Abstract
Objectives: Patients in underdeveloped countries may be left behind by advances in telehealthcare. We surveyed chronically ill patients with low incomes in Honduras to measure their use of mobile technologies and willingness to participate in mobile disease management support. Materials and Methods: 624 chronically ill primary care patients in Honduras were surveyed. We examined variation in telephone access across groups defined by patients' sociodemographic characteristics, diagnoses, and access to care. Logistic regression was used to identify independent correlates of patients' interest in automated telephonic support for disease management. Results: Participants had limited education (mean 4.8 years), and 65% were unemployed. Eighty-four percent had telephone access, and 78% had cell phones. Most respondents had voicemail (61%) and text messaging (58%). Mobile technologies were particularly common among patients who had to forego clinic visits and medications due to cost concerns (each p < 0.05). Most patients (>80%) reported that they would be willing to receive automated calls focused on appointment reminders, medication adherence, health status monitoring, and self-care education. Patients were more likely to be willing to participate in automated telemedicine services if they had to cancel a clinic appointment due to transportation problems or forego medication due to cost pressures. Conclusions: Even in this poor region of Honduras, most chronically ill patients have access to mobile technology, and most are willing to participate in automated telephone disease management support. Given barriers to in-person care, new models of mobile healthcare should be developed for chronically ill patients in developing countries.
Key words: telehealth, telemedicine, home health monitoring
Chronically ill patients with low incomes in Honduras were studied concerning the use of mobile technologies and willingness to participate in mobile disease management support. Logistic regression was used to identify independent correlates. Although participants had limited education and 65% were unemployed, 84% had telephone access, and 78% had cell phones with most having voicemail (61%) and text messaging (58%). Most patients (>80%) reported that they would be willing to receive automated calls focused on appointment reminders, medication adherence, health status monitoring, and self-care education.
Introduction
Sixty percent of all deaths worldwide are due to chronic diseases, and 80% of those deaths occur in low- to middle-income countries.1–3 According to the World Health Organization, 2010 marks a turning point in which cardiovascular diseases will become the leading cause of death in the developing world.2 Diabetes alone represents an international public health crisis, with a global prevalence in 2030 of 439 million people compared to 285 million people today.4
Latin America faces all of the challenges that make this epidemic of chronic disease difficult, including social strains from high unemployment, inadequate public health infrastructures, and low levels of community awareness.5 A report from the Inter-American Development Bank6 found that most Central and South-American countries allocate fewer resources to healthcare than required and are not using those resources effectively, typically spending only $500 per person per year and relying heavily on out-of-pocket payments. An aging population, migration to urban centers, and the ubiquitous presence of fast food all have caused chronic cardiovascular disease rates to skyrocket. Over the next 10 years, deaths from chronic diseases will increase by 17%, with diabetes rates increasing by 80%.4,7
Ongoing, proactive monitoring and self-management support are essential for effective chronic illness care.8,9 Unfortunately, most health systems in the United States still have not found ways to provide those services given resource constraints, and access barriers are far worse in less developed countries.
Patient-centered information technologies represent a potential tool for increasing both the quality and quantity of chronic disease management support in the developing world.10–14 Mobile telephone technology holds particular promise for bringing health assessment, education, and other services to patients between in-person encounters.15,16 Overall, mobile phone penetration in Latin America and the Caribbean is close to 80%, markedly higher than the world average of 58%. Nearly half a billion people in the region (including 360 million living on less than $300 per month) have cell phones, and that number is growing rapidly.17 In Colombia, 85% of all citizens have a cell phone, with an absolute increase from 2 million users in 1999 to 42 million 10 years later.18 In other Latin American countries, there are now more telephones than residents.19 Mobile healthcare interventions are particularly attractive in Latin America because in many areas a person can receive a mobile phone call without a monthly subscription to a calling plan or paying any minute charges. As a result, patients have less financial disincentive to respond to health outreach calls than patients in the United States.
The potential of mobile healthcare in Latin American has been recognized by national governments, large private funders driving social policy such as the Bill and Melinda Gates Foundation, and international groups such as the World Health Organization.14,20 However, a recent survey of decision makers across Latin America found that most felt that program development in this area was inadequate.21 The Inter-American Development Bank (the largest lender in the region) recently launched the “Mobile Citizen” program, which is designed to spur innovation in new uses of these technologies, by bringing together leaders in the region with international experts and potential sources of technical assistance and sustainable funding.6
Despite these trends, an emphasis on mobile health technology could leave behind some of the most vulnerable patients. In particular, communities with a high prevalence of chronic diseases, low levels of educational attainment, and high unemployment may have significantly lower telephone penetration rates. Available data suggest substantial variability in telephone access across Latin American countries, with rates significantly lower in nations such as El Salvador or Honduras that have some of the weakest economies. According to a World Information Society Report,17 rates of mobile phone use in Honduras doubled between 2004 and 2005, however, at that time less than 30% of the population had mobile phone access. Data on mobile communication access across population groups defined by chronic diseases or socioeconomic correlates have not been published. Automated telephone calls have been shown to be an effective adjunct to chronic illness care in the United States.22–25 However, the receptivity of patients in less developed countries to this technology is unknown.
