Abstract
The impact of prenatal alcohol exposure on memory and brain development was investigated in 92 African-American, young adults who were first identified in the prenatal period. Three groups (Control, n=26; Alcohol-related Neurodevelopmental Disorder, n=36; and Dysmorphic, n=30) were imaged using structural MRI with brain volume calculated for multiple regions of interest. Memory was measured using the Verbal Selective Reminding Memory Test and its nonverbal counterpart, the Nonverbal Selective Reminding Memory Test, which each yielding measures of learning and recall. For both Verbal and Nonverbal Recall and Slope, linear trends were observed demonstrating a spectrum of deficits associated with prenatal alcohol exposure. Dysmorphic individuals performed significantly poorer than unexposed controls on 5 of 6 memory outcomes. Alcohol-exposed individuals demonstrated significantly lower total brain volume than controls, as well as lower volume in a number of specific regions including hippocampus. Mediation analyses indicated that memory performance associated with effects of prenatal alcohol exposure was mediated from dysmorphic severity through hippocampal volume, particularly right hippocampus. These results indicate that the association between the physical effects of prenatal alcohol exposure and deficits in memory are mediated by volumetric reduction in specific brain regions.
Fetal alcohol syndrome (FAS) and the spectrum of associated disorders that result from maternal alcohol use during gestation (i.e., fetal alcohol spectrum disorders, FASDs) are among the most common developmental disorders (Centers for Disease Control and Prevention, 2009). Through its impact on the developing brain, gestational alcohol exposure is believed to affect physical functioning and cognition across the lifespan and to be associated with an array of secondary disabilities affecting behavior and adaptive performance (e.g., Streissguth, Barr, Kogan, & Bookstein, 1996) (see Jacobson & Jacobson, 2002; Kable & Coles, 2004; Mattson & Riley, 1998 for reviews). Despite the prevalence of FASDs and their comprehensive impact on affected individuals, there is still a limited literature on the nature of the neuropsychological outcomes and brain-behavior relationships in adults. In the present study, we explored the association between the impact of prenatal alcohol exposure on physical features including brain volume and on learning and memory in alcohol-affected young adults whose prenatal exposure was documented and quantified.
Prenatal alcohol exposure and memory
Both human studies (e.g., Mattson, Riley, Gramling, Delis, & Jones, 1998; Pei, Rinaldi, Rasmussen, Massey, & Massey, 2008; Streissguth, Bookstein, Sampson, & Barr, 1989) and animal models (Becker, Randall, Salo, Saulnier, & Weathersby, 1994; Driscoll, Streissguth, & Riley, 1990) have shown associations between poorer performance on learning and memory tasks and prenatal alcohol exposure. Currently, the preponderance of evidence suggests that alcohol exposure affects the encoding, or learning, aspect of memory rather than retrieval of previously-learned material (e.g., Coles, et al, 1991; Kerns, Don, Mateer & Streissguth, 1997; Mattson, et al., 1996; Willford, Richardson, Leech, & Day, 2004). The finding of deficits in initial encoding implicates the hippocampus which is known to be associated with episodic memory and encoding, particularly of spatial information. (For review of prenatal alcohol exposure and hippocampal functioning, see Berman & Hannigan, 2000.) However, there is also evidence that deficits shown by alcohol-affected individuals are more significant when mnemonic strategy use is required for effective performance, implicating deficits in metamemory development and/or executive functioning. Compared to typical controls, both children and adults prenatally exposed to alcohol show differences in the frequency and type of strategies used to encode information. In the Kerns et al (1997) study, adults with FAS used less semantic clustering and made more frequent intrusion errors on a word-list verbal learning task. Similarly, children with FASD showed deficits in their use of serial and semantic clustering, and this lack of strategy use was correlated with poorer memory performance (Roebuck-Spencer & Mattson, 2004). In addition, differences in learning slopes have been reported by Mattson and Roebuck (2002), suggesting that non-exposed children learned information at a faster rate compared to those prenatally exposed to alcohol (Mattson & Roebuck, 2002). In that study, learning slope differences were task-dependent, and slower rates were observed on verbal but not nonverbal tasks. The researchers suggested that poorer performance resulted from less frequent use of available encoding strategies during the verbal task by the clinical group (although this explanation would not account for the similar performance on the nonverbal task). Thus, there is evidence that the encoding deficits demonstrated in FASD may be influenced by those areas of the brain that support executive functioning, that is, the frontal regions. If deficits in frontal regions contribute to encoding deficits, such effects should be more apparent in young adults than in children whose frontal lobes are less mature.
Although there is an extensive animal literature, there are as yet only a few human studies that have examined the impact of prenatal exposure on the relationship between brain structure and functioning. Animal studies have reported deficits in spatial memory associated with hippocampal volume reductions (Berman & Hannigan, 2000; Klintsova, Helfer, Calizo, et al, 2007; Livy, Miller, Maier, & West, 2003) but cannot provide evidence regarding verbal memory deficits. The single human study on the relationship between hippocampal structure and memory in FASD was recently published by Willoughby, Sherd, Nash and Rovet (2008). These authors found a relationship between hippocampal volume, verbal learning and both verbal and spatial recall in clinically-referred children and concluded that observed deficits in memory function shown by alcohol-exposed children could be attributed to long-term abnormalities in hippocampal development. They also speculated that normal age-related increases in hippocampal volume were reduced by alcohol-exposure. While consistent with expectations about the nature of this relationship, there are some limitations in these results due to sample characteristics and the necessarily correlational nature of such research. First, only the left hippocampus was found to be affected in the alcohol group while it was the right hippocampus that showed the most significant correlations with memory function. In addition, there was a more than 40 point difference in ability scores (i.e. IQ) between the FASD and the Contrast groups, raising concerns that the observed effects may have been secondary to global differences in cognitive abilities or to the conditions that led to these intellectual differences. Finally, the authors’ conclusion that there is an alcohol-exposure related failure in the growth of the hippocampus during later childhood is inconsistent with some reports (Giedd, Vaitzus, Hamberger, Lange, Rajapakse, & Kaysen, et al., 1996; Yurgelun-Todd, Kilgore, & Cintron, 2003) that the hippocampus does not substantially change in volume during this period. However, it is known that reductions in hippocampal volume are associated with certain environmental factors, such as stress (Bremner, 2006), which may have affected results in the clinical group investigated. These limitations are acknowledged by the authors who urged more attention to this understudied area.
Several studies have used functional MRI to evaluate the relationship between performance on verbal and spatial learning tasks and certain frontal regions in alcohol-exposed samples. Using memory tasks in fMRI protocols, Sowell and her colleagues (O’Hare, Lu, Houston, Bookheimer, Mattson, O’Connor, & Sowell, 2009; Sowell, Lu, O’Hare, McCourt, Mattson, O’Connor, & Bookheimer, 2007; Sowell, Mattson, Kan, Thompson, Riley, & Toga, 2008) have reported associations in children with FASD between activation in certain frontal regions (i.e., right dorsal frontal cortex) and verbal paired associate learning and on a standardized list learning task. Similarly, Malisza, Allman, Shiloff, Jakobson, Longstaff, & Chudley (2005) found associations between frontal activity (inferior-medial frontal; orbital gyrus) during working memory tasks in both adults and children with FASD.
In the current study, we examined the relative contribution to memory performance of different brain regions known to be associated with encoding and strategy use in alcohol-affected young adults. Although it is clear that most of the cortex contributes to effective learning, the primary anatomic substrates of memory have been identified from both animal and human studies. The medial temporal regions (specifically the hippocampus, as well as entorhinal and parahippocampus and fusiform gyri) are known to be associated with learning and memory (Van Petten, 2004). The role of the hippocampus in encoding, consolidation and retrieval of episodic memory is well described (Squire, 1998; Kramer, et al. 2005; Van Petten, 2004) and damage to structures in this region interferes with episodic memorization. The direct contribution of the frontal regions to memory function appears to be more related to executive functioning; that is, allocation of mental resources and the application of strategies to deal more efficiently with learning tasks (Wheeler, Stuss, & Tulving, 1995) and the storage and retrieval of long term memories (Smith & Squire, 2009). Memory performance therefore may be dependent on the effectiveness of such strategies. Thus, it can be hypothesized that in alcohol-affected individuals who have microcephaly and demonstrate memory deficits, volume reductions in the medial temporal regions including the hippocampus and frontal regions should be present, and these reductions may, in turn, be related to poorer performance on tasks of memory and learning. Further, we hypothesized that reductions in specific brain regions associated with memory function, specifically medial temporal and frontal regions, would be associated with decrements in recall and learning rate. We anticipated that hippocampal volume would be associated with both recall and learning rate and that volume of frontal regions would be associated with recall, particularly of verbal material. Finally, because both brain volume and observable physical features are presumed to result from the impact of prenatal alcohol exposure during embryonic and fetal development, we hypothesized that there would be a significant relationship between the severity of physically observable alcohol effects (that is, dysmorphic features) and both brain volume and memory function, with brain volume mediating this relationship.
