Abstract
Background
Limited empirical data are available on the effects of genetic counseling and testing among African American women.
Objective
To evaluate the effects of genetic counseling and testing in African American women based on different levels of exposure: (a) women who were randomized to culturally tailored (CTGC) and standard genetic counseling (SGC) to women who declined randomization (non-randomized group), (b) participants and non-participants in genetic counseling, and (c) BRCA1 and BRCA2 (BRCA1/2) test result acceptors and decliners.
Design
Randomized trial of genetic counseling conducted from February 2003 to November 2006.
Measures
We evaluated changes in perceived risk of developing breast cancer and cancer worry.
Results
Women randomized to CTGC and SGC did not differ in terms of changes in risk perception and cancer worry compared to decliners. However, counseling participants had a significantly greater likelihood of reporting reductions in perceived risk compared to non-participants (p = 0.03). Test result acceptors also had a significantly greater likelihood of reporting decreases in cancer worry (p = 0.03). However, having a cancer history (p = 0.03) and a BRCA1/2 prior probability (p = 0.04) were associated with increases in cancer worry.
Conclusions
Although CTGC did not lead to significant improvements in perceived risk or psychological functioning, African American women may benefit from genetic counseling and testing. Continued efforts should be made to increase access to genetic counseling and testing among African American women at increased risk for hereditary disease. But, follow-up support may be needed for women who have a personal history of cancer and those with a greater prior probability of having a BRCA1/2 mutation.
Key Words: African American, BRCA1, BRCA2, Cultural factors, Genetic counseling
It is estimated that about 16–28% of African American women who have a personal or family history of breast and/or ovarian cancer that is suggestive of hereditary disease carry a BRCA1 or BRCA2 (BRCA1/2) mutation [1,2,3]. Because of the excess rates of breast cancer morbidity and mortality among African American women [4] and the similarities between hereditary disease and breast cancer in this population [5], efforts are now focused on increasing access to genetic counseling and testing in this population [6]. Recent research has shown that uptake of genetic counseling and testing is variable among African Americans [6,7,8]. However, regardless of whether women choose to receive BRCA1/2 test results, participation in genetic counseling may be beneficial to African American women because of the attention given to psychological issues and provision of personalized risk information.
To our knowledge, only a single observational study has evaluated the impact of genetic counseling and testing among African Americans who were members of one BRCA1 kindred [9]. This study, which provided participants with culturally targeted education materials, found that receiving BRCA1 test results did not lead to adverse psychological functioning. Specifically, intrusive thoughts about cancer and attempts to avoid cancer-related thoughts and feelings did not change significantly among African American women following disclosure of positive BRCA1 test results and non-carriers reported significant declines in distress [9].
Increasingly, cultural factors are being recognized as being important to decisions about cancer prevention and control. Prior studies have shown that cultural beliefs and values such as temporal orientation, or the extent to which individuals are more focused on past, present, or future concerns and outcomes [10], are important to attitudes about and participation in genetic counseling and testing for BRCA1/2 mutations [11,12]. For this reason, culturally tailored interventions, or protocols in which beliefs and values related to temporal orientation and other cultural factors are targeted through written or verbal strategies, are being developed and evaluated [13,14]. In our previous work, culturally tailored genetic counseling (CTGC) was not associated with increased uptake of BRCA1/2 test results among African American women [7]; however, women who received CTGC were more likely than those who received standard counseling to report that the counselor lessened their worries [15]. This finding suggests that CTGC may have greater psychological benefits relative to standard protocols. Therefore, we evaluated the effects of CTGC and standard genetic counseling (SGC) on psychological outcomes among African American women in a randomized trial. While informed decision-making is the primary outcome of genetic counseling, perceived risk and cancer-related distress are also important outcomes of genetic counseling and testing, because they influence cancer screening behaviors [16,17]. Since limited empirical data are not available on whether or not African American women derive any benefit from genetic counseling, we also compared changes in psychological outcomes between women who completed genetic counseling and those who declined, regardless of randomization. To expand our knowledge on the impact of BRCA1/2 testing among African American women, we also determined whether decisions to have genetic testing and receive results had a significant independent association with changes in psychological functioning.
Methods
Study Participants
The study was approved by the Institutional Review Board at the University of Pennsylvania. Participants were adult women who self-identified as being African American and/or Black and who had a minimum 5% prior probability of having a BRCA1/2 mutation. Participants were recruited into the study between February 2003 and November 2006. It should be noted that some women (n = 28) had previously participated in an epidemiological study designed to identify genetic risk factors for breast cancer; however, genetic counseling, clinical testing, and test results were not provided to women as part of the epidemiological study.
