Abstract
Iodine deficiency (ID) is the world's single most important preventable cause of brain damage and mental retardation. Iodine deficiency disorders (IDDs) is a public health problem in 130 countries, affecting 13% of the world population. The simplest solution to prevent the IDD is to consume iodized common salt every day. In India, significant progress has been achieved toward elimination of IDD, in the last 30 years. Satisfactory levels of urinary iodine excretion and iodine content of salt have been documented by the research surveys conducted by research scientists. The results indicate that we are progressing toward elimination of IDD. IDD is due to a nutritional deficiency, which is prima-rily that of iodine, in soil and water. IDD is known to re-appear if the IDD Control Program is not sustained. To ensure that the population continues to have intake of adequate amount of iodine, there is a need of i) periodic surveys to assess the magnitude of the IDD with respect to impact of iodized salt (IS) intervention; ii) strengthening the health and nutrition education activities to create demand for IS and iii) development of a monitoring information system (MIS) for ensuring that the adequately IS is available to the beneficiaries.
Keywords: Goiter, iodine, salt, urinary iodine excretion
Introduction
Iodine deficiency (ID) is the single most important preventable cause of brain damage.(1) Iodine deficiency disorders (IDDs) refer to all of the consequences of ID in a population, which can be prevented by ensuring that the population has an adequate intake of iodine. Iodine is one of the essential elements. Its daily per capita requirement is 150 µg. Iodine is required for the synthesis of the thyroid hormones, thyroxine (T4 ) and triiodothyronine (T3). Iodine is present in the superficial layers of the soil and absorbed by crops grown on it. Glaciations, heavy snow and heavy rain leach away iodine from the soil. This problem is further accelerated by deforestation and soil erosion. Consumption of crops and plants grown on iodine-deficient soils leads to ID in populations solely dependent on this vegetation for their iodine requirements. When iodine intake falls below the recommended levels, the thyroid may no longer be able to synthesize sufficient amounts of thyroid hormones. The resulting low level of thyroid hormones in the blood (hypothy-roidism) is the principal factor responsible for damage to the developing brain of fetus.(2)
ID causes its impact right from the development of fetus to people of all age groups. It results in abortion, stillbirth, mental retardation, deaf-mutism, squint, dwarfism, goiter of all ages, neuromotor defects, etc. ID directly affects human resource development, which in turn greatly affects the human productivity and country′s development at large. People living in areas affected by severe ID may have an intelligence quotient (IQ) of up to 13.5 points below that of those from comparable communities in areas where there is no ID.(3)
Magnitude of IDD
IDD constitutes a major nutrition deficiency disorder in India. The survey conducted by the central and state health directorates, Indian Council of Medical Research and medical colleges have demonstrated that not even a single state is free from the problem of IDD. Out of 582 districts in the country, district level surveys conducted in 324 districts have revealed that IDD is a major public health problem in 263 districts, i.e. a total goiter prevalence rate of 10% and more in the population.(4) Realizing the magnitude of the problem, the Government of India launched a 100% centrally assisted National Goitre Control Programme (NGCP) in 1962. In 1992, the NGCP was renamed as NIDDCP. The program has the following objectives:(4)
initial surveys to assess the magnitude of the IDDs;
supply of iodized salt (IS) in place of common salt; and
resurveys to assess the impact of IS after every 5 years.
The Government of India under the Prevention of Food Adulteration Act (PFA) has defined that IS should have a minimum of 30 ppm iodine at the production level and a minimum of 15 ppm at the retail trader level. India has adopted a policy of Universal Salt Iodization (USI) in 1983 to ensure that all edible salt for human and animal con-sumption is iodized. The major activities undertaken under the program include i) production and distribution of IS; ii) establishment of goiter cell in all states and UTs; iii) information education and communication activities to increase the consumption of IS; iv) to achieve effective inter-sectoral coordination amongst various government sectors participating in implementation of NIDDCP; v) laboratory support for assessing iodine content of salt and urinary iodine excretion (UIE) levels estimation; vi) training of health functionaries in IDD at different levels; and vii) establishment of monitoring and reporting system for NIDDCP.(4)
Progress achieved toward elimination of IDD in India
According to World Health Organization (WHO), to assess progress toward elimination of IDD, the following two activities should be undertaken: i) measurement of UIE levels and ii) analysis of the iodine content of salt. The data available on these two aspects from India reflect the success story.