Method
Participants
The sample included 92 young adults participating in a longitudinal study of the effects of prenatal alcohol exposure on development. Mothers of participants were recruited between 1980 and 1986 from an urban hospital serving a predominantly African-American, low income population. All women applying for prenatal care were screened for the quantity and frequency of alcohol use during pregnancy. Those who reported consuming at least one ounce of absolute alcohol per week (equivalent to two drinks) and those who reported consuming no alcohol while pregnant were invited to participate in the initial study. No financial incentives were offered at recruitment. Amount of alcohol consumed by those who met criteria for inclusion as drinkers ranged from 1 to 75 ounces of absolute alcohol per week (oz/AA/wk) with an average of 10.3 oz/AA/wk (that is, more than 20 drinks a week). Alcohol use was determined by self report as biological measures often used to confirm such use in other circumstances are unreliable in pregnancy. The mothers who drank during pregnancy were advised that it could have negative health consequences for the baby and that they should stop. Those who agreed were provided with referrals to treatment programs.
Infants meeting inclusion criteria were enrolled at birth and have been evaluated periodically since that time. At the postnatal examination, infants were assessed for growth patterns and presence of dysmorphic physical features related to prenatal alcohol exposure (Coles, Smith, Fernhoff & Falek, 1985). In evaluations completed at seven years of age, at mid-adolescence, and as part of the protocol for the current young adult follow-up, participants were again assessed for physical features using the Dysmorphia Checklist (Coles, Fernhoff, Lynch, Falek, & Dellis, 1997). This Checklist, which was developed for use in the initial infancy study, is similar to that used by other investigators (Jones, et al. 2006; Holme et al, 2005). It was administered without knowledge of the participants’ alcohol exposure status by a pediatric geneticist or a nurse trained by the geneticist and included a weighted list of 30 physical characteristics associated with prenatal alcohol exposure. Those that are considered to be sentinel features of FAS (e.g., absent/indistinct philtrum; short palpebral fissures) are weighted as “3” while other characteristics that are observed in FASD may be weighted as 2 (e.g., ptosis, hypoplastic mandible ) or 1 (e.g., clinodactyly). Weighted scores are then summed to yield a total “dysmorphia” score. Validity of this measure has been measured via correlation with alcohol use levels reported by mothers (Coles, et al. 1997) and reliability via test-retest assessments in a clinical setting (Blackston, et al., 2004). This measure has been used consistently throughout this longitudinal study. At each follow-up, participants also completed tests of intellectual ability (e.g., Wechsler, 1991; Wechsler, 1999).
For the young adult follow-up, 108 individuals were selected for imaging and, of these, 92 had useable data. The sample in this paper includes three groups of participants: 1) Control (n=26): Participants whose mothers did not consume alcohol during pregnancy; 2) Dysmorphic (DYSM; n = 30): Participants who were exposed to alcohol prenatally and received a checklist score at least one standard deviation above the mean of the sample of all participants; and 3) Alcohol Exposed (ARND, n = 36): Participants who were exposed to alcohol prenatally, but whose dysmorphia scores were less than one standard deviation above the mean of the sample and whose intelligence test scores (Wechsler, 1991; Wechsler, 1999) at the mid-adolescent or young adult follow-up were in the same range as those in the Dysmorphic group (that is, IQ <84, which is 1 standard deviation less than the population mean). This selection process assured that imaging sessions were completed for those who showed cognitive effects of prenatal exposure even though physical effects were not apparent. Using the Institute of Medicine’s (IOM: Stratton, et al, 1996) nomenclature, they are designated as having “alcohol related neurodevelopment disorder-ARND”. Sixteen of the 108 participants who were imaged were excluded for the following reasons: Left handed (1 excluded from the Control group and 1 from the ARND group); Poor quality images: (3 excluded from the Control group, 8 from the Dysmorphic group, and 3 from the ARND group).
Procedure
Eligible participants from the longitudinal cohort were contacted by mail or phone concerning the young adult wave of the follow-up study. Those who were interested in participating completed a consent procedure in which the study goals and procedures were explained and they were allowed to ask questions; consent forms approved by the Emory University School of Medicine Institutional Review Board were signed. During this process, the confidentiality of participants’ mothers was protected; that is, no information about mother’s alcohol or other substance use during the pregnancy of the now-adult child was revealed. For the evaluation visit, participants were transported by project outreach workers to the laboratory for a day-long evaluation which included an assessment of memory and ability, a medical evaluation, and an interview session. In addition to transportation, participants received lunch and compensation ($100 per session) for their time and effort.
Participants who were eligible for the imaging component based on group assignment and intelligence scores were screened for other factors that would exclude them from the imaging procedure. These factors included presence of metal in the body (e.g., pins, screws, braces on teeth, bullet fragments), pregnancy, extreme obesity, or claustrophobia. Women were asked to complete a pregnancy test on the day of the appointment. For the imaging session, participants were transported to the Emory campus. All participants completed a training session for the task used in the functional portion of the imaging session. When these procedures were completed, the participant was taken to Emory Hospital where the imaging session took place.
Measures
Structural Imaging and Data Analysis
For each participant, T1-weighted images were obtained on a 3.0 Tesla Siemens Magnetom TRIO scanner (Siemens Medical Solutions, Malvern, PA) with an MPRAGE sequence (TR = 2600 ms, TE = 3.02 ms, Flip Angle = 8°, voxel size = 1×1×1 mm3). With these images, FreeSurfer (http://surfer.nmr.mgh.harvard.edu/fswiki, version 4.0.1) was used to automatically segment sub-cortical structures and cortical regions (Dale, Fischl, & Sereno, 1999; Desikan et al., 2006; Fischl, Sereno, & Dale, 1999; Fischl et al., 2002; Fischl et al., 2004) through FreeSurfer’s troubleshooting reconstruction work flow (see details on: https://surfer.nmr.mgh.harvard.edu/fswiki/RecommendedReconstruction). During this procedure, manual edits were carried out to remove the optic nerve and part of the dura which was incorrectly segmented as grey matter. After the reconstruction was finished, volumetric data for the segmented cortical and subcortical regions were also automatically calculated by FreeSurfer. Of all these segmented areas, those most often associated with learning and memory were selected as the regions of interest (ROIs) and their volumetric data were used in further analysis.
Assessment of Learning and Memory
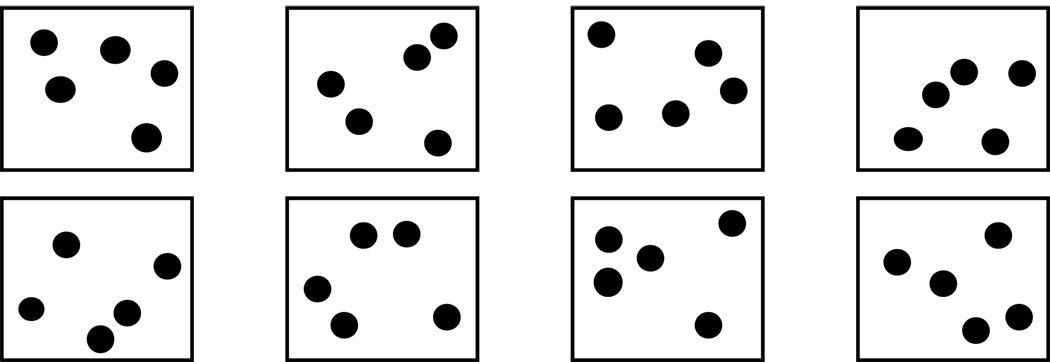
Learning and memory were assessed using the Verbal Selective Reminding Memory Test (VSRT) (Buschke and Fuld, 1974) and its nonverbal counterpart, the Nonverbal Selective Reminding Memory Test (NVSRT) (Fletcher, 1985). We have reported on the results of these memory procedures in a previous paper (Coles, et al, 2010) and will describe these procedures briefly here. The VSRT requires an individual to recall a list of 12 unrelated words that are orally presented at the rate of 1 word every 2 seconds. The words are: Shine, Disagree, Fat, Wealthy, and Drunk, Pin, Grass, Moon, Prepare, Prize, Duck, and Leaf. Eight learning trials are presented. For each trial, the person is reminded only of those words that were not recalled correctly on the previous trial. The person is then asked to provide all the words on the list, including those that were previously recalled without reminders. The NVSRT consists of an array of dots that are presented in 8 separate boxes (See Figure 1). The examiner points to a targeted dot in each of the boxes and the person is then required to point to the same dots during the recall trial. Similar to the procedure used with its verbal equivalent, the person is reminded on subsequent trials only of the targeted dots that were not recalled. Then they are required to recall all of the targeted dots, including those that were recalled previously without reminders. In this paper, the dependent variables include number of words/dots recalled immediately after the final learning trial, delayed recall (number of words/dots recalled after 30 minutes), and learning slope1 as a measure of efficiency of encoding.
Figure 1.
Stimuli for the Nonverbal Selective Reminding Task. The task is to recall the targeted dot from each box.
