Abstract
Objective
To investigate the combined effects of cisplatin and the histone deacetylase (HDAC) inhibitors suberoylanilide hydroxamic acid (SAHA) or sirtinol on HeLa cells and assess the mechanism underlying HDAC inhibitor-cisplatin synergy.
Methods
The antineoplastic actions of cisplatin, SAHA and sirtinol, alone and in combination, were evaluated using the tetrazolium dye-based MTT cell proliferation assay, DAPI nuclear staining and cytotoxicity analysis.
Results
Exposure to cisplatin, SAHA or sirtinol alone induced a dose-dependent reduction in HeLa cell viability. Combined treatment with cisplatin and SAHA or sirtinol was significantly more cytotoxic than cisplatin alone. Individually, cisplatin, SAHA and sirtinol activated caspase-3 and induced apoptosis, but the effects of combined treatment were greater. Importantly, both HDAC inhibitors dose-dependently inhibited the expression of the antiapoptotic proteins Bcl-2 and x-linked inhibitor of apoptosis protein (XIAP).
Conclusion
The combination of cisplatin and SAHA or sirtinol had synergistic effect on the HeLa cell viability. This potentiation of cisplatin activity was associated with HDAC inhibitor-mediated down-regulation of Bcl-2 and XIAP. These may result from the relaxation of chromatin by these HDAC inhibitors that increase cisplatin sensitivity by enhancing the accessibility of DNA to cisplatin and transcriptional regulators.
Keywords: Cervical cancer, Apoptosis, Cisplatin, Suberoylanilide hydroxamic acid, Sirtinol
INTRODUCTION
Modulation of chromatin structure through histone acetylation/ deacetylation is one of the major mechanisms involved in the regulation of gene expression.1-3 Increased histone acetylation causes chromatin to decondense and is associated with increased transcription.4-7 Increased activity of histone deacetylase (HDAC), which down-regulates histone acetylation, has been observed in various cancer types.8 Through acetylation of histones, HDAC inhibitors induce chromatin relaxation and favor transcription.
Previous studies have demonstrated that treatment with HDAC inhibitors alters gene transcription, resulting in a pro-apoptotic expression profile characterized by increased expression of pro-apoptotic genes/proteins, and decreased expression of anti-apoptotic genes/proteins, including Bcl-2, Bcl-Xl, MCL1 and x-linked inhibitor of apoptosis protein (XIAP).9-14 Treatment with HDAC inhibitors also promotes accumulation of ROS in tumor cells.10,15,16 These inhibitors induce growth arrest and apoptosis in various cancer cell lines in vitro and suppress tumor growth in animal xenograft models.17-19 Several HDAC inhibitors, including suberoylanilide hydroxamic acid (SAHA), tributyrin, and depsipeptide, are currently under investigation in clinical trials as antineoplastic agents for use in patients with hematologic and solid malignancies.20-22
SAHA, which inhibits class I and class II HDAC enzymes, has been shown to overcome multidrug resistance in different cancer cells in vitro, and to induce p53-independent apoptosis via the mitochondrial pathway.23 Sirtinol belongs to the class III histone deacetylase family and is an inhibitor of SIRT1 (silent mating type information regulation 2 homolog 1), the closest mammalian homolog of yeast Sir2. It has been shown that the SIRT1 levels are up-regulated in various drug-resistant cell lines and SIRT1 knockdown by siRNA transfection increases drug sensitivity in these cells.24
The chemotherapeutic agent cisplatin binds to DNA to form covalent platinum-DNA adducts. It is known that a tight chromatin structure prevents cisplatin from accessing DNA, and relaxation of chromatin by HDAC inhibitors may increase the accessibility of DNA to chemotherapeutic agents.25 Cisplatin is effective against many types of cancer, including cervical cancer, but its use is often restricted due to side effects and the development of drug-resistance. Cisplatin resistance is often thought to arise due to the induction of DNA repair enzymes, overexpression of Bcl-2, and increased levels of reduced glutathione (GSH) and associated enzymes. XIAP, a direct inhibitor of caspase-3 and caspase-7, modulates the Bax/cytochrome c pathway by inhibiting caspase-9.26,27 Cisplatin sensitivity in ovarian and uterine cancer cells has been shown to involve XIAP.28,29
Increasing the effectiveness of cisplatin-based chemotherapy will require a means to overcome the side effects of, and resistance to, cisplatin. Given the biological effects of HDAC inhibitors on cancer cells and the known mechanisms of cisplatin resistance noted above, we postulated that the combined treatment with cisplatin and an HDAC inhibitor would increase the anticancer efficacy of cisplatin. Here, we tested this hypothesis by investigating the potentiation of cisplatin activity by HDAC inhibitors SAHA and sirtinol in HeLa cervical cancer cells, and sought to determine the mechanism underlying the synergistic effect of combined treatment.
