Abstract
Objective:
In this study, relationships between sleep quality and borderline personality disorder were examined using 2 self-report measures.
Method:
Using a cross-sectional design in a sample of convenience of internal medicine outpatients, we surveyed men and women (N=76), aged 18 years or older, who were seeking nonemergent medical care during the period January 2009 to September 2009. Sleep quality was assessed with the Pittsburgh Sleep Quality Index (PSQI) and borderline personality was assessed with 2 measures: the borderline personality scale of the Personality Diagnostic Questionnaire-4 (PDQ-4) and the Self-Harm Inventory (SHI).
Results:
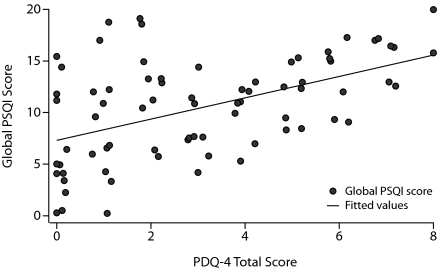
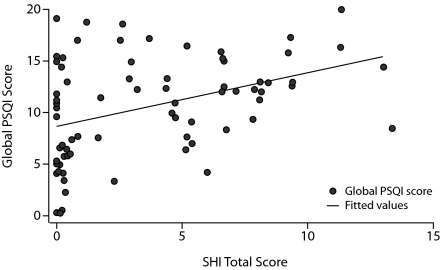
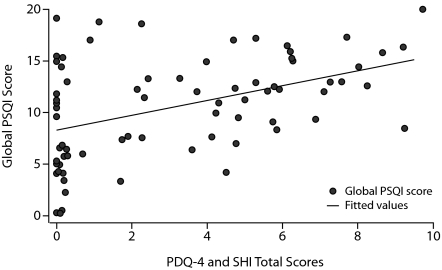
The global PSQI score was statistically significantly associated with scores on the PDQ-4 (P < .01), the SHI (P < .01), and the combination PDQ-4 and SHI (P < .01). With regard to the components of the PSQI, subjective sleep quality (P < .05), sleep duration (P < .05), and daytime dysfunction (P < .01) were all statistically significantly associated with scores on the PDQ-4, and sleep latency was statistically significantly associated with the combined PDQ-4 and SHI (P < .05).
Conclusions:
Individuals with borderline personality symptomatology demonstrate a poorer overall quality of sleep than those without these symptoms.
Borderline personality disorder (BPD) is a longstanding personality dysfunction that is characterized by, among other features, ongoing difficulties with self-regulation. Self-regulation deficits in individuals with this Axis II disorder may manifest in a variety of symptomatic areas, including eating disorders (ie, anorexia or bulimia nervosa, binge-eating disorder, obesity), drug/alcohol misuse and/or dependence, pain intolerance (ie, chronic pain syndromes), and promiscuity. Because the types of self-regulation difficulties in patients with BPD tend to be wide ranging, we speculated about a possible relationship between BPD and sleep disturbances (ie, sleep regulation difficulties).
Few empirical studies have examined sleep disturbances in individuals with BPD. Of those that have, the majority have explored electroencephalogram (EEG) aberrations in comparison with a control group (ie, a normal and/or depressed cohort).1–11 According to the findings of these studies, various types of EEG abnormalities may be present, most commonly a decrease in rapid eye movement (REM) latency and a decrease in slow-wave sleep. However, findings across studies have varied, and 1 study found no EEG differences between those with versus those without BPD.12 In addition, these various and at times subtle EEG abnormalities have been described by several investigators as nonspecific or nonpathognomonic.13–15
In addition to EEG sleep studies of patients with BPD, other types of sleep investigations have been undertaken as well. For example, Battaglia and colleagues16 examined abnormalities in heart rate during non-REM sleep. Compared with controls, those with BPD evidenced a smaller index of tonic heart rate during non-REM sleep. In addition, Semiz and colleagues17 examined subjective sleep quality in 88 Turkish patients with BPD using the Pittsburgh Sleep Quality Index (PSQI).18 Compared with controls, the cohort with BPD evidenced a greater frequency of nightmares, heightened dream anxiety, and more disturbed sleep quality. In this study, heightened dream anxiety was associated with a higher rate of traumatic experiences.18
To summarize, the preponderance of existing research has examined EEG abnormalities during sleep in individuals with BPD, and only 1 study has examined subjective sleep quality in patients with BPD. In this latter study of subjective sleep quality,17 the study sample consisted of Turkish patients, 54% were male, and the subjects were inpatients on a research unit for personality disorders. The unique ethnic sample, atypical gender distribution, and inpatient recruitment site each potentially compromise the ability to generalize findings to other populations.
