Abstract
The development of iatrogenic nerve lesions during and following limb lengthening procedures present a challenge to orthopedic surgeons. Early treatment of nerve damage is critical in salvaging full function of the nerve. Precise location of damage, however, must be determined in order to appropriately administer treatment. We report a patient with a short humerus caused by a growth arrest undergoing a 7-cm lengthening who developed a neurapraxic injury of the radial nerve. Nerve compromise was noted 1 month into the lengthening program. Nerve conduction studies and electromyography could not be used to determine the precise site of injury. Likewise, magnetic resonance imaging and computed tomography were contraindicated and inconclusive, respectively, due to the presence of a metallic external fixation device. High-resolution ultrasonography (US) findings, however, correlated with our clinical examination of the patient's radial nerve function and permitted identification of the precise site of nerve involvement. Treatment was administered by removing a causative half-pin. Several days following treatment, nerve function returned to normal. There are a limited number of articles in the literature regarding nerve injuries associated with limb lengthening and their corrective treatments. The outcome of this case underscores the usefulness of US over various other diagnostic techniques under certain circumstances.
Keywords: ultrasound, neurapraxia, humeral lengthening, osteotomy, monolateral frame, distraction osteogenesis
Introduction
Peripheral nerve injury is a common complication that can be caused by a variety of surgical procedures [9, 19, 21]. The reported incidence of nerve damage during and following a limb lengthening procedure varies from 3% to 30% [1, 6–8, 10, 13, 18, 20, 22]. It is a particular concern in an orthopedic setting because it can lead to impairment of limb function. While the magnitude of correction and lengthening that can be tolerated by neurovascular structures has not yet been established, it is related to the amount of lengthening that nerves have to undergo, the rate of correction, and the anatomic relationship nerves have to their surrounding bones and soft tissues [3].
Electromyography (EMG) and nerve conduction studies (NCS) are generally used to diagnose nerve injury in order to determine severity and subsequent treatment [4, 5, 21]. Although EMG and NCS are useful diagnostic tools, they often fail in providing reliable information regarding the precise site of nerve involvement [17, 21]. Magnetic resonance (MR) imaging and computed tomography (CT) are useful in detecting lesions; however, they are problematic in that artifacts arising from metallic orthopedic hardware present an obstacle to obtaining an optimal image [15]. Moreover, use of MR imaging is expensive, contraindicated with most external fixation, and may not be readily available in some clinical settings [17].
Recent technological advancements in ultrasonography (US) have made it a useful and practical diagnostic tool in the identification and treatment of nerve injuries. High-resolution US has the ability to identify and differentiate a variety of lesions including nerve entrapments, nerve tumors, and traumatic nerve lesions [2, 11].
This article presents a case of radial nerve neurapraxia which developed during humeral lengthening with an EBI monolateral frame (EBI; Parsippany, NJ) and its treatment using US to detect the precise site of nerve involvement.
Case Report
A 50-year-old man presented with a unilateral short left humerus secondary to proximal humerus growth arrest. Functionally, the patient had restricted abduction of the left shoulder joint. He complained of difficulty reaching with the left arm and was unhappy with the deformity and asymmetry resulting from the shortening. The patient complained of pain in his left shoulder during activities, such as exercise and lifting, as well as with overhead abduction and flexion of the left shoulder joint. The patient had a limb length discrepancy of 8 cm (Fig. 1a, b). Range of motion of the left shoulder measured 20° of extension to 90° of flexion and 60° of abduction. Left elbow range of motion measured 0° of extension to 130° of flexion. Left wrist range of motion measured 70° of palmar flexion, 70° of dorsiflexion, 70° of supination, and 90° of pronation. Radial, median, and ulnar nerve motor and sensory examinations were assessed as within normal limits. Motor examination of the left side was noted as 5/5 motor power of the upper limb and hand. There was possible history of trauma as a child, although patient could not fully recall. It is likely, however, that a childhood infection affecting his proximal humerus resulted in growth arrest and joint damage. The patient had received no past treatment for the deformity. He had no significant medical history, and a review of systems was otherwise without pertinence.
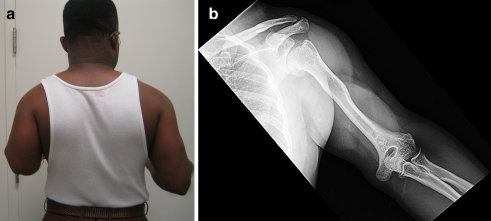
Fig. 1.
a A preoperative photograph from behind the patient demonstrates the difference in humeral lengths. b This radiograph is an anteroposterior (AP) view of the short left humerus
The patient was treated by a gradual lengthening of the left humerus using the principal of distraction osteogenesis with an EBI monolateral frame (EBI; Parsippany, NJ). For the initial surgery, regional anesthesia was administered via an interscalene block, without use of any paralytic agent so that any potential irritation of the radial nerve could still be observed intraoperatively. The frame was mounted using four 6-mm hydroxyapatite-coated half-pins. These pins were placed percutaneously; two were placed proximally, just below the head of the humerus, and two distally, just proximal to the olecranon fossa. A multiple drill hole transverse osteotomy of the humerus was performed. Distraction started on the eighth day after surgery at a rate of 1/4 turn corresponding to 1/4 mm, four times daily. Immediately following surgery and again at the first postoperative visit, the neurologic exam was normal.
