Introduction
Human immunodeficiency virus (HIV) is known to increase the morbidity and mortality among people with tuberculosis (TB).(1,2) Various systemic complications due to HIV among cases of TB have been reported.(3–8) But, there is paucity of information quantifying the risk of systemic complications due to HIV among cases of TB. A pair-matched case-control study comparing cases of HIV-TB co-infection with TB would help in quantifying the risk. Thus, this study was undertaken in one of the tertiary care referral centers of coastal South India.
Materials and Methods
A hospital record-based pair-matched case-control study was undertaken after obtaining the required consent from the institutional ethics committee in two tertiary care hospitals of Kasturba Medical College, Mangalore, Karnataka State.
Operational definitions
TB was confirmed bacteriologically (i.e., smear-positive for acid fast bacilli) and HIV status was confirmed by the criteria established by the National AIDS Control Organization (NACO), India. (9)Cases were patients of HIV-TB co-infection irrespective of age and gender. Controls were patients of TB. All those cases and controls whose records were available with the hospital for the last 1 year were included in the study.
Sample size
Using the formula N = (Zα+Zβ)2(p1q1+p2q2)/(p2-p1)2.p1and p2were assumed to be 56% and 10%, respectively.(10,11) With a power of 0.01 and a precision set at 0.05, we got 14 cases. With a ratio of four controls for each case, we had to get 56 pair-matched controls.
Sampling
The list of cases fulfilling the eligibility criteria was made. The cases were then categorized according to age, sex and the following confounding factors, i.e. smoking, alcoholism, diabetes mellitus, hypertension, chronic obstructive pulmonary diseases (COPD) and malignancies. A similar list of controls for the same period was prepared. By simple random sampling, 14 cases were obtained. From a similar list for controls, 56 controls pair-matched for age, gender and confounding factors was obtained.
Matching
Age was matched in 5-year intervals. The gender was also matched. The following confounding factors were matched, i.e. smoking, alcoholism, diabetes mellitus, hypertension, COPD and malignancies.
Study instrument
A semi-structured proforma was used to collect the basic details of the patients (like name, age, sex, occupation, socioeconomic status) and for the categorization of cases and controls, Co-morbidities and complications were devised after pretesting and were used for data collection.
Analysis
Odds ratios were computed to quantify the risk of complications using the formula,
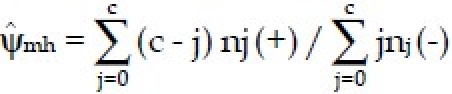
where “nj (+)” denotes the number of matched sets in which case is (+) and exactly “j” of controls are (+). Similarly, “nj(−)” denotes the number of matched sets in which case is (−) and exactly “j” of controls are (+).(12)
Results
Patient characteristics
The number of cases according to age groups in years (numbers in each age group) is as follows: 0-18 (1), 19-49 (7), 50-70 (4) and >71 (2).
Gender
Males (11) and females (3).
Occupation
Manual laborers (6), business men (2), semiskilled workers (5) and student (1).
Distribution of confounding factors
Smokers (2), alcoholics (2), diabetics (3), hypertension (1), COPD (1) and oral cancer (1). The confounding factors were matched. Controls with oral cancer were of different stages.
The morbidity profile along with the odds ratios are presented in Table 1.
Table 1.
Morbidity profile of cases and controls along with the odds ratios
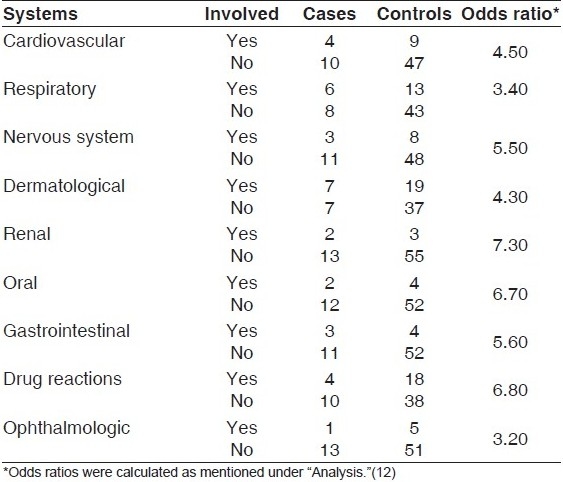
Some of the complications like cytomegalovirus retinitis, renal calculus, urinary tract infection, candidiasis, cholecystitis, splenomegaly, gastroenteritis, scabies, impetigo, Tinea corporis, Herpes Zoster, cryptococcal meningitis and tubercular meningitis, pericardial effusion, drug reactions (pancreatitis, peripheral neuropathy, anemia, gastritis and metabolic acidosis) were found exclusively among cases as compared with controls.
Discussion
We could not get comparable studies. In a retrospective cohort study,(2) it was found that the case fatality rate was higher among HIV-TB co-infection as compared with TB cases after adjusting for confounding factors. We found that a higher proportion of the cases was males and in the middle-aged group. Higher morbidity among the middle-aged group and males has been reported from USA.(13) A higher proportion among males may be because of underdetection among females.(14) Economic compulsions and stigma associated with HIV may be a barrier for the detection of HIV-TB co-infection.(15)
Case-control studies with small numbers and only hospital-based controls make interpretations difficult. Being a tertiary care center, the referred patient profiles may not be representative, creating a bias. Because of paucity of information, this study gives inputs to plan further prospective cohort studies required to arrive at relative and attributable risks.