Assessment of Cognitive Ability
Cognitive ability (that is, IQ) was assessed using the Wechsler Abbreviated Scale of Intelligence (WASI; Wechsler, 1999). This is a short form of the most widely used measure of adult ability and demonstrates a high correlation with longer versions of this test. The WASI was administered as part of a larger neuropsychological battery by a psychologist or graduate student trained in assessment who was blind to alcohol group status.
Medical Evaluation. Dysmorphia Exam
A nursing examination was carried out for each participant. This included a screen of hearing and vision, a medical history, as well as completion of the Dysmorphia Checklist for this adult visit. Nurses carrying out the examination were trained by a geneticist familiar with the physical signs associated with prenatal alcohol exposure. Current scores were used for all analyses described in this paper. Alcohol Use. Alcohol abuse is often associated with memory deficits (Schottenbauer, Hommer, Weingartner, 2007). For this reason, adult participants were interviewed regarding their own current alcohol and other drug use. They completed the Addiction Severity Index (ASI: McLellan et al, 1992) and the Drug Checklist (Coles, et al., 1992). Information about alcohol use included a quantity/frequency measure that allowed calculation of ounces of absolute alcohol used each week (oz/AA/wk) as well as information about alcohol use history. In addition, urine samples were requested to screen for drug use, and blood samples were collected to evaluate the effects of alcohol on liver function. Laboratory tests were used to confirm self report.
Archival records
Information was obtained from archival records regarding maternal drug and alcohol use and results of previous measurements of participants’ ability and physical effects of alcohol (i.e., dysmorphia checklist scores). These measures were used to initially categorize the groups for recruitment.
Data Analytic Plan
The purpose of this paper is to demonstrate that cognitive deficits found in individuals who were prenatally exposed to alcohol result from effects on brain volume and that observable physical effects of alcohol (dysmorphia) are indicative of underlying effects on brain. To test these hypotheses, it is necessary to demonstrate that exposed individuals have cognitive deficits, in this case, poorer memory performance, as well as reduction in volume in specific brain regions. It is also necessary to demonstrate a relationship between observable features associated with prenatal exposure and the proposed mediator (brain volume) and between the mediator and the memory outcome. In order to evaluate these hypotheses, we adopted the following analytic strategy.
Memory Performance
To examine the effects of prenatal alcohol exposure on learning and recall, we selected three indicators of performance for each memory test. These were: Total amount recalled at the final learning trial (Time 8) which should reflect participants’ “best performance”, learning rate (i.e., slope) which reflects a participant’s encoding efficiency, and recall following a 30 minute delay which indicates the amount actually retained. Thus, there were 6 outcome variables, 3 each for the Verbal and the Nonverbal Memory Tests. Multivariate analyses of variance were used with these outcomes as the dependent variables and Exposure group (3: Control, Dysmorphic, ARND) as the independent factor. Analysis of the linear tread was included as a planned comparison, and Bonferroni procedures carried out post hoc to identify significant group differences.
Brain Volume
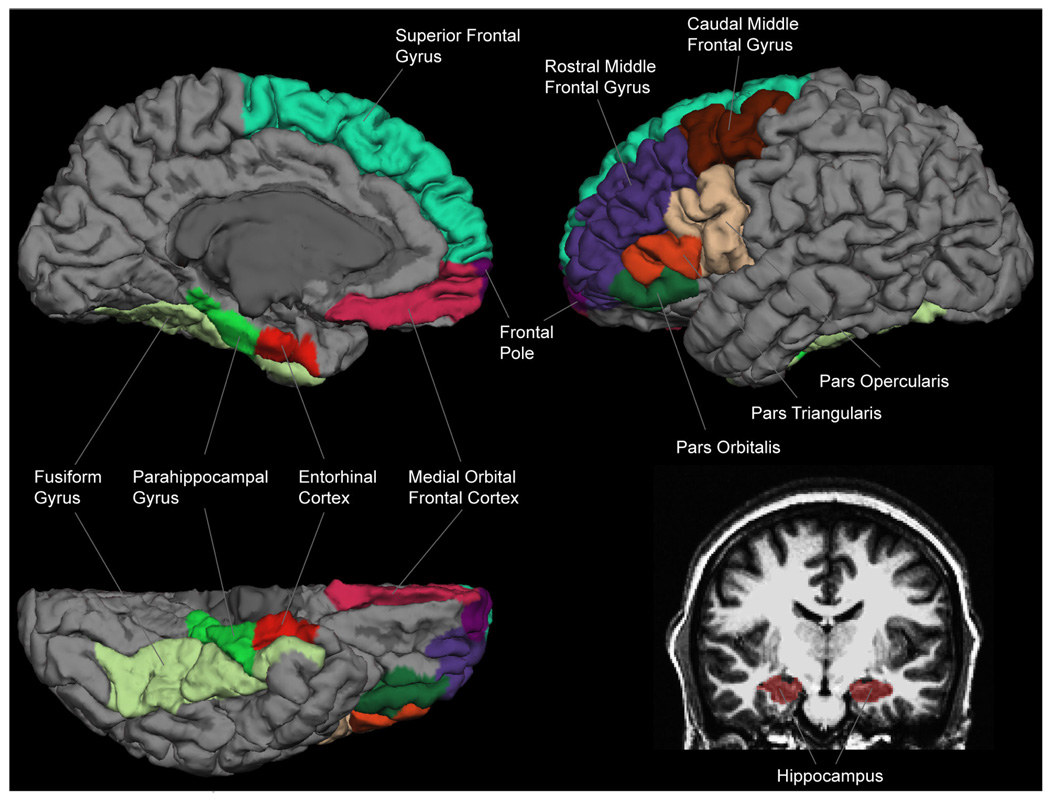
Volume of ROIs was obtained through an automated segmentation of T1-weighted images and multivariate analysis of variance, as described above, was used to examine the impact of prenatal exposure on brain volume. Candidate brain regions were selected a priori. In the Medial Temporal region, we included the hippocampus, entorhinal cortex, parahippocampal gyrus, and fusiform gyrus, which are associated with encoding and memory. In the Frontal lobes, we included areas from anterior (medial orbital frontal, superior frontal, frontal pole, parsobitalis, rostral medial frontal) and Medial Frontal (caudalmiddlfrontal, parsopercularis, parastrangularis) which are associated with working memory and the employment of memory strategies (Brown, McKone, & Ward, 2010; Churchwell, Morris, Musso, & Kesner, 2010). GLM in SPSS 15.0 was used for statistical analysis. Because women have smaller brain volumes than men, gender was used as a covariate. Group (Control, Dysmorphic and ARND) was set as a between-subject factor. For regions showing the group main effect, pair-wise comparisons among the three participant groups were performed using the Least Significant Difference (LSD) method.
Brain/Behavior Relationships
To examine the extent to which brain volume accounted for variance associated with memory performance, the six indices of memory efficiency were used as dependent variables in a series of stepwise regression procedures with the volume of ROIs from the medial temporal and frontal regions (from both right and left hemispheres), as predictors.
Mediation Analyses
The final goal of the analysis was to demonstrate that the PAE effects on brain mediated the relationship between physical characteristics associated with prenatal alcohol exposure and memory performance. To test the hypothesis that volume reductions in specific brain regions mediate the relationship between observable physical characteristics of alcohol exposure (dysmorphic features) and memory outcomes, multiple mediation analyses were performed using Preacher and Hayes’ (2008a) procedure. This procedure allows the evaluation of the indirect effect of two or more mediating variables at the same time with the significance of each proposed mediator evaluated in the context of the full model (Preacher & Hayes, 2008b). In these analyses, a bootstrapping resampling strategy was employed with 5,000 bootstrap samples used. The models tested included physical characteristics of alcohol (dysmorphia score) as the independent variable (IV), memory outcomes (6 outcomes) as the dependent variables (DVs) and hippocampal volume and other candidate brain regions as potential mediating variables (MV). For each memory outcome examined, mediation analysis used those brain regions that the regression analyses had selected as contributing significant variance to that specific outcome. Coefficients showing the relationships between the independent variable, each mediating variable and the dependent variable were calculated as well as the total effect (IV plus MVs) on the DV, direct effect (IV minus MVs) on the DV, and the significance of total and specific indirect (Mvs) effects.
Results
Characteristics of the Study Sample
The demographic, physical and exposure characteristics of the study participants are shown in Table 1. There were no significant group differences in gender, ethnicity, income, education, or current alcohol use. On the factors that characterize the effects of alcohol, dysmorphic features, ability level, and growth, the DYSM group was significantly different from the other two groups; these results were expected given the criteria for group assignment. Current alcohol use by adult participants was unrelated to memory performance or brain volume.
Table 1.