At 25-days of follow-up, X-rays showed a distraction gap of 16 mm with good bone formation. There was no indication of deformity, dislocation, fracture, or loosening of the fixator pins. The patient complained of patchy numbness on the dorsum of his left hand. Clinical examination revealed decreased sensation on the dorsum of the patient's left hand across the first and second metacarpals, an area of approximately 1 × 1 cm. Motor function was 4/5 of his wrist and thumb extension. Elbow extension was 5/5. The patient had a negative Tinel's sign. Elbow and shoulder range of motions had not changed. He was instructed to slow the rate of distraction down to 1/2 mm per day.
At 32-day follow-up, X-rays showed a distraction gap of 18 mm and indicated early bone formation. Motor function remained 4/5, and his extensor pollicis longus was 4/5. Elbow extension was 5/5. Despite slowing the distraction rate, radial nerve function had not improved. There was no pain referable to the nerve. He was otherwise able to flex his fingers and thumb well. Elbow and shoulder range of motions had not changed. MRI could not be done due to the presence of an external fixator. CT was performed but was not helpful. Multiple contiguous computed tomographic axial images were obtained from the proximal humerus to the elbow joint at 0.8 mm slice intervals and reformatted in the coronal and sagittal planes. Assessment, however, was compromised due to streak artifact, which limited an evaluation of the position of the distal screws to the position of the radial nerve.
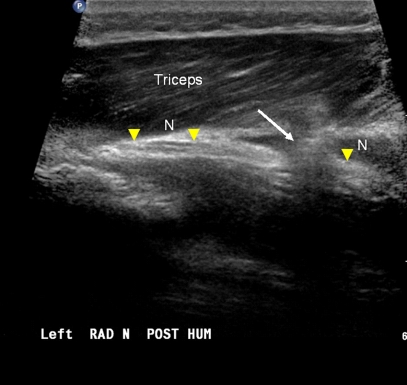
Ultrasound was performed with an IU22 scanner (Philips Medical) used with an L12-5 linear phased array transducer. Findings indicated that of the two distal pins in the limb distraction device, the more proximal pin was seen to come in close proximity to the radial nerve as it passed along the lateral margin of the humerus. There was extensive perineural scar reaction seen in this location which in part encompassed the nerve. The margin of the pin was seen to abut the radial nerve as it passed posteriorly to anteriorly (Fig. 2).
Fig. 2.
a. The longitudinal sonogram depicting the radial nerve in long axis (N) on either side of the pin and adjacent scar reaction (arrow). The latter presents as a distortion of the adjacent fat planes and muscle. The triceps muscle is labeled
The frame was modified in order to relieve the scar reaction. A half-pin was placed just distal to the most distal half-pin in a posterolateral to anteromedial direction. It was then attached to the frame. Following this, the implicated causative half-pin, which was initially the proximal of the distal half-pins, was removed (Fig. 3a, b). Lengthening was continued.
Fig. 3.
a This radiograph is an AP view of humerus prior to performing surgery to reposition the more proximal of the distal pins. b This radiograph is an AP view obtained following repositioning of the pin. Note the altered placement and configuration of the distal half-pins attached to the monolateral frame
At 28-days of follow-up after repositioning of the fixator pin, X-rays showed a distraction gap of 40 mm with good bone formation. Patient stated that sensation to the dorsal aspect of his left hand completely returned. Sensory clinical examination indicated no deficit and was normal. Extensor pollicis longus was 5/5 and wrist extension and flexion were 5/5. Upon completion of distraction, a total of 7 cm length was achieved (Fig. 4a, b). Extensor pollicis longus remained 5/5, and wrist extension and flexion both remained 5/5. Patient remained in the frame for a total of 6 months and 20 days. At 11-day follow-up after frame removal, review of X-rays showed excellent healing of the regenerate. Clinical examination indicated that all incisions were healed completely, and there was no swelling or edema of the left upper extremity. Neurologic function was normal. At 4-month follow-up after frame removal, the patient had equal limb lengths (Fig. 5a–d). Elbow range of motion measured 0° to 130°. The patient regained all of his preoperative shoulder range of motion.