Procedures
Detailed information about the study procedures has been provided previously [6] and is summarized here. Eligible women were invited to participate in the study following referral from clinical and community oncology resources. Verbal consent for enrollment was obtained using a structured consent script. In a small number of cases, more than one person from a family was enrolled in the study; however, this occurred in less than 10% of families and the average number of individuals per family was one. After enrollment, the baseline interview was completed. At the end of the interview, women were invited to participate in genetic counseling. Those who accepted the invitation were randomized to CTGC or SGC. We used a computer-based randomization program to assign women to counseling interventions. Women from the same family were assigned to the same counseling group.
Following randomization, women were scheduled for an individual genetic counseling session. Genetic counseling was provided at no cost to all participants. All sessions were completed at the University of Pennsylvania using semi-structured counseling protocols (see Interventions) after obtaining written informed consent. SGC lasted about 90 min and CTGC lasted about 90–120 min. At the end of counseling, women were given an opportunity to provide a blood sample for genetic testing. Those who were interested in testing met with a medical oncologist to discuss new medical issues and were offered a clinical breast examination. Possible test result outcomes and the risks and benefits of genetic testing were reviewed by the medical oncologist. At the end of this appointment, women who were interested in testing provided written informed consent and gave a blood sample. Genetic testing was provided at no cost to women with a ≥10% prior probability of having a BRCA1/2 mutation; for women with a 5–9% prior probability, these costs were submitted for payment by the participant's insurance company. When test results became available, a test results disclosure session was scheduled.
During this session, BRCA1/2 test results were provided by the genetic counselor and medical oncologist after obtaining written informed consent. Women were also given information about their risk of developing cancer, individualized guidelines for surveillance and prevention, and risk of having a BRCA1/2 mutation among family members. Regardless of test result and randomization to CTGC or SGC, all women received a written report that included an interpretation of their BRCA1/2 test result and guidelines for medical management. Women were also contacted by the study genetic counselor approximately 2 weeks following the disclosure session to answer any additional questions and to provide referrals for surveillance and prevention options, if needed. All participants were contacted 1 month after disclosure or the date that counseling, testing, and/or results were declined for a follow-up telephone interview to re-assess psychological functioning.
Interventions
The CTGC and SGC protocols have been described in detail elsewhere [7,15]. Both protocols were semi-structured and included visual aids. All genetic counseling sessions were conducted by a board-certified genetic counselor, who was white. Adherence to the protocols was monitored by reviewing audio tapes of selected sessions and documenting the issues that were addressed during SGC and CTGC. SGC consisted of education about hereditary breast and ovarian cancer, the process of genetic testing for BRCA1/2 mutations, and interpretation of genetic test results. Information about cancer risks associated with BRCA1/2 mutations and the probability of having a BRCA1/2 mutation was provided to women as part of the SGC protocol. Women also received information about the benefits, limitations, and risks of genetic testing. Information about the unique aspects of breast cancer in African American women was also provided to women as part of the SGC protocol.
The educational information provided as part of SGC was also given to women randomized to CTGC. CTGC differed from SGC in that cultural beliefs and values related to health care decision-making were addressed. Consistent with guidelines for culturally competent genetic counseling [18,19], the CTGC protocol incorporated discussion of beliefs and values related to spirituality and religion, temporal orientation, and communalism, which have been associated with decisions about genetic testing, medical care, and risk perceptions among African American women [20,21,22]. Specifically, a genogram and structured probes were used in the CTGC protocol to encourage women to discuss how these beliefs and values would be used to make decisions about genetic testing and cope with testing outcomes.
Measures
Sociodemographics. Age, income, marital status, education and employment status were obtained during the baseline telephone interview.
Clinical Factors. Clinical factors included personal history of breast and/or ovarian cancer, prior probability of having a BRCA1/2 mutation and family history of disease. Personal and family history of cancer was obtained by self-report. We used risk estimation models (e.g. BRCApro) and mutation prevalence tables to estimate each woman's probability of having a BRCA1/2 mutation (5–9% or ≥10%) [23]. Women were also categorized as having 2 or more or fewer than 2 affected relatives based on the total number of family members diagnosed with breast and/or ovarian cancer.
Genetic Counseling and Testing Variables. Genetic counseling and testing variables included: (a) randomization to genetic counseling protocols, (b) participation in genetic counseling, and (c) BRCA1/2 testing decisions. For randomization to genetic counseling interventions, we compared women who were randomized to CTGC or SGC. Since many African American women may decline participation in genetic counseling following randomization [6,7], or may decline to be randomized, those who declined randomization were included in the comparison of CTGC and SGC as a non-randomized control group. For participation in genetic counseling, women who completed pre-test counseling (regardless of randomization) were categorized as participants. Women who declined the invitation for genetic counseling and those who did not complete counseling after randomization were categorized as non-participants in the analysis of participation in genetic counseling. For BRCA1/2 testing decisions, women who participated in pre-test genetic counseling, provided a blood sample for testing and received genetic test results were categorized as test result acceptors. Test result decliners included women who declined to participate in pre-test counseling, those who participated in pre-test counseling but declined to provide a blood sample for testing, and women who declined to receive test results after participating in pre-test counseling and providing a blood sample for testing.