Demographic, Prenatal Exposure, and Growth Characteristics for Participants (N=92) by Exposure Group
| Variable | Group | Statistic | Significance | ||
|---|---|---|---|---|---|
| Control (n= 26)a | ARND(n=36)a | DYSM (n= 30)a | |||
| Gender – % male | 46.2 | 27.8 | 46.7 | X2(2)=3.202 | n.s. |
| Ethnicity – % African-American | 100 | 97.2 | 100 | X2(2)=1.573 | n.s. |
| Age at imaging, M (SD) | 22.7 (1.7) | 23.1 (1.6) | 23.1 (2.2) | F(2,89)=.429 | n.s. |
| Monthly income – $ in past 30 days, M (SD) n=91 | 1263 (1765) | 643 (455) | 1242 (1811) | F(2,88)=2.002 | n.s. |
| Education completed – years, M (SD) n=91 | 12.3 (1.6) | 11.7 (1.5) | 11.8 (1.3) | F(2,88)=1.188 | n.s. |
| Full-scale IQ, M (SD) n=91 | 84.0 (8.6) | 80.5 (12.1) | 76.0 (12.0) | F(2,88)=3.506 | p=.034 |
| Dysmorphia rating at adult visit, M (SD) n=91 | 3.62 (3.3) | 4.7 (3.8) | 9.43 (7.8) | F(2,88)=9.893 | p<.001 |
| Adultweight – lbs., M (SD) n=90b | F(2,84)=7.647 | p=.001 | |||
| Male | 203.6 (55.2) | 198.3 (52.5) | 161.6 (47.4) | ||
| Female | 175.4 (46.8) | 172.3 (48.1) | 130.1 (29.5) | ||
| Adult head circumference - cm, M (SD) n=91b | F(2,85)=4.780 | p=.011 | |||
| Male | 59.9 (1.8) | 58.5 (1.6) | 56.7 (3.4) | ||
| Female | 57.2 (4.0) | 57.1 (2.9) | 55.5 (3.5) | ||
| Amount of alcohol use currently by adult – AA per week, M (SD) | 0.87 (2.02) | 1.32 (1.89) | 0.86 (1.43) | F(2,88)<1 | ns |
| Amount of alcohol exposure during pregnancy – AA per week, M (SD) | 0 (0) | 7.7 (13.1) | 13.5 (13.6) | F(289)=9.904 | p<.001 |
| Cigarettes during pregnancy – % using, n=91 | 30.1 | 65.7 | 83.3 | X2(2)=16.679 | p<.001 |
| Marijuana during pregnancy – % using | 19.2 | 36.1 | 30 | X2(2)=2.084 | n.s. |
| Cocaine during pregnancyc – % using, n=88 | 0 | 13.9 | 7.7 | X2(2)=3.981 | n.s. |
If data for a variable are not available for some participants, the n used for the analysis is noted next to the variable name.
Two-way Group X Gender analyses of variance were completed for growth variables. In addition to group effects noted in table, gender was significant for adult weight and for adult head circumference. No interaction effects were significant.
Recruitment occurred before the “cocaine epidemic” on the 1980s; “crack” use did not occur and frequency and amount of cocaine use was low.
Memory
As shown in Table 2, with the exception of Delayed Recall of Nonverbal items, all comparisons demonstrated significant differences in performance associated with Group with a significant linear tread in the expected direction. That is, the Control group showed the most and the Dysmorphic group the least efficient learning and recall, with the ARND group intermediate. For the five variables which showed differences, the Control group was always significantly better than the Dysmorphic group.
Table 2.
Recall Outcomes by Exposure Group and Modality (N=92)
| Control | ARND | DSYM | |||
|---|---|---|---|---|---|
| Recall Outcome | (n=26) | (n=36) | (n=30) | Statistic1 | |
| Verbal | |||||
| Recall 8th Trial Final Learning Trial |
10.2 (1.8) | 9.2 (2.0) | 8.4 (2.6) | F(2, 87)=4.82, p<.01 C> DYSM2 |
|
| Linear trend: p<.003 | |||||
| Delayed Recall | 8.3 (2.6) | 7.3 (2.7) | 6.4 (2.6) | F(2, 86)=3.4, p<.04 C> DYSM2 |
|
| Linear trend: p<.01 | |||||
| Learning Slope | 0.36(0.14) | 0.33 (0.14) | 0.26 (0.13) | F(2, 87)=3.96 p<.02 C> DYSM2 |
|
| Linear trend: p<.007 | |||||
| Nonverbal | |||||
| Recall 8th Trial Final Learning Trial |
7.3 (1.0) | 6.5 (1.7) | 5.7 (2.4) | F(2, 89)=5.21, p<.007 C> DYSM2 |
|
| Linear trend: p<.002 | |||||
| Delayed Recall | 5.7 (1.8) | 5.8 (1.8) | 5.507 (2.2) | F(2, 86)=1.05 ns | |
| Learning Slope | 0.24 (0.1) | 0.21 (0.12) | 0.14 (0.16) | F(2,87)=3.82, p<.03 C> DYSM2 |
|
| Linear trend: p<.01 | |||||
Multivariate analysis of variance
Bonferroni post hoc analysis
Brain Volume
Although there was an overall reduction in brain volume associated with the alcohol exposure group (F (2, 89) =3.82, p<.03) with many regions affected, we are concerned, in this paper, with those areas most often associated with learning and memory. Those brain regions that may affect memory function (regions of interest, ROIs) are shown in Figure 2. Table 3 shows the results of the analyses listing both the Brodmann areas involved and the group differences in volume. For simplification, the volumetric data from the homologous regions in the left and right hemispheres were combined in Table 3, although volumes in each hemisphere were also analyzed separately.
Figure 2.
Brain regions (ROIs) examined in the current study. The cortical ROIs are shown on a cortical surface from the medial, lateral and inferior views. The sub-cortical ROI (hippocampus) is shown on a T1-weighted image.
Table 3.
Total Brain Volume in Cubic Millimeters (Mean and Standard Deviation) in Medial Temporal and Frontal Regions by Alcohol Group (N=92). Multivariate Analysis controlling for Gender
| 1. | 2 | 3 | |||
|---|---|---|---|---|---|
| Control | ARND | Dysmorphic | Statistic | ||
| Brain Region | Brodmann Area |
n=26 | n=36 | n=30 | |
| Medial Temporal | M (SD) | M (SD) | M (SD) | ||
| Hippocampus | 7271.81 | 7064.86 | 6658.4 | F(2,88)=5.5, p<.006 | |
| (919.27) | (870.57) | (972.91) | 1&2>3, p<.004 | ||
| Parahippocampal gyrus | 27, 28, 34–36 | 3871.54 (542.59) |
3370.36 (388.23) |
3101.8 (470.87) |
F(2,88)=22.25, p<.000 |
| 1>2>3, p<.000 | |||||
| Endorinal | 28,34 | 3351.73 | 3261.13 | 3217.97 | F(2,88)<1, NS |
| (550.54) | (596.29) | (581.72) | No groups sig diff | ||
| Fuisform | 19, 20, 37 | 16793.77 (2670.14) |
15827.92 (2329.52) |
14770.23 (2300.72) |
F(2,88)=7.07, p<.001 |
| 1&2>3, p<.006 | |||||
| Frontal | |||||
| Frontal Pole | 10,11 | 1792.15 | 1697.39 | 1731.83 | F(2,88) <1, NS |
| (245.61) | (293.09) | (311.08) | No groups sig diff | ||
| Caudalmiddlefrontal | 6 | 11301.96 | 10196.28 | 9956.9 | F(2,88)=3.33, p<.04 |
| (2479.74) | (1778.42) | (2067.34) | 1& 2>3, p<.01 | ||
| Medialorbitalfrontal | 11,12 | 8603.54 | 7972.58 | 7975.5 | F(2,88)=2.11, NS |
| (1452.53) | (1179.35) | (1147.22) | 1>3, p<.05 | ||
| Superior Frontal | 9, 10 | 41076.15 (4872.54) |
38511.64 (3795.22) |
37058.43 (4883.35) |
F(2,88)=7.53, p<.001 |
| 1&2>3, p<.000 | |||||
| Rostral Medial Frontal | 10, 46 | 29081.04 (4258.5) |
27244.44 (3921.29) |
25736.6 (5313.45) |
F(2,88)=5.18, p<.007 |
| 1&2>3, p<.003 | |||||
| Parsopercularis | 44 | 8208.12 | 7746.17 | 7578.47 | F(2,88)=1.57, NS |
| (1788.25) | (1083.1) | (1304.72) | No groups sig diff | ||
| Parastrangularis | 45 | 8327.88 | 7519.11 | 7257.97 | F(2,88)=4.79, p<.01 |
| (1455.57) | (1391.79) | (1509.76) | 1>3, p.003 | ||
| Parsorbitalis | 47 | 4890.96 (794.85) |
4645.67 (637.64) |
4334.60 (825.41) |
F(2,88)=5.61, p<.005 |
| 1&2>3, p.003 | |||||
In these data, there were significant group differences in all areas except the entorhinal, the frontal pole and the parastrangularis. In most cases, the ARND group’s data were intermediate between that of the unexposed controls and the dysmorphic group’s results. This pattern of outcomes was also noted for the right but not the left hippocampus when these regions were examined separately (left hippocampus (LH): F (2, 89) =1.88, ns; right hippocampus (RH): F (2, 89) =5.82, p<.004). Several other medial temporal regions (right fusiform, F (2, 89) =6.07, p<.003; left (F (2, 89) =15.16, p<.000) and right (F (2, 89) =15.16, p<.000) parahippocampal gyrus) showed specific differences associated with the alcohol group. Frontal regions did not show significant hemispheric differences related to group.