Fig. 4.
a This radiograph depicts an AP view at end of distraction showing 7 cm of lengthening with regenerate formation. b The clinical photograph obtained at the end of lengthening
Fig. 5.
a A clinical photograph obtained at 4 months of follow-up after frame removal showing equal humeral lengths. b A clinical photograph obtained at 4 months follow-up after frame removal showing maximum elbow flexion and the actively extended thumb. c The AP radiographic view taken at 4 months follow-up after frame removal. d The lateral view obtained at 4 months follow-up after frame removal
Discussion
Iatrogenic nerve lesions present a challenge to orthopedic surgeons. It is a complication associated with limb lengthening [13, 19] as nerves are forced to stretch along with other anatomic structures. A nerve might also become compromised as a result of the use of fixation devices placed near the nerve itself [14]. Whether nerve damage is caused directly during surgery or secondary to naturally occurring postoperative complications (e.g., excessive scar formations and hematomas [21]), early treatment is critical in salvaging full function of the nerve. Selection of treatment is contingent upon the etiology and severity of nerve damage [1] as well as its precise location [14].
Reliable and readily available diagnostic tools greatly enhance a physician's ability to determine the type of nerve lesion and the localization of an injury. Earlier surgical intervention to treat injuries increases the likelihood of a shorter recovery time and overall recovery of nerve function [19, 21]. Although EMG and NCS are useful diagnostic tools, they often fail in providing reliable information regarding the precise site of nerve involvement [17, 21]. MRI and CT are helpful; however, they are expensive, often not readily available [17], and are not optimal in the presence of metallic objects [15] (i.e., external fixators and internal implants).
Advanced high-resolution US can be used to identify and differentiate a variety of nerve lesions [2, 11]. Several reports indicate its successful application in the assessment and localization of nerve damage [4, 11, 14, 16, 17, 21]. Successful application of US for the purpose of identifying nerve lesions has been reported due to its high detection rate and accuracy, its low cost, wide availability, and ease of use [16]. Although it becomes difficult to identify various non-superficial nerves solely with US [16, 17], several studies indicate its advantageous utilization in the detection and localization of nerves in the upper extremities [2, 4, 12, 14].
In this case, a patient undergoing lengthening of the left humerus developed a scar reaction adjacent to an area encompassing the radial nerve as a result of the placement of a half-pin serving to stabilize a monolateral rail frame. EMG and NCS were not feasible in determining the localization of the compromised nerve. Likewise, MRI was not feasible due to the presence of a metallic external fixation device. A CT scan was done but was not helpful. US findings, on the other hand, corresponded with our clinical examination of the patient's radial nerve function. The causative half-pin was identified, subsequently removed, and a new one was inserted more distally, avoiding further irritation of the nerve. Rapid improvement of motor and sensory function of the radial nerve resulted from pin repositioning allowing the patient to continue with the lengthening program.
There are a limited number of articles in the literature regarding nerve injuries during and after limb lengthening and their corrective treatments. The outcome of this case underscores the usefulness of US over various other diagnostic techniques under certain circumstances. Its addition to an orthopedic surgeon's repertoire of diagnostic tools enhances his or her ability to determine treatment quickly and effectively in cases of suspected nerve injury, particularly with regard to limb lengthening.
Footnotes
Each author certifies that he or she has no commercial associations (e.g., consultancies, stock ownership, equity interest, patent/licensing arrangements, etc.) that might pose a conflict of interest in connection with the submitted article.
Each author certifies that all investigations were conducted in conformity with ethical principles of research and that informed consent for participation in the study was obtained.