Between June and August 2009, we surveyed a large sample of chronically ill adults within two primary care centers of North Central Honduras. One of the goals of that survey was to identify the potential feasibility of mobile healthcare programs for chronic disease management. Patients reported their access to mobile communication tools such as cell phones and text messaging, as well as their willingness to participate in various forms of telehealth support for chronic disease management that would take advantage of automated patient calls. Here, we report the results of that survey overall, and describe variation in the potential viability of telehealth services cross subgroups defined by patients' sociodemographic and clinical characteristics.
Methods
Recruitment
The study was a cross-sectional survey of an outpatient population with chronic illnesses. Participants were identified at the time of a primary care visit to one of two primary care centers in Santa Cruz de Yojoa, Honduras; additional participants living in the immediate area were surveyed in their homes. To be eligible, respondents had to be greater than 18 years of age and report that they had been told by a doctor that they had one of the following chronic health problems: cardiovascular disease (either a prior infarction or heart disease), cancer, pulmonary disease (bronchitis or asthma), hypertension, high cholesterol, diabetes, liver disease, HIV, tuberculosis, depression, or arthritis. All respondents completed a written informed consent. The study was approved by a university human subjects committee as well as the Honduran medical centers' leadership.
Measures
The survey was developed in English and then translated and back translated to Spanish using multiple bilingual staff (both native Spanish speakers and native English speakers). Respondents reported their age, gender, and educational attainment using categories developed for a prior survey of chronically ill patients in Honduras.26 Questions about patients' access to cell phones, landline phones, voicemail, and text messaging were developed specifically for this study. Respondents also were asked: “Would you be willing to receive telephone messages previously recorded by a clinician to … ” as a prompt about the following services: “remind you about upcoming appointments,” “give you advice about your use of medications,” “help your physicians monitor your symptoms,” and “give you information about your diseases and how you can manage your self-care better.” For the current study, we examined the number of respondents who answered “yes,” who would be willing to participate in each service type, versus those who responded either “no” or “unsure.”
Additional questions asked about transportation problems and cost-related barriers to care. To measure transportation barriers, patients were first asked how long they had to travel to reach their usual source of outpatient care. For analyses presented here, we created a binary indicator of whether patients traveled more than an hour to reach the clinic (yes vs. no). Patients also were asked: “In the past year did you ever cancel a clinic appointment because you did not have transportation” (yes vs. no). To measure cost-related access barriers, patients were asked: “In the past year, did you ever avoid visiting a hospital or clinic because you were worried about the cost?” “Did you avoid buying medication that you needed because you were worried about the cost?” And “Did you ever take less medication than you were prescribed because of the cost?” Patients who responded affirmatively to either of the two medication cost questions were considered to have medication cost barriers.
Analysis
Initial analyses used chi-square statistics to examine bivariate differences across genders and levels of educational attainment in respondents' other sociodemographic and clinical characteristics. We then examined variation across sociodemographic and clinical groups in the proportion of respondents with access to various telecommunication technologies and their willingness to receive telephone-based support for their disease management. Finally, we used multivariate logistic models to identify the independent correlates of participants' willingness to participate in automated telephone support for disease management. Each multivariate model included as covariates those factors found to be at least marginally associated (p < 0.10) in bivariate analysis with patients' willingness to participate in that service.
Results
Respondent Characteristics
A total of 624 patients completed the survey. Overall, 61% of respondents were women, 21% had no more than a primary school education (mean 4.8 years), and 65% were unemployed (Table 1). The average age of respondents was 51.2 years, with 24% age 60 or older, and 18% over age 70. On average, participants reported 2.3 chronic health problems, including diabetes (23%), pulmonary disease (24%), hypertension (32%), depression (23%), arthritis (21%), and cardiovascular disease (11%). Patients with pulmonary disease, hypertension, depression, and arthritis were more likely to be women and to have less formal education (all p < 0.05).
Table 1.