Brain/Behavior Relationships
Results of stepwise regression analyses are shown in Table 4. All analyses yielded significant models. For Verbal Recall at Trial 8, the model accounting for most variance was significant (F (8,91=4.75, p<.001) with an R of .647, and an R2 of .419, suggesting that the predictive factors accounted for approximately 42% of the variance in verbal recall. For Nonverbal Recall at Trial 8, a similar procedure yielded a model that explained approximately 25% of the variance (F (8.91) =3.52, p<.001). Note that hippocampus and other Medial Temporal regions were all retained as predictors, while a cluster of frontal regions (Table 4) were retained in the Verbal but not the Nonverbal model.
Table 4.
Regression Models: Brain Volume and Selected Memory Outcomes
| Recall Trial 8 | |||||||
|---|---|---|---|---|---|---|---|
| Verbal Recall-Trial 8 | Nonverbal Recall-Trial 8 | ||||||
| ROI Volume | Beta | t-score | p-value | Beta | t-score | p-value | |
| Model 1 | Left Hippocampus | −.184 | <1 | ns | −.063 | <1 | ns |
| Right Hippocampus | .572 | 2.87 | .005 | .475 | 2.36 | .02 | |
| Model 2 | Left Hippocampus | −.176 | <1 | ns | −.028 | <1 | ns |
| Right Hippocampus | .71 | 3.30 | .001 | .433 | 1.9 | .06 | |
| L Parahippocampus | −.03 | <1 | ns | −.04 | <1 | ns | |
| R Parahippocampus | −.05 | <1 | ns | −.18 | 1.45 | ns | |
| L Endorinal Cortex | −.003 | <1 | ns | −.132 | −1.09 | ns | |
| R Endorinal Cortex | −.095 | <1 | ns | −.20 | 1.95 | .06 | |
| L Fusiform | −.34 | −2.67 | .009 | −.15 | −.1.13 | ns | |
| R Fusiform | −.009 | <1 | ns | .089 | <1 | ns | |
| Frontal | (Selected below) | ||||||
| R Superior Frontal | .431 | 3.32 | .001 | Not in model | |||
| R Parsopercularis | −.307 | −2.98 | .004 | Not in model | |||
| L Parsorbitalis | .290 | 2.58 | .01 | Not in model | |||
| R Rostral Medial Frontal |
−.266 | −2.87 | .02 | Not in model | |||
| Slope | |||||||
| Verbal Slope | NonVerbal Slope | ||||||
| ROI Volume | Beta | T-score | p-value | Beta | T- score |
p-value | |
| Model 1 | Left Hippocampus | −.459 | −2.18 | .03 | −.091 | <1 | ns |
| Right Hippocampus | .586 | 2.78 | .007 | .439 | 2.14 | .04 | |
| Model 2 | Left Hippocampus | −.431 | −1.90 | .05 | −.084 | <1 | ns |
| Right Hippocampus | .709 | 2.91 | .005 | .518 | 2.2 | .03 | |
| L Parahippocampus | −.03 | <1 | ns | −.134 | <1 | ns | |
| R Parahippocampus | .16 | 1.25 | ns | .16 | 1.22 | ns | |
| L Endorinal Cortex | −.11 | <1 | ns | .16 | 1.29 | ns | |
| R Endorinal Cortex | .04 | <1 | ns | −.02 | <1 | ns | |
| L Fusiform | −.26 | −1.83 | .07 | −.17 | −1.25 | ns | |
| R Fusiform | −.03 | <1 | ns | .029 | <1 | ns | |
| Frontal | (selected below) | ||||||
| R Frontal Pole | Not in model | −.276 | −2.62 | .01 | |||
| Delayed Recall | |||||||
| Verbal Delayed Recall | NonVerbal Delayed Recall | ||||||
| ROI Volume | Beta | t-score | p-value | Beta | t-score | p-value | |
| Model 1 | Left Hippocampus | −.249 | −1.21 | ns | −.198 | <1 | ns |
| Right Hippocampus | .546 | 2.65 | .009 | .548 | 2.70 | .008 | |
| Model 2 | Left Hippocampus | −1.91 | <1 | ns | −.202 | <1 | ns |
| Right Hippocampus | .755 | 2.24 | .002 | .668 | 2.90 | .005 | |
| L Parahippocampus | −.049 | <1 | ns | −.02 | <1 | ns | |
| R Parahippocampus | −.024 | <1 | ns | −.01 | <1 | ns | |
| L Endorinal Cortex | −.017 | <1 | ns | .28 | −2.28 | .025 | |
| R Endorinal Cortex | −.077 | <1 | ns | .195 | 1.84 | .07 | |
| L Fusiform | −.30 | −2.21 | .03 | .116 | <1 | ns | |
| R Fusiform | .139 | <1 | ns | .064 | <1 | ns | |
| Frontal | (selected below) | ||||||
| R Parsopercularis | −.266 | −2.37 | .02 | Not in model | |||
Recall Trial 8: Verbal: Model 1: R=.42, R2=.18, F(2, 89)=9.54, p<.000; Model 2: R=.65, R2=.42, F(12,79)=4.75, p<.000; Nonverbal: Model 1: R=.42, R2=.18, F(2, 89)=9.61, p<.000; Model 2: R=.50, R2=.25, F(8, 83)=3.52, p<.001.
Slope: Verbal: Model 1: R=.29, R2=.08, F(2, 89)=4.02, p<.02; Model 2: R=.38, R2=.14, F(8, 83)=1.73, p=.10; NonVerbal: Model 1: R=.36, R2=.13, F(2, 89)=6.5, p<.002; Model 2: R=.47, R2=.22, F(9,82)=2.59, p<.01.
Delayed Recall: Verbal: Model 1: R=.35, R2=.12, F(2, 89)=6.21, p<.003; Model 2: R=.49, R2=.24, F(9,82)=2.83, p<.006; NonVerbal: Model 1: R=.39, R2=.15, F(2, 89)=7.84, p<.001; Model 2: R=.49, R2=.24, F(8, 83)=3.23, p<.003.
For Verbal Slope, only hippocampal ROIs entered the model with 8% of the variance accounted for, with R=.29, F (2, 91) =4.02, p<.02 and only right hippocampus was statistically significant (t=2.78, p<.007). For Nonverbal Slope, there was a similar pattern; however, in the full model, which accounted for 22% of variance (R=.47, F (9, 92) =2.59, p=.01), one frontal ROI (right frontal pole) was also significant (t=−2.62, <p<.01).
For Verbal Delayed Recall (Table 4), the model accounting for most variance (R=.489, R2 =.24, F (8, 91) =2.87, p<.006) had right hippocampus, left fusiform and right parsopercularis as significant predictors, that is, it included both Medial Temporal and Frontal regions. For Nonverbal Delayed Recall, the model (R=.487, R2 = .24, F (8, 91) =3.23, p<.003) included only Medial Temporal ROIs, the right hippocampus and left entorhinal as significant predictors. A further set of regression analyses were carried out adding global ability level (Full Scale Intellectual Quotient, FSIQ: Weschler, 1999) to the predictors to determine whether memory efficiency could be attributed to global ability level. For Verbal Delayed Recall, IQ added significant variance (beta=.274, t=2.34, p<.02) to the other factors. For other memory outcomes, IQ did not add significant variance to performance beyond that accounted for by volume of candidate brain regions.
Evaluation of Mediation of Memory Performance by Brain Volume
As shown above, analyses of memory performance and volume of brain ROIs indicated that both sets of outcomes were related to prenatal alcohol exposure. Regression modeling indicated that the volume in certain brain regions was associated with recall performance and the efficiency of learning (slope). A final step was to examine the hypothesis that memory efficiency was impacted by the effects of prenatal alcohol exposure acting through effects on brain, particularly on hippocampus. Based on the results of the regression analyses (Table 4), the Preacher and Hayes procedure (2008a) was used to examine the extent to which volume in the hippocampus and other candidate brain regions in medial temporal and frontal regions mediated the relationship between dysmorphic features and memory outcome. The procedure allows the assessment of more than one mediator simultaneously. Each of the six memory outcomes was examined independently to see how the addition of specific mediators (brain volume ROIs) affected the relationship between the predictor (dysmorphic features) and the outcomes (recall and learning rate). Only those brain regions that regression models (see Table 4) found to be associated with a particular memory outcome were included in the mediation models (for example, see Nonverbal Recall-Trial 8 in Table 4 in which only right hippocampus is implicated).