Perceived Risk. We used a validated Likert style item to evaluate breast cancer risk perceptions [22,24]. Specifically, women were asked what their chances of getting breast cancer were compared to other women their age (1 = much lower to 5 = much higher). As in previous reports [25], women who reported that both breasts were removed at baseline were excluded from the analysis of risk perceptions. Thus, the sample size for the perceived risk analysis is slightly lower than for other analyses.
Cancer Worry. We used the Breast Cancer Worry Scale to evaluate psychological functioning [26]. This is a 3-item Likert style scale that evaluates the extent to which women thought about their chances of developing breast cancer and how much these thoughts affected their mood and ability to perform their daily activities. This scale had acceptable internal consistency in this sample (Cronbach's alpha = 0.72).
Statistical Analysis
The trial initially called for enrollment of 360 women; for reasons of feasibility, this was reduced to 180 women. The initial design provided 80% power to detect differences between the randomized groups of about 20% in test acceptance, and about one standard deviation in cancer worry; the revised design provided 80% power to detect differences of about 30% in test acceptance and 1.5 standard deviations in cancer worry. Our power to detect changes in risk perception and psychological functioning for our comparisons between women who were randomized to CTGC and SGC and those in the non-randomized control group was necessarily reduced due to the relatively small size of the non-randomized group; here we had about 80% power to detect difference of approximately 2 standard deviations.
First, we generated descriptive statistics to characterize the study sample in terms of sociodemographic factors and clinical characteristics. We then conducted χ2 tests of association to determine if counseling groups were unbalanced with respect to these characteristics and to identify factors that were associated with participation in genetic counseling and retention in the follow-up telephone interview. Bivariate analyses were also conducted to evaluate the relationship between sociodemographic and clinical factors and baseline levels of study outcomes. Next, we used ordered logistic regression analysis to evaluate the effects of randomization to CTGC and SGC on perceived risk and psychological functioning. For these analyses, change scores between baseline and 1 month follow-up were calculated and were grouped into categories that roughly balanced the distributions for both measures. This resulted in 6 categories for changes in cancer worry (decrease of 3 or more units, decrease of 2 units, decrease of one unit, no change, increase of one unit, increase of 2 or more units) and 4 categories for change in perceived risk (decrease of 2 or more units, decrease of one unit, no change, increase of one or more units). For both measures, positive values indicated an increase in the outcome while negative values indicated a decrease. Variables that were associated significantly (p < 0.05) with randomization, participation in genetic counseling and study retention were included in each of the regression models as controlling factors. Sociodemographic and clinical factors associated with baseline levels of study outcomes were included in the regression models if they were significant predictive factors or if they caused confounding, assessed as >10% change in other estimated odds ratios in the models.
Results
Enrollment Rates and Sample Characteristics
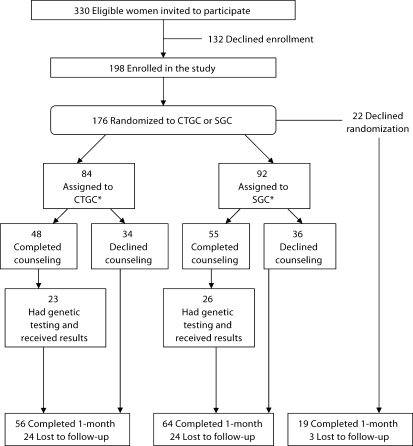
A total of 330 eligible women were invited to participate and 198 (60%) enrolled in the study (fig. 1). Of the women who enrolled in the study, 176 accepted the invitation to participate in genetic counseling and were randomized to CTGC and SGC. With the exception of education and income, women who accepted the invitation for genetic counseling did not differ from those who declined in terms of sociodemographic or clinical characteristics. Women with household incomes greater than USD 35,000 were most likely to agree to randomization (χ2 = 4.14, p = 0.04) as were those with greater education (χ2 = 21.8, p = 0.001). There were no differences in sociodemographic or clinical characteristics between women who were randomized to CTGC or SGC; however, women who had previously participated in the epidemiological study were most likely to have been assigned to SGC (χ2 = 7.43, p = 0.01). With respect to participation in genetic counseling among women who were randomized to CTGC or SGC, those with a ≥10% prior probability of having a BRCA1/2 mutation were most likely to complete counseling (χ2 = 10.44, p = 0.001) as were women who had a personal history of cancer (χ2 = 4.59, p = 0.03). No other sociodemographic or clinical factors were associated significantly with participating in genetic counseling.