In the present study, we examined among internal medicine outpatients relationships between subjective sleep quality using the PSQI and BPD according to 2 self-report measures.
Clinical Points
♦ Patients with increasing borderline personality symptomatology appear to evidence increasingly poor sleep quality according to the findings of this study.
♦ According to the Pittsburgh Sleep Quality Index, borderline personality disorder is associated with poor subjective sleep quality, shortened sleep duration, greater daytime dysfunction, and greater sleep latency; however, whether these findings are directly attributable to borderline personality disorder or a comorbid disorder, such as posttraumatic stress disorder, is unknown.
METHOD
Using a cross-sectional sample of convenience, we surveyed 76 respondents in an internal medicine outpatient clinic regarding sleep quality, using the PSQI, and borderline personality symptoms, using the borderline personality scale of the Personality Diagnostic Questionnaire-4 (PDQ-4)19 and the Self-Harm Inventory (SHI).20
Participants
Participants were men and women, aged 18 years or older, who were being seen in an outpatient internal medicine facility that is predominantly staffed by resident physicians. This clinic is located in the suburbs of a midsized, midwestern city. The sample was one of convenience (ie, patients were approached as clinical demands allowed). Exclusion criteria were medical (ie, severe pain), cognitive (eg, dementia), or psychiatric (eg, psychotic) illness that would preclude the successful completion of a survey booklet.
During the study period (January 2009–September 2009), 149 patients were approached; 116 agreed to participate, for a response rate of 78%. Of the 76 respondents included in our analyses (ie, those who completed all study materials), 74.6% were female and 25.4% male, ranging in age from 18 to 70 years (mean = 41.6, SD = 13.8). Most participants were white (84%); however, 6 participants were black, 2 Hispanic, and 2 Native American. With regard to educational attainment, all but 6.6% (n = 5) had at least graduated high school, whereas 26.6% (n = 20) had earned a college degree. One participant did not complete any demographic information but completed all other measures.
Procedure
During assigned clinic times, one of the investigators (H.C.E.) recruited participants from his clinical caseload according to time availability and the preceding inclusion/exclusion criteria, which were informally assessed. Following an explanation of the project, including potential risks and benefits, participants were asked to complete a 6-page survey booklet.
The cover page of the survey booklet contained the elements of informed consent, and completion of the survey booklet was assumed to be implied consent. In the survey booklet, we initially inquired about demographic information. We then explored subjective sleep quality using the PSQI.18 The PSQI is a 19-item, self-report questionnaire that explores subjective sleep quality over the past month. The last item relates to impressions of a bed partner and was deleted for this study, leaving a total of 18 items. The PSQI contains 7 component scores (ie, subjective sleep quality, sleep latency, sleep duration, habitual sleep efficiency, sleep disturbances, use of sleeping medications, daytime dysfunction), and these may be coalesced into 1 global score, with higher scores indicating poorer sleep quality. A global PSQI score > 5 is considered to be a sensitive and specific measure of poor sleep quality.
We used 2 measures for the assessment of BPD—the borderline personality scale of the PDQ-419 and the SHI.20 The borderline personality disorder scale of the PDQ-419 is a 9-item, true/false, self-report measure that consists of the diagnostic criteria for borderline personality that are listed in the DSM-IV. A score ≥ 5 is highly suggestive of BPD. Earlier versions of the PDQ have been confirmed as useful screening tools for borderline personality in both clinical21,22 and nonclinical samples,23 including the use of the free-standing borderline scale.24
The SHI20 is a 22-item, yes/no, self-report measure that explores participants’ lifetime histories of self-harm behavior. Each item in the inventory is preceded by the statement, “Have you ever intentionally, or on purpose,” and items include, “overdosed,” “cut yourself on purpose,” “burned yourself on purpose,” and “hit yourself.” Each endorsement is in the pathological direction, and the SHI total score is the summation of “yes” responses. SHI total scores ≥ 5 are highly suggestive of the diagnosis of BPD. Indeed, in comparison with the Diagnostic Interview for Borderlines,25 the gold standard for the diagnosis of borderline personality disorder in research settings, the SHI demonstrates an accuracy in diagnosis of 84%.20
Following completion of materials, participants were directed to place their survey booklets into sealed envelopes, which were then stored in a secure location to await statistical analysis. The institutional review boards of both the affiliated community hospital and university approved this project.