MATERIALS AND METHODS
1. Cell culture and reagents
HeLa cells, obtained from the American Type Culture Collection, were cultured in DMEM medium supplemented with 10% fetal bovine serum, 100 IU/mL penicillin and 100 µg/mL streptomycin in a humidified atmosphere of 5% CO2 in air at 37℃. Cisplatin and sirtinol were purchased from Sigma Chemical Co. (St. Louis, MO, USA), SAHA was purchased from Alexis Biochemicals (San Diego, CA, USA).
2. MTT cell viability assay
The viability of HeLa cells following treatment with cisplatin, SAHA or sirtinol alone, and in the indicated combinations, was measured using an MTT (3-[4,5-dimethylthiazol-2-yl]-2,5-diphenyl tetrazolium bromide) assay (Sigma). Cells were plated in triplicate wells (1.5×104 cells/well) of 96-well flat-bottomed plates and incubated overnight prior to drug exposure. Cells were then incubated with different concentrations of cisplatin, SAHA, sirtinol or a combination of cisplatin and one of the HDAC inhibitors. After exposure to the indicated concentrations/ drug combinations for 48 hours, 10 µL of MTT reagent was added to each well. Cells were then incubated for 3 hours with MTT, after which 100 µL of stop mix solution (20% SDS in 50% dimethyl formamide) was added and cells were incubated for an additional 1 hour. Absorbance was measured at a wavelength of 540 nm using a spectrophotometer.
3. Nuclear staining with DAPI
After treatment with HDAC inhibitor and/or cisplatin, the cells were fixed with 3.7% paraformaldehyde (Sigma) in PBS for 8 minutes at room temperature. Fixed cells were washed with PBS and stained with a 4,6-diamidino-2-phenylindole (DAPI; Sigma) solution for 5 minutes at room temperature. The cells were then washed three more times with PBS and analyzed using a fluorescence microscope.
4. Western blot analysis
The cells were harvested and lysed, and the protein concentration in lysates was quantified using the Bradford method. For Western blot analysis, an equal amount of protein (40 µg) was separated by electrophoresis on SDS-polyacrylamide gels and transferred to nitrocellulose membranes by electroblotting. Blots were probed with the desired antibodies for 1 hour, incubated with diluted enzyme-linked secondary antibody, and then visualized by enhanced chemiluminescence as recommended by the manufacturer (Amersham).
5. Cytotoxicity analysis
We used the combination index method of Chou and Talalay30 to determine whether the observed interactions between cisplatin and SAHA or sirtinol were additive or synergistic. If the interaction is additive, the sum of the effects of the two drugs should be equal to the product of their fractional activities. The representative function is f(u)1,2=f(u)1 ×f(u)2, where f(u)1 is the fraction unaffected by drug 1, f(u)2 is the fraction unaffected by drug 2 and f(u)1,2 is the fraction unaffected by drugs 1 and 2. The expected (presumed to be additive) and observed survival rates of HeLa cells obtained from the three independent drug-combination treatments were analyzed by Student's t-test. p<0.05 was considered significant.