Status of UIE in India
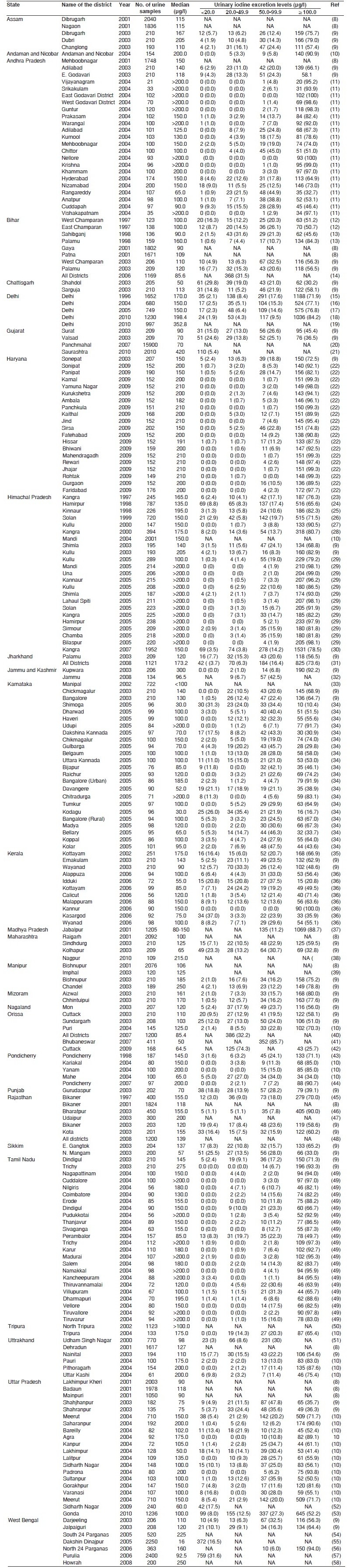
In a community with optimal iodine nutriture, the median UIE levels should be in the range of 100-200 µg/l.(5) The status of UIR levels in different regions of country has been extensively assessed by district level surveys in the recent years [Table 1]. More than 86% of districts had median UIE levels of 100 mcg/l, indicating success of NIDDCP.
Table 1.
Urinary iodine excretion levels in selected districts of India
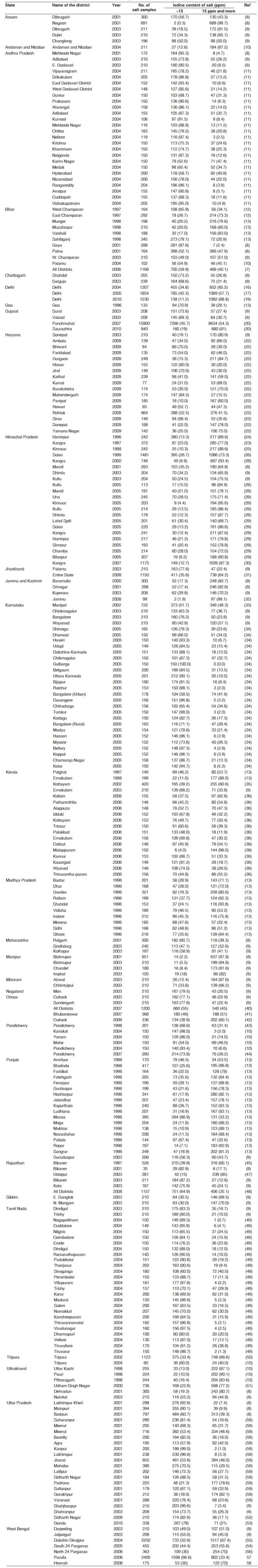
Status of iodine content of salt in India
The level of salt iodization should provide a physiological intake of 100-150 µg/day, which should bring the median UIE level within a range of 100-200 µg/l. To achieve this, 30 ± 10 ppm iodine needs to be added to salt at the manufacturing level.(5) The status of salt iodization in different districts of the country has been extensively assessed in the recent years. Table 2 depicts the same. More than 58% of districts had an iodine content of salt of 15 ppm and more at beneficiary level, indicating success of Universal Salt Iodization Program activity in the country.