Description of the Sample
| |
Gender % |
Education % |
Total N (%) |
|||
|---|---|---|---|---|---|---|
| |
Male |
Female |
Primary |
Secondary |
>Secondary |
|
| N = 624 | 38.8 | 61.2 | 21.3 | 52.7 | 26.0 | 624 (100.0) |
|
Demographics | ||||||
| Age in years | ||||||
| <50 |
41.0 |
59.0 |
6.3 |
51.0 |
42.7 |
288 (46.2) |
| 50–59 |
36.5 |
63.5 |
18.1 |
66.1 |
15.8 |
127 (20.4) |
| 60–69 |
29.5 |
70.5 |
34.0 |
52.6 |
13.4 |
97 (15.5) |
| 70+ |
43.9 |
56.1 |
52.7 |
42.0 |
5.4 |
112 (18.0) |
| Female |
— |
— |
|
|
|
|
| No |
— |
— |
21.1 |
51.5 |
27.4 |
242 (38.8) |
| Yes |
— |
— |
21.7 |
53.7 |
24.6 |
382 (61.2) |
| Education | ||||||
| Primary |
38.2 |
61.8 |
— |
— |
— |
|
| Secondary |
37.8 |
62.2 |
— |
— |
— |
|
| >Secondary |
41.4 |
58.6 |
— |
— |
— |
|
| Employeda,b | ||||||
| No |
21.8 |
78.2 |
26.4 |
54.9 |
18.7 |
406 (65.1) |
| Yes |
70.8 |
29.3 |
11.9 |
48.6 |
39.5 |
218 (34.9) |
|
Perceived healtha,b | ||||||
| Good/V. good/Ex |
48.9 |
51.2 |
13.7 |
48.0 |
38.3 |
175 (28.0) |
| Fair/poor |
34.8 |
65.2 |
24.3 |
54.6 |
21.2 |
449 (72.0) |
|
Chronic diseases | ||||||
| Diabetes | ||||||
| No |
38.7 |
61.3 |
22.8 |
50.3 |
26.2 |
484 (77.5) |
| Yes |
39.4 |
60.6 |
16.4 |
60.7 |
22.9 |
140 (22.5) |
| Pulmonarya,b | ||||||
| No |
42.0 |
58.0 |
19.0 |
52.1 |
26.9 |
473 (75.8) |
| Yes |
28.6 |
71.4 |
28.5 |
48.3 |
23.2 |
151 (24.2) |
| Hypertensiona,b | ||||||
| No |
42.5 |
57.6 |
20.9 |
48.7 |
30.4 |
427 (68.4) |
| Yes |
30.9 |
69.1 |
22.5 |
60.7 |
16.8 |
197 (31.6) |
| High cholesterol | ||||||
| No |
39.3 |
60.7 |
21.1 |
51.6 |
27.3 |
489 (78.3) |
| Yes |
37.1 |
62.9 |
22.2 |
56.3 |
21.5 |
135 (21.7) |
| Depressiona,b | ||||||
| No |
44.0 |
56.0 |
22.5 |
48.2 |
29.3 |
472 (75.6) |
| Yes |
23.2 |
76.8 |
17.8 |
66.5 |
15.8 |
134 (21.4) |
| Arthritisa,b | ||||||
| No |
41.6 |
58.4 |
19.2 |
51.3 |
29.5 |
490 (78.6) |
| Yes |
28.2 |
71.8 |
28.6 |
57.9 |
13.5 |
134 (21.4) |
| Cardiovascular disease | ||||||
| No |
38.3 |
61.7 |
20.6 |
52.7 |
26.7 |
555 (88.9) |
| Yes |
43.3 |
56.7 |
27.5 |
52.2 |
20.3 |
69 (11.1) |
|
Access barriers | ||||||
| Transportation problem | ||||||
| No |
44.1 |
55.9 |
19.4 |
47.8 |
32.9 |
356 (57.1) |
| Yes |
31.8 |
68.2 |
23.9 |
59.3 |
16.8 |
268 (42.9) |
| >1 h travel time | ||||||
| No |
37.2 |
62.9 |
19.8 |
53.7 |
26.5 |
510 (81.7) |
| Yes |
46.0 |
54.0 |
28.1 |
48.3 |
23.7 |
114 (18.3) |
| Medication CRNa,b | ||||||
| No |
44.6 |
55.4 |
15.7 |
46.1 |
38.3 |
230 (36.9) |
| Yes |
35.4 |
64.6 |
24.6 |
56.6 |
18.8 |
394 (63.1) |
| Outpatient visit CRNb | ||||||
| No |
42.0 |
58.0 |
17.1 |
51.4 |
31.4 |
350 (56.1) |
| Yes | 34.6 | 65.4 | 26.6 | 54.4 | 19.0 | 274 (43.9) |
Significant differences in the gender distribution (p < 0.05).
Significant differences in the distribution across education levels (p < 0.05).
CRN, cost-related nonadherence.
Note: Cell entries are row percentages.
Telephone Access
Despite their generally low incomes and limited educational attainment, most respondents had access to mobile technologies (Table 2). Overall, 78.2% of all respondents reported having a cell phone, 27.2% reported having a landline, and 83.8% reported having one or the other phone types. The majority of all respondents reported having access to voicemail (60.5%) and text messaging services (58%). Among respondents with a cell phone, 82% reported that their phone was in service all or most of the time.
Table 2.
