Abstract
We report a case of an 83-year-old gentleman presenting with acute low back pain and radicular left lower extremity pain after golfing. A magnetic resonance imaging (MRI) of the lumbar spine revealed a low-signal-density lesion compressing the L5 nerve. A computed tomography scan was then ordered, confirming an extra-foraminal disc protrusion at the L5–S1 level, containing a focus of gas that was compressing the left L5 nerve root and communicating with the vacuum disc at L5–S1. After a failed left L5 transforaminal epidural steroid injection, the patient was brought back for a percutaneous intradiscal aspiration of the vacuum disc gas. This resulted in immediate relief for the patient. A follow-up MRI performed 2 months after the procedure found an approximate 25% reduction in the size of the vacuum disc herniation. Six months after the procedure, the patient remains free of radicular pain. This case report suggests that a percutaneous aspiration of gas from a vacuum disc herniation may assist in the treatment of radicular pain.
Keywords: vacuum disc phenomenon, lumbar spine, intervertebral disc, epidural gas, percutaneous procedure
Introduction
Radiographic lucency in the intervertebral disc, also known as vacuum phenomenon is often observed on computed tomography (CT) and has been described by many authors [7, 8, 11, 19–21, 25, 26, 34, 35, 39]. Despite this, there are very few reports of patients who present with clinical symptoms of lumbar radiculopathy resulting from a disc protrusion containing a collection of gas [2–6, 17, 29, 31, 33, 36, 38]. We present magnetic resonance imaging (MRI), CT and fluoroscopic findings as well as a percutaneous treatment option for a case of symptomatic gas-filled herniation in a patient with an acute L5 radiculopathy.
Case report
An 83-year-old man with a 17-year history of chronic low back pain secondary to L4–5 spondylolisthesis managed conservatively presented with an acute onset of severe left leg pain. This was different from his prior symptoms and first appeared a few weeks prior to presentation after golfing and performing his lumbar flexion exercises at home.
His repeat physical exam revealed painful lumbar extension with increased radicular pain into the left leg, no dural tension signs and no focal neurologic deficits. Hip range of motion was near full and pain free. Gait was antalgic on the left.
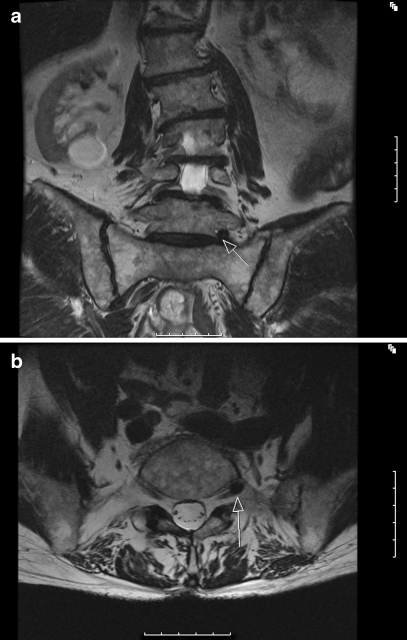
Due to the severe nature of the pain and limitations with mobility, an MRI study was obtained (Fig. 1a, b). This study demonstrated multi-level, severe degenerative disc disease with multi-level zygapophysial joint hypertrophy. At the L5–S1 level, there was a small mass demonstrating low signal intensity located in the exit zone of left neural foramen impinging the left L5 nerve root. Our initial impression was that this was a calcified disc fragment.