Table 2.
Iodine content of salt samples collected at beneficiary level in selected districts of India
A countrywide evaluation conducted under NFHS-3, in 2005-2006 measured the iodine content of cooking salt [Table 3]. Overall, 49% of the households used salt that was iodized at the recommended level of 15 ppm or more. About 22% salt was inadequately iodized i.e. less than 15 ppm. It was found that the use of IS varied dramatically from one state to another. The use of IS was high (90% and more) in the northeastern region where salt is transported by railways. However, all the states in the southern region had low levels of use of adequately IS, ranging from only 21% in Tamil Nadu to 43% in Karnataka.(6)
Table 3.
Percent distribution of households with salt tested for iodine content, by level of iodine in salt (parts per million), according to state, India, 2005-06:NFHS-3
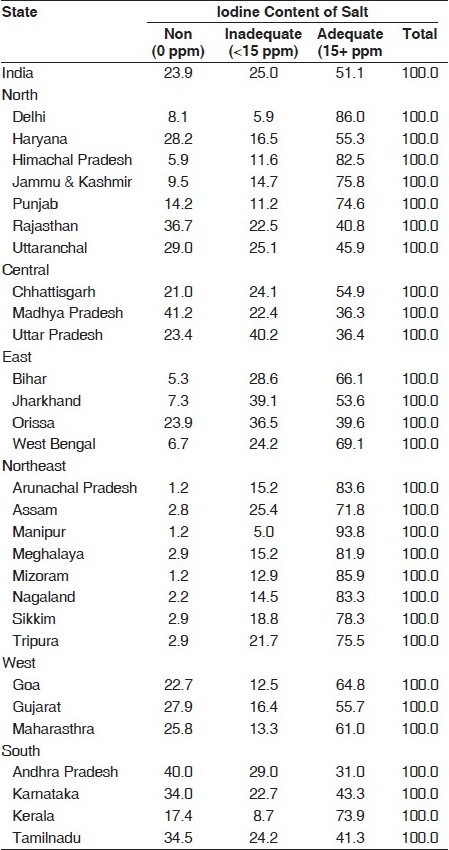
The salt department, under its monitoring information system, receives reports from State Health Authorities. During 2005, the reports received from 12 states revealed that 73.7% of IS tested by State Health Laboratories under State Health Department were adequately iodized (15 ppm and more iodine).(7)
Contribution of salt department in the success of NIDDCP
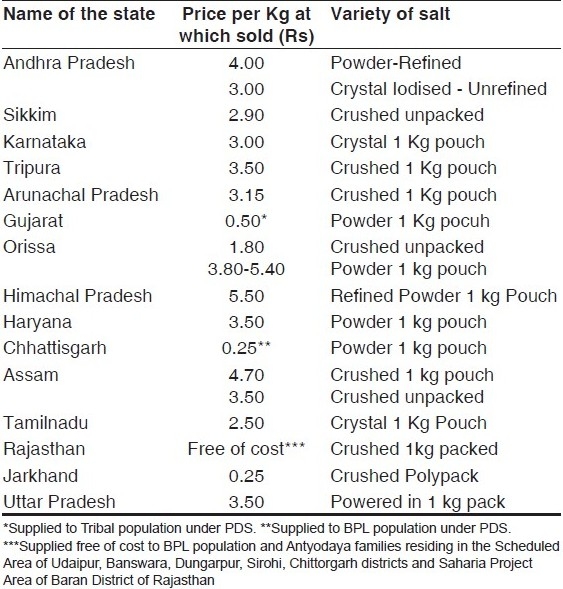
The production of IS in country was about 0.2 million tons in 1983. This had increased to about 5.3.million tons in 2009. There are 807 salt iodization units including 42 refineries, which have a total installed capacity of production of 116 lakh tons. This capacity established is more than double the requirement of salt for human consumption in the country. The Salt Department has facilitated the establishment of 18 potassium iodate manufacturing units to help salt producers to iodize the salt. The sustained joint efforts of NIDDCP and Salt Department have ensured that IS is distributed through Public Distribution System for below the poverty line (BPL) population in the 15 states of the country [Table 4].(7)
Table 4.