References
- 1.Atar D, Lehman WB, Grant AD, Strongwater A, Frankel V, Golyakhovsky V. Treatment of complex limb deformities in children with the Ilizarov technique. Orthopedics. 1991;14:961–967. doi: 10.3928/0147-7447-19910901-07. [DOI] [PubMed] [Google Scholar]
- 2.Bodner G, Huber B, Schwabegger A, Lutz M, Waldenberger P. Sonographic detection of radial nerve entrapment within a humerus fracture. J Ultrasound Med. 1999;18:703–706. doi: 10.7863/jum.1999.18.10.703. [DOI] [PubMed] [Google Scholar]
- 3.Chuang TY, Chan RC, Chin LS, Hsu TC. Neuromuscular injury during limb lengthening: a longitudinal follow-up by rabbit tibial model. Arch Phys Med Rehabil. 1995;76:467–470. doi: 10.1016/S0003-9993(95)80580-X. [DOI] [PubMed] [Google Scholar]
- 4.Cokluk C, Aydin K. Ultrasound examination in the surgical treatment for upper extremity peripheral nerve injuries: part I. Turk Neurosurg. 2007;17:277–282. [PubMed] [Google Scholar]
- 5.Cokluk C, Aydin K. Ultrasound examination in the surgical treatment of lower extremity peripheral nerve injuries: part II. Turk Neurosurg. 2007;17:197–201. [PubMed] [Google Scholar]
- 6.Coleman SS. Simultaneous femoral and tibial lengthening for limb length discrepancies. Arch Orthop Trauma Surg. 1985;103:359–366. doi: 10.1007/BF00435441. [DOI] [PubMed] [Google Scholar]
- 7.Coleman SS, Stevens PM. Tibial lengthening. Clin Orthop Relat Res. 1978;136:92–104. [PubMed] [Google Scholar]
- 8.Dahl MT, Gulli B, Berg T. Complications of limb lengthening. A learning curve. Clin Orthop Relat Res. 1994;301:10–18. [PubMed] [Google Scholar]
- 9.Eggli S, Hankemayer S, Muller ME. Nerve palsy after leg lengthening in total replacement arthroplasty for developmental dysplasia of the hip. J Bone Joint Surg Br. 1999;81:843–845. doi: 10.1302/0301-620X.81B5.9610. [DOI] [PubMed] [Google Scholar]
- 10.Eldridge JC, Bell DF. Problems with substantial limb lengthening. Orthop Clin North Am. 1991;22:625–631. [PubMed] [Google Scholar]
- 11.Fornage BD. Sonography of peripheral nerves of the extremities. Radiol Med. 1993;85:162–167. [PubMed] [Google Scholar]
- 12.Foxall GL, Skinner D, Hardman JG, Bedforth NM. Ultrasound anatomy of the radial nerve in the distal upper arm. Reg Anesth Pain Med. 2007;32:217–220. doi: 10.1016/j.rapm.2007.02.006. [DOI] [PubMed] [Google Scholar]
- 13.Galardi G, Comi G, Lozza L, Marchettini P, Novarina M, Facchini R, Paronzini A. Peripheral nerve damage during limb lengthening. Neurophysiology in five cases of bilateral tibial lengthening. J Bone Joint Surg Br. 1990;72:121–124. doi: 10.1302/0301-620X.72B1.2298769. [DOI] [PubMed] [Google Scholar]
- 14.Karabay N, Toros T, Ademoglu Y, Ada S. Ultrasonographic evaluation of the iatrogenic peripheral nerve injuries in upper extremity. Eur J Radiol. 2008. (in press). [DOI] [PubMed]
- 15.Lee MJ, Kim S, Lee SA, Song HT, Huh YM, Kim DH, Han SH, Suh JS. Overcoming artifacts from metallic orthopedic implants at high-field-strength MR imaging and multi-detector CT. Radiographics. 2007;27:791–803. doi: 10.1148/rg.273065087. [DOI] [PubMed] [Google Scholar]
- 16.Martinoli C, Bianchi S, Dahmane M, Pugliese F, Bianchi-Zamorani MP, Valle M. Ultrasound of tendons and nerves. Eur Radiol. 2002;12:44–55. doi: 10.1007/s00330-001-1161-9. [DOI] [PubMed] [Google Scholar]
- 17.Martinoli C, Bianchi S, Derchi LE. Ultrasonography of peripheral nerves. Semin Ultrasound CT MR. 2000;21:205–213. doi: 10.1016/S0887-2171(00)90043-X. [DOI] [PubMed] [Google Scholar]
- 18.Nogueira MP. Obstacles in limb lengthening: nerve problems. In: Rozbruch SR, Ilizarov S, editors. Limb lengthening and reconstruction surgery. New York: Informa Healthcare; 2007. pp. 669–675. [Google Scholar]
- 19.Nogueira MP, Paley D, Bhave A, Herbert A, Nocente C, Herzenberg JE. Nerve lesions associated with limb-lengthening. J Bone Joint Surg Am. 2003;85-A:1502–1510. doi: 10.2106/00004623-200308000-00011. [DOI] [PubMed] [Google Scholar]
- 20.Paley D. Problems, obstacles, and complications of limb lengthening by the Ilizarov technique. Clin Orthop Relat Res. 1990;250:81–104. [PubMed] [Google Scholar]
- 21.Peer S, Bodner G, Meirer R, Willeit J, Piza-Katzer H. Examination of postoperative peripheral nerve lesions with high-resolution sonography. AJR Am J Roentgenol. 2001;177:415–419. doi: 10.2214/ajr.177.2.1770415. [DOI] [PubMed] [Google Scholar]
- 22.Velazquez RJ, Bell DF, Armstrong PF, Babyn P, Tibshirani R. Complications of use of the Ilizarov technique in the correction of limb deformities in children. J Bone Joint Surg Am. 1993;75:1148–1156. doi: 10.2106/00004623-199308000-00004. [DOI] [PubMed] [Google Scholar]