Fig. 1.
a, b A T2-weighted coronal MRI depicting a small mass demonstrating low signal intensity in the exit zone of left neural foramen impinging the left L5 nerve root
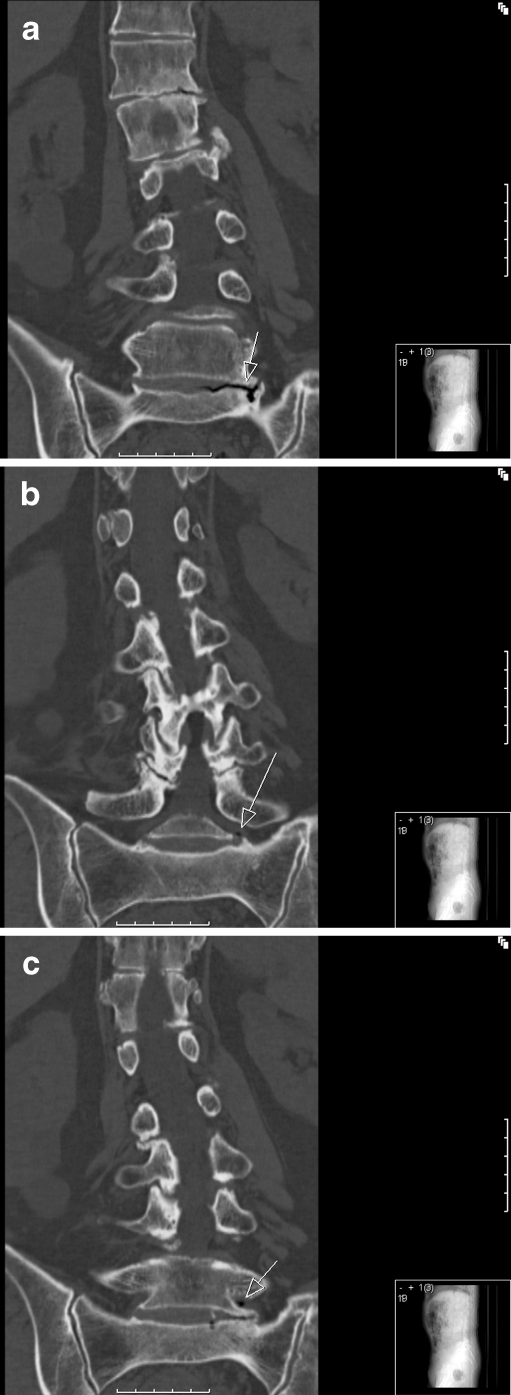
The patient underwent a fluoroscopic left L5 transforaminal epidural steroid injection (TFESI) with only minimal symptom relief. A CT scan of the lumbar spine was then obtained and demonstrated that the mass visualised on MRI was an extra-foraminal disc protrusion containing a focus of gas projecting into the exit zone of the left L5 nerve root with resulting impingement (Figs. 2 and 3).
Fig. 2.
This CT axial image demonstrates a small collection of gas located in the exit zone of left neural foramen impinging the left L5 nerve root
Fig. 3.
a–c These CT coronal images demonstrate gas within the disc and extending into the left neural foramen
Given these data, an attempt was made to percutaneously aspirate the focus of gas under fluoroscopic guidance. Following this procedure, the patient failed to have sustained relief of his symptoms and a repeat MRI failed to demonstrate any significant interval change in the size of the collection of gas. We then performed a discogram which demonstrated communication of the vacuum disc with the foraminal mass (Figs. 4 and 5). Aspiration from the intradiscal space was performed using a 10-cm3 glass syringe. A repeat fluoroscopic left L5 TFESI was then administered simultaneously with the intradiscal aspiration. The patient experienced immediate onset of pain relief. A follow-up (f/u) MRI was performed 2 months after the procedure, which found a reduction in the size of the gas bubble. Measurements were performed directly by a board-certified radiologist on high-resolution images using a PAC monitor and the area measurement tool. Measurements were taken of images (axial, coronal and sagittal) that were taken preaspiration (pre) and at follow-up. A decrease in area was found in two of the three planes. The areas were as follows: axial (pre, 41 mm2; f/u, 29 mm2), coronal (pre, 58 mm2; f/u, 47 mm2), sagittal (pre, 24 mm2; f/u, 24 mm2). Whilst the pocket of gas was not completely eliminated, its decrease in size correlated with an improvement in his clinical symptoms (Fig. 6). At 6 months post-procedure, the patient remains symptom free and continues to golf.