Recall at Trial Eight
Verbal Recall was examined in a series of mediation models because so many candidate regions contributed to the regression model. Only regions that had a significance level of less than .05 were considered. Right hippocampal volume was a significant mediator of recall (Effect=−.079. se=.027, z=−2.87, p<.004), but the fusiform region was not (Effect= .029. se=.017, z=1.66, p=.10). Similarly, right parsorbitalis (Effect= .004. se=.014, z=0.32, p=.75), right rostral medial frontal (Effect= .028. se=.023, z=1.22, p=.22) and right parsopercularis (Effect= .025. se=.0175, z=1.69, p=.09) regions were not found to mediate this relationship. Thus, only right hippocampus (RH) was a significant mediator (Effect= −.057 se=.022, z=−2.59, p<.01) in the relationship between alcohol-related dysmorphic features and verbal recall. The unmediated relationship (c path: Coefficient=−. 141, se=.041, t=−3.44, p<.0009) was reduced significantly when RH was added (c’ path: Coefficient=−.091, se=.043, t=−2.15, p<.04).
For the nonverbal test, only RH volume was tested as a mediator since other brain regions did not show a significant relationship with the DV. It was found that the addition of RH significantly (Effect= −.041, se=.016, z=−2.52, p<.01) reduced the relationship (c path: Coefficient=−. 129, se=.034, t=−4.12, p<.0001) between the dysmorphic features and recall although this relationship remained significant (c’ path: coefficient=−.089, se=.034, t=−2.72, p<.007) suggesting that other factors have not been identified.
Learning Slope
For verbal learning slope, both left and right hippocampal volume were tested as mediators as other brain regions did not reach significance in the regression model. In this analysis the significant relationship between dysmorphic features and learning efficiency (c path: coefficient=−.005, se=.003, t=−2.01, p<.05) was reduced to non-significance (c’ path: coefficient=−.004, se=.003,t=−1.36,p=.18) when these factors were added, with both LH (effect=.005, se=.002, z=1.97, p<.05) and RH (effect= −.005, se=.003, z=−2.24, p<.03) being significant mediators to this relationship. For nonverbal learning slope, only RH was used as a mediator and was found to significantly (effect=−.003, se=.001, z=−2.24, p<.03) affect the relationship between dysmorphic features and learning efficiency (c path: coefficient=−.007, se=.002, t=−3.02, p<.003; c’ path: coefficient=−.004. se=.002, t=−1.82. p=.07).
Delayed recall
For verbal delayed recall, volume of the RH as well as left fusiform, from the Medial Temporal region and right parsopercularis from the Frontal region were included in the model. Before the addition of the mediators, a significant relationship was observed between dysmorphic features and delayed recall (c path: coefficient=. 117, se=.051, t=−2.30, p<.03); with the addition of the mediators, this relationship was no longer significant (c’ path: coefficient=−.075, se=.051, t=−1.47, p=.15). RH was found to be the significant mediator (effect=−.110, se=.036, z=−3.06, p<.002), with the other two regions only approaching significant level: left fusiform (effect=.037, se=.021, z=1.73, p=.08) and right parsopercularis (effect=.032, se=.018, z=1.73, p=.08).
For nonverbal delayed recall, RH and left endorinal cortex were entered as mediators. The significant relationship between dysmorphic features and delayed recall (c path: coefficient=−. 119, se=.033, t=−3.59, p<.0006) was reduced (c’ path: coefficient=−.073, se=.034, t=−2.13, p<.04) by the addition of these mediators. However, only RH (effect=−.053, se=.02, z—2.63, p<.009) was identified as a significant mediator. Left endorinal cortex was not significant (effect=.007, se=.009, z=0.86, p=.39).
Discussion
The current studied examined the impact of prenatal alcohol exposure on brain development and memory function with the expectation that both would be impaired as a function of such exposure, and that the impact on the brain could be shown to mediate the relationship between physical features and cognitive outcomes. Although there has been an assumption that this relationship exists, it has not been demonstrated explicitly. Several previous studies have reported significant correlations between imaging findings and neurocognitive outcomes (O’Hare, et al., 2009; Malisza, et al, 2005; Sowell, et al. 2007; Sowell, et al. 2008). However, none has examined the role of observable physical effects of exposure in the complex brain-behavior relationship.
In the current study, individuals identified as alcohol affected had significantly smaller brains than those who were not exposed. Even the non-dysmorphic ARND individuals, who did not demonstrate behavior problems and who had no clinical diagnosis, could be discriminated from their age and SES-matched controls based on brain volume in several areas. The dysmorphic individuals demonstrated significant differences from the nonexposed controls in memory function on the majority of the measures investigated. This group performed more poorly than the nonexposed control group in terms of learning rate and amount recalled on both verbal and nonverbal tasks. However, examination of Table 3 suggests that, as suspected, there is a spectrum of impact. All of these outcomes demonstrated a significant linear trend, with the ARND group intermediate to the unexposed controls and the clearly affected dysmorphic group.
There was also an effect of dysmorphic status, a marker of the effects of alcohol exposure, on memory, and this was shown to be mediated by the size of the hippocampus. These results confirm those previously observed in animal models of FASD (Berman & Hannigan, 2000) and suggest that the physiological basis for this specific neurocognitive function, the ability to encode information, is impaired as a result of prenatal exposure. While volume of brain region is a crude measure that only suggests the way in which alcohol has affected brain development and, as a result learning rate and memory function, these results suggest that further research is warranted to understand how memory is affected by prenatal exposure and whether there are any ways in which individuals can compensate for these injuries.
Some research has suggested that nonverbal (or visual/spatial) memory is more affected by alcohol-exposure than verbal memory (Kaemingk & Halverson, 2000;Uecker & Nadel, 1998). In contrast, the current results suggest that both verbal and nonverbal memory were affected equally and that these effects have a similar basis, an effect on the hippocampus, particularly the right hippocampus. Examining the role of other memory-related brain regions did not offer additional information. In this sample, right hippocampal volume was more affected than the left and it appeared to mediate many of the effects of alcohol on memory function. It may be assumed that the right hippocampus is more associated with nonverbal than verbal encoding and such a relationship may account for some of these findings. However, as noted by other authors (Smith & Squire, 2009; Wheeler, et al, 1995), verbal memory often relies more heavily than nonverbal, on learned memory strategies to support encoding. Use of such strategies relies on functions supported by frontal regions so that, to the extent that such strategies are available to the individual, the learning process may be more or less effective. Thus, learning based on repetition or exposure (as is probably the case for both memory tasks used here) may be mediated directly by the hippocampus, while memory tasks that require strategy use may employ both hippocampus and frontal areas, a result that is suggested by the regression models in Table 4. However, to evaluate this hypothesis would require a different type of memory task than was used in this study, one designed to require specific strategy use for effective memorization.
There are limitations in the current study. The sample was selected from a low income population and, for this reason, some of these results may not generalize to different populations. In addition, the sample included only those who were able to complete the imaging protocol. Thus, those most severely affected by alcohol may not have been able to participate. Only right handed individuals were included in the study. However, this restriction did not eliminate a great number of participants, and there was no systematic bias associated with group status. Finally, as in all prenatal exposure studies, the investigators did not have control over the administration of the drug nor over the behavior of individuals subsequent to enrollment. This is particularly true in a long-term study of this kind. Thus, it is possible that there are other factors influencing outcomes in the alcohol-affected group. We controlled these factors to the extent possible through the original subject selection process which allowed us to document the extent of alcohol and other drug exposure and to monitor other possible environmental confounders such as educational status and current alcohol use.
Although prenatal alcohol exposure is a leading cause of developmental and learning problems in the United States and world wide, there has been insufficient research examining neurodevelopment outcomes in a systematic manner. To some extent, this problem is the result of the difficulty inherent in finding appropriate research samples. In working with human samples, there are always limitations. Clinically-based studies are systematically biased in well known ways, and one advantage associated with the current study is access to a cohort of young adults whose prenatal exposure is well documented. Most other imaging studies of FASD have relied on clinical samples with retrospective reports of exposure that introduce a greater degree of variance than is present here. However, exposure samples of this kind often do not include the whole range of negative outcomes that may be apparent in those applying for clinical care. Having convergent data from different kinds of studies assures that results can be relied on.
These results strongly suggest that, even after more than two decades, learning and memory are impacted by prenatal exposure and that these effects are mediated through teratogenic damage to the developing brain that is not resolved with maturity. This study also provides evidence that, despite a spectrum of impact, individuals showing the physical effects of their exposure are more likely to demonstrate behavioral effects as well. For this reason, early identification is critical in order to implement appropriate interventions to facilitate positive outcomes and prevent secondary disabilities in this vulnerable population.
