Introduction
Healthcare workers (HCWs) are potentially exposed to blood and body fluids (BBF) in the course of their work and therefore are at risk of infection with blood-borne pathogens. Worldwide, three million HCWs experience percutaneous exposure to blood-borne viruses each year (two million hepatitis B, 900,000 hepatitis C and 300,000 human immunodeficiency virus).(1) Exposure to BBF can occur through a percutaneous injury (needle-stick injury, NSI) or mucocutaneous incident (BBF splash). Awareness regarding this occupational risk led to the issue of guidelines by CDC as universal precautions (UPs) in 1987, later updated in 1996.(2)
Despite detailed guidelines, the knowledge and understanding of UPs among HCWs even in developed countries has been found to be inadequate.(3) In developing countries, including India, the situation is worse and occupational safety of HCWs remains a neglected issue.(4,5)
Evidence exists that compliance with UPs reduces the risk of infections and protects healthcare practitioners.(6,7) However, there are many reasons for poor compliance.(4) In India, very few studies, with varying focus, have been conducted in this field. Thus, the present study was conducted to assess the knowledge, attitude, practices and barriers to compliance of UPs among HCWs in LokNayak Hospital in order to target the intervention programs appropriately.
Materials and Methods
A cross-sectional survey was carried out. Nurses and interns from all wards of LokNayak Hospital were studied as they are involved in collecting blood samples and administering injections. Those working in the labour room and operation theater were excluded as they form a different exposure category.
Expecting the prevalence of correct knowledge regarding UPs to be 50%, alpha 5% and chance error ±10%, the sample size worked out to be 96; therefore, 100 HCWs, comprising of 50 nurses and 50 interns, were studied. Respondents from complete lists of both categories were selected using simple random sampling. A questionnaire was prepared based on the WHO and CDC guidelines on UPs and was pre-tested before finalization.
Institutional ethical committee clearance was obtained. Data were collected by personal interview after verbal consent. A database was created in MS Excel. Chi square test was used for comparing proportions and statistical significance was taken as P <0.05.
Results
The responses were clubbed in major domains as per the objectives of the study. A high proportion of them were very worried (67%, 95% confidence interval 56.9−76.1) about incidents of NSI and BBF splashes. The complete schedule of hepatitis B vaccine was not followed by 23% of the HCWs.
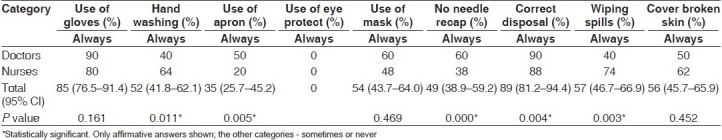
Table 1depicts the level of knowledge, risk perception and attitude of study subjects toward UPs. It shows that misconceptions persist despite a high level of awareness regarding UPs and that nurses had an overall low level of correct knowledge as compared with interns. Table 2 shows statistically significant differences between interns and nurses regarding various aspects of compliance with UPs.
Table 1.
Knowledge, risk perception and attitude toward UPs
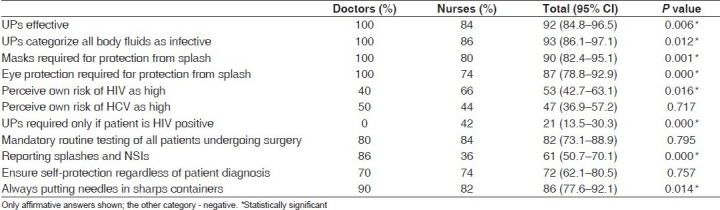
Table 2.
Compliance with universal precautions among HCWs
The perceived barriers to compliance with UPs, like too busy to use personal protective equipment (PPE) and not using PPE as colleagues do not use it, may offend patients, and discomfort in PPE use was seen to be statistically significantly higher in nurses as compared with interns (P < 0.004). The above barriers ranged between 42 and 68% for nurses and 12 and 24% for interns. However, the perceived barrier for use of PPE during emergencies was high, at 66% in both groups (P = 1.000).
A large proportion (76%, 66.4-84) felt that they were adequately trained in the use of PPE, and 85% (76.5-91.4) perceived knowing the procedure to be followed in case of an NSI. However, only 46% (36.0-56.3) had ever received training and 10% (4.9-17.6) received this training during the previous year.
Availability of PPE, sharps containers and waste segregation was commented upon in affirmative by 42% (32.2-52.3), 60% (49.7-69.7) and 69% (59.0-77.9), respectively. More nurses than doctors said that PPE (P = 0.015) and sharps containers were available (P = 0.003) and that segregation of waste at the point of generation was taking place (P = 0.000).
