Abstract
Aim
Few data exist to aid the clinician in prognosis after paediatric intracerebral haemorrhages (ICHs). Recently, ICH volume as a per cent of total brain volume (TBV) was shown to help predict outcomes in children. Thus, we sought to develop a bedside method of TBV estimation using typical hospital imaging software, and to validate the ABC/2 method for children in order to determine ICH volume and aid prognosis.
Method
The study group comprised 23 children and adolescents with non-traumatic, acute ICH who had undergone head computed tomography (CT) and who were available for analysis. The median age of participants, 14 males (61%) and nine females (39%), was 6 years (range 0–16y; mean 7.8y; SD 5.3y). Preterm infants born at less than 37 weeks’ gestation and term infants with pure intraventricular haemorrhages were excluded. Manual segmentation, which is the criterion standard for measurement of ICH volume and TBV, requires specialized software and is time-consuming. We therefore used the well-known ‘ABC/2 × slice thickness’ method to calculate ICH volume and TBV, thus allowing ICH size to be reported as a percentage of TBV regardless of the absolute size of ICH.
Results
The estimated ICH volume was highly accurate compared with the criterion standard (R2=0.97 and R2=0.93; combined R2=0.96), as was the estimated TBV (R2=0.89 and R2=0.77; combined R2=0.83). The interrater reliability was high for both ICH volume and TBV, with an intraclass correlation coefficient (ICC) of 0.94 and 0.80, respectively. Therefore, using no specialized software, we accurately measured ICH volume as a percentage of TBV.
Interpretation
The ABC/2 × slice thickness method is a possible bedside tool for the clinician that can aid prognosis after paediatric ICH.
What this paper adds.
This paper suggests an accurate method for determining intracerebral haemorrhage volume and total brain volume in children at the bedside using clinically available tools (standard imaging software and a calculator).
This study presents a tool for outcome prediction when patient care decisions must be made rapidly.
This paper compares the reported methods for rapid volume estimation.
In developed countries, stroke is among the top 10 causes of death in children.1 Non-traumatic haemorrhage accounts for almost 50% of stroke in children, although few studies have focused on it, and few data exist to aid in prognosis for the clinician.2 Intracerebral haemorrhage (ICH) volume is a strong predictor of poor outcome in adults, and recently the association has been shown both retrospectively and prospectively in children.3–5 In children, in contrast to adults, measurement of absolute ICH volume is not sufficient for prognosis because total brain volume (TBV) triples in childhood. For accurate comparison among haemorrhages, haemorrhage volume has been described as a percentage of TBV (ICH/TBV). Haemorrhages ≥2% of TBV (~30cm3 in adults) are associated with moderate neurological deficit,7 whereas an ICH volume ≥4% of TBV (~60cm3 in adults) is associated with death or vegetative state.4 Determining ICH volume using the criterion standard tracing method is slow; additionally, determining the TBV can take over an hour per patient, and both require special software. These issues restrict this useful association to research settings without further optimization.
To rapidly estimate ICH volume in adults, the ABC/2 method, a modification of the equation for ellipsoid volume, has been widely used by clinicians to assist in treatment decisions and to provide prognostic information6; however, ABC/2 is not commonly applied to ICH in children.7 In contrast to adult ICH, paediatric ICH is not usually caused by hypertension. Further, ICH morphology may differ from that of adults, possibly making this estimation method unfit. Using typical hospital imaging software, we sought to develop a method for bedside TBV estimation and to validate the ABC/2 method for children.
During the manuscript preparation phase of this study, Beslow et al. published a similar bedside method in a different cohort of children.7 This convergence of research shows that a shortcut method for ICH volume estimation in children is of interest, and may in the future be an important tool in patient care; therefore, we have added a comparison of the two methods to our study.
METHOD
Patient population
A retrospective hospital-based cohort of children with spontaneous ICH was identified by ICD-9 code. Children eligible for inclusion were term-born infants more than 28 days old up to adolescents <18 years old with non-traumatic, acute ICH who had undergone head CT and who were available for analysis.4 Preterm infants born at less than 37 weeks’ gestation and term-born infants with pure intraventricular haemorrhage were excluded. Thirty children were identified over a 5-year period and seven were excluded because their haemorrhage had a very large ventricular component.
Volume calculations
The ABC/2 volume estimation is based on a simplification of the ellipsoid volume equation. As described by Kothari et al.,6 to estimate ICH volume, A=maximum length (in cm), B=width perpendicular to A on the same head CT slice, and C=the number of slices multiplied by the slice thickness (Fig. 1). To estimate TBV, A=maximum length of the brain along the falx, B=maximum width of the brain (not necessarily measured on the same head CT slice as A), and C=number of head CT slices, starting from the point at which the temporal lobe tips became visible, multiplied by the slice thickness.