RESULTS
1. Cytotoxicity of cisplatin, SAHA or sirtinol, alone and in combination
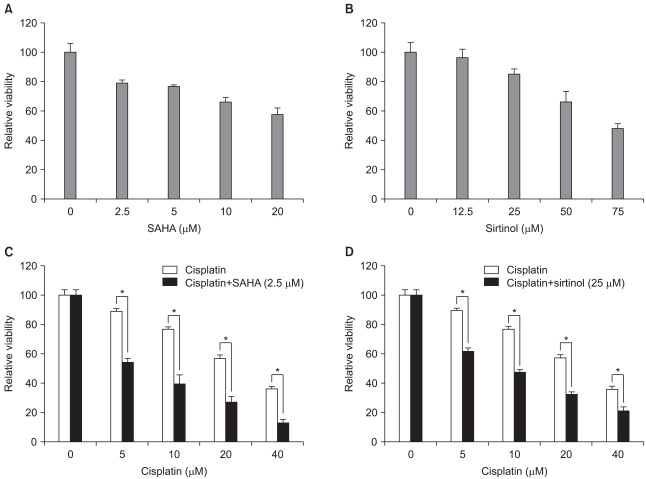
We first exposed HeLa cells to the conventional anticancer drug cisplatin or to SAHA or sirtinol, two HDAC inhibitors belonging to different structural classes, to investigate the possible cytotoxic effects of these three drugs alone. MTT assays revealed that, after incubating with HeLa cells for 48 hours, each of these drugs had a dose-dependent inhibitory effect on HeLa cell viability (Fig. 1A and B, and the black portion of C). Of the three compounds, cisplatin reduced cell viability to the greatest extent. We then tested the responses of HeLa cells to combinations of different concentrations of cisplatin (5, 10, 20, and 40 µm) and SAHA (2.5 µm) or sirtinol (25 µm). When tested alone, both SAHA (2.5 µm) and sirtinol (25 µm) reduced cell viability by about 20% (21% for SAHA and 16% for sirtinol). As shown in Fig. 1, the observed viability in HeLa cells treated with combinations of cisplatin and SAHA (2.5 µm) or sirtinol (25 µm) was less than that expected for an additive model at each concentration of cisplatin tested, indicating synergy. Although both HDAC inhibitors synergized with cisplatin to inhibit cell viability, the combination of cisplatin and SAHA was more effective than the cisplatin/sirtinol combination (Fig. 1C and D).
Fig. 1.
Inhibition of HeLa cell growth by suberoylanilide hydroxamic acid (SAHA), sirtinol or cisplatin, alone and in combination. Cells were assayed for viability using MTT assays after treating for 48 hr with increasing doses of SAHA (A), sirtinol (B), or cisplatin (C or D black column) alone, or with a combination of cisplatin and SAHA (C) or cisplatin and sirtinol (D). Results are expressed as the means±SEs of three independent experiments. *p<0.05.
2. Morphological features of apoptosis in HeLa cells treated with HDAC inhibitors and/or cisplatin
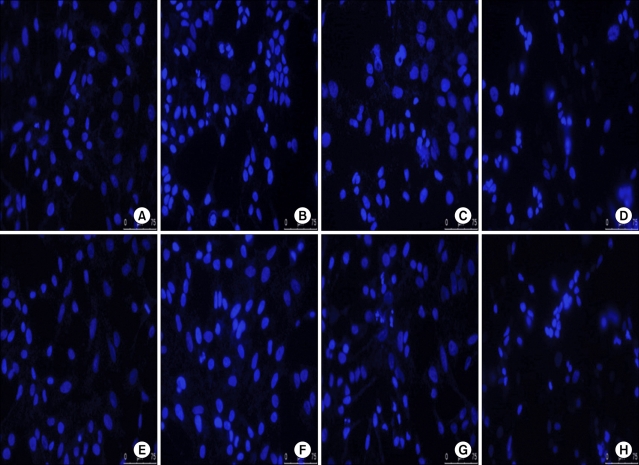
To determine whether the growth inhibition by cisplatin and/or HDAC inhibitors was associated with apoptotic cell death, we treated cells for 48 hours with cisplatin, SAHA or sirtinol, alone, or with HDAC inhibitor/cisplatin combinations, and then examined nuclear morphology in DAPI-stained cells. With DAPI nuclear staining, cells with condensed and fragmented nuclei are judged to be apoptotic. Treatment of HeLa cells with SAHA (2.5 µm), sirtinol (25 µm) or cisplatin (10 µm) alone induced a modest level of apoptosis. However, the combination of cisplatin (10 µm) and SAHA (2.5 µm) or sirtinol (25 µm) induced a significantly greater degree apoptosis than that seen with cisplatin alone (Fig. 2). These results indicate a good correspondence between the extent of apoptosis and growth inhibition, and suggest that the cell death induced in HeLa cells by cisplatin, SAHA and sirtinol, alone or in combination, is largely apoptotic in nature.
Fig. 2.