States undertaking distribution of iodized salt through public distribution system
Areas requiring strengthening to achieve the elimination of IDD
A high priority is needed to be given to the NIDDCP by the state governments to prevent irregular distribution of IS.
Adequate enforcement of PFA by the state/UT governments is required to ensure that the quality of IS is available to the beneficiary.
Adequate coordination is required between salt traders and food inspectors in the states (the implementers of PFA) for smooth procurement, distribution and sale of IS.
There are three states which have not implemented the ban notification in all the districts on sale of non-IS. This is helping the sale of non-IS. There is need of implementing complete ban in the entire state.
There is a need of undertaking regular periodic surveys for monitoring of UIE levels and assessing the iodine contents of salt. This would help in identifying the areas with poor iodine content of salt and initiating the remedial measures.
In southern states that have high level of literacy but there is resistance for the consumption of IS, qualitative research is required for identification of points of resistance toward consumption of IS.
IS versus iodized oil in the prevention of IDD
The inexpensive technology, a time-honored and time-tested one, for the control of IDD is the iodization of common salt. Programs for IDD control must rest squarely and socially on this technology. Periodic parenteral administration of iodated oil (not presently manufactured in India) at times is suggested as an alternative approach, especially in areas inaccessible to common salt. It is difficult to imagine any area in India, which is now inaccessible to common salt but readily accessible to disposable syringes and to an army of “injectors”. There has been a steep rise in the HIV seropositivity rate and hepatitis "B" carriers in India during the last few years. The consequences of resorting to a technology that is dependent on repeated injections could increase the risk of transmission of HIV and hepatitis B and is not recommended.
Conclusion
The sustainability of activities of NIDDCP is vital for achieving elimination of IDD. The subjects with large goiter are no more seen. The hidden consequences like neonatal hypothyroidism in specific areas may possibly continue. There is a need of undertaking IDD surveys to assess the current incidence of neonatal hypothyroidism. There is a need to give more emphasis on impact of ID on loss of IQ points in school children and their poor scholastic performance.