Access to Telephone Technology Among Chronically Ill Patients in Honduras
| N = 624 | Cell Phone | Any Phone | Voicemail | Text Messaging |
|---|---|---|---|---|
|
Total |
78.2 |
83.8 |
60.5 |
58.0 |
|
Demographics | ||||
| Age in yearsa–d | ||||
| <50 |
87.2 |
91.7 |
61.5 |
66.0 |
| 50–59 |
81.0 |
86.6 |
59.1 |
56.7 |
| 60–69 |
79.4 |
82.5 |
59.8 |
57.7 |
| 70+ |
50.9 |
61.6 |
42.9 |
39.3 |
| Female | ||||
| No |
80.0 |
84.8 |
54.6 |
55.4 |
| Yes |
76.0 |
81.4 |
61.6 |
61.2 |
| Educationa–d | ||||
| Primary |
58.7 |
63.2 |
41.4 |
36.8 |
| Secondary |
81.2 |
87.5 |
64.7 |
62.6 |
| >Secondary |
88.3 |
93.2 |
55.6 |
66.1 |
| Employeda–d | ||||
| No |
74.4 |
81.5 |
53.0 |
52.7 |
| Yes |
85.3 |
88.1 |
65.6 |
67.9 |
|
Perceived health statusa–d | ||||
| Good/V. Good/Ex. |
83.4 |
89.1 |
66.3 |
65.7 |
| Fair/poor |
76.2 |
81.7 |
53.9 |
55.0 |
|
Chronic diseases | ||||
| Diabetesb | ||||
| No |
76.6 |
82.2 |
57.7 |
57.6 |
| Yes |
83.6 |
89.3 |
55.7 |
59.3 |
| Pulmonarya–d | ||||
| No |
80.3 |
85.4 |
60.3 |
61.3 |
| Yes |
71.5 |
77.5 |
48.3 |
47.7 |
| Hypertensionc | ||||
| No |
76.5 |
81.9 |
52.2 |
53.2 |
| Yes |
81.6 |
87.8 |
68.4 |
68.4 |
| High cholesterolc | ||||
| No |
77.1 |
83.2 |
54.7 |
56.2 |
| Yes |
82.2 |
85.9 |
66.7 |
64.4 |
| Depressionc,d | ||||
| No |
78.6 |
84.5 |
54.8 |
55.6 |
| Yes |
77.0 |
81.6 |
65.1 |
65.1 |
| Arthritisa,b | ||||
| No |
80.4 |
86.1 |
57.7 |
59.1 |
| Yes |
69.9 |
75.2 |
56.4 |
54.1 |
| Cardiovascular diseaseb | ||||
| No |
79.6 |
84.8 |
57.8 |
57.9 |
| Yes |
66.7 |
75.4 |
53.6 |
58.0 |
|
Access barriers | ||||
| Transportation problemc,d | ||||
| No |
76.1 |
82.3 |
48.6 |
54.2 |
| Yes |
81.0 |
85.8 |
69.0 |
63.1 |
| >1 h travel timeb,c | ||||
| No |
79.4 |
85.3 |
59.2 |
59.6 |
| Yes |
72.8 |
77.2 |
49.1 |
50.9 |
| Medication CRNc,d | ||||
| No |
74.4 |
80.4 |
40.4 |
48.3 |
| Yes |
80.6 |
85.8 |
67.3 |
63.7 |
| Outpatient visit CRNa–c | ||||
| No |
75.1 |
81.1 |
52.6 |
57.7 |
| Yes | 82.1 | 87.2 | 63.5 | 58.4 |
Significant differences in the number of patients with cell phones (p < 0.05).
Significant differences in the number of patients with any phone (p < 0.05).
Significant differences in the number of patients with voicemail (p < 0.05).
Significant differences in the number of patients with text messaging (p < 0.05).
Note: Cell entries are row percentages.
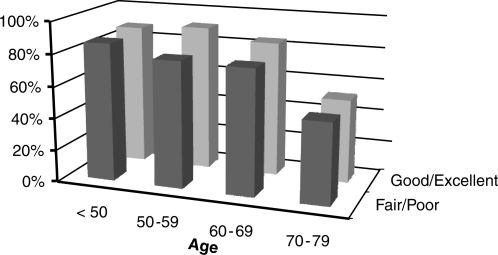
Telephone access was more common among individuals under age 70, although there was little variation across age groups below that cutoff. Seventy-nine percent of respondents between the ages of 61 and 70 reported having a cell phone, and the majority of this group also reported voicemail and text messaging services. Cell phone services were common across groups defined by patients' educational attainment and employment status (Table 2 and Fig. 1). However, cell phone features such as voicemail and text messaging were reported by less than half of respondents with at most a primary school education. Unemployed respondents were less likely to have telephone access, although even in this group >81% still reported having either a cell phone or landline.
Fig. 1.
Proportion of respondents with cell phones, by age and perceived health status.
Telephone access varied across groups defined by respondents' chronic diseases and access to care. Patients were less likely to have a cell phone if they had pulmonary disease or arthritis. Patients who reported having to cancel an outpatient appointment due to transportation problems were more likely than other patients to report access to voicemail (69% vs. 49%) and text messaging (63% vs. 54%; both p < 0.05). Patients who reported underuse of medications due to cost pressures also were more likely than other patients to report voicemail access (67% vs. 40%) and text messaging (64% vs. 48%).
Willingness to Participation in Automated Telephone Messaging as Part of a Self-Management Support Program
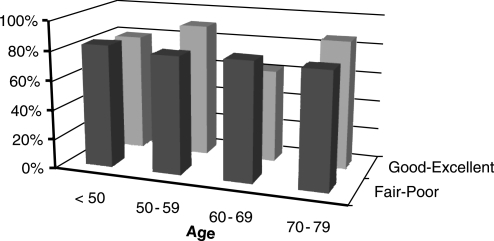
In general, the majority of respondents were willing to use automated messages as part of a telehealth service designed to improve their chronic illness care (Table 3 and Fig. 2). Eighty-eight percent of respondents reported that they would be willing to receive automated telephone reminders about upcoming appointments, 83.2% were willing to receive information about medication adherence, 79.5% were willing to receive automated health status monitoring for their symptoms and self-care needs, and 81.1% were willing to participate in automated self-management education.
Table 3.