Induction of apoptosis in HeLa cells by suberoylanilide hydroxamic acid (SAHA), sirtinol or cisplatin, alone and in combination. Cells were incubated for 48 hr with 2.5 µm SAHA (B), 25 µm sirtinol (F) or 10 µm cisplatin (C and G) alone, or with 2.5 µm SAHA/10 µm cisplatin (D) or 25 µm sirtinol/10 µm cisplatin (H) combinations. (A) and (E) are controls. The cells were sampled, fixed and stained with DAPI; stained nuclei were then observed under a fluorescence microscope using a blue filter.
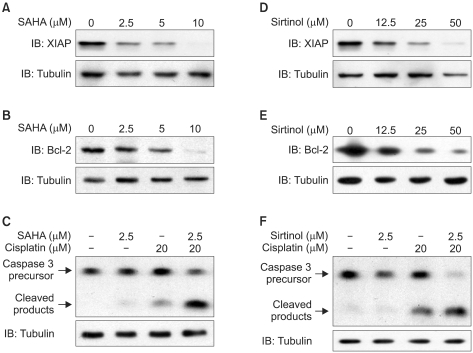
3. Inhibition of Bcl-2 and XIAP expression by HDAC inhibitors
Apoptotic cell death is highly regulated by pro-apoptotic and anti-apoptotic modulators. Bcl-2 and XIAP are anti-apoptotic proteins that are relevant to chemoresistance to cisplatin. To determine whether SAHA or sirtinol down-regulated the expression of Bcl-2 and/or XIAP in HeLa cells, we isolated cellular proteins after exposure to different concentrations of SAHA and sirtinol for 24 hours, and performed immunoblotting. The results of Western-blot analyses indicated that treatment with either SAHA (0, 2.5, 5, and 10 µm) or sirtinol (0, 12.5, 25, and 50 µm) induced a dose-dependent decrease in the levels of Bcl-2 and XIAP (Fig. 3A, B, D, and E).
Fig. 3.
Down-regulation of XIAP and Bcl-2 levels and activation of caspase-3. HeLa cells were treated with the indicated concentrations of SAHA, sirtinol or cisplatin, alone or as SAHA/cisplatin or sirtinol/cisplatin combinations, for 24 hours and then analyzed by immunoblotting. (A, B, D, and E) SAHA (0, 2.5, 5, or 10 µm) or sirtinol (0, 12.5, 25, or 50 µm) induced a dose-dependent reduction in XIAP and Bcl-2 levels. (C) Induction of the cleaved (activated) form of caspase-3 by SAHA (2.5 µm) and cisplatin (20 µm) alone, and by combined SAHA (2.5 µm)/cisplatin (20 µm) treatment. (F) Induction of the cleaved (activated) form of caspase-3 by sirtinol (25 µm) and cisplatin (20 µm) alone, and by combined sirtinol (25 µm)/cisplatin (20 µm) treatment.
4. Increased levels of activated caspase-3 by combined cisplatin/HDAC inhibitor treatment
Caspases are thought to be vital in mediating various apoptotic responses, including those induced by cisplatin. Caspase-3, which is cleaved proteolytically from its inactive precursor form into active fragments by various apoptotic stimuli, is an important apoptotic effector in both the intrinsic and extrinsic pathways of apoptotic cell death. To assess the effects of HDAC inhibitors on the caspase pathway, we measured caspase-3 activation in HeLa cells after a 24-hour treatment with cisplatin, SAHA or sirtinol, alone or in combination, using an immunoblotting method. We found that SAHA (2.5 µm) and sirtinol (25 µm) alone induced minimal activation of caspase-3, whereas the level of caspase-3 activation induced by cisplatin alone (20 µm) was readily apparent. Notably the cisplatin (20 µm)/ SAHA (2.5 µm) and cisplatin (20 µm)/sirtinol (25 µm) combinations strongly induced caspase-3 activation (Fig. 3C and F), demonstrating that the combinations of cisplatin with SAHA or sirtinol were more effective apoptosis-inducing stimuli than were cisplatin or HDAC inhibitors alone.