IDD is a nutritional deficiency that prima-rily results from deficiency of iodine in soil and water. IDD can therefore re-emerge at any time after its elimination, if program success is not sus-tained. There is evidence that ID is returning to some countries where it had been eliminated in the past. Hence, we need continued efforts for all time to come in the future.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
References
- 1.Bleichrodt N, Born MA. A meta-analysis of research on iodine and its relationship to cognitive development. In: Stanbury J, editor. The damaged brain of iodine deficiency: Cognitive, behavioral, neuromotor, and educative aspects. New York: Cognizant Communication Cor-poration; 1994. pp. 195–200. [Google Scholar]
- 2.Umesh K. Iodine deficiency disorders, Chapter in the Recent advances in Pediatrics. In: Gupte S, editor. New Delhi: Jaypee Brothers; 1998. pp. 310–27. [Google Scholar]
- 3.Umesh K. National Nutrition Programmes in India in child Nutrition-The Indian Scene. In: Mehta MN, Kulkarni M, editors. Bombay, India: Sai Creation and Advertising Co. printing Press; 1991. pp. 78–107. [Google Scholar]
- 4.Tiwari BK, Ray I, Malhotra RL. New Delhi: 2006. Policy Guidelines on National Iodine Deficiency Disorders Control Programme-Nutrition and IDD Cell.Directorate of Health Services, Ministry of Health and Family Welfare; pp. 1–22. Government of India. [Google Scholar]
- 5.Delange F, Robertson A, McLoughney E, Gerasimov G. Geneva: World Health organization; 1998. Elimination of iodine deficiency disorders in Central and Eastern Europe, the Commonwealth of independent states, and the Baltic states.Proceeding of a Conference held in Munich, Germany, 3-6 Sep 1997. [Google Scholar]
- 6.International Institute for Population Sciences (IIPS) and ORC Macro National Family Health Survey (NFHS 3) 2005-2006. Mumbai IIPS; New Delhi: Ajanta Offset and Packagings Limited; 2006. pp. 260–90. [Google Scholar]
- 7.Annual Report of Salt Department 2008-2009. Jaipur: Salt Department Press; pp. 23–39. Salt Commissioner, Post Box No 139, Lavan Bhawan, Lavan Marg, Jaipur. [Google Scholar]
- 8.Micronutrient Deficiency disorders in 16 Districts of India. Part 1 Report of an ICMR Task Force Study-District Nutrition Project Indian Council of Medical research.New Delhi: Gowarsons publishers Privarte limited; 2001. New Delhi: Gowarsons publishers Privarte limited; 2001. pp. 16–8. [Google Scholar]
- 9.Current Status of IDD in select Districts of different regions of country. National Institute of Nutrition. Hyderabad: NIN Press; 2003. pp. 11–28. [Google Scholar]
- 10.Kapil U, Singh P. Current status of urinary iodine excretion levels in 116 districts of India. J Trop Pediatr. 2004;50:245–7. doi: 10.1093/tropej/50.4.245. [DOI] [PubMed] [Google Scholar]
- 11.Kapil U, Singh P, Pathak P. Current status of iodine nutriture and iodine content of salt in Andhra Pradesh. Indian Pediatr. 2004;41:165–9. [PubMed] [Google Scholar]
- 12.Kapil U, Singh J, Prakash R, Sundaresan S, Ramachandran S, Tandon M. Assessment of iodine deficiency in selected blocks of east and west Champaran districts of Bihar. Indian Pediatr. 1997;34:1087–91. [PubMed] [Google Scholar]
- 13.Kapil U, Nayar D. Dr P C Sen Memorial Award Paper Status of salt iodisation and iodine deficiency in selected districts of different states of India. Indian J Public Health. 1998;42:75–80. [PubMed] [Google Scholar]