Acknowledgments
We acknowledge the financial support from the Indian Council of Medical Research (ICMR) under the research initiative, Short Term Studentship (STS), for this study.
Footnotes
Source of Support:Indian Council of Medical Research (ICMR) under the research initiative, Short Term Studentship (STS),
Conflict of Interest: None declared.
References
- 1.Global tuberculosis control: Surveillance, planning, financing, WHO Report. Geneva; 2008. [last cited on 2009 Jun 4]. World Health Organisation. Available from: http://www.who.int/tb/publications/global_report/2009/pdf/chapter1.pdf . [Google Scholar]
- 2.Churchyard GJ, Kleinschmidt I, Corbett EL, Murray J, Smith J, De Cock KM, et al. Factors associated with an increased case-fatality rate in HIV-infected and non-infected South African gold miners with pulmonary tuberculosis. Int J Tuberc Lung Dis. 2000;4:705–12. [PubMed] [Google Scholar]
- 3.Salami AK, Katibi IA. Human immunodeficiency virus-associated tuberculosis: Pattern and trend in the University of Ilorin Teaching Hospital. Afr J Med Med Sci. 2006;35:457–60. [PubMed] [Google Scholar]
- 4.Kassu A, Mengistu G, Ayele B, Diro E, Mekonnen F, Ketema D, et al. Coinfection and clinical manifestations of tuberculosis in human immunodeficiency virus-infected and uninfected adults at a teaching hospital, northwest Ethiopia. J Microbiol Immunol Infect. 2007;40:116–22. [PubMed] [Google Scholar]
- 5.Wells CD, Cegielski JP, Nelson LJ, Laserson KF, Holtz TH, Finlay A, et al. HIV infection and multidrug resistance tuberculosis: The perfect storm. J Infect Dis. 2007;15:86–107. doi: 10.1086/518665. [DOI] [PubMed] [Google Scholar]
- 6.Swaminathan S, Paramasivan CN, Ponnuraja C, Iliyas S, Rajasekaran S, Narayanan PR. Antituberculosis drug resistance in patients with HIV and tuberculosis in south India. Int J Tuberc Lung Dis. 2005;9:896–900. [PubMed] [Google Scholar]
- 7.Kumar A, Upadhyay S, Kumari G. Clinical presentation, treatment outcome and survival among the HIV infected children with culture confirmed tuberculosis. Curr HIV Res. 2007;5:499–504. doi: 10.2174/157016207781662434. [DOI] [PubMed] [Google Scholar]
- 8.Kauban C, Bercion R, Koulla-Shiro S. HIV seroprevelance rate and incidence of adverse skin reactions in adults with pulmonary tuberculosis receiving thiacetazone free anti-tuberculosis treatment in Yaounde, Cameroon. East Afr Med J. 1997;74:474–7. [PubMed] [Google Scholar]
- 9.National AIDS Control organization- Guidelines on HIV testing. [last accessed on 2009 Jun 5]. Available from: http://www.nacoonline.org/Quick_Links/Publication/Blood_Safety__Lab_Services/Operational__Technical_guidelines_and_policies/Guidelines_for_HIV_test/
- 10.Telzak EE. Tuberculosis and human immunodeficiency virus infection. Med Clin North Am. 1997;81:345–60. doi: 10.1016/s0025-7125(05)70521-6. [DOI] [PubMed] [Google Scholar]
- 11.Ray D, Abel R. Incidence of smear-positive tuberculosis from 1981-83 in a rural population of south india. Tuber Lung Dis. 1995;76:190–5. doi: 10.1016/s0962-8479(05)80003-6. [DOI] [PubMed] [Google Scholar]
- 12.Schlesselman JJ. Chapter 6, Unit 7.8. New York: Oxford University Press; 1982. Case-Control Studies: Design, Conduct, Analysis; pp. 216–20. [Google Scholar]
- 13.Albalak R, O'Brien RJ, Kammerer JS, O'Brien SM, Marks SM, Castro KG, et al. Trends in tuberculosis/human immunodeficiency virus comorbidity, United States, 1993-2004. Arch Intern Med. 2007;167:2443–52. doi: 10.1001/archinte.167.22.2443. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Cassels A, Heineman E, LeClerq S, Gurung PK, Rahut CB. Tuberculosis case finding in eastern Nepal. Tubercle. 1982;63:175–85. doi: 10.1016/s0041-3879(82)80028-7. [DOI] [PubMed] [Google Scholar]
- 15.Harsha Kumar HN, Jayaram S, Ramakrishna RM, Ganesh SK, Kotian MS. Recent trends in HIV incidence in coastal South India: Implications for prioritising HIV control strategies. Open Med. 2009;3:26–30. [PMC free article] [PubMed] [Google Scholar]