Fig. 4.
A lateral view on fluoroscopic imaging demonstrating intradiscal injection of contrast followed by aspiration
Fig. 5.
An AP view on fluoroscopic imaging demonstrating intradiscal injection of contrast outlining the gas-filled disc protrusion followed by aspiration
Fig. 6.
This T2-weighted axial MRI depicts a reduction in size of the small mass, demonstrating low signal intensity and decreased compression of the left L5 nerve root
Discussion
The “vacuum phenomenon” (VP) or intradiscal gas refers to the radiolucent visualisation of gaseous collections in the intervertebral disc space. It is formed by the accumulation of gas liberated from the surrounding tissue [7]. This finding was first described by Fick [24] in 1910. Magnusson [37] was the first to report this phenomenon in the intervertebral discs and described them as “vacuum intervertebral discs”. He postulated that the creation of space within the disc was subsequently filled by gas due to a reduction in barometric pressure. Historically, VP in the intervertebral disc has also been called “phantom nucleus pulposus” [25] and “intervertebral disc fissures” [26] in the medical literature. VP is frequently seen in degenerative disc disease, and Knuttson [39] was the first to correlate VP with disc degeneration in 1942. However, VP is also associated with infection, trauma, spinal injection procedures and metabolic disease [8, 9, 16, 22].
VP is a fairly common finding that can be observed in 1–3% of spinal radiographs [26, 34, 35]. However, the incidence may rise to 20% [25] with elderly individuals. Not surprisingly, it is observed in almost 50% [8, 21] of CT examinations of spine patients over the age of 40 years.
Although VP has been widely reported, reports of patients with nerve root compression and radicular symptoms associated with intraspinal gas have been rare. Gulati and Weinstein [12] postulated that intraspinal gas probably comes from tears in the annulus fibrosis in disc with VP. The gas can be associated with a herniation and can be found within the herniation itself [15, 18], or it can also be found free within the spinal canal, with or without herniation [12].
Anda [10] first described a 62-year-old with left L5 radiculopathy secondary to an intradural disc herniation with VP in 1987. In the subsequent year, he reported a 40-year-old patient with left L5 radiculopathy from a disc fragment with gas compressing the L5 nerve root at the exit zone of the neural foramen [5]. The first patient was treated surgically, and the second patient improved with conservative management.
Demierre et al. [36] reported a case of a 37-year-old male with left S1 radiculopathy from a gas-filled pseudocyst. Needle puncture under CT guidance as well as surgical puncture both failed to prevent recurrence. A second surgery with dissection and removal of the involved section of posterior longitudinal ligament was necessary for definitive treatment.
There are several other authors who have reported findings of nerve root compression due to a gas-filled disc herniation. However, most of these patients were treated surgically [1, 13, 14, 23, 27, 30, 32]. Righini and colleagues [28] reported two cases of patients with gas-filled lumbar disc herniations that were treated exclusively via percutaneous aspiration. One patient was treated under fluoroscopic guidance, and the other was treated under CT guidance. Although the authors were able to visualise the gas collection under CT guidance in the second patient, they had to assume that the needle was in the correct position for the first patient.
In our patient, using a percutaneous intradiscal approach with contrast allowed visualisation using a fluoroscopic technique. Our previous attempt using an ESI failed to resolve his radicular pain; however, the subsequent aspiration provided immediate and sustained relief from this rare cause of lumbar radiculopathy and obviated the need for any surgical intervention. A follow-up MRI performed 2 months after the procedure showed that the size of the vacuum disc herniation had decreased substantially in size. Although there was no complete resolution radiographically, clinically his pain resolved.
In the future, we would consider intradiscal aspiration as a first-line treatment if we encounter this rare condition again. This is the first reported case of using this technique in the management of patients with lumbar radiculopathy from a vacuum disc herniation, and this technique should be considered prior to surgical intervention.