Fig. 1.
Study participation. *Women who were pending completion of counseling (n = 3) or the 1-month follow-up (n = 4), and those who became ineligible for the follow-up (n = 1) were excluded from the analysis. The final sample included 56 women assigned to CTGC, 64 assigned to SGC, and 19 non-randomized decliners who were retained in the study.
Among women who were eligible for the 1-month follow-up telephone interview (n = 190), 73% were retained. Only being unemployed was associated significantly with being lost to follow-up (χ2 = 10.02, p = 0.002). There were no differences in retention between women who were randomized to CTGC or SGC (χ2 = 0.15, p = 0.70) and those who agreed to randomization and women who declined (χ2 = 2.21, p = 0.14). The sample included in this analysis included 139 women (56 women randomized to CTGC, 64 randomized to SGC, and 19 non-randomized decliners) who were retained in the study.
Table 1 shows the characteristics of the study sample and figure 1 shows the number of women who were randomized to CTGC and SGC and participated in genetic counseling and testing. Among women who had genetic testing, 7 were mutation carriers (17%), 28 were BRCA1/2negative (67%), and 7 (17%) had variants of uncertain significance. Marital status (Kruskal-Wallis χ2 = 3.88, p = 0.05), education (Kruskal-Wallis χ2 = 6.75, p = 0.01), and income (Kruskal-Wallis χ2 = 5.15, p = 0.02) were associated significantly with risk perception at baseline. Marital status (Kruskal-Wallis χ2 = 5.93, p = 0.01), age (Kruskal-Wallis χ2 = 13.48, p = 0.0002), BRCA1/2 prior probability (Kruskal-Wallis χ2 = 6.86, p = 0.01), family history of cancer (Kruskal-Wallis χ2 = 4.03, p = 0.05), and randomization to CTGC or SGC (Kruskal-Wallis χ2 = 6.0, p = 0.05) were also associated significantly with cancer worry at baseline.
Table 1.
Sample characteristics (n = 139)
| Variable | Level | n (%) |
|---|---|---|
| Age | ≤50 | 82 (59%) |
| >50 | 57 (41%) | |
| Marital status | unmarried | 97 (70%) |
| married | 42 (30%) | |
| Education level | ≥ some college | 97 (70%) |
| ≤ high school | 42 (30%) | |
| Employment status | employed | 95 (68%) |
| unemployed | 44 (32%) | |
| Income* | <35,000 USD | 71 (51%) |
| >35,000 USD | 67 (49%) | |
| Insurance status | yes | 134 (96%) |
| no | 5 (4%) | |
| Cancer history | affected | 96 (69%) |
| unaffected | 43 (31%) | |
| Family history of cancer | 2 or more relatives | 88 (63%) |
| less than 2 relatives | 51 (37%) | |
| BRCA1/2 prior probability | ≥10% | 78 (56%) |
| 5–9% | 61 (44%) | |
| Genetic counseling | participants | 79 (57%) |
| non-participants | 60 (43%) | |
| BRCA1/2 testing decisions | accept | 42 (30%) |
| decline | 97 (70%) | |
One participant was missing data for income.
Effect of Genetic Counseling and Testing Decisions on Risk Perception
The results of the regression analyses for changes in risk perception are shown in table 2. There were no differences in changes in risk perception between women who were randomized to CTGC and SGC and those in the non-randomized group. These results were confirmed in analyses that evaluated changes in risk perception between participants in CTGC and SGC, genetic counseling non-participants, and those in the non-randomized group (likelihood ratio test [LRT] = 5.14, p = 0.16). There were also no differences in changes in risk perception between participants in CTGC and SGC (LRT = 0.07, p = 0.79) and BRCA1/2 testing decisions did not have a significant effect on changes in risk perception (table 2). However, regardless of the type of genetic counseling, participation had a significant effect on changes in risk perception. Counseling participants had a significantly greater likelihood of reporting decreases in perceived risk of developing breast cancer compared to non-participants. We repeated these analyses excluding women who had a bilateral mastectomy at follow-up and the results were unchanged (data not shown).
Table 2.