DISCUSSION
Cisplatin is effective in neoadjuvant and conventional chemotherapy in the treatment of cervical cancer. Despite the impressive anti-neoplastic activity of cisplatin, severe side effects and drug resistance restricts its use in cancer therapy. High doses of cisplatin are more effective than low doses in cancer chemotherapy. Unfortunately, several severe side effects, notably nephrotoxicity and ototoxicity, limit the dose that can be given to patients. Moreover, the repeated use of cisplatin promotes resistance to cisplatin-induced apoptosis in cancer cells. Thus, drugs that sensitize cancer cells to cisplatin could increase the clinical efficacy of cisplatin. Unlike conventional chemotherapeutic agents, which often cause DNA damage in both cancer and normal tissues, HDAC inhibitors display strong cancer selectivity and cause less toxicity to normal tissues.31
In this study, we found that both SAHA and sirtinol exerted a dose-dependent cytotoxic effect on HeLa cells. Importantly, low concentrations of SAHA or sirtinol synergized with cisplatin in combination therapy to induce a level of cytotoxicity greater than that mediated by either agent alone, or that predicted by an additive model. Of the two combinations, the cisplatin/ SAHA combination produced a more marked reduction in cell viability. DAPI staining and Western-blot analyses revealed that combined treatment with cisplatin and a low concentration of either of the two HDAC inhibitors markedly increased caspase-3 activation and apoptosis in HeLa cells compared with cisplatin alone.
Cisplatin cytotoxicity appears to correlate with DNA adduct formation.32 Cisplatin, along with a number of other exogenous toxins, is detoxified by glutathione, the most abundant intracellular thiol and a critical cellular antioxidant,33,34 through the formation of glutathione adducts.35,36 Among the mechanisms that contribute to cellular resistance to cisplatin are those that involve up-regulation of the anti-apoptotic proteins Bcl-2 and XIAP. Bcl-2 overexpression has been shown to increase cisplatin resistance in a number of experimental models.37-41 Bcl-2 overexpression in the mitochondrial outer membrane inhibits the characteristic increase in reactive oxygen species observed in cells exposed to a number of apoptotic triggers.42,43 Moreover, Bcl-2-mediated cisplatin resistance is associated with an increase in glutathione levels, and glutathione synthesis is required for Bcl-2-mediated cisplatin resistance.44 Similarly, XIAP levels are known to regulate cisplatin sensitivity in some uterine cell lines.29
Through acetylation of histones, SAHA and sirtinol relax chromatin, increasing the accessibility of DNA to transcription factors and thereby regulating the expression of a number of genes, including those for Bcl-2 and XIAP. Thus, the significantly increased cell death induced in cells by the combination of cisplatin and low concentrations of SAHA or sirtinol compared with cisplatin alone is likely due, at least in part, to down-regulation of Bcl-2 and XIAP by these HDAC inhibitors. By promoting chromatin decondensation, SAHA and sirtinol also provides greater DNA access to cisplatin. These actions sensitize HeLa cells to cisplatin, and thus are also likely to contribute to the synergistic cytotoxicity of cisplatin and HDAC inhibitors toward HeLa cells. Collectively, these results may indicate that relaxation of chromatin by SAHA or sirtinol increases the effectiveness of cisplatin by enhancing the accessibility of DNA to both cisplatin and transcriptional regulators. The first action directly increases the sensitivity of cells to cisplatin; the second contributes to increased sensitivity (and potentially to decreased resistance) to cisplatin by down-regulating anti-apoptosis regulators.
Footnotes
No potential conflict of interest relevant to this article was reported.