Footnotes
Each author certifies that he or she has no commercial associations (e.g. consultancies, stock ownership, equity interest, patent/licencing arrangements, etc.) that might pose a conflict of interest in connection with the submitted article.
Each author certifies that his or her institution has approved the reporting of this case, that all investigations were conducted in conformity with ethical principles of research and that informed consent for participation in the study was obtained.
The study is a case report or individual case and therefore its level of evidence is a 3.
References
- 1.Anda S, Stovring J, Ro M. CT of extraforaminal disc herniation with associated vacuum phenomenon. Neuroradiology. 1988;30(1):76–77. doi: 10.1007/BF00341949. [DOI] [PubMed] [Google Scholar]
- 2.Beks JW, Weeme CA. Herniated lumbar discs in teenagers. Acta Neurochir (Wien) 1975;31(3–4):195–199. doi: 10.1007/BF01406292. [DOI] [PubMed] [Google Scholar]
- 3.Borgesen SE, Vang PS. Herniation of the lumbar intervertebral disk in children and adolescents. Acta Orthop Scand. 1974;45(4):540–549. doi: 10.3109/17453677408989177. [DOI] [PubMed] [Google Scholar]
- 4.Bradford DS, Garcia A. Lumbar intervertebral disk herniations in children and adolescents. Orthop Clin North Am. 1971;2(2):583–592. [PubMed] [Google Scholar]
- 5.Bulos S. Herniated intervertebral lumbar disc in the teenager. J Bone Joint Surg Br. 1973;55(2):273–278. [PubMed] [Google Scholar]
- 6.Burnei G, Gavriliu S, Vlad C, Georgescu I, Hurmuz L, Hodorogea D. Discal hernia in children and teenagers: medical, surgical and recovery treatment. Rom J Intern Med. 2006;44(4):477–481. [PubMed] [Google Scholar]
- 7.Cohen SP, Hurley RW, Christo PJ, Winkley J, Mohiuddin MM, Stojanovic MP. Clinical predictors of success and failure for lumbar facet radiofrequency denervation. Clin J Pain. 2007;23(1):45–52. doi: 10.1097/01.ajp.0000210941.04182.ea. [DOI] [PubMed] [Google Scholar]
- 8.Cohen SP, Stojanovic MP, Crooks M, et al. Lumbar zygapophysial (facet) joint radiofrequency denervation success as a function of pain relief during diagnostic medial branch blocks: a multicenter analysis. Spine J. 2008;8(3):498–504. doi: 10.1016/j.spinee.2007.04.022. [DOI] [PubMed] [Google Scholar]
- 9.Dreyfuss P, Halbrook B, Pauza K, Joshi A, McLarty J, Bogduk N. Efficacy and validity of radiofrequency neurotomy for chronic lumbar zygapophysial joint pain. Spine. 2000;25(10):1270–1277. doi: 10.1097/00007632-200005150-00012. [DOI] [PubMed] [Google Scholar]
- 10.Ebersold MJ, Quast LM, Bianco AJ., Jr Results of lumbar discectomy in the pediatric patient. J Neurosurg. 1987;67(5):643–647. doi: 10.3171/jns.1987.67.5.0643. [DOI] [PubMed] [Google Scholar]
- 11.Gibson MJ, Szypryt EP, Buckley JH, Worthington BS, Mulholland RC. Magnetic resonance imaging of adolescent disc herniation. J Bone Joint Surg Br. 1987;69(5):699–703. doi: 10.1302/0301-620X.69B5.3680327. [DOI] [PubMed] [Google Scholar]