Effect of genetic counseling and testing decisions on risk perception
| Variable | Level | Comparisons |
|||||
|---|---|---|---|---|---|---|---|
| Intention-to-treat: CTGC vs non-randomized control (a) SGC vs non-randomized control (b) |
Participation in genetic counseling: participants vs non-participants |
Testing decisions: accept vs decline |
|||||
| OR | 95% CI | OR | 95% CI | OR | 95% CI | ||
| Study group | + | 0.47 (a) | 0.16, 1–41 | 0.45 | 0.22, 0.92* | 0.46 | 0.20, 1.05‡ |
| 0.55 (b) | 0.18, 1.73 | ||||||
| Education level | ≥ some college | 1.26 | 0.56, 2.86 | 1.16 | 0.54, 2.47 | 1.16 | 0.54, 2.48 |
| ≤ high school | |||||||
| Employment status | employed | 1.07 | 0.52, 2.20 | 1.10 | 0.53, 2.29 | 1.01 | 0.49, 2.08 |
| unemployed | |||||||
| Cancer history | affected | 0.82 | 0.38, 1.78 | 0.91 | 0.42, 1.97 | 0.95 | 0.44, 2.07 |
| unaffected | |||||||
| BRCA1/2 prior | ≥10% | 1.34 | 0.65, 2.72 | 1.24 | 0.61, 2.54 | 1.11 | 0.52, 2.38 |
| probability | 5–9% | ||||||
| Prior study | yes | 1.32 | 0.50, 3.48 | 1.30 | 0.51, 3.35 | 1.42 | 0.57, 3.66 |
| participation | no | ||||||
** p < 0.01
Comparisons are described above.
p < 0.05
p < 0.10.
Effect of Genetic Counseling and BRCA1/2 Testing Decisions on Psychological Functioning
Table 3 shows the results of the regression analyses for psychological functioning. There were no changes in cancer worry among women who were randomized to CTGC and SGC compared to those in the non-randomized decliner group. In analyses that compared women in the non-randomized group to participants in CTGC or SGC and non-participants who declined following randomization, the effect of SGC was significant (OR = 0.31, 95% CI = 0.11, 0.90, p = 0.03). This result should be interpreted with caution since the overall effect of study groups was not significant (LRT = 5.14, p = 0.16) and participation in genetic counseling did not have a significant effect on changes in psychological functioning (table 3). However, test result acceptors had a significantly greater likelihood of reporting decreases in cancer worry compared to test result decliners. Women who had a personal history of cancer and those with a ≥10% prior probability also had a significantly greater likelihood of reporting increases in cancer worry compared to unaffected women and those who had a lower prior probability. Cancer history and BRCA1/2 prior probability had significant effects on changes in functioning when the comparison was counseling participants versus non-participants as well as test result acceptors versus decliners (table 3). We repeated these analyses excluding women who were diagnosed with a cancer recurrence and the results were unchanged (data not shown).
Table 3.
Effect of genetic counseling and testing decisions on psychological functioning
| Variable | Level | Comparisons |
|||||
|---|---|---|---|---|---|---|---|
| Intention-to-treat: CTGC vs non-randomized control (a) SGC vs non-randomized control (b) |
Participation in genetic counseling: participants vs non-participants |
Testing decision: accept vs decline |
|||||
| OR | 95% CI | OR | 95% CI | OR | 95% CI | ||
| Study group | + | 0.46 (a) | 0.17, 1.23 | 0.65 | 0.35, 1.23 | 0.44 | 0.21, 0.93* |
| 0.39 (b) | 0.14, 1.08‡ | ||||||
| Education level | ≥ some college | 0.87 | 0.42, 1.81 | 0.71 | 0.37, 1.40 | 0.72 | 0.36, 1.40 |
| ≤ high school | |||||||
| Employment status | employed | 1.12 | 0.58, 2.18 | 1.11 | 0.57, 2.15 | 0.97 | 0.50, 1.90 |
| unemployed | |||||||
| Cancer history | affected | 1.86 | 0.89, 3.88 | 2.06 | 0.99, 4.30* | 2.27 | 1.08, 4.77* |
| unaffected | |||||||
| BCRA1/2 prior | ≥10% | 2.45 | 1.24, 4.85** | 2.55 | 1.29, 5.03** | 2.23 | 1.11, 4.47* |
| probability | 5–9% | ||||||
| Prior study | yes | 1.28 | 0.51, 3.21 | 1.45 | 0.60, 3.53 | 1.61 | 0.66, 3.89 |
| participation | no | ||||||
Comparisons are described above.
p < 0.01
p < 0.05
p < 0.10.
Discussion
Despite significant efforts, breast cancer morbidity and mortality continues to be substantially greater in African American women compared to women from other ethnic and racial groups [4]. Genetic counseling and testing for BRCA1/2 mutations is a strategy for providing women with information about their risk of developing breast cancer and addressing concerns about disease [27,28]. To our knowledge, this is the first randomized trial to evaluate the effects of CTGC and SGC on psychological outcomes among African American women at increased risk for having a BRCA1/2 mutation.