Interest in Chronic Illness Self-Management Support from Automated Telephone Calls
| N = 624 | ATC Appointment Reminders | ATC Adherence Support | ATC Health Monitoring | ATC Self-Care Education |
|---|---|---|---|---|
|
Total |
88.5 |
83.2 |
79.5 |
81.1 |
|
Demographics | ||||
| Age in years | ||||
| <50 |
86.5 |
82.6 |
80.2 |
82.3 |
| 50–59 |
90.6 |
85.8 |
79.5 |
81.9 |
| 60–69 |
78.4 |
81.4 |
76.3 |
77.3 |
| 70+ |
85.7 |
83.0 |
80.4 |
80.4 |
| Female | ||||
| No |
84.5 |
81.8 |
78.1 |
80.0 |
| Yes |
87.8 |
84.8 |
81.0 |
82.3 |
| Educationb–d | ||||
| Primary |
85.0 |
80.5 |
75.3 |
77.4 |
| Secondary |
87.8 |
86.7 |
83.6 |
85.7 |
| >Secondary |
83.3 |
78.4 |
74.7 |
74.7 |
| Employeda,b | ||||
| No |
83.3 |
80.8 |
77.8 |
79.1 |
| Yes |
90.8 |
87.6 |
82.6 |
84.9 |
|
Perceived health | ||||
| Good/V. Good/Ex |
84.6 |
82.3 |
78.3 |
80.6 |
| Fair/Poor |
86.4 |
83.5 |
79.0 |
81.3 |
|
Chronic diseases | ||||
| Diabetes | ||||
| No |
85.9 |
82.1 |
80.1 |
81.2 |
| Yes |
85.7 |
86.4 |
77.1 |
80.7 |
| Pulmonaryd | ||||
| No |
86.3 |
84.8 |
80.3 |
82.9 |
| Yes |
84.8 |
78.2 |
76.8 |
75.5 |
| Hypertensiona–d | ||||
| No |
83.8 |
79.8 |
75.5 |
76.5 |
| Yes |
90.8 |
90.8 |
88.3 |
91.3 |
| Cholesterol | ||||
| No |
86.5 |
82.8 |
78.5 |
80.5 |
| Yes |
83.7 |
84.4 |
83.0 |
83.0 |
| Depressiond | ||||
| No |
85.1 |
82.0 |
78.1 |
79.2 |
| Yes |
88.2 |
86.8 |
83.6 |
86.8 |
| Arthritis | ||||
| No |
85.9 |
82.6 |
78.0 |
80.8 |
| Yes |
85.7 |
85.0 |
77.4 |
82.0 |
| Cardiovascular disease | ||||
| No |
86.1 |
82.7 |
79.4 |
81.2 |
| Yes |
84.1 |
87.0 |
79.7 |
79.7 |
|
Access barriers | ||||
| Transportation problema–d | ||||
| No |
82.0 |
77.5 |
73.3 |
75.3 |
| Yes |
91.0 |
90.7 |
87.7 |
88.8 |
| >1 h travel time | ||||
| No |
86.1 |
83.9 |
80.2 |
82.0 |
| Yes |
85.1 |
79.8 |
76.3 |
77.2 |
| Medication CRNa–d | ||||
| No |
78.3 |
72.2 |
66.1 |
69.6 |
| Yes |
90.4 |
89.6 |
87.3 |
87.8 |
| Outpatient visit CRNa,c,d | ||||
| No |
83.4 |
80.7 |
75.1 |
78.0 |
| Yes | 89.0 | 86.1 | 85.0 | 85.0 |
Significant differences in the number of patients willing to participate in ATC appointment reminders (p < 0.05).
Significant differences in the number of patients willing to participate in ATC adherence support (p < 0.05).
Significant differences in the number of patients willing to participate in ATC health monitoring (p < 0.05).
Significant differences in the number of patients willing to participate in ATC self-care education (p < 0.05).
ATC, automated telephone calls.
Note: Cell entries are row percentages.
Fig. 2.
Proportion of respondents interested in receiving automated telephone self-care education, by age and perceived health status.
With a few exceptions, there was little variation in respondents' interest in these services across ages, genders, or other sociodemographic or clinical subgroups. Patients with pulmonary disease were somewhat less likely to report a willingness to participate in automated telephone self-care education, whereas patients with hypertension were more interested than other patients in receiving appointment reminders, adherence support, health status monitoring, and self-care information via automated calls.
Patients who reported transportation and cost barriers to care were consistently more likely to report a willingness to participate in telehealthcare. For example, compared to patients who had not had to cancel a medical appointment in the prior year due to a transportation problem, those who had cancelled an appointment were more likely to report a willingness to participate in automated appointment reminders (91% vs. 82%), medication adherence reminders (91% vs. 78%), health status monitoring (88% vs. 73%), and self-management support (89% vs. 75%; all p < 0.05). A similar pattern was observed with respect to groups that did and did not report cost-related medication underuse or failure to seek care due to a cost concern.
In multivariate analyses, we identified a number of independent correlates of patients' willingness to participate in chronic illness self-management support using automated telephone calls (Table 4). Employed participants were significantly more likely than unemployed participants to report a willingness to use automated telephone appointment reminders, and patients with hypertension were more likely to report a willingness to receive both these messages as well as automated telephonic adherence support. Patients reporting that they had missed an appointment in the prior year due to a transportation problem were significantly more likely to report a willingness to participate in automated assistance with adherence, health monitoring, and self-care. Controlling for covariates, patients who reported taking less medication than prescribed due to cost pressures were more likely to report a willingness to participate in appointment reminders, adherence support, and education about their disease self-management.
