Introduction
Malaria is one of the major public health problem in the developing world and accounts for 300 to 500 million cases and more than 1 millions deaths annually.(1,2) India is one of the highly endemic countries and reports about 1.8 millions cases per year, of which 40-50% are due to Plasmodium falciaprum.(3) Early and complete treatment based on correct diagnosis can prevent complications and deaths.(4,5) Microscopy is the most accurate and relative inexpensive tool and considered gold standard for malaria diagnosis,(6) but it is not always possible in remote field conditions. As per National Vector Borne Disease Control Programme (NVBDCP) estimates, about 40% of the cases occur in the difficult outreach areas, where microcopy results cannot reach within 24 hours.(7) Hence for these areas use of RDKs has been advocated. However these RDKs are quite expensive as well as temperature sensitive and require certain environment specification for proper functioning.(6,7) Hence for proper use and stock management of RDKs field staff including MPWs and ASHAs needs training and constant supervision.
Chhattisgarh is a tribal dominated state of central India (Census 2001)(8) with high malarial burden,(3) had the case load of 1, 23495, in the year 2008.(9,10) The major area of concern continues to be the high proportion of Plasmodium falciaprum cases (70-80%)(9) in the last many years. To reduce the case burden and mortality, World Bank has identified 11 high endemic, of total 16 districts in the state, for first phase of its intervention project.(7) Govt of India too has supplied RDKs (for diagnosis of Plasmodium falciaprum cases), with the intension of providing early diagnosis in remote inaccessible areas of the state. The Present analysis has been undertaken to assess the use of RDKs by district health authorities, of Chhattisgarh, as per the GOI guidelines.
Materials and Methods
The report presents the finding from six district of Chhattisgarh about, the use of RDKs. The data was collected by survey of each district, lasting for five days during the years 2009 and 2010. Survey teams each consisting of two experienced field staff and a team leader (Doctor), visited different health facilities, namely community health centers (CHCs), primary health centers (PHCs) and health subcenters (HSCs), so as to include three to four CHCs, five to eight PHCs and 8 to 14 HSCs from each district. Selection of health facilities was based on the malaria burden (Annual Parasite Index and pf %) as well as approachability and operational feasibility for the survey. Thus the number of health facilities was not uniform for all surveyed districts. During the survey all the available health staffs were interviewed, records were scrutinized and stock of RDKs (if any available), was checked. The information was recorded on the schedules which were predesigned and tested in field. Visits were also made in the remotest villages, to interview four to five ASHAs from each of the district. During the interview ASHAs were enquired about the availability and use of RDKs and blood slides. They were also asked to demonstrate the use of RDKs and blood slides to record their actual skills.
Results
As show in Table 1, the survey included information from 19 (39.6% of total, in surveyed districts) CHCs, 34 (15.4% of total in surveyed districts) PHCs, 56 (3.5% of total in surveyed districts) HSCs and 29 ASHAs. API of surveyed district ranged from 8 to 12 and Plasmodium falciaprum % ranged from 30 to 98%. As becomes clear from Table 2that 30 to 50% of the procured RDKs were utilized at microscopic centers, mostly for OPD cases (passive reporting) and a few for IPD (indoor cases). Majority of microscopy centers were located at CHCs as only 3 (8.8%) of 34 surveyed PHCs had functional microscopy centers. One of the PHC microscopy center, couldn't utilized 74.6% of the 750 procured RDKs, hence got expired and discarded. Only one of 56 surveyed HSCs, procured 136 RDKs, of which 75 (55.8%) were found to cross expiry date, by the survey team and remaining 60 (44.2%), as per HSC records, were utilized. However none of the HSC staff knew the technique of using RDKs. Another PHC procured 300 RDKs and used 49.7% and remaining 50.3% were going to expire in the same month when the survey was conducted. In Korea district although the survey team couldn't trace record about the procurement of RDKs from any of surveyed health facilities but they found a stock of 91 expired RDKs in the one of CHC laboratory of the district.
Table 1.
Health facilities included in the survey of six districts of Chhattisgarh (2008/09)
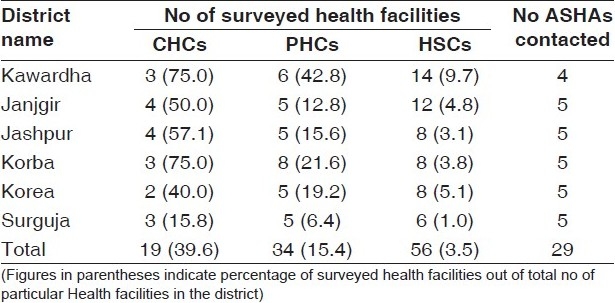
Table 2.