Discussion
This study indicates that most of the HCWs in an urban tertiary health care facility (HCF) in India possessed incomplete knowledge, as shown by other studies in developed(3) as well as developing countries, including India.(4,5) This lack of appropriate knowledge may be a factor leading to a high level of anxiety among them regarding exposure to BBF and NSIs.
Our study findings regarding use of apron, mask and eye protection have been corroborated by a study in a tertiary HCF in Iran, although use of eye protection in their study was slightly better (6.7%).(8)
Doctors were better than nurses in almost all aspects of compliance except hand washing, as shown by other studies too.(9) Our study findings of a low level of compliance with UPs among HCWs have also been noted in other studies.(3,4,8) It seems probable that an incomplete understanding of the principles underlying UPs among urban tertiary HCWs affected their practices and led to reduced compliance than expected in this group.
Perceived barriers to compliance with UPs clearly influence HCW's ability and willingness to comply with them in practice. Inability to use PPE during emergencies, overwork and busy schedules have also been shown in similar settings.(5,10) The other reasons for non-compliance overlap with those reported in studies from developed and developing countries.(3–5,8) The level of compliance seen in this study could also be due to the low level of training received by the HCWs and the low availability of equipment, as shown by other studies.(10)
To conclude, interventions to improve UPs' compliance among HCWs in tertiary HCFs in India are urgently needed. A multifaceted approach promoting positive perception of UPs compliance should include training (initial and periodic), adequate supply of PPE, provision of hepatitis B vaccination and development of appropriate infection control and injury surveillance programmes.
Limitations of the study
Actual compliance with UPs (as opposed to self-reported compliance) is probably lower than that reported due to social desirability bias.
Acknowledgments
The authors are grateful to ICMR, New Delhi, for sanctioning the Short Term Studentship Project; Dean, MAMC; MS, LNJP Hospital; and Prof G K Ingle, HoD, Department of Community Medicine, MAMC, New Delhi.
Footnotes
Source of Support: ICMR, New Delhi
Conflict of Interest: None declared.
References
- 1.World Health Report 2002: Reducing risks, promoting healthy life. [Last accessed on 2008 Jan]. Available from: http://www.who.int/whr/en. [DOI] [PubMed]
- 2.Universal precautions for prevention of Transmission of HIV and other blood borne infections. [Last accessed on 2008 Jan]. Available from: http://www.cdc.gov/ncidod/dhqp/bp_universal_precautions.html .
- 3.Roberts C. Universal Precautions: Improving the knowledge of trained nurses. Br J Nurs. 2000;9:43–7. doi: 10.12968/bjon.2000.9.1.6412. [DOI] [PubMed] [Google Scholar]
- 4.Kermode M, Jolley D, Langkham B, Thomas MS, Holmes W, Gifford SM. Compliance with Universal Precautions among health care workers in rural north India. Am J Infect Control. 2005;33:27–33. doi: 10.1016/j.ajic.2004.07.014. [DOI] [PubMed] [Google Scholar]
- 5.Wu S, Li L, Wu Z, Cao H, Lin C, Yan Z, et al. Universal precautions in the era of HIV/AIDS: Perception of health service providers in Yunnan, China. AIDS Behav. 2008;12:806–14. doi: 10.1007/s10461-007-9278-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Curran E. Reducing the risk of health care acquired infection. Nurs Stand. 2001;16:45–52. doi: 10.7748/ns2001.09.16.1.45.c3086. [DOI] [PubMed] [Google Scholar]
- 7.Sharbaugh RJ. The risk of occupational exposure and infection with infectious disease. Nurs Clin North Am. 1999;34:493–506. [PubMed] [Google Scholar]
- 8.Vaziri S, Najafi F, Miri F, Jalalvandi F, Almasi A. Practice of standard precautions among health care workers in a large teaching hospital. Indian J Med Sci. 2008;62:292–4. [PubMed] [Google Scholar]
- 9.Suchitra JB, Lakshmi DN. Impact of education on Knowledge, Attitude and Practices among various categories of health care workers on nosocomial infections. Indian J Med Microbiol. 2007;25:181–7. doi: 10.4103/0255-0857.34757. [DOI] [PubMed] [Google Scholar]
- 10.Chacko J, Isaac R. Percutaneous injuries among medical interns and their knowledge and practice of post-exposure prophylaxis for HIV. Indian J Public Health. 2007;51:127–9. [PubMed] [Google Scholar]