Table 4.
Adjusted Odds Ratios from Logistic Models Predicting Willingness to Participate in Chronic Illness Self-Management Support Using Automated Telephone Calls
| N = 624 | ATC Appointment Reminders | ATC Adherence Support | ATC Health Monitoring | ATC Self-Care Education |
|---|---|---|---|---|
|
Demographics | ||||
| Education | ||||
| Primary |
Ref |
Ref |
Ref |
Ref |
| Secondary |
1.13 |
1.42 |
1.66a |
1.60 |
| >Secondary |
0.9 |
0.97 |
1.13 |
0.93 |
| Employed | ||||
| No |
Ref |
Ref |
— |
Ref |
| Yes |
2.48b |
2.08 |
— |
1.72 |
|
Chronic diseases | ||||
| Pulmonary | ||||
| No |
— |
Ref |
Ref |
Ref |
| Yes |
— |
0.71 |
0.77 |
0.62a |
| Hypertension | ||||
| No |
Ref |
Ref |
— |
— |
| Yes |
1.81a |
2.09a |
— |
— |
| Depression | ||||
| No |
— |
— |
— |
Ref |
| Yes |
— |
— |
— |
1.28 |
|
Access barriers | ||||
| Transportation problem | ||||
| No |
Ref |
Ref |
Ref |
Ref |
| Yes |
1.62 |
2.00a |
2.56a |
1.73a |
| Medication CRN | ||||
| No |
Ref |
Ref |
— |
Ref |
| Yes |
2.10a |
3.24b |
— |
2.98b |
| Outpatient visit CRN | ||||
| No |
Ref |
Ref |
— |
Ref |
| Yes | 0.87 | 0.54 | — | 0.67 |
p < 0.05.
p < 0.01.
Note: Cell entries are adjusted odds ratios.
Discussion
A recent article in a national newspaper in Guatemala reported that the number of cell phone users within that country increased in 2009 by 15% or 2.35 million subscribers (Prensa Libre, March 16, 2010). Those data are consistent with other reports that mobile technology is diffusing rapidly in Latin America,17 and the current study demonstrates that even in a low-income area of Honduras—an area in which less than 30% of the population reported mobile phones as recently as 2005—the majority of chronically ill adults now have cell phones that include text messaging and voicemail. We found that mobile technology was common across socioeconomic strata, including among older patients, patients with at most a primary school education, patients who were unemployed, and patients with a wide variety of chronic health problems.
We also found that the majority of patients in Honduras were willing to participate in various forms of pro-active outreach designed to improve their illness self-care via automated telephone messaging. Several review articles have concluded that proactive telehealthcare is an important component of chronic disease management.27–29 However, between-visit telephone support by clinicians tends to be costly, taking a significant amount of staff time. Automated calling systems are one strategy for increasing the efficiency of between-visit telephone support, and studies conducted in the United States suggest that automated calls can be used to gather reliable data on patients' clinical status, as well as to improve chronic disease outcomes such as patients' self-care or physiologic control.22,30,31
We found important differences in patients' willingness to participate in automated telehealth services according to indicators of their access to care. In particular, patients who reported having to cancel appointments because of transportation problems and those who reported having to forego treatment due to cost were especially interested in receiving telehealthcare. Telehealth would clearly be a promising strategy for bringing self-care support to patients with complex chronic conditions who have difficulty attending face-to-face appointments. Further research is needed to understand why patients reporting cost-related medication underuse might be more accepting of telehealth, and how such services might improve their adherence.
It is unclear why patients with pulmonary diseases were less likely to have telephone access than patients without those conditions. We do know that pulmonary patients were significantly more likely to be women and to have at most a primary school education. Each of these factors was associated with patients' employment status (e.g., only 29% of employed respondents were women compared to 78% of unemployed respondents). It may well be that patients with pulmonary diseases were less likely to report access to telephones because they are relatively disadvantaged socioeconomically and lack the resources to purchase phones, share a phone with a male partner working outside of the household, or have less resources at their disposal to purchase calling cards. Pulmonary patients may have been less likely to express interest in automated telephone self-care education either because of their more limited telephone access or because they view their condition as more intermittent, less controllable, and therefore less important for ongoing proactive disease care. These findings highlight the importance of mixed methods research, including qualitative interviews, to truly understand causal processes when developing telemedicine interventions for unfamiliar environments such as this community in Honduras.
Very few other reports have documented the feasibility of telehealth services in Latin America. One report from Colombia found that the vast majority of physicians in that country have Internet access, and that 80% were interested in cell-phone-based self-management support.20 Two other studies found high acceptance rates, including patients' willingness to participate in mental health counseling via telephone.14,32 Unpublished results from a recent telehealth satisfaction survey in Colombia show that 73% of patients considered teleconsultation at least equally effective or more effective compared to a face-to-face medical consultation, and 80% were satisfied with this alternative to in-person visits. The current study adds to the growing evidence suggesting that a greater investment in telehealth programs would be both feasible, well-received by patients, and a potentially valuable approach to increasing access and effectiveness of chronic illness care.