- 14.Sankar R, Moorthy D, Pandav CS, Tiwari JS, Karmarkar MG. Tracking progress towards sustainable elimination of iodine deficiency disorders in Bihar. Indian J Pediatr. 2006;73:799–802. doi: 10.1007/BF02790389. [DOI] [PubMed] [Google Scholar]
- 15.Kapil U, Saxena N, Ramachandran S, Balamurugan A, Nayar D, Prakash S. Assessment of iodine deficiency disorders using the 30 cluster approach in the National Capital Territory of Delhi. Indian Pediatr. 1996;33:1013–7. [PubMed] [Google Scholar]
- 16.Kapil U, Sethi V, Goindi G, Pathak P, Singh P. Elimination of iodine deficiency disorders in Delhi. Indian J Pediatr. 2004;71:211–2. doi: 10.1007/BF02724271. [DOI] [PubMed] [Google Scholar]
- 17.Kapil U, Singh P. Combating iodine deficiency in national capital territory of delhi, India--lessons learnt. J Trop Pediatr. 2005;51:62–3. doi: 10.1093/tropej/fmh079. [DOI] [PubMed] [Google Scholar]
- 18.Agarwal J, Pandav CS, Karmarkar MG, Nair S. Community monitoring of the National Iodine Deficiency Disorders Control Programme in the National Capital Region of Delhi. Public Health Nutr. 2010;1:1–4. doi: 10.1017/S1368980010000297. [DOI] [PubMed] [Google Scholar]
- 19.Marwaha RK, Tandon N, Desai A, Kanwar R, Mani K. Iodine nutrition in upper socioeconomic school children of Delhi. Indian Pediatr. 2010;47:335–8. doi: 10.1007/s13312-010-0063-9. [DOI] [PubMed] [Google Scholar]
- 20.Misra S, Kantharia SL, Damor JR. Prevalence of goitre in 6 -12 years school-going children of Panchmahal district in Gujarat, India. Indian J Med Res. 2007;126:475–9. [PubMed] [Google Scholar]
- 21.Chudasama RK, Verma PB, Mahajan RG. Iodine nutritional status and goiter prevalence in 6-12 years primary school children of Saurashtra region, India. World J Pediatr. 2010;6:233–7. doi: 10.1007/s12519-010-0221-0. [DOI] [PubMed] [Google Scholar]
- 22.Kapil U. Urinary iodine excretion levels amongst schoolchildren in Haryana. Indian Pediatr. 2009;46:57–97. [PubMed] [Google Scholar]
- 23.Kapil U, Saxena N, Ramachandran S, Sharma TD, Nayar D. Status of iodine deficiency in selected blocks of Kangra District, Himachal Pradesh. Indian Pediatr. 1997;34:338–40. [PubMed] [Google Scholar]
- 24.Sohal KS, Sharma TD, Kapil U, Tandon M. Assessment of iodine deficiency disorders in district Hamirpur, Himachal Pradesh. Indian Pediatr. 1998;35:1008–11. [PubMed] [Google Scholar]
- 25.Kapil U, Sharma NC, Ramachandran S, Nayar D, Vashisht M. Iodine deficiency in district Kinnaur, Himachal Pradesh. Indian J Pediatr. 1998;65:451–3. doi: 10.1007/BF02761141. [DOI] [PubMed] [Google Scholar]
- 26.Sohal KS, Sharma TD, Kapil U, Tandon M. Current status of prevalence of goiter and iodine content of salt consumed in District Solan, Himachal Pradesh. Indian Pediatr. 1999;36:1253–6. [PubMed] [Google Scholar]
- 27.Kapil U. Status of urinary iodine excretion in post salt iodization phase in selected districts of India. Indian Pediatr. 2000;37:1282–4. [PubMed] [Google Scholar]
- 28.Kapil U, Sohal KS, Sharma TD, Tandon M, Pathak P. Assessment of iodine deficiency disorders using the 30 cluster approach in district Kangra, Himachal Pradesh, India. J Trop Pediatr. 2000;46:264–6. doi: 10.1093/tropej/46.5.264. [DOI] [PubMed] [Google Scholar]
- 29.Kapil U, Sharma TD, Singh P, Dwivedi SN, Kaur S. Thirty years of a ban on the sale of noniodized salt: Impact on iodine nutrition in children in Himachal Pradesh, India. Food Nutr Bull. 2005;26:255–8. doi: 10.1177/156482650502600301. [DOI] [PubMed] [Google Scholar]