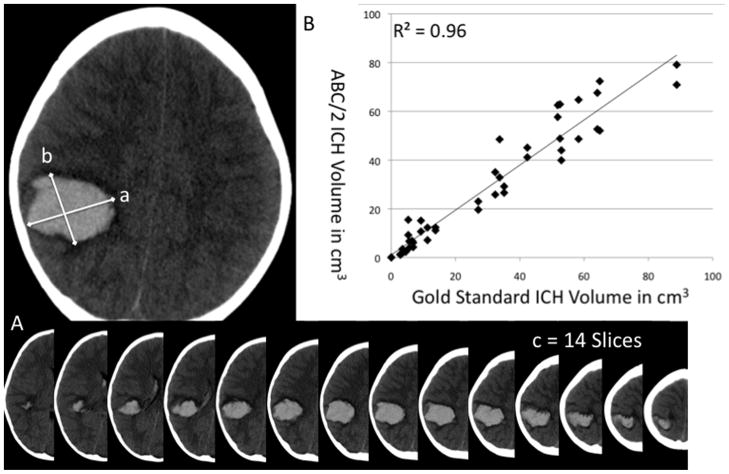
Figure 1.
(A) ABC/2 method for estimation of intracerebral haemorrhage (ICH) volume: maximum length (a), width perpendicular (b), number of slices (c). (B) Criterion standard ICH volume versus ABC/2.
To estimate TBV using XYZ/2, which is the Beslow method,7 X=maximum length of the brain, Y=largest diameter perpendicular to X, and Z=number of slices from the vertex to the foramen magnum.
Two raters used the ABC/2 method to calculate ICH and TBV. One rater used the alternative XYZ/2 method for comparing TBV because it has been shown to be reproducible with R2~0.96.7
Results were compared with the criterion standard method, manual slice-by-slice segmentation using ImageJ software (https://rsbweb.nih.gov/ij/download.html).
Statistical analysis
Interrater reliability for ABC/2 estimation of ICH volume and TBV was measured with intraclass correlation coefficients. Wilcoxon signed-rank tests were used to determine whether the estimated ABC/2 volumes and criterion standard manual segmentation volumes differed significantly. After log transformation of data to approximate a normal distribution, linear regression was performed to determine the correlation of the estimated measures with the volumetric measures. R2 was reported as the result. For sensitivity and specificity, haemorrhages were analysed in two sets: ≤2% of TBV versus >2%; and ≤4% of TBV versus >4% of TBV.4,5 Statistical analysis was performed using STATA version 11.0 (STATA Corp., College Station, TX, USA). The institutional review board approved this study.
RESULTS
ICH volume: ABC/2 versus criterion standard
In 23 children with a median age of 6 years (range 0–16y; mean 7.8y; SD 5.3y), 14 males (61%) and nine females (39%), the median ICH volume was determined to be 27cm3 (range 0.05–88cm3) using manual segmentation and 20cm3 (range 0.01–77cm3) using the ABC/2 method. Three patients with infratentorial haemorrhages were not excluded: all three had haemorrhages <0.5% of TBV, and one had ICH evacuation. Given the small sample, it is difficult to compare infra-and supratentorial ICH groups. There was no significant difference in measured volume using the Wilcoxon signed-rank test (median difference 7cm3; p=0.09). Correlation between log-transformed measurements of ICH volume obtained by ABC/2 and manual tracing was very high (rater 1, R2=0.97; rater 2, R2=0.93; combined, R2=0.96), as was interrater reliability with an ICC of 0.94 (95% confidence interval [CI] 0.89–0.99) (Fig. 1).
Total brain volume: ABC/2 versus criterion standard
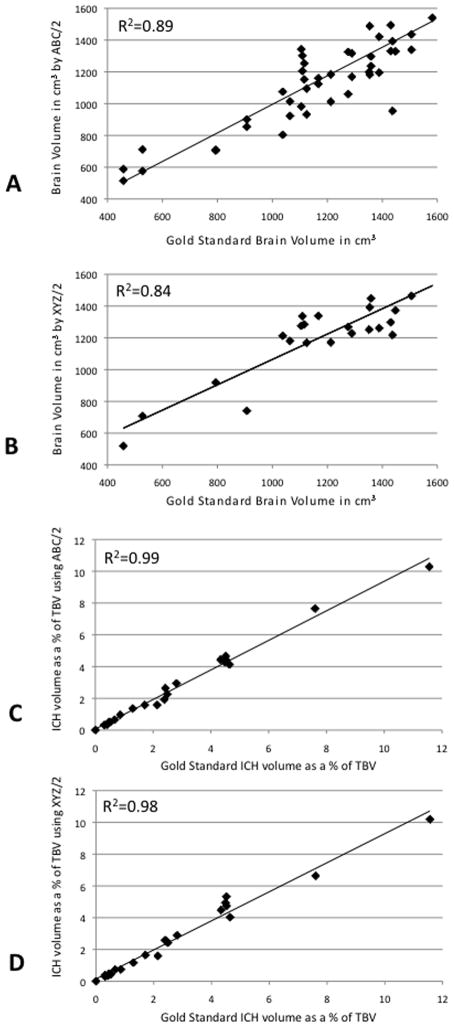
Median TBV was 1212cm3 by manual tracing (range 457–1582cm3) and 1202cm3 by ABC/2 (442–1837cm3). There was no statistical difference between manual tracing and ABC/2 using the Wilcoxon signed-rank test (median difference 10cm3; p=0.09). The correlation between log-transformed measurements of TBV by ABC/2 and manual tracing was good (R2=0.89 and R2=0.77) (Figure 2). The interrater reliability was high, with an ICC of 0.80 (95% CI: 0.66–0.95).