RESULTS
The responses of participants to the queries regarding sleep quality are shown in Table 1. Of the 76 respondents, 12 (15.8%) scored in the top quartile of the global PSQI score, indicating severe sleep difficulties. For the entire sample, of the 7 different sleep quality components, habitual sleep efficiency was the most commonly self-rated component score of extreme difficulty (36.8%), whereas only 9 (11.8%) respondents indicated extreme difficulty with regard to daytime dysfunction.
Table 1.
Respondents (N = 76) Reporting Severe Sleep Difficulties According to PSQI Scales, and Spearman's Correlations of Ordinal PSQI Scales With PDQ-4, SHI, and PDQ-4 + SHI Scores
| Endorsed Severe Sleep Difficulty, n (%) | Spearman's Correlations | |||
| PSQI | PDQ-4 | SHI | PDQ-4 + SHI | |
| Subjective sleep quality | 20 (26.3) | 0.41* | 0.27 | 0.31 |
| Sleep latency | 24 (31.6) | 0.36 | 0.37 | 0.39* |
| Sleep duration | 25 (32.9) | 0.40* | 0.32 | 0.34 |
| Habitual sleep efficiency | 28 (36.8) | 0.31 | 0.26 | 0.32 |
| Sleep disturbances | 12 (15.8) | 0.26 | 0.32 | 0.33 |
| Use of sleep medications | 12 (15.8) | 0.21 | 0.12 | 0.14 |
| Daytime dysfunction | 9 (11.8) | 0.43** | 0.34 | 0.36 |
| Global score | 12 (15.8) | 0.50** | 0.42** | 0.46** |
*P < .05.
**P < .01.
Abbreviations: PDQ-4 = Personality Diagnostic Questionnaire-4, PSQI = Pittsburgh Sleep Quality Index, SHI = Self-Harm Inventory.
Next, we examined correlations between the PSQI and borderline personality symptomatology according to PDQ-4 and SHI scores (Table 1, Figures 1–3). We further included a composite measure of individuals who scored positively for BPD on both measures. As our sleep quality components and global PSQI scores are ordinal variables, we tested our correlations using Spearman's ρ with Bonferroni corrections for multiple comparisons. In these analyses, subjective sleep quality, sleep duration, and daytime dysfunction were all statistically significantly associated with scores on the PDQ-4. Sleep latency was statistically significantly associated with the combined PDQ-4 + SHI measure. Finally, the global PSQI score was statistically significantly associated with all 3 assessment approaches to BPD.
Figure 1.
Global PSQI Score by PDQ-4 Total Score
Abbreviations: PDQ-4 = Personality Diagnostic Questionnaire-4, PSQI = Pittsburgh Sleep Quality Index.
Figure 2.
Global PSQI Score by SHI Total Score
Abbreviations: PSQI = Pittsburgh Sleep Quality Index, SHI = Self-Harm Inventory.
Figure 3.
Global PSQI Score by PDQ-4 and SHI Total Scores
Abbreviations: PDQ-4 = Personality Diagnostic Questionnaire-4, PSQI = Pittsburgh Sleep Quality Index, SHI = Self-Harm Inventory.
DISCUSSION
To summarize the present findings, global PSQI scores demonstrated statistically significant correlations with all assessment approaches to BPD, indicating that increasing borderline personality symptomatology is associated with an increased likelihood of sleep disturbances. This finding echoes those of Semiz and colleagues.17 As for the specific types of sleep disturbances encountered in BPD, our individual measures demonstrated associations with different components. Explicitly, increasing scores on the PDQ-4 were associated with increasingly poor subjective sleep quality, shortened sleep duration, and greater daytime dysfunction, whereas increasing scores on the combination PDQ-4/SHI were only associated with greater sleep latency. Scores on the SHI were not associated with any PSQI components. So, the pattern of sleep disturbances appears variable depending on the measure used for assessment. However, regardless of BPD measure, the global sleep scores were all correlated with BPD.