Although culturally competent interventions are hypothesized to improve health outcomes in ethnic and racial minorities [29,30], CTGC did not lead to significant changes in perceived risk or psychological functioning in the present study. This finding is consistent with a recent study which found that culturally tailored information about cancer screening and dietary behaviors was not more effective than a combined intervention that addressed both behavioral and cultural factors in improving mammography utilization and fruit and vegetable intake among African American women [13]. A possible explanation for our finding is that the individualized nature of genetic counseling is sufficient to address the needs of African American women. However, our previous work has shown that immediately after pre-test counseling, African American women who received CTGC were significantly more likely to report that the counselor lessened their worries compared to those who received SGC [15]. It could be that women derive greater benefits from CTGC, but these effects are diminished as women move from pre-test counseling to making testing. This may explain why receipt of BRCA1/2 test results was associated with significant changes in cancer worry. Another possible explanation is that CTGC is more effective for women who hold certain beliefs and values (e.g. greater religiosity, temporal orientation). Future studies should evaluate whether the effects of CTGC are moderated by women's cultural beliefs and values.
We found that counseling participants were most likely to report reductions in perceived risk whereas women who received BRCA1/2 test results were most likely to report reductions in cancer worries compared to decliners. It is possible that decreases in cancer worry were observed among test result acceptors because the information provided during pre-test counseling was reinforced by the medical oncologist and genetic counselor during subsequent visits. However, an equally plausible explanation is that cancer worries were reduced as a result of receiving BRCA1/2 test results. A recent study found that depressive symptoms and anxiety decreased significantly following test result disclosure in both mutation carriers and non-carriers who were members of African American BRCA1 kindred [9]. Because test results were highly correlated with BRCA1/2 testing decisions, we did not evaluate the effects of receiving positive, negative, or inconclusive BRCA1/2 test results on cancer worry. However, previous research has shown that uncertainty is reduced following genetic testing among African Americans regardless whether the results are positive or negative [31].
While reduction in cancer worry is clearly a benefit of genetic testing, it is important to consider whether reduction in perceived risk following genetic counseling is beneficial to African American women, especially in light of previous research which has shown that African American women with a personal and/or family history of breast cancer may not recognize that they have an increased risk of developing disease [22,][32]. Greater perceived risk has been positively associated with utilization of cancer screening and risk reduction options among women in the general population [16] and those from hereditary cancer families [17], respectively. Since African American women may not feel vulnerable to developing breast cancer before genetic counseling and testing [22,32], further reductions in perceived risk may not be beneficial. On the other hand, African American women are likely to base their risk perceptions on subjective factors such as worries about affected family members [32] and thoughts about past experiences [22]; thus, reductions in perceived risk may be an indication that genetic counseling is an effective strategy for addressing these concerns. Nevertheless, participation in genetic counseling alone may not be sufficient to improve psychological functioning among African American women; there was no difference in changes in cancer worry between counseling participants and non-participants. Further, women who had a personal history of cancer and those who had a greater prior probability of having a BRCA1/2 mutation were likely to experience increases in cancer worry.
In considering the results of this study, some limitations should be noted. First, our findings are generalizable to African American women who are recruited from clinical and community resources. Other potential limitations may be that we did not evaluate the effects of BRCA1/2 test results on changes in study outcomes because of the small number of women who received genetic test results. Also, we compared the effects of CTGC and SGC to a non-randomized control group. This decision was based on ethical concerns surrounding randomizing women to a non-intervention or wait-list control group. By including a non-randomized control group, we were able to compare the effects of CTGC and SGC to no counseling in addition to evaluating the effects of 2 alternate forms of genetic counseling. This approach, along with comparing counseling participants versus non-participants and test result acceptors versus decliners, allowed us to conduct a comprehensive evaluation of all aspects of genetic counseling and testing for BRCA1/2 mutations in a population that is under-represented in cancer prevention and control research. While the beneficial effect of genetic counseling in the absence of testing is less clear, our findings support continuing efforts to increase access to genetic counseling and testing among African American women. But, additional follow-up may be needed for women who have a personal history of cancer and those who have a 10% or greater prior probability of having a BRCA1/2 mutation to address worries about developing cancer.
Acknowledgements
This research was supported by Department of Defense grant #DAMD17-00-1-0262 (to C.H.H.) and National Human Genome Research Institute grant #P50HG004487. We are very appreciative of all of the women who participated in this research. We would like to acknowledge Aliya Collier, BA, Kiyona Brewster, MA, and Benita Weathers, MPH for their contributions to the study.
Footnotes
Trial registration: www.clinicaltrials.gov (registration #NCT00419510).