Acknowledgements
This work was supported by the National Institute Alcohol Abuse and Alcoholism (R01 AA014373) and was supported, in part, by the Biomedical Imaging Technology Center of Emory University. We also want to thank the families and young adults whose participation has made this research possible and Sharron Paige for her invaluable and untiring contributions.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Slopes were calculated using the formula (mean {TR}=mean {TR}1 to {TR}8; covariate {TR}=−7*( {TR}1 -m{TR)−5*({TR}2- m{TR})−3*({TR}3 -m{TR})−1*({TR}4-m{TR})+1*( {TR }5+3*({TR}6-m{TR}) +5*{TR}7-m{TR}) +7*{TR}8-m{TR}) with Slope=covariate {TR}/168).
References
- Blackston RD, Coles CD, Kable JA, Seitz R. Reliability and validity of the Dysmorphia Checklist: Relating severity of dysmorphia to cognitive and behavioral outcomes in children with prenatal alcohol exposure; Poster presented at the American Society of Human Genetics Annual Meeting; Toronto, Canada. 2004. [Google Scholar]
- Becker HC, Randall CL, Salo AL, Saulnier JL, Weathersby RT. Animal research: Charting the course for FAS. Alcohol Health & Research World. 1994;18:10–16. [PMC free article] [PubMed] [Google Scholar]
- Berman RF, Hannigan JH. Effects of prenatal alcohol exposure on the hippocampus: Spatial behavior, electrophysiology, and neuroanatomy. Hippocampus. 2000;10:94–110. doi: 10.1002/(SICI)1098-1063(2000)10:1<94::AID-HIPO11>3.0.CO;2-T. [DOI] [PubMed] [Google Scholar]
- Bremner JD. Stress and brain atrophy. CNS and Neurological Disorders- Drug Targets. 2006;5(5):503–512. doi: 10.2174/187152706778559309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown J, McKone E, Ward J. Deficits of long-term memory in ecstasy users are related to cognitive complexity of the task. Psychopharmacology. 2010;209:51–67. doi: 10.1007/s00213-009-1766-2. [DOI] [PubMed] [Google Scholar]
- Buschke H, Fuld PA. Evaluating storage, retention and retrieval in disordered memory and learning. Neurology. 1974;24:1019–1025. doi: 10.1212/wnl.24.11.1019. [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention (CDC), National Task Force on Fetal Alcohol Syndrome and Fetal Alcohol Effect Post Exposure Writing Group. Carmichael Olsen H, et al. A call to action: Advancing essential services and research of fetal alcohol spectrum disorders. Centers for Disease Control publication. 2009 [Google Scholar]
- Churchwell JC, Morris AM, Musso ND, Kesner RP. Prefrontal and hippocampal contributions to encoding and retrieval of spatial memory. Neurobiology: Learning and Memory. 2010 doi: 10.1016/j.nlm.2009.12.008. epub ahead of print. [DOI] [PubMed] [Google Scholar]
- Coles CD, Brown RT, Smith IE, Platzman KA, et al. Effects of prenatal alcohol exposure at school age: I. Physical and cognitive development. Neurotoxicology and Teratology. 1991;13(4):357–367. doi: 10.1016/0892-0362(91)90084-a. [DOI] [PubMed] [Google Scholar]
- Coles CD, Fernhoff PM, Lynch ME, Falek A, Dellis E. Manual for scoring the Dysmorphia Checklist: Newborn version. Emory University; 1997. [Google Scholar]
- Coles CD, Lynch ME, Kable JA, Johnson KC, Goldstein FC. Verbal and Nonverbal Memory in Adults Prenatally Exposed to Alcohol. Alcoholism: Clinical and Experimental Research. 2010;34(5):897–906. doi: 10.1111/j.1530-0277.2010.01162.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Coles CD, Platzman KA, Raskind-Hood CL, Brown RT, Falek A, Smith IE. A comparison of children affected by prenatal alcohol exposure and attention deficit, hyperactivity disorder. Alcoholism: Clinical and Experimental Research. 1997;21(1):150–161. [PubMed] [Google Scholar]
- Coles CD, Platzman KA, Smith IE, James ME, Falek A. Effects of cocaine and alcohol use in pregnancy on neonatal growth and neurobehavioral status. Neurotoxicology and Teratology: 1992;14:23–33. doi: 10.1016/0892-0362(92)90025-6. [DOI] [PubMed] [Google Scholar]
- Coles CD, Smith IE, Fernhoff PM, Falek A. Neonatal neurobehavioral characteristics as correlates of maternal alcohol use during gestation. Alcoholism: Clinical & Experimental Research. 1985;9:454–460. doi: 10.1111/j.1530-0277.1985.tb05582.x. [DOI] [PubMed] [Google Scholar]
- Dale AMB, Fischl B, et al. Cortical surface-based analysis. I. Segmentation and surface reconstruction. Neuroimage. 1999;9(2):179–194. doi: 10.1006/nimg.1998.0395. [DOI] [PubMed] [Google Scholar]
- Desikan RS, Segonne F, et al. An automated labeling system for subdividing the human cerebral cortex on MRI scans into gyral based regions of interest. Neuroimage. 2006;31(3):968–980. doi: 10.1016/j.neuroimage.2006.01.021. [DOI] [PubMed] [Google Scholar]
- Driscoll CD, Streissguth AP, Riley EP. Prenatal alcohol exposure: Comparability of effects in humans and animal models. Neurotoxicology and Teratology. 1990;12(3):231–237. doi: 10.1016/0892-0362(90)90094-s. [DOI] [PubMed] [Google Scholar]
- Fletcher J. Memory for verbal and nonverbal stimuli in learning disability subgroups: Analysis by selective reminding. Journal of Experimental Child Psychology. 1985;40(2):244–259. doi: 10.1016/0022-0965(85)90088-8. [DOI] [PubMed] [Google Scholar]
- Fischl B, Salat DH, et al. Whole brain segmentation: automated labeling of neuroanatomical structures in the human brain. Neuron. 2002;33(3):341–355. doi: 10.1016/s0896-6273(02)00569-x. [DOI] [PubMed] [Google Scholar]
- Fischl B, Sereno MI, et al. Cortical surface-based analysis. II: Inflation, flattening, and a surface-based coordinate system. Neuroimage. 1999;9(2):195–207. doi: 10.1006/nimg.1998.0396. [DOI] [PubMed] [Google Scholar]
- Fischl B, van der Kouwe A, et al. Automatically parcellating the human cerebral cortex. Cerebral Cortex. 2004;14(1):11–22. doi: 10.1093/cercor/bhg087. [DOI] [PubMed] [Google Scholar]
- Giedd JN, Vaitzus C, Hamberger SD, Lange N, Rajapakse JC, Kaysen D, et al. Quantitative MRI of the temporal lobe, amygdala, and hippocampus in normal human development: Ages 4–18 years. Journal of Comparative Neurology. 1996;366:223–230. doi: 10.1002/(SICI)1096-9861(19960304)366:2<223::AID-CNE3>3.0.CO;2-7. [DOI] [PubMed] [Google Scholar]
- Hoyme HE, May PA, Kalberg WO, Kodituwakku P, Gossage JP, Trujillo PM, Buckley DG, Miller JH, Aragon AS, Khaole N, Viljoen DL, Jones KL, Robinson LK. A practical clinical approach to diagnosis of fetal alcohol spectrum disorders: Clarification of the 1996 Institute of Medicine Criteria. Pediatrics. 2005:117. doi: 10.1542/peds.2004-0259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jacobson JL, Jacobson SW. Effects of prenatal alcohol exposure on child development. Alcohol Research & Health. 2002;26(4):282–286. [PMC free article] [PubMed] [Google Scholar]
- Jones KL, Robinson LK, Bakhireva LN, Marintcheva G, Storojev V, Strhova A, Sergeevskaya S, Budantseva B, Mattson SN, Riley EP, Chambers CD. Accuracy of the diagnosis of physical features of fetal alcohol syndrome by pediatricians after specialized training. Pediatrics. 2006;118:1734–1738. doi: 10.1542/peds.2006-1037. [DOI] [PubMed] [Google Scholar]
- Kable JA, Coles CD, Brown RT, editors. Handbook of Pediatric Psychology in School Settings. Mahwah, NJ: Lawrence Erlbaum Associates Publishers; 2004. Teratology of alcohol: Implications for school settings. [Google Scholar]
- Kaemingk KL, Halverson PT. Spatial memory following prenatal alcohol exposure: More than a material specific memory deficit. Child Neuropsychology. 2000;6(2):115–128. doi: 10.1076/chin.6.2.115.7058. [DOI] [PubMed] [Google Scholar]
- Kerns K, Don A, Mateer CA, Streissguth AP. Cognitive deficits in nonretarded adults with fetal alcohol syndrome. Journal of Learning Disabilities. 1997;30(6):685–693. doi: 10.1177/002221949703000612. [DOI] [PubMed] [Google Scholar]
- Klintsova Helfer, Calizo Dong, Goodlett Greenough. Persistent impairment of hippocampal neurogenesis in young adult rats following early postnatal alcohol exposure. Alcoholism: Clinical and Experimental Research. 2007;31(12):2073–2082. doi: 10.1111/j.1530-0277.2007.00528.x. [DOI] [PubMed] [Google Scholar]