Use of RDKs at Microscopic center in six districts of Chhattisgarh (2008-09)
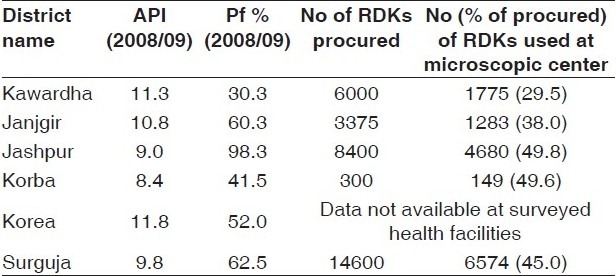
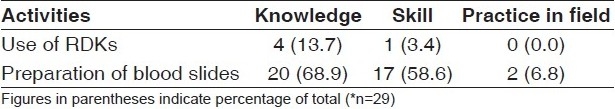
Table 3depicts diagnosing ability of ASHAs. As shown 27 (93.1%) of 29 ASHAs, included in survey were working in the difficult outreach areas, mainly involved in giving presumptive treatment to the fever cases. Interview of ASHAs reveled that although 26 (89.7%) of them were trained in the malaria diagnosis and treatment but only four had knowledge about use of RDKs and 20 (68.9%) about preparation of slides. Only one could demonstrate use of RDKs and 17 could prepare the blood slides on the spot. In actual field only two ASHAs were preparing blood slides and none were having RDKs. None of the ASHAs had any reporting format to record antimalarials activities.
Table 3.
Diagnosing ability of ASHA of six district of Chhattisgarh (2009-10)
The survey teams also tried to find out the record keeping and storage system of RDKs in the health facilities, which was almost non-existent. None of the interviewed staff including the medical officers were aware of the available stock of RDKs. Further to add to our observation, RDKs were invariably stored in laboratory of CHCs, even not protected from heat and direct sunlight. Seventeen of 19 interviewed block medical officers (BMOs) were not aware of the guidelines about the use and storage of RDKs.
Discussion
Observations made in the study are not in accordance with the current guidelines of NVBDCP which clearly state use of RDKs to be reserved for inaccessible remote areas, mostly at sub center/village level, where microscope is not possible.(7) In fact the present scenario is just the opposite, as the RDKs were used maximum for the diagnosis of OPD cases at the microscopic centers, mostly at CHC level. Moreover any form of documentation or recording of stocks was also grossly lacking at all levels. The health staff including the medical officers seems to lack the desired knowledge, accountability for proper use, storage and stock management of RDKs. This instruments are quite expensive,(6) hence their use need to be channelized in better cost effective manner. Multiple purpose workers (MPWs) at subcenters and ASHAs in the community who are supposed to use RDKs were also lacking the skills as well as knowledge. The findings are in line with observations of others.(11) The supply of the kits at the periphery (remote subcenters and inaccessible endemic villages) was also grossly lacking. None of the ASHAs in our study had any RDKs. Other researches from Assam have also reported indiscriminate use of RDKs. Another important observation is general non availability of malaria microscopy at PHC level. Our teams found many PHC laboratories with non functional microscope. Strengthening of PHC laboratory will increase the accessibility for malaria diagnosis and thereby reduce the burden on CHCs, thus avoiding delay in diagnosis (after 24 hours).
There is need to for formulating a more detailed block wise, action plan in district PIPs (Programme implementation Plans), to calculate actual requirement of RDKs as per API and Plasmodium falciaprum %, followed by a closer monitoring and inbuilt system of concurrent evaluation. This will identify the deviations at the outset so that corrective actions are initiated and deviations rectified. The health system staffs too need prior sensitization and training before implementing the Guidelines.
Acknowledgments
The authors are thankful to Central and District authority for all support needed for survey. Our sincere thanks also go to the field staff and medical officers for helping in data collection.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
References
- 1.World Health Organization. World Malaria Report 2008: HTM/ GMT/2008.1.
- 2. [last retrieved on 2009 Sep 8]. Available from: http://www.malaria.com/info/malaria-faq.php .
- 3. [last retrieved on 2009 Sep 8]. Available from: http://nvbdcp.gov.in/malaria3.html .
- 4.Reetha AM, Sharma SK, Tyagi PK, Valecha N, Nagpal BN, Dash AP. Operation feasibitlity of rapid diagnostics and blister packs used for malaria control in high transmission area of Chhattisgarh and Orissa. Indian J Med Res. 2007;125:65–72. [PubMed] [Google Scholar]
- 5.Geneva: World Health Organization; Geneva: World Health Organization; 2000. World Health Organization. Roll Back Malaria: A global partnership. [Google Scholar]
- 6.Belizario VY, Pasay CJ, Bersabe MJ, de Leon WU, Guerrero DM, Bugaoisan VM. Field evaluation of malaria rapid diagnosis of P.falciparum and non specific P.falciparum infection. Southeast Asian J Trop Med Public Health. 2005;36:252–61. [PubMed] [Google Scholar]
- 7.Guidelines for Diagnosis and Treatment of Malaria in India 2009, Government of India. [last retrieved on 2009 Sep 8]. Available from: http://nvbdcp.gov.in/Doc/Guidelines_for_Diagnosis___Treatment.pdf .
- 8. [last retrieved on 2009 Sep 8]. Available from: http://www.censusindia.gov.in/Census_Data_2001/Census_data_finder/ A_Series/ SC_ ST.htm .
- 9.Government of Chhattisgarh NRHM Project Implementation Plan 2009-2010
- 10. [last retrieved on 2009 Sep 8]. Available from: http://www.mohfw.nic.in/NRHM/Documents/NRHM%20Mission%20 Document. PDF .
- 11.Hardev Prasad: Evaluation of malaria control programme in three selected district of Assam. J Vector Borne Dis. 2009;46:280–87. [PubMed] [Google Scholar]