- 12.Gofeld M, Jitendra J, Faclier G. Radiofrequency denervation of the lumbar zygapophysial joints: 10-year prospective clinical audit. Pain Physician. 2007;10(2):291–300. [PubMed] [Google Scholar]
- 13.Hidalgo-Ovejero AM, Martinez-Grande M, Garcia-Mata S. Disc herniation with gas. Spine (Phila Pa 1976). 1994;19(19):2210–2212. [DOI] [PubMed]
- 14.Kawaguchi S, Yamashita T, Ida K, Ikeda T, Ohwada O. Gas-filled intradural cyst of the lumbar spine. Case report. J Neurosurg. 2001;95(2 Suppl):257–259. doi: 10.3171/spi.2001.95.2.0257. [DOI] [PubMed] [Google Scholar]
- 15.Kornick C, Kramarich SS, Lamer TJ, Todd Sitzman B. Complications of lumbar facet radiofrequency denervation. Spine. 2004;29(12):1352–1354. doi: 10.1097/01.BRS.0000128263.67291.A0. [DOI] [PubMed] [Google Scholar]
- 16.Lau P, Mercer S, Govind J, Bogduk N. The surgical anatomy of lumbar medial branch neurotomy (facet denervation) Pain Med. 2004;5(3):289–298. doi: 10.1111/j.1526-4637.2004.04042.x. [DOI] [PubMed] [Google Scholar]
- 17.Luukkonen M, Partanen K, Vapalahti M. Lumbar disc herniations in children: a long-term clinical and magnetic resonance imaging follow-up study. Br J Neurosurg. 1997;11(4):280–285. doi: 10.1080/02688699746041. [DOI] [PubMed] [Google Scholar]
- 18.Manejias EM, Hu J, Tatli Y, Lutz GE. Lumbar zygapophysial joint radiofrequency denervation: a long-term clinical outcome study. HSS J. 2008;4(2):180–187. doi: 10.1007/s11420-008-9082-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Martinez-Lage JF, Fernandez Cornejo V, Lopez F, Poza M. Lumbar disc herniation in early childhood: case report and literature review. Childs Nerv Syst. 2003;19(4):258–260. doi: 10.1007/s00381-003-0720-6. [DOI] [PubMed] [Google Scholar]
- 20.Martinez-Lage JF, Martinez Robledo A, Lopez F, Poza M. Disc protrusion in the child. Particular features and comparison with neoplasms. Childs Nerv Syst. 1997;13(4):201–207. doi: 10.1007/s003810050069. [DOI] [PubMed] [Google Scholar]
- 21.Matsui H, Terahata N, Tsuji H, Hirano N, Naruse Y. Familial predisposition and clustering for juvenile lumbar disc herniation. Spine. 1992;17(11):1323–1328. doi: 10.1097/00007632-199211000-00011. [DOI] [PubMed] [Google Scholar]
- 22.Mikeladze G, Espinal R, Finnegan R, Routon J, Martin D. Pulsed radiofrequency application in treatment of chronic zygapophyseal joint pain. Spine J. 2003;3(5):360–362. doi: 10.1016/S1529-9430(03)00065-2. [DOI] [PubMed] [Google Scholar]
- 23.Mortensen WW, Thorne RP, Donaldson WF,3rd. Symptomatic gas-containing disc herniation. Report of four cases. Spine (Phila Pa 1976). 1991;16(2):190–192. [DOI] [PubMed]
- 24.Nath S, Nath CA, Pettersson K. Percutaneous lumbar zygapophysial (facet) joint neurotomy using radiofrequency current, in the management of chronic low back pain: a randomized double-blind trial. Spine. 2008;33(12):1291–1297; discussion 1298. [DOI] [PubMed]
- 25.Ozgen S, Konya D, Toktas OZ, Dagcinar A, Ozek MM. Lumbar disc herniation in adolescence. Pediatr Neurosurg. 2007;43(2):77–81. doi: 10.1159/000098377. [DOI] [PubMed] [Google Scholar]