Although this is one of the first large studies of its kind, it is important to recognize that the sample was not designed to be representative of all chronically ill adults, either in Honduras or in the larger region. Given that almost all Honduran patients have to pay out-of-pocket for health services and the very high rates of cost-related service underuse we observed, we expect that patients with less serious health problems (and potentially more effective disease self-management) were under-represented. Also, patients were asked to report on their hypothetical willingness to participate in automated telephone disease management. Actual program participation rates—both initial recruitment for such programs as well as long-term adherence—would likely depend on factors such as the user-friendliness of the system and patients' perception of benefit. Given the high degree of cost sensitivity we observed, clinics and health systems should consider alternative ways of funding such programs, rather than through patient charges.
In conclusion, we found that the majority of chronically ill patients in rural Honduras—including patients who are unemployed, are elderly, and have limited educational attainment—have access to cell phones, which could be used to connect patients with their healthcare team between face-to-face encounters. Most patients were willing to participate in automated telephone messaging that supports a variety of the core features of chronic illness care management, including visit reminders, promotion of medication adherence, health status monitoring, and self-care education. Interest in automated telephone care was particularly great among patients with transportation problems or financial barriers to medication use. Efforts within and across countries should explore ways to effectively build on what is known regarding the design of telehealth programs, taking advantage of the explosion of cell phone access in less developed countries and bringing disease management services to patients with significant barriers to access.
Acknowledgments
This research was funded jointly by the University of Michigan School of Public Health Global Health Summer Internship Program, the Michigan Diabetes Research and Training Center (NIH # DK020572), and the Michigan Institute for Clinical and Health Research (NIH #UL1RR024986). Dr. Piette is a VA Senior Research Career Scientist and Faculty Associate of the University of Michigan Center for Global Health. Laura Chess and Olga Semenova collected the data in Honduras. Dr. Armando Matiz Reyes provided important administrative support for the study, and Dr. José I. Valenzuela gave important feedback on a draft of the article. The authors thank the patient participants as well as Professor Maria Guzman Segovia, La Clinica Santa Lucia (Dr. Francisco Pineda), El Centro de Salud Publico, Francisco Beltran de Santa Cruz de Yojoa (Dr. Josue Banegas), and Consultorio Medico La Luz (Dr. Blanca Luz Rubi).
Disclosure Statement
No competing financial interests exist.
References
- 1.Daar AS. Singer PA. Persad DL, et al. Grand challenges in chronic non-communicable diseases. Nature. 2007;450:494–496. doi: 10.1038/450494a. [DOI] [PubMed] [Google Scholar]
- 2.Cardiovascular Disease Prevention and Control. 2010. www.who.int/dietphysicalactivity/publications/facts/cvd/en/ [Aug 1;2010 ]. www.who.int/dietphysicalactivity/publications/facts/cvd/en/
- 3.Geneva: WHO; 2005. [Aug 1;2010 ]. WHO Facing the Facts: The Impact of Chronic Disease in the Americas. [Google Scholar]
- 4.The Diabetes Atlas. 2009. www.idf.org/Facts_and_Figures. [Aug 1;2010 ]. www.idf.org/Facts_and_Figures
- 5.Millennium Development Goals Report. 2009. www.un.org/millenniumgoals/reports.shtml. [Aug 1;2010 ]. www.un.org/millenniumgoals/reports.shtml
- 6.Mobile Health: The potential of mobile telephony to bring health care to the majority. 2009. http://idbdocs.iadb.org/wsdocs/getdocument.aspx?docnum=1728061. [Aug 1;2010 ]. http://idbdocs.iadb.org/wsdocs/getdocument.aspx?docnum=1728061
- 7.Health in the Americas. 2007. www.paho.org/hia/archivosvol2/paisesing/honduras%20english.pdf. [Aug 1;2010 ]. www.paho.org/hia/archivosvol2/paisesing/honduras%20english.pdf
- 8.Bodenheimer T. Wagner EH. Grumbach K. Improving primary care for patients with chronic illness. JAMA. 2002;288:1775–1779. doi: 10.1001/jama.288.14.1775. [DOI] [PubMed] [Google Scholar]
- 9.Von Korff M. Gruman J. Schaefer J. Curry SJ. Wagner EH. Collaborative management of chronic illness. Ann Intern Med. 1997;127:1097–1102. doi: 10.7326/0003-4819-127-12-199712150-00008. [DOI] [PubMed] [Google Scholar]
- 10.Organization WH. Health Telematics Policy in Support of the WHO's Health-for-All strategy for Global Health Development: Report of the WHO Group Consultation on Health Telematics; Geneva, Switzerland. Dec 11–17;1997–1998 ; [Google Scholar]
- 11.Geneva, Switzerland: 2005. [Aug 1;2010 ]. Health and the Millennium Development Goals. [Google Scholar]