- 30.Kapil U, Sharma TD, Singh P. Iodine status and goiter prevalence after 40 years of salt iodisation in the Kangra District, India. Indian J Pediatr. 2007;74:135–7. doi: 10.1007/s12098-007-0005-2. [DOI] [PubMed] [Google Scholar]
- 31.Patro BK, Saboth P, Zodpey S, Shukla A, Karmarkar MG, Pandav CS. Tracking progress toward elimination of iodine deficiency disorders in Jharkhand, India. Indian J Community Med. 2008;33:182–5. doi: 10.4103/0970-0218.42061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Bhat IA, Pandit IM, Mudassar S. Study on Prevalence of lodine Deficiency Disorder and Salt Consumption Patterns in Jammu Region. Indian J Community Med. 2008;33:11–4. doi: 10.4103/0970-0218.39236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Rao RS, Kamath R, Das A, Nair NS, Keshavamurthy Prevalence of goitre among school children in coastal Karnataka. Indian J Pediatr. 2002;69:477–9. doi: 10.1007/BF02722647. [DOI] [PubMed] [Google Scholar]
- 34.Kapil U, Singh P, Dwivedi SN. Status of iodine deficiency amongst school children in twenty four districts in southern India. Indian J Physiol Pharmacol. 2005;49:369–72. [PubMed] [Google Scholar]
- 35.Kapil U, Jayakumar PR, Singh P, Aneja B, Pathak P. Assessment of iodine deficiency in Kottayam district, Kerala State: A pilot study. Asia Pac J Clin Nutr. 2002;11:33–5. doi: 10.1046/j.1440-6047.2002.00241.x. [DOI] [PubMed] [Google Scholar]
- 36.Kapil U, Singh P, Dwivedi SN, Pathak P. Status of iodine nutriture and universal salt iodisation at beneficiaries levels in Kerala State, India. J Indian Med Assoc. 2006;104:165–7. [PubMed] [Google Scholar]
- 37.Gakkhar RK, Bhardwaj VK, Chansoria M, Jain S, Visnoi R. Prevalence of goitre in school-going children in Jabalpur. Indian J Pediatr. 2001;68:229–33. doi: 10.1007/BF02723195. [DOI] [PubMed] [Google Scholar]
- 38.Menon KC, Skeaff SA, Thomson CD, Gray AR, Ferguson EL, Zodpey S, et al. Concurrent micronutrient deficiencies are prevalent in nonpregnant rural and tribal women from central India. Nutrition. 2010. Available from: http://www.ncbi.nlm.nih.gov/pubmed/20558038. Last accessed on 2010 Oct 7 . [DOI] [PubMed]
- 39.Kapil U, Singh P. Status of Iodine content of salt and urinary iodine excretion levels in India. Pak J Nutrition. 2003;2:361–73. [Google Scholar]
- 40.Moorthy D, Patro BK, Das BC, Sankar R, Karmakar MG, Pandav CS. Tracking progress towards sustainable elimination of iodine deficiency disorders in Orissa. Indian J Public Health. 2007;51:211–5. ICCIDD. [PubMed] [Google Scholar]
- 41.Sethy PG, Bulliyya G, Mallick G, Swain BK, Kar SK. Iodine deficiency in urban slums of Bhubaneswar. Indian J Pediatr. 2007;74:917–21. doi: 10.1007/s12098-007-0169-9. [DOI] [PubMed] [Google Scholar]
- 42.Panigrahi A. Iodine status of women in reproductive age group in urban slums of Cuttack City, Orissa. Indian J Public Health. 2009;53:34–6. [PubMed] [Google Scholar]
- 43.Kapil U, Ramachandran S, Tandon M. Assessment of iodine deficiency in Pondicherry. Indian Pediatr. 1998;35:357–9. [PubMed] [Google Scholar]
- 44.Mohanty B, Basu S, Sarkar S. Estimation of salt iodine in Pondicherry District. Indian J Public Health. 2007;51:77–8. [PubMed] [Google Scholar]
- 45.Bhardwaj AK, Nayar D, Ramachandran S, Kapil U. Assessment of iodine deficiency in district Bikaner, Rajasthan. Indian J Matern Child Health. 1997;8:18–20. [PubMed] [Google Scholar]