References
- 1.Khochbin S, Verdel A, Lemercier C, Seigneurin-Berny D. Functional significance of histone deacetylase diversity. Curr Opin Genet Dev. 2001;11:162–166. doi: 10.1016/s0959-437x(00)00174-x. [DOI] [PubMed] [Google Scholar]
- 2.Marmorstein R, Roth SY. Histone acetyltransferases: function, structure, and catalysis. Curr Opin Genet Dev. 2001;11:155–161. doi: 10.1016/s0959-437x(00)00173-8. [DOI] [PubMed] [Google Scholar]
- 3.Roth SY, Denu JM, Allis CD. Histone acetyltransferases. Annu Rev Biochem. 2001;70:81–120. doi: 10.1146/annurev.biochem.70.1.81. [DOI] [PubMed] [Google Scholar]
- 4.Lee DY, Hayes JJ, Pruss D, Wolffe AP. A positive role for histone acetylation in transcription factor access to nucleosomal DNA. Cell. 1993;72:73–84. doi: 10.1016/0092-8674(93)90051-q. [DOI] [PubMed] [Google Scholar]
- 5.Grunstein M. Histone acetylation in chromatin structure and transcription. Nature. 1997;389:349–352. doi: 10.1038/38664. [DOI] [PubMed] [Google Scholar]
- 6.Struhl K. Histone acetylation and transcriptional regulatory mechanisms. Genes Dev. 1998;12:599–606. doi: 10.1101/gad.12.5.599. [DOI] [PubMed] [Google Scholar]
- 7.Strahl BD, Allis CD. The language of covalent histone modifications. Nature. 2000;403:41–45. doi: 10.1038/47412. [DOI] [PubMed] [Google Scholar]
- 8.Marks PA, Rifkind RA, Richon VM, Breslow R, Miller T, Kelly WK. Histone deacetylases and cancer: causes and therapies. Nat Rev Cancer. 2001;1:194–202. doi: 10.1038/35106079. [DOI] [PubMed] [Google Scholar]
- 9.Zhang XD, Gillespie SK, Borrow JM, Hersey P. The histone deacetylase inhibitor suberic bishydroxamate regulates the expression of multiple apoptotic mediators and induces mitochondria-dependent apoptosis of melanoma cells. Mol Cancer Ther. 2004;3:425–435. [PubMed] [Google Scholar]
- 10.Rosato RR, Maggio SC, Almenara JA, Payne SG, Atadja P, Spiegel S, et al. The histone deacetylase inhibitor LAQ824 induces human leukemia cell death through a process involving XIAP down-regulation, oxidative injury, and the acid sphingomyelinase-dependent generation of ceramide. Mol Pharmacol. 2006;69:216–225. doi: 10.1124/mol.105.017145. [DOI] [PubMed] [Google Scholar]
- 11.Mitsiades CS, Mitsiades NS, McMullan CJ, Poulaki V, Shringarpure R, Hideshima T, et al. Transcriptional signature of histone deacetylase inhibition in multiple myeloma: biological and clinical implications. Proc Natl Acad Sci USA. 2004;101:540–545. doi: 10.1073/pnas.2536759100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Peart MJ, Smyth GK, van Laar RK, Bowtell DD, Richon VM, Marks PA, et al. Identification and functional significance of genes regulated by structurally different histone deacetylase inhibitors. Proc Natl Acad Sci U S A. 2005;102:3697–3702. doi: 10.1073/pnas.0500369102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Moore PS, Barbi S, Donadelli M, Costanzo C, Bassi C, Palmieri M, et al. Gene expression profiling after treatment with the histone deacetylase inhibitor trichostatin A reveals altered expression of both pro- and anti-apoptotic genes in pancreatic adenocarcinoma cells. Biochim Biophys Acta. 2004;1693:167–176. doi: 10.1016/j.bbamcr.2004.07.001. [DOI] [PubMed] [Google Scholar]
- 14.Duan H, Heckman CA, Boxer LM. Histone deacetylase inhibitors down-regulate bcl-2 expression and induce apoptosis in t(14;18) lymphomas. Mol Cell Biol. 2005;25:1608–1619. doi: 10.1128/MCB.25.5.1608-1619.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ruefli AA, Ausserlechner MJ, Bernhard D, Sutton VR, Tainton KM, Kofler R, et al. The histone deacetylase inhibitor and chemotherapeutic agent suberoylanilide hydroxamic acid (SAHA) induces a cell-death pathway characterized by cleavage of Bid and production of reactive oxygen species. Proc Natl Acad Sci U S A. 2001;98:10833–10838. doi: 10.1073/pnas.191208598. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Rosato RR, Almenara JA, Dai Y, Grant S. Simultaneous activation of the intrinsic and extrinsic pathways by histone deacetylase (HDAC) inhibitors and tumor necrosis factor-related apoptosis-inducing ligand (TRAIL) synergistically induces mitochondrial damage and apoptosis in human leukemia cells. Mol Cancer Ther. 2003;2:1273–1284. [PubMed] [Google Scholar]
