Hand Surgery American. 1984;9:222–226. doi: 10.1016/s0363-5023(84)80146-x. [DOI] [PubMed] [Google Scholar]
- 26.Arnould C, Penta M, Thonnard JL. Hand impairments and their relationship with manual ability in children with cerebral palsy. Journal of Rehabilitation Medicine. 2007;39:708–714. doi: 10.2340/16151977-0111. [DOI] [PubMed] [Google Scholar]
- 27.Gordon AM, Duff SV. Relation between clinical measures and fine manipulative control in children with hemiplegic cerebral palsy. Developmental Medicine and Child Neurology. 1999;41:586–591. doi: 10.1017/s0012162299001231. [DOI] [PubMed] [Google Scholar]
- 28.Randall M, Carlin JB, Chondros P, Reddihough D. Reliability of the Melbourne assessment of unilateral upper limb function. Developmental Medicine and Child Neurology. 2001;43:761–767. doi: 10.1017/s0012162201001396. [DOI] [PubMed] [Google Scholar]
- 29.Bourke-Taylor H. Melbourne Assessment of Unilateral Upper Limb Function: Construct validity and correlation with the Pediatric Evaluation of Disability Inventory. Developmental Medicine and Child Neurology. 2003;45:92–96. [PubMed] [Google Scholar]
- 30.Romain M, Benaim C, Allieu Y, Pelissier J, Chammas M. Assessment of hand after brain damage with the aim of functional surgery. Annales de Chirurgie de la Main et du Membre Superieur. 1999;18:28–37. doi: 10.1016/s0753-9053(99)80054-4. [DOI] [PubMed] [Google Scholar]
- 31.House JH, Gwathmey FW, Fidler MO. A dynamic approach to the thumb-in palm deformity in cerebral palsy. Journal of Bone and Joint Surgery American. 1981;63:216–225. [PubMed] [Google Scholar]
- 32.Tresilian JR, Stelmach GE, Adler CH. Stability of reach-to-grasp movement patterns in Parkinson’s disease. Brain. 1997;120:2093–2111. doi: 10.1093/brain/120.11.2093. [DOI] [PubMed] [Google Scholar]
- 33.Adamovich SV, Berkinblit MB, Hening W, Sage J, Poizner H. The interaction of visual and proprioceptive inputs in pointing to actual and remembered targets in Parkinson’s disease. Neuroscience. 2001;104:1027–1041. doi: 10.1016/s0306-4522(01)00099-9. [DOI] [PubMed] [Google Scholar]
- 34.Ronnqvist L, Rosblad B. Kinematic analysis of unimanual reaching and grasping movements in children with hemiplegic cerebral palsy. Clinical Biomechanics. 2007;22:165–175. doi: 10.1016/j.clinbiomech.2006.09.004. [DOI] [PubMed] [Google Scholar]
- 35.Kluzick J, Fetters L, Coryell J. Quantification of control: A preliminary study of effects of neurodevelopmental treatment on reaching in children with spastic cerebral palsy. Physical Therapy. 1990;70:65–76. doi: 10.1093/ptj/70.2.65. [DOI] [PubMed] [Google Scholar]
- 36.Levin MF, Cirstea CM, Archambault P, Son F, Roby-Brami A. Impairment and compensation of reaching in patients with stroke and cerebral palsy. In: Latash M, editor. Progress in motor control, structure-function relations in voluntary movements. Vol. 2. Champaign, Illinois: Human Kinetics; 2002. pp. 103–123. [Google Scholar]
- 37.Michaelsen SM, Levin MF. Short-term effects of practice with trunk restraint on reaching movements in patients with chronic stroke: A controlled trial. Stroke. 2004;35:1914–1919. doi: 10.1161/01.STR.0000132569.33572.75. [DOI] [PubMed] [Google Scholar]
- 38.Klingels K, De Cock P, Desloovere K, Huenaerts C, Molenaers G, Van Nuland I, Huysmans A, Feys H. Comparison of the Melbourne Assessment of Unilateral Upper Limb Function and the Quality of Upper Extremity Skills Test in hemiplegic CP. Developmental Medicine and Child Neurology. 2008;50:904–909. doi: 10.1111/j.1469-8749.2008.03123.x. [DOI] [PubMed] [Google Scholar]
- 39.Kiryu T, So RH. Sensation of presence and cybersickness in applications of virtual reality for advanced rehabilitation. Journal of Neuroengineering and Rehabilitation. 2007;4:34. doi: 10.1186/1743-0003-4-34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Adamovich SV, Fluet GG, Merians AS, Mathai A, Qiu Q. Incorporating haptic effects into three-dimensional virtual environments to train the hemiparetic upper extremity. IEEE Transactions on Neural Systems and Rehabilitation Engineering. 2009;17:512–520. doi: 10.1109/TNSRE.2009.2028830. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Adamovich SV, Fluet GG, Mathai A, Qiu Q, Lewis J, Merians AS. Design of a complex virtual reality simulation to train finger motion for persons with hemiparesis: A proof of concept study. Journal of Neuroengineering and Rehabilitation. 2009;6:28. doi: 10.1186/1743-0003-6-28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Krebs HI, Mernoff S, Fasoli SE, Hughes R, Stein J, Hogan N. A comparison of functional and impairment-based robotic training in severe to moderate chronic stroke: A pilot study. NeuroRehabilitation. 2008;23:81–87. [PMC free article] [PubMed] [Google Scholar]
- 43.Magill RA. Motor learning and control. 8. Boston, MA: McGraw-Hill; 2006. [Google Scholar]
- 44.Lang C, Macdonald J, Gnip C. Counting repetitions: An observational study of outpatient therapy for people with hemiparesis post-stroke. Journal of Neurologic Physical Therapy. 2007;31:3–11. doi: 10.1097/01.npt.0000260568.31746.34. [DOI] [PubMed] [Google Scholar]