- 26.Parisini P, Silvestre M, Greggi T, Miglietta A, Paderni S. Lumbar disc excision in children and adolescents. Spine. 2001;26(18):1997–2000. doi: 10.1097/00007632-200109150-00011. [DOI] [PubMed] [Google Scholar]
- 27.Pierpaolo L, Luciano M, Fabrizio P, Paolo M. Gas-containing lumbar disc herniation. A case report and review of the literature. Spine (Phila Pa 1976). 1993;18(16):2533–2536. [DOI] [PubMed]
- 28.Righini A, Lucchi S, Reganati P, Zavanone M, Bettinelli A. Percutaneous treatment of gas-containing lumbar disc herniation. Report of two cases. J Neurosurg. 1999;91(1 Suppl):133–136. doi: 10.3171/spi.1999.91.1.0133. [DOI] [PubMed] [Google Scholar]
- 29.Rugtveit A. Juvenile lumbar disc herniations. Acta Orthop Scand. 1966;37(4):348–356. doi: 10.3109/17453676608989425. [DOI] [PubMed] [Google Scholar]
- 30.Salpietro FM, Alafaci C, Collufio D, et al. Radicular compression by lumbar intraspinal epidural gas pseudocyst in association with lateral disc herniation. Role of the posterior longitudinal ligament. J Neurosurg Sci. 2002;46(2):93–95; discussion 95. [PubMed]
- 31.Shillito J., Jr Pediatric lumbar disc surgery: 20 patients under 15 years of age. Surg Neurol. 1996;46(1):14–18. doi: 10.1016/0090-3019(96)00035-3. [DOI] [PubMed] [Google Scholar]
- 32.Simonetti G, Martino V, Santilli S, Chiappetta F. Lumbar root compression by a gas-containing cyst in the extradural space. Case report. J Neurosurg Sci. 1992;36(2):101–102. [PubMed] [Google Scholar]
- 33.Smorgick Y, Floman Y, Millgram MA, Anekstein Y, Pekarsky I, Mirovsky Y. Mid- to long-term outcome of disc excision in adolescent disc herniation. Spine J. 2006;6(4):380–384. doi: 10.1016/j.spinee.2005.10.015. [DOI] [PubMed] [Google Scholar]
- 34.Boxem K, Eerd M, Brinkhuize T, Patijn J, Kleef M, Zundert J. Radiofrequency and pulsed radiofrequency treatment of chronic pain syndromes: the available evidence. Pain Pract. 2008;8(5):385–393. doi: 10.1111/j.1533-2500.2008.00227.x. [DOI] [PubMed] [Google Scholar]
- 35.Wijk RM, Geurts JW, Lousberg R, et al. Psychological predictors of substantial pain reduction after minimally invasive radiofrequency and injection treatments for chronic low back pain. Pain Med. 2008;9(2):212–221. doi: 10.1111/j.1526-4637.2007.00367.x. [DOI] [PubMed] [Google Scholar]
- 36.Varlotta GP, Brown MD, Kelsey JL, Golden AL. Familial predisposition for herniation of a lumbar disc in patients who are less than twenty-one years old. J Bone Joint Surg Am. 1991;73(1):124–128. [PubMed] [Google Scholar]
- 37.Zamani MH, MacEwen GD. Herniation of the lumbar disc in children and adolescents. J Pediatr Orthop. 1982;2(5):528–533. doi: 10.1097/01241398-198212000-00012. [DOI] [PubMed] [Google Scholar]
- 38.Zhu Q, Gu R, Yang X, Lin Y, Gao Z, Tanaka Y. Adolescent lumbar disc herniation and hamstring tightness: review of 16 cases. Spine. 2006;31(16):1810–1814. doi: 10.1097/01.brs.0000226047.83475.e4. [DOI] [PubMed] [Google Scholar]
- 39.Zucker L, Amacher AL, Eltomey A. Juvenile lumbar discs. Childs Nerv Syst. 1987;3(2):125–127. doi: 10.1007/BF00271141. [DOI] [PubMed] [Google Scholar]