- 12.Car J. Sheikh A. Email consultations in health care: Scope and effectiveness. Br Med J. 2004;329:435–438. doi: 10.1136/bmj.329.7463.435. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Institute of Medicine. Crossing the quality chasm: A new health system for the 21st century. Washington, DC: National Academy Press; 2001. [PubMed] [Google Scholar]
- 14.Valenzuela JI. Arguello A. Cendales JG. Rizo CA. Web-based asynchronous teleconsulting for consumers in Colombia: A case study. J Med Internet Res. 2007;9:e33. doi: 10.2196/jmir.9.4.e33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Internet World Statistics for South America. www.internetworldstats.com/south.htm. [Aug 1;2010 ]. www.internetworldstats.com/south.htm
- 16.GESICA Investigators. Randomised trial of telephone intervention in chronic heart failure: DIAL trial. Br Med J (Clin Res Ed) 2005;331:425–429. doi: 10.1136/bmj.38516.398067.E0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.World Information Society 2007 Report: Beyond WSIS. 2007. www.itu.int/osg/spu/publications/worldinformationsociety/2007/report.html. [Aug 1;2010 ]. www.itu.int/osg/spu/publications/worldinformationsociety/2007/report.html
- 18.Asociación de la Industria Celular en Colombia. Densidad celular en Colombia. www.asocel.org.co/pdf/densidad_celular_en_%20colombia_90.pdf. [Aug 1;2010 ]. www.asocel.org.co/pdf/densidad_celular_en_%20colombia_90.pdf
- 19.World Bank. Private Sector Development Blog. http://psdblog.worldbank.org/psdblog/2006/06/more_cell_phone.html. [Aug 1;2010 ]. http://psdblog.worldbank.org/psdblog/2006/06/more_cell_phone.html
- 20.Valenzuela JI. Camacho JC. Arguello A. Cendales JG. Fajardo R. Perceptiones de los trabajadores del sector salud frente a Internet y las tecnologias moviles en Colombia. Rev Panam Salud Publica. 2009;25:367–374. doi: 10.1590/s1020-49892009000400012. [DOI] [PubMed] [Google Scholar]
- 21.Sapag JC. Lange I. Campos S. Piette JD. Innovaciones para el cuidado y autocuidado de personas con enfermedades cronicas en America Latina: Oportunidades y desafios para el trabajo en red. [Innovation for the care and self-care of persons with chronic diseases in Latin America: Opportunities and challenges for collaborative work.] Panamerican J Public Health. 2010;27:1–9. doi: 10.1590/s1020-49892010000100001. [DOI] [PubMed] [Google Scholar]
- 22.Piette JD. Weinberger M. McPhee SJ. Mah CA. Kraemer FB. Crapo LM. Do automated calls with nurse follow-up improve self-care and glycemic control among vulnerable patients with diabetes? Am J Med. 2000;108:20–27. doi: 10.1016/s0002-9343(99)00298-3. [DOI] [PubMed] [Google Scholar]
- 23.Piette JD. McPhee SJ. Weinberger M. Mah CA. Kraemer FB. Use of automated telephone disease management calls in an ethnically diverse sample of low-income patients with diabetes. Diabetes Care. 1999;22:1302–1309. doi: 10.2337/diacare.22.8.1302. [DOI] [PubMed] [Google Scholar]
- 24.Piette JD. Patient education via automated calls: A study of English- and Spanish-speakers with diabetes. Am J Prev Med. 1999;17:138–141. doi: 10.1016/s0749-3797(99)00061-6. [DOI] [PubMed] [Google Scholar]
- 25.Piette JD. Weinberger M. Kraemer FB. McPhee SJ. Impact of automated calls with nurse follow-up on diabetes treatment outcomes in a department of veterans affairs health care system: A randomized controlled trial. Diabetes Care. 2001;24:202–208. doi: 10.2337/diacare.24.2.202. [DOI] [PubMed] [Google Scholar]
- 26.Milton EC. Herman WH. Aiello AE. Danielson KR. Mendoza-Alvelarez MO. Piette JD. Validation of a type 2 diabetes screeening tool in rural Honduras. Diabetes Care. 2010;33:275–277. doi: 10.2337/dc09-1021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Clark RA. Inglis SC. McAlister FA. Smith AL. Telemonitoring or structured telephone support programmes for patients with chronic heart failure: Systematic review and meta-analysis. Br Med J. 2007;334:942–950. doi: 10.1136/bmj.39156.536968.55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Stead LF. Perera R. Lancaster T. Telephone counselling for smoking cessation. Cochrane Database Syst Rev. 2006;6:CD002850. doi: 10.1002/14651858.CD002850.pub2. [DOI] [PubMed] [Google Scholar]
- 29.Wu L. Forbes A. While A. Griffiths P. Telephone follow-up to improve glycaemic control in patients with type 2 diabetes: A systematic review and meta-analysis of controlled trials. Cochrane Database Syst Rev. (in press). [DOI] [PubMed]
- 30.Goldberg LR. Piette JD. Walsh MN, et al. Randomized trial of a daily electronic home monitoring system in patients with advanced heart failure: The weight monitoring in heart failure (wharf) trial. Am Heart J. 2003;146:705–712. doi: 10.1016/S0002-8703(03)00393-4. [DOI] [PubMed] [Google Scholar]
- 31.Piette JD. Weinberger M. McPhee SJ. The effect of automated calls with telephone nurse follow-up on patient-centered outcomes of diabetes care: A randomized, controlled trial. Med Care. 2000;38:218–230. doi: 10.1097/00005650-200002000-00011. [DOI] [PubMed] [Google Scholar]
- 32.Piette JD. Lange I. Issel M, et al. Use of telephone care in a cardiovascular disease management programme for type 2 diabetes patients in Santiago, Chile. Chronic Illn. 2006;2:87–96. doi: 10.1177/17423953060020020401. [DOI] [PubMed] [Google Scholar]