References
- 1.Nanda R, Schumm LP, Cummings S, Fackenthal JD, Sveen L, Ademuyiwa F, Cobleigh M, Esserman L, Lindor NM, Neuhausen SL, Olopade OI. Genetic testing in an ethnically diverse cohort of high-risk women: a comparative analysis of BRCA1 and BRCA2 mutations in American families of European and African ancestry. JAMA. 2005;294:1925–1933. doi: 10.1001/jama.294.15.1925. [DOI] [PubMed] [Google Scholar]
- 2.Frank TS, Deffenbaugh AM, Reid JE, Hulick M, Ward BE, Lingenfelter B, Gumpper KL, Scholl T, Tavtigian SV, Pruss DR, Critchfield GC. Clinical characteristics of individuals with germline mutations in BRCA1 and BRCA2: analysis of 10,000 individuals. J Clin Oncol. 2002;20:1480–1490. doi: 10.1200/JCO.2002.20.6.1480. [DOI] [PubMed] [Google Scholar]
- 3.Gao Q, Tomlinson G, Das S, Cummings S, Sveen L, Fackenthal J, Schumm P, Olopade OI. Prevalence of BRCA1 and BRCA2 mutations among clinic-based African American families with breast cancer. Hum Genet. 2000;107:186–191. doi: 10.1007/s004390000290. [DOI] [PubMed] [Google Scholar]
- 4.American Cancer Society . Cancer Facts and Figures – 2007. Atlanta: American Cancer Society; 2007. [Google Scholar]
- 5.Olopade OI, Fackenthal JD, Dunston G, Tainsky MA, Collins F, Whitfield-Broome C. Breast cancer genetics in African Americans. Cancer. 2003;97:236–245. doi: 10.1002/cncr.11019. [DOI] [PubMed] [Google Scholar]
- 6.Halbert CH, Brewster K, Collier A, Smith C, Kessler L, Weathers B, Stopfer JE, Domchek S, Wileyto EP. Recruiting African American women to participate in hereditary breast cancer research. J Clin Oncol. 2005;23:7967–7973. doi: 10.1200/JCO.2004.00.4952. [DOI] [PubMed] [Google Scholar]
- 7.Halbert CH, Kessler L, Stopfer JE, Domchek S, Wileyto EP. Low rates of acceptance of BRCA1 and BRCA2 test results among African American women at increased risk for hereditary breast-ovarian cancer. Genet Med. 2006;8:576–582. doi: 10.1097/01.gim.0000237719.37908.54. [DOI] [PubMed] [Google Scholar]
- 8.Kinney AY, Simonsen SE, Baty BJ, Mandal D, Neuhausen SL, Seggar K, Holubkov R, Smith K. Acceptance of genetic testing for hereditary breast ovarian cancer among study enrollees from an African American kindred. Am J Med Genet A. 2006;140:813–826. doi: 10.1002/ajmg.a.31162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kinney AY, Bloor LE, Mandal D, Simonsen SE, Baty BJ, Holubkov R, Seggar K, Neuhausen S, Smith K. The impact of receiving genetic test results on general and cancer-specific psychologic distress among members of an African American kindred with a BRCA1 mutation. Cancer. 2005;104:2508–2516. doi: 10.1002/cncr.21479. [DOI] [PubMed] [Google Scholar]
- 10.Strathman A, Joireman J, editors. Understanding Behavior in the Context of Time: Theory, Research, and Applications. Mahwah, NJ: Lawrence Erlbaum Assoc.; 2005. [Google Scholar]
- 11.Edwards TA, Thompson HS, Kwate NO, Brown K, McGovern MM, Forman A, Kapil-Pair N, Jandorf L, Bovbjerg DH, Valdimarsdottir HB. Association between temporal orientation and attitudes about BRCA1/2 testing among women of African descent with family histories of breast cancer. Patient Educ Couns. 2008;72:276–282. doi: 10.1016/j.pec.2008.03.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Gurmankin Levy A, Micco E, Putt M, Armstrong K. Value for the future and breast cancer-preventive health behavior. Cancer Epidemiol Biomarkers Prev. 2006;15:955–960. doi: 10.1158/1055-9965.EPI-05-0169. [DOI] [PubMed] [Google Scholar]
- 13.Kreuter MW, Sugg-Skinner C, Holt CL, Clark EM, Haire-Joshu D, Fu Q, Booker AC, Steger-May K, Bucholtz D. Cultural tailoring for mammography and fruit and vegetable intake among low-income African American women in urban public health centers. Prev Med. 2005;41:53–62. doi: 10.1016/j.ypmed.2004.10.013. [DOI] [PubMed] [Google Scholar]
- 14.Kreuter MW, McClure SM. The role of culture in health communication. Annu Rev Public Health. 2004;25:439–455. doi: 10.1146/annurev.publhealth.25.101802.123000. [DOI] [PubMed] [Google Scholar]
- 15.Charles S, Kessler L, Stopfer JE, Domchek S, Halbert CH. Satisfaction with genetic counseling for BRCA1 and BRCA2 mutations among African American women. Patient Educ Couns. 2006;63:196–204. doi: 10.1016/j.pec.2005.10.007. [DOI] [PubMed] [Google Scholar]