From these data, we believe that we can conservatively conclude that individuals with BPD experience disturbances in overall sleep quality. A number of factors may account for this finding in patients with BPD including their inherent self-regulatory deficits manifesting as sleep regulation difficulties; comorbid psychiatric disorders such as depression, substance abuse, and posttraumatic stress disorder; prescribed psychotropic medications; and psychosocial stressors.
These data have a number of potential limitations. These include the self-report nature of the data and the inherent limitations of this form of data collection, the tendency for the PDQ-4 to be overinclusive (ie, generate false positives), use of a sample of convenience (ie, risk of sampling bias), and the small sample size. However, this is the first study of subjective sleep quality in a US sample of patients with BPD. In addition, the assessment of sleep quality was undertaken with a standardized measure, and the study utilized 2 measures of BPD. Overall, findings indicate that individuals with borderline personality symptomatology experience poorer sleep quality regardless of assessment measure, although the explicit problematic components of sleep warrant further investigation.
Potential conflicts of interest: None reported.
Funding/support: None reported.
REFERENCES
- 1.McNamara E, Reynolds CF, 3rd, Soloff PH, et al. EEG sleep evaluation of depression in borderline patients. Am J Psychiatry. 1984;141(2):182–186. doi: 10.1176/ajp.141.2.182. [DOI] [PubMed] [Google Scholar]
- 2.Reynolds CF, 3rd, Soloff PH, Kupfer DJ, et al. Depression in borderline patients: a prospective EEG sleep study. Psychiatry Res. 1985;14(1):1–15. doi: 10.1016/0165-1781(85)90084-8. [DOI] [PubMed] [Google Scholar]
- 3.Akiskal HS, Yerevanian BI, Davis GC, et al. The nosologic status of borderline personality: clinical and polysomnographic study. Am J Psychiatry. 1985;142(2):192–198. doi: 10.1176/ajp.142.2.192. [DOI] [PubMed] [Google Scholar]
- 4.Lahmeyer HW, Val E, Gaviria FM, et al. EEG sleep, lithium transport, dexamethasone suppression, and monoamine oxidase activity in borderline personality disorder. Psychiatry Res. 1988;25(1):19–30. doi: 10.1016/0165-1781(88)90154-0. [DOI] [PubMed] [Google Scholar]
- 5.Benson KL, King R, Gordon D, et al. Sleep patterns in borderline personality disorder. J Affect Disord. 1990;18(4):267–273. doi: 10.1016/0165-0327(90)90078-m. [DOI] [PubMed] [Google Scholar]
- 6.Battaglia M, Ferini-Strambi L, Smirne S, et al. Ambulatory polysomnography of never-depressed borderline subjects: a high-risk approach to rapid eye movement latency. Biol Psychiatry. 1993;33(5):326–334. doi: 10.1016/0006-3223(93)90321-4. [DOI] [PubMed] [Google Scholar]
- 7.Battaglia M, Ferini Strambi L, Bertella S, et al. First-cycle REM density in never-depressed subjects with borderline personality disorder. Biol Psychiatry. 1999;45(8):1056–1058. doi: 10.1016/s0006-3223(98)00213-3. [DOI] [PubMed] [Google Scholar]
- 8.De la Fuente JM, Bobes J, Vizuete C, et al. Sleep-EEG in borderline patients without concomitant major depression: a comparison with major depressives and normal control subjects. Psychiatry Res. 2001;105(1–2):87–95. doi: 10.1016/s0165-1781(01)00330-4. [DOI] [PubMed] [Google Scholar]
- 9.Asaad T, Okasha T, Okasha A. Sleep EEG findings in ICD-10 borderline personality disorder in Egypt. J Affect Disord. 2002;71(1–3):11–18. doi: 10.1016/s0165-0327(01)00357-3. [DOI] [PubMed] [Google Scholar]