- Kramer JH, Rosen HJ, Du A-T, Schuff N, Hollnagel C, Weiner MW, Miller BL, Delis DC. Dissociations in hippocampal and frontal contributions to episodic memory performance. Neuropsychology. 2005;19:799–805. doi: 10.1037/0894-4105.19.6.799. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Livy DJ, Miller EK, Maier SE, West JR. Fetal alcohol exposure and temporal vulnerability: Effects of binge-like alcohol exposure on the developing rat hippocampus. Neurotoxicology and Teratology. 2003;25(4):447–458. doi: 10.1016/s0892-0362(03)00030-8. [DOI] [PubMed] [Google Scholar]
- McLellan AT, Kushner H, Metzger D, Peters R, Smith I, Grissom G, Pettinati H, Argeriou M. The fifth edition of the Addiction Severity Index. Journal of Substance Abuse Treatment. 1992;9(3):199–213. doi: 10.1016/0740-5472(92)90062-s. [DOI] [PubMed] [Google Scholar]
- Malisza KL, Allman A-A, Shiloff D, Jakobson L, Longstaffe S, Chudley AE. Evaluation of spatial working memory function in children and adults with fetal alcohol spectrum disorders: A functional magnetic resonance imaging study. Pediatric Research. 2005;58(6):1150–1157. doi: 10.1203/01.pdr.0000185479.92484.a1. [DOI] [PubMed] [Google Scholar]
- Mattson SN, Riley EP. A review of the neurobehavioral deficits in children with fetal alcohol syndrome or prenatal exposure to alcohol. Alcoholism: Clinical and Experimental Research. 1998;22(2):279–294. doi: 10.1111/j.1530-0277.1998.tb03651.x. [DOI] [PubMed] [Google Scholar]
- Mattson SN, Riley EP, Delis DC, Stern C, Jones KL. Verbal learning and memory in children with fetal alcohol syndrome. Alcoholism: Clinical & Experimental Research. 1996;20(5):810–816. doi: 10.1111/j.1530-0277.1996.tb05256.x. [DOI] [PubMed] [Google Scholar]
- Mattson SN, Riley EP, Gramling L, Delis DC, Jones KL. Neuropsychological comparison of alcohol-exposed children with or without physical features of fetal alcohol syndrome. Neuropsychology. 1998;12(1):146–153. doi: 10.1037//0894-4105.12.1.146. [DOI] [PubMed] [Google Scholar]
- Mattson SN, Roebuck TM. Acquisition and retention of verbal and nonverbal information in children with heavy prenatal alcohol exposure. Alcoholism: Clinical and Experimental Research. 2002;26(6):875–882. [PubMed] [Google Scholar]
- O’Hare ED, LU LH, Houston SM, Bookheimer SY, Mattson SN, O’Connor MJ, Sowell ER. Altered frontal-parietal functioning during verbal working memory in children and adolescents with heavy prenatal alcohol exposure. Human Brain Mapping, …. 2009 doi: 10.1002/hbm.20741. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pei JR, Rinaldi CM, Rasmussen C, Massey V, Massey D. Memory patterns of acquisition and retention of verbal and nonverbal information in children with fetal alcohol spectrum disorders. Canadian Journal of Clinical Pharmacology/Journal Canadien de Pharmacologie Clinique. 2008;15(1):e44–e56. [PubMed] [Google Scholar]
- Preacher KJ, Hayes AF. Asymptotic and resampling strategies for assessing and comparing indirect effects in multiple mediator models. Behavior Research Methods. 2008a;40(3):879–891. doi: 10.3758/brm.40.3.879. [DOI] [PubMed] [Google Scholar]
- Preacher KJ, Hayes AF. The Ohio State University; 2002b. SPSS Macro for multiple mediation. Written by Andrew F. Hayes. http://www.comm.ohio-state.edu/ahayes. [Google Scholar]; Richardson GA, Ryan C, Willford J, Day NL, Goldschmidt L. Prenatal alcohol and marijuana exposure: Effects on neuropsychological. 2002 doi: 10.1016/s0892-0362(02)00193-9. [DOI] [PubMed] [Google Scholar]
- Roebuck-Spencer TM, Mattson SN. Implicit strategy affects learning in children with heavy prenatal alcohol exposure. Alcoholism: Clinical and Experimental Research. 2004;28(9):1424–1431. doi: 10.1097/01.alc.0000139826.25247.5b. [DOI] [PubMed] [Google Scholar]
- Schottenbauer MA, Hommer D, Weingartner H. Memory deficits among alcoholics: performance on a selective reminding task. Aging, Neuropsychology, and Cognition. 2007;14(5):505–516. doi: 10.1080/13825580600681305. [DOI] [PubMed] [Google Scholar]
- Smith CN, Squire LR. Medial temporal lobe activity during retrieval of semantic memory is related to the age of the memory. Journal of Neuroscience. 2009;28(29(4)):930–938. doi: 10.1523/JNEUROSCI.4545-08.2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sowell ER, Lu LH, O’Hare ED, McCourt ST, Mattson SM, O’Connor MJ, Bookheimer SY. Functional magnetic resonance imaging of verbal learning in children with heavy prenatal alcohol exposure. NeuroReport. 2007;18(7):635–639. doi: 10.1097/WNR.0b013e3280bad8dc. [DOI] [PubMed] [Google Scholar]
- Sowell ER, Mattson SN, Kan E, Thompson PM, Riley EP, Toga AW. Abnormal cortical thickness and brain-behavior correlation patterns in individuals with heavy prenatal alcohol exposure. Cerebral Cortex. 2008;18:136–144. doi: 10.1093/cercor/bhm039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Squire LR. Memory systems: Les systemes mnesiques. Academie des sciences. 1998;321:153–156. doi: 10.1016/s0764-4469(97)89814-9. [DOI] [PubMed] [Google Scholar]
- Stratton K, Howe C, Battaglia F, editors. Fetal Alcohol Syndrome: Diagnosis, Epidemiology, Prevention, and Treatment. Washington, DC: National Academy Press; 1996. pp. 154–193. [Google Scholar]
- Streissguth AP, Barr HM, Kogan J, Bookstein FL. Final Report to the Centers for Disease Control and Prevention (CDC) Seattle: University of Washington, Fetal Alcohol and Drug Unit; 1996. Understanding the Occurrence of Secondary Disabilities in Clients with Fetal Alcohol Syndrome (FAS) and Fetal Alcohol Effects (FAE) Tech. Rept. No. 96-06. [Google Scholar]
- Streissguth AP, Bookstein FL, Sampson PD, Barr HM. Neurobehavioral effects of prenatal alcohol: III. PLS analyses of neuropsychologic tests. Neurotoxicology and Teratology. 1989;11(5):493–507. doi: 10.1016/0892-0362(89)90026-3. [DOI] [PubMed] [Google Scholar]
- Uecker A, Nadel L. Spatial but not object memory impairments in children with fetal alcohol syndrome. American Journal on Mental Retardation. 1998;103(1):12–18. doi: 10.1352/0895-8017(1998)103<0012:SBNOMI>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- Van Petten C. Relationship between hippocampal volume and memory ability in healthy individuals across the lifespan: Review and meta-analysis. Neuropsychologia. 2004;42:1394–1413. doi: 10.1016/j.neuropsychologia.2004.04.006. [DOI] [PubMed] [Google Scholar]
- Wechsler D. Wechsler Intelligence Scale for Children (WISC-III) San Antonio, TX: The Psychology Corporation; 1991. [Google Scholar]
- Wechsler D. Wechsler Abbreviated. San Antonio, TX: The Psychological Corporation; 1999. Wechsler Abbreviated Scale of Intelligence (WASI) [Google Scholar]
- Wheeler MA, Stuss DT, Tulving E. Frontal lobe damage produces episodic memory impairments. Journal of the International Neuropsychological Society. 1995;1:525–536. doi: 10.1017/s1355617700000655. [DOI] [PubMed] [Google Scholar]
- Willford JA, Richardson GA, Leech SL, Day NL. Verbal and visuospatial learning and memory function in children with moderate prenatal alcohol exposure. Alcoholism: Clinical and Experimental Research. 2004;28(3):497–507. doi: 10.1097/01.alc.0000117868.97486.2d. [DOI] [PubMed] [Google Scholar]
- Willoughby KA, Sheard ED, Nash K, Rovet J. Effects of prenatal alcohol exposure on hippocampal volume, verbal learning, and verbal and spatial recall in late childhood. Journal of the International Neuropsychological Society. 2008;14:1022–1033. doi: 10.1017/S1355617708081368. [DOI] [PubMed] [Google Scholar]
- Yurgelun-Todd D, Killgore WD, Cintron CB. Cognitive correlates of medial temporal lobe development across adolescence: A magnetic resonance imaging study. Perceptual and Motor Skills. 2003;96:3–17. doi: 10.2466/pms.2003.96.1.3. [DOI] [PubMed] [Google Scholar]