- 16.Katapodi MC, Lee KA, Facione NC, Dodd MJ. Predictors of perceived breast cancer risk and the relation between perceived risk and breast cancer screening: a meta-analytic review. Prev Med. 2004;38:388–402. doi: 10.1016/j.ypmed.2003.11.012. [DOI] [PubMed] [Google Scholar]
- 17.Graves KD, Peshkin BN, Halbert CH, DeMarco TA, Isaacs C, Schwartz MD. Predictors and outcomes of contralateral prophylactic mastectomy among breast cancer survivors. Breast Cancer Res Treat. 2007;104:321–329. doi: 10.1007/s10549-006-9423-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Greb A. Multiculturalism and the practice of genetic counseling. In: Baker DL, Schuette JL, Uhlmann WR, editors. A Guide to Genetic Counseling. New York: Wiley-Liss; 1998. [Google Scholar]
- 19.Weil J. Psychosocial Genetic Counseling. New York: Oxford University Press; 2000. [Google Scholar]
- 20.Hughes C, Fasaye GA, LaSalle VH, Finch C. Sociocultural influences on participation in genetic risk assessment and testing among African American women. Patient Educ Couns. 2003;51:107–114. doi: 10.1016/s0738-3991(02)00179-9. [DOI] [PubMed] [Google Scholar]
- 21.Lannin DR, Mathews HF, Mitchell J, Swanson MS, Swanson FH, Edwards MS. Influence of socioeconomic and cultural factors on racial differences in late-stage presentation of breast cancer. JAMA. 1998;279:1801–1807. doi: 10.1001/jama.279.22.1801. [DOI] [PubMed] [Google Scholar]
- 22.Brewster K, Wileyto EP, Kessler L, Collier A, Weathers B, Stopfer JE, Domchek S, Halbert CH. Sociocultural predictors of breast cancer risk perceptions in African American breast cancer survivors. Cancer Epidemiol Biomarkers Prev. 2007;16:244–248. doi: 10.1158/1055-9965.EPI-06-0481. [DOI] [PubMed] [Google Scholar]
- 23.Domchek SM, Eisen A, Calzone K, Stopfer J, Blackwood A, Weber BL. Application of breast cancer risk prediction models in clinical practice. J Clin Oncol. 2003;21:593–601. doi: 10.1200/JCO.2003.07.007. [DOI] [PubMed] [Google Scholar]
- 24.Kessler L, Collier A, Brewster K, Smith C, Weathers B, Wileyto EP, Halbert CH. Attitudes about genetic testing and genetic testing intentions in African American women at increased risk for hereditary breast cancer. Genet Med. 2005;7:230–238. doi: 10.1097/01.gim.0000159901.98315.fe. [DOI] [PubMed] [Google Scholar]
- 25.Schwartz MD, Peshkin BN, Hughes C, Main D, Isaacs C, Lerman C. Impact of BRCA1/BRCA2 mutation testing on psychologic distress in a clinic-based sample. J Clin Oncol. 2002;20:514–520. doi: 10.1200/JCO.2002.20.2.514. [DOI] [PubMed] [Google Scholar]
- 26.Lerman C, Trock B, Rimer BK, Jepson C, Brody D, Boyce A. Psychological side effects of breast cancer screening. Health Psychol. 1991;10:259–267. doi: 10.1037//0278-6133.10.4.259. [DOI] [PubMed] [Google Scholar]
- 27.Biesecker BB. Goals of genetic counseling. Clin Genet. 2001;60:323–330. doi: 10.1034/j.1399-0004.2001.600501.x. [DOI] [PubMed] [Google Scholar]
- 28.Biesecker BB, Boehnke M, Calzone K, Markel DS, Garber JE, Collins FS, Weber BL. Genetic counseling for families with inherited susceptibility to breast and ovarian cancer. JAMA. 1993;269:1970–1974. [PubMed] [Google Scholar]
- 29.Betancourt, Green AR, Carrillo JE, Ananeh-Firempong O., 2nd Defining cultural competence: a practical framework for addressing racial/ethnic disparities in health and health care. Public Health Rep. 2003;118:293–302. doi: 10.1016/S0033-3549(04)50253-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Brach C, Fraser I. Can cultural competency reduce racial and ethnic health disparities? A review and conceptual model. Med Care Res Rev. 2000;57(suppl 1):181–217. doi: 10.1177/1077558700057001S09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Baty BJ, Dudley WN, Musters A, Kinney AY. Uncertainty in BRCA1 cancer susceptibility testing. Am J Med Genet C. 2006;142:241–250. doi: 10.1002/ajmg.c.30112. [DOI] [PubMed] [Google Scholar]
- 32.Hughes C, Lerman C, Lustbader E. Ethnic differences in risk perception among women at increased risk for breast cancer. Breast Cancer Res Treat. 1996;40:25–35. doi: 10.1007/BF01806000. [DOI] [PubMed] [Google Scholar]