- 10.De la Fuente JM, Bobes J, Morlán I, et al. Is the biological nature of depressive symptoms in borderline patients without concomitant Axis I pathology idiosyncratic? sleep EEG comparison with recurrent brief, major depression and control subjects. Psychiatry Res. 2004;129(1):65–73. doi: 10.1016/j.psychres.2004.05.025. [DOI] [PubMed] [Google Scholar]
- 11.Philipsen A, Feige B, Al-Shajlawi A, et al. Increased delta power and discrepancies in objective and subjective sleep measurements in borderline personality disorder. J Psychiatr Res. 2005;39(5):489–498. doi: 10.1016/j.jpsychires.2005.01.002. [DOI] [PubMed] [Google Scholar]
- 12.Ogiso Y, Moriya N, Ikuta N, et al. Relationship between clinical symptoms and EEG findings in borderline personality disorder. Jpn J Psychiatry Neurol. 1993;47(1):37–46. doi: 10.1111/j.1440-1819.1993.tb02027.x. [DOI] [PubMed] [Google Scholar]
- 13.Guilbert P, Nabet M, Leroy C. Sleep disorders in patients with personality disorders. Encephale. 1987;13(2):73–82. [PubMed] [Google Scholar]
- 14.Steiner M, Links PS, Korzekwa M. Biological markers in borderline personality disorders: an overview. Can J Psychiatry. 1988;33(5):350–354. doi: 10.1177/070674378803300507. [DOI] [PubMed] [Google Scholar]
- 15.Lahmeyer HW, Reynolds CF, 3rd, Kupfer DJ, et al. Biologic markers in borderline personality disorder: a review. J Clin Psychiatry. 1989;50(6):217–225. [PubMed] [Google Scholar]
- 16.Battaglia M, Ferini-Strambi L, Smirne S, et al. Cardiac autonomic function during sleep of never-depressed borderline subjects: a pilot study. J Psychiatr Res. 1995;29(5):397–405. doi: 10.1016/0022-3956(95)00012-t. [DOI] [PubMed] [Google Scholar]
- 17.Semiz UB, Basoglu C, Ebrinc S, et al. Nightmare disorder, dream anxiety, and subjective sleep quality in patients with borderline personality disorder. Psychiatry Clin Neurosci. 2008;62(1):48–55. doi: 10.1111/j.1440-1819.2007.01789.x. [DOI] [PubMed] [Google Scholar]
- 18.Buysse DJ, Reynolds CF, 3rd, Monk TH, et al. The Pittsburgh Sleep Quality Index: a new instrument for psychiatric practice and research. Psychiatry Res. 1989;28(2):193–213. doi: 10.1016/0165-1781(89)90047-4. [DOI] [PubMed] [Google Scholar]
- 19.Hyler S. Personality Diagnostic Questionnaire-4 (PDQ-4) New York, NY: New York State Psychiatric Institute; 1995. [Google Scholar]
- 20.Sansone RA, Wiederman MW, Sansone LA. The Self-Harm Inventory (SHI): development of a scale for identifying self-destructive behaviors and borderline personality disorder. J Clin Psychol. 1998;54(7):973–983. doi: 10.1002/(sici)1097-4679(199811)54:7<973::aid-jclp11>3.0.co;2-h. [DOI] [PubMed] [Google Scholar]
- 21.Dubro AF, Wetzler S, Kahn MW. A comparison of three self-report questionnaires for the diagnosis of DSM-III personality disorders. J Pers Disord. 1988;2:256–266. [Google Scholar]
- 22.Hyler SE, Lyons M, Rieder RO, et al. The factor structure of self-report DSM-III Axis II symptoms and their relationship to clinicians’ ratings. Am J Psychiatry. 1990;147(6):751–757. doi: 10.1176/ajp.147.6.751. [DOI] [PubMed] [Google Scholar]
- 23.Johnson JG, Bornstein RF. Utility of the Personality Diagnostic Questionnaire-Revised in a nonclinical sample. J Pers Disord. 1992;6:450–457. [Google Scholar]
- 24.Patrick J, Links P, Van Reekum R, et al. Using the PDQ-R BPD scale as a brief screening measure in the differential diagnosis of personality disorder. J Pers Disord. 1995;9:266–274. [Google Scholar]
- 25.Kolb JE, Gunderson JG. Diagnosing borderline patients with a semistructured interview. Arch Gen Psychiatry. 1980;37(1):37–41. doi: 10.1001/archpsyc.1980.01780140039004. [DOI] [PubMed] [Google Scholar]