- 46.Kapil U, Singh P, Pathak P, Singh C. Assessment of iodine deficiency disorders in district Bharatpur, Rajasthan. Indian Pediatr. 2003;40:147–9. [PubMed] [Google Scholar]
- 47.Pradhan R, Choudhry M. Assessment of iodine deficiency disorders in urban areas of Udaipur District, Rajasthan. Indian Pediatr. 2003;40:406–9. [PubMed] [Google Scholar]
- 48.Ategbo EA, Sankar R, Schultink W, van der Haar F, Pandav CS. An assessment of progress toward universal salt iodization in Rajasthan, India, using iodine nutrition indicators in school-aged children and pregnant women from the same households. Asia Pac J Clin Nutr. 2008;17:56–62. [PubMed] [Google Scholar]
- 49.Kapil U, Singh P, Dwivedi SN, Pathak P. Profile of iodine content of salt and urinary iodine excretion levels in selected districts of Tamil Nadu. Indian J Pediatr. 2004;71:785–7. doi: 10.1007/BF02730711. [DOI] [PubMed] [Google Scholar]
- 50.Chandra AK, Ray I. Evaluation of the effectiveness of salt iodization status in Tripura, north east India. Indian J Med Res. 2002;115:22–7. [PubMed] [Google Scholar]
- 51.Mittal M, Tandon M, Raghuvanshi RS. Iodine status of children and use of iodized salt in Tarai region of North India. J Trop Pediatr. 2000;46:300–2. doi: 10.1093/tropej/46.5.300. [DOI] [PubMed] [Google Scholar]
- 52.Chandra AK, Bhattacharjee A, Malik T, Ghosh S. Etiological factors for the persistence of endemic goiter in selected areas of Siddharthnagar district in Eastern Uttar Pradesh, India. J Pediatr Endocrinol Metab. 2009;22:317–25. doi: 10.1515/jpem.2009.22.4.317. [DOI] [PubMed] [Google Scholar]
- 53.Yadav S, Gupta SK, Godbole MM, Jain M, Singh U, Pavithran VP, et al. Persistence of severe iodine-deficiency disorders despite universal salt iodization in an iodine-deficient area in Gonda northern India. Public Health Nutr. 2010;13:424–9. doi: 10.1017/S1368980009990280. [DOI] [PubMed] [Google Scholar]
- 54.Chandra AK, Tripathy S, Ghosh D, Debnath A, Mukhopadhyay S. Iodine nutritional status and prevalence of goitre in Sundarban delta of South 24-Parganas, West Bengal. Indian J Med Res. 2005;122:419–24. [PubMed] [Google Scholar]
- 55.Das DK, Chakraborty I, Biswas AB, Sarkar GN, Shrivastava P, Sen S. Iodine deficiency disorders among school children of Dakshin Dinajpur District, West Bengal. Indian J Public Health. 2005;49:68–72. [PubMed] [Google Scholar]
- 56.Sen TK, Biswas AB, Chakrabarty I, Das DK, Ramakrishnan R, Manickam P, et al. Persistence of iodine deficiency in Gangetic flood-prone area, North 24-Parganas West Bengal, India. Asia Pac J Clin Nutr. 2006;15:528–32. [PubMed] [Google Scholar]
- 57.Biswas AB, Chakraborty I, Das DK, Roy RN, Ray S, Kunti SK. Assessment of iodine deficiency disorders in Purulia district, West Bengal, India. J Trop Pediatr. 2006;52:288–92. doi: 10.1093/tropej/fml003. [DOI] [PubMed] [Google Scholar]
- 58.Chandra AK, Debnath A, Tripathy S. Iodine nutritional status among school children in selected areas of Howrah District in West Bengal, India. J Trop Pediatr. 2008;54:54–7. doi: 10.1093/tropej/fmm063. [DOI] [PubMed] [Google Scholar]
- 59.Kapil U, Tondon M, Pathak P, Pradhan R. Assessment of current status of salt iodization at the beneficiary level in selected districts of Uttar Pradesh, India. Indian Pediatr. 2001;38:654–7. [PubMed] [Google Scholar]