- 17.Marks PA, Richon VM, Rifkind RA. Histone deacetylase inhibitors: inducers of differentiation or apoptosis of transformed cells. J Natl Cancer Inst. 2000;92:1210–1216. doi: 10.1093/jnci/92.15.1210. [DOI] [PubMed] [Google Scholar]
- 18.Bolden JE, Peart MJ, Johnstone RW. Anticancer activities of histone deacetylase inhibitors. Nat Rev Drug Discov. 2006;5:769–784. doi: 10.1038/nrd2133. [DOI] [PubMed] [Google Scholar]
- 19.Butler LM, Agus DB, Scher HI, Higgins B, Rose A, Cordon-Cardo C, et al. Suberoylanilide hydroxamic acid, an inhibitor of histone deacetylase, suppresses the growth of prostate cancer cells in vitro and in vivo. Cancer Res. 2000;60:5165–5170. [PubMed] [Google Scholar]
- 20.Sandor V, Bakke S, Robey RW, Kang MH, Blagosklonny MV, Bender J, et al. Phase I trial of the histone deacetylase inhibitor, depsipeptide (FR901228, NSC 630176), in patients with refractory neoplasms. Clin Cancer Res. 2002;8:718–728. [PubMed] [Google Scholar]
- 21.Duvic M, Zhang C. Clinical and laboratory experience of vorinostat (suberoylanilide hydroxamic acid) in the treatment of cutaneous T-cell lymphoma. Br J Cancer. 2006;95(S1):S13–S19. [Google Scholar]
- 22.O'Connor OA. Clinical experience with the novel histone deacetylase inhibitor vorinostat (suberoylanilide hydroxamic acid) in patients with relapsed lymphoma. Br J Cancer. 2006;95(S1):S7–S12. [Google Scholar]
- 23.Ruefli AA, Bernhard D, Tainton KM, Kofler R, Smyth MJ, Johnstone RW. Suberoylanilide hydroxamic acid (SAHA) overcomes multidrug resistance and induces cell death in P-glycoprotein-expressing cells. Int J Cancer. 2002;99:292–298. doi: 10.1002/ijc.10327. [DOI] [PubMed] [Google Scholar]
- 24.Chu F, Chou PM, Zheng X, Mirkin BL, Rebbaa A. Control of multidrug resistance gene mdr1 and cancer resistance to chemotherapy by the longevity gene sirt1. Cancer Res. 2005;65:10183–10187. doi: 10.1158/0008-5472.CAN-05-2002. [DOI] [PubMed] [Google Scholar]
- 25.Kim MS, Blake M, Baek JH, Kohlhagen G, Pommier Y, Carrier F. Inhibition of histone deacetylase increases cytotoxicity to anticancer drugs targeting DNA. Cancer Res. 2003;63:7291–7300. [PubMed] [Google Scholar]
- 26.Deveraux QL, Roy N, Stennicke HR, Van Arsdale T, Zhou Q, Srinivasula SM, et al. IAPs block apoptotic events induced by caspase-8 and cytochrome c by direct inhibition of distinct caspases. EMBO J. 1998;17:2215–2223. doi: 10.1093/emboj/17.8.2215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Deveraux QL, Leo E, Stennicke HR, Welsh K, Salvesen GS, Reed JC. Cleavage of human inhibitor of apoptosis protein XIAP results in fragments with distinct specificities for caspases. EMBO J. 1999;18:5242–5251. doi: 10.1093/emboj/18.19.5242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Asselin E, Mills GB, Tsang BK. XIAP regulates Akt activity and caspase-3-dependent cleavage during cisplatin-induced apoptosis in human ovarian epithelial cancer cells. Cancer Res. 2001;61:1862–1868. [PubMed] [Google Scholar]
- 29.Gagnon V, Van Themsche C, Turner S, Leblanc V, Asselin E. Akt and XIAP regulate the sensitivity of human uterine cancer cells to cisplatin, doxorubicin and taxol. Apoptosis. 2008;13:259–271. doi: 10.1007/s10495-007-0165-6. [DOI] [PubMed] [Google Scholar]