Figure 2.
Criterion standard method: (A) total brain volume (TBV) versus TBV estimation using ABC/2, (B) TBV versus TBV estimation using XYZ/2. (C) ICH as per cent of TBV versus per cent using ABC/2. (D) ICH as per cent of TBV versus per cent using XYZ/2.
ABC/XYZ comparison
Beslow et al.7 recently described a similar bedside method, termed ABC/XYZ, in a different cohort of children. We compared the two methods, which differ only in how TBV is calculated. The correlation between log-transformed TBV as determined by XYZ/2 and manual tracing was good (R2=0.84). Representing haemorrhage volume as a percentage of TBV, both methods perform extremely well compared with manual segmentation: using ABC/2, R2=0.99; using ABC/XYZ, R2=0.98 (Fig. 2).
Sensitivity and specificity: estimation versus manual segmentation
Patients with haemorrhages >4% of TBV have significantly increased odds of death or vegetative state,4 while patients with >2% of TBV have significantly increased odds of neurological deficit.7 The ABC/2 method categorized patients with 100% sensitivity and specificity for haemorrhages ≥4% of TBV, and 92% sensitivity and 100% specificity for haemorrhages ≥2% of TBV. The ABC/XYZ method categorized patients with 100% sensitivity and specificity for haemorrhages ≥4% of TBV, and 100% sensitivity and 92% specificity for haemorrhages ≥2% of TBV.
DISCUSSION
This study demonstrates that the rapid ‘ABC/2 × slice thickness’ method of estimating ICH volume may be applied to children. When extended to also calculate TBV, this method allows estimation of ICH volume and TBV, as well as calculation of haemorrhage volume as a percentage of TBV. Paediatric haemorrhage volumes and brain volumes can be calculated at any computer without special imaging software. The method is fast and accurate, and retains excellent sensitivity and specificity for categorizing patients as having haemorrhages ≥2% or ≥4% of TBV.
A comparison of the ABC/2 and ABC/XYZ methods of estimating ICH volume in children showed that both methods perform well. There was no clinically significant difference in either method for TBV estimation (R2=0.84–0.89), sensitivity, or specificity. Therefore, although the methods are slightly different, neither has a distinct advantage.
Larger studies are needed to more accurately correlate functional outcome with both ICH volume and ICH location. There were three infratentorial haemorrhages among the participants in our study, all of which were small (<0.5% TBV), and they did not seem to have a difference in outcomes, which contrasts with the findings of adult studies. Despite the limitations, this method will allow physicians to quickly calculate paediatric ICH volume at the bedside and adjust for TBV, therefore aiding in prognosis.
Acknowledgments
GRANT SUPPORT
This research was supported by K12 NCRR 017627 and K23 NS 062110 to LCJ.
LIST OF ABBREVIATIONS
- ICH
Intracerebral haemorrhage
- TBV
Total brain volume
Footnotes
DISCLOSURES AND FUNDING
None of the authors has any conflict of interest or disclosures.
References
- 1.National Center for Health Statistics. Deaths, percentage of total deaths, and death rates for the 10 leading causes of death in selected age groups, by race and sex: United States. 2005 [Internet] (cited 16 March 2010). Available from: http://cdc.gov/nchs/data/nvsr/nvsr58/nvsr58_08.pdf.
- 2.Fullerton HJ, Wu YW, Zhao S, Johnston SC. Risk of stroke in children: ethnic and gender disparities. Neurology. 2003;61:189–94. doi: 10.1212/01.wnl.0000078894.79866.95. [DOI] [PubMed] [Google Scholar]
- 3.Broderick JP, Brott TG, Duldner JE, Tomsick T, Huster G. Volume of intracerebral hemorrhage. A powerful and easy-to-use predictor of 30-day mortality. Stroke. 1993;24:987–93. doi: 10.1161/01.str.24.7.987. [DOI] [PubMed] [Google Scholar]
- 4.Jordan LC, Kleinman JT, Hillis AE. Intracerebral hemorrhage volume predicts poor neurologic outcome in children. Stroke. 2009;40:1666–71. doi: 10.1161/STROKEAHA.108.541383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Beslow LA, Storm PB, Licht DJ, et al. Predictors of outcome in childhood intracerebral hemorrhage: a prospective consecutive cohort study. Stroke. 2010;41:313–18. doi: 10.1161/STROKEAHA.109.568071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kothari RU, Brott T, Broderick JP, et al. The ABCs of measuring intracerebral hemorrhage volumes. Stroke. 1996;27:1304–5. doi: 10.1161/01.str.27.8.1304. [DOI] [PubMed] [Google Scholar]
- 7.Beslow LA, Ichord RN, Kasner SE, et al. ABC/XYZ estimates intracerebral hemorrhage volume as a percent of total brain volume in children. Stroke. 2010;41:691–4. doi: 10.1161/STROKEAHA.109.566430. [DOI] [PMC free article] [PubMed] [Google Scholar]