- 30.Chou TC, Talalay P. Quantitative analysis of dose-effect relationships: the combined effects of multiple drugs or enzyme inhibitors. Adv Enzyme Regul. 1984;22:27–55. doi: 10.1016/0065-2571(84)90007-4. [DOI] [PubMed] [Google Scholar]
- 31.Papeleu P, Vanhaecke T, Elaut G, Vinken M, Henkens T, Snykers S, et al. Differential effects of histone deacetylase inhibitors in tumor and normal cells-what is the toxicological relevance? Crit Rev Toxicol. 2005;35:363–378. doi: 10.1080/10408440590935639. [DOI] [PubMed] [Google Scholar]
- 32.Reed E, Yuspa SH, Zwelling LA, Ozols RF, Poirier MC. Quantitation of cis-diamminedichloroplatinum II (cisplatin)-DNA-intrastrand adducts in testicular and ovarian cancer patients receiving cisplatin chemotherapy. J Clin Invest. 1986;77:545–550. doi: 10.1172/JCI112335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Anderson ME. Glutathione: an overview of biosynthesis and modulation. Chem Biol Interact. 1998;111-112:1–14. doi: 10.1016/s0009-2797(97)00146-4. [DOI] [PubMed] [Google Scholar]
- 34.Schroder CP, Godwin AK, O'Dwyer PJ, Tew KD, Hamilton TC, Ozols RF. Glutathione and drug resistance. Cancer Invest. 1996;14:158–168. doi: 10.3109/07357909609018891. [DOI] [PubMed] [Google Scholar]
- 35.Ishikawa T, Ali-Osman F. Glutathione-associated cis-diamminedichloroplatinum( II) metabolism and ATP-dependent efflux from leukemia cells: molecular characterization of glutathione-platinum complex and its biological significance. J Biol Chem. 1993;268:20116–20125. [PubMed] [Google Scholar]
- 36.Meister A. Glutathione metabolism and its selective modification. J Biol Chem. 1988;263:17205–17208. [PubMed] [Google Scholar]
- 37.Mese H, Sasaki A, Alcalde RE, Nakayama S, Matsumura T. Regulation of apoptosis reduction in the cisplatin-resistant A431 cell line by Bcl-2 and CPP32. Chemotherapy. 2000;46:69–76. doi: 10.1159/000007258. [DOI] [PubMed] [Google Scholar]
- 38.Miyake H, Hara I, Yamanaka K, Arakawa S, Kamidono S. Synergistic enhancement of resistance to cisplatin in human bladder can cer cells by overexpression of mutant-type p53 and Bcl-2. J Urol. 1999;162:2176–2181. doi: 10.1016/S0022-5347(05)68155-4. [DOI] [PubMed] [Google Scholar]
- 39.Miyake H, Hanada N, Nakamura H, Kagawa S, Fujiwara T, Hara I, et al. Overexpression of Bcl-2 in bladder cancer cells inhibits apoptosis induced by cisplatin and adenoviral-mediated p53 gene transfer. Oncogene. 1998;16:933–943. doi: 10.1038/sj.onc.1201602. [DOI] [PubMed] [Google Scholar]
- 40.Zangemeister-Wittke U, Schenker T, Luedke GH, Stahel RA. Synergistic cytotoxicity of bcl-2 antisense oligodeoxynucleotides and etoposide, doxorubicin and cisplatin on small-cell lung cancer cell lines. Br J Cancer. 1998;78:1035–1042. doi: 10.1038/bjc.1998.624. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Simonian PL, Grillot DA, Merino R, Nunez G. Bax can antagonize Bcl-XL during etoposide and cisplatin-induced cell death independently of its heterodimerization with Bcl-XL. J Biol Chem. 1996;271:22764–22772. doi: 10.1074/jbc.271.37.22764. [DOI] [PubMed] [Google Scholar]
- 42.Hockenbery DM, Oltvai ZN, Yin XM, Milliman CL, Korsmeyer SJ. Bcl-2 functions in an antioxidant pathway to prevent apoptosis. Cell. 1993;75:241–251. doi: 10.1016/0092-8674(93)80066-n. [DOI] [PubMed] [Google Scholar]
- 43.Voehringer DW. BCL-2 and glutathione: alterations in cellular redox state that regulate apoptosis sensitivity. Free Radic Biol Med. 1999;27:945–950. doi: 10.1016/s0891-5849(99)00174-4. [DOI] [PubMed] [Google Scholar]
- 44.Yao MK, Desilets H, Charles MT, Boulanger R, Tweddell RJ. Effect of mycorrhization on the accumulation of rishitin and solavetivone in potato plantlets challenged with Rhizoctonia solani. Mycorrhiza. 2003;13:333–336. doi: 10.1007/s00572-003-0267-0. [DOI] [PubMed] [Google Scholar]