Abstract
Objective
To examine the underreporting of sexually transmitted infections (STI) (i.e., no STI by self-report but have at least one STI through biological testing or clinical examination) and factors associated with underreporting among female sex workers (FSWs) in China.
Methods
A total of 454 FSWs were recruited from entertainment establishments in a rural county of Guangxi, China. Participants completed a self-administered survey about their demographic and working characteristics, history of STI (past or current infections), sexual history and practices, and HIV/STI-related knowledge and perceptions; 411 of the sample were also tested for syphilis, Neisseria gonorrheae, Chlamydia, Trichomonas, and genital warts.
Results
About 18% (79 of 411) of the sample reported a history of STI (past or current infections). Biological testing or clinical examination revealed at least one STI (acute STI) for 42% (171 of 411) of the sample. Only 9% (37 of 411) of FSWs with acute STI reported an STI through self-report, which resulted in 33% (134 of 411) of FSWs who were considered underreporting their STI. STI underreporting was independently associated with younger age (adjusted odds ratio [aOR] 0.87, 95% confidence interval [CI] 0.76-0.99), a shorter duration of commercial sex (aOR 0.97, 95% CI 0.94-0.99), poorer knowledge of STI (aOR 0.81, 95% CI 0.70-0.94), and less sexual risks (aOR 0.52, 95% CI 0.41-0.66).
Conclusions
Underreporting of STI was prevalent in FSWs, especially among women with perceived lower STI risks. The underreporting might be largely due to their perception of low risks for STI and unawareness of STI symptoms (including asymptomatic STIs). Future studies of FSWs should identify those new in commercial sex with lower STI awareness and perceived risks and encourage them to seek timely and appropriate testing and treatment.
Introduction
In sexual risk-reduction research, reliance on self-reported outcome measures has been a matter of continuing controversy.1,2 Self-reported sexually transmitted infection (STI) has been used as a proxy indicator for sexual risk behaviors.3–6 However, self-reported STI has questionable accuracy, and underreporting is commonly seen, particularly in high-risk populations.7 The underreporting of STI may result from a number of factors: patients were not tested and were unaware of any symptoms or diagnosis, especially asymptomatic STI; patients were tested but unaware of the diagnosis because the results were not received or not understood; and patients were tested and aware of the diagnosis but did not report it.8 Despite the questionable accuracy of self-reported STI, it is still widely used in behavioral research of sexual risk reduction, mostly because data collection by self-report can be easily incorporated into existing survey instruments at low financial and personnel cost. Few studies have explored the issues of STI underreporting,7–11 and fewer of these existing studies explored factors associated with underreporting. In addition, most of the existing studies were conducted in the Western countries, and there is a lack of studies on STI underreporting in developing countries, particularly in areas where the STI epidemic is growing rapidly, such as China.
China has observed a substantial growth in the STI epidemic.12 STI has become the third most common infectious disease in China.13 According to the National STD Surveillance System, close to 1 million new STI cases have been reported annually in recent years, and there was an average annual increase of 39% from 1985 to 2004.14 It is acknowledged, however, that reported STIs make up only a small portion of the real number, accounting for only 10% of the actual number of infection cases.13 A number of emerging social factors may be facilitating the rapid (and continued) increase in STI.15 One of these factors is the widespread commercial sex that has played a major role in China's escalating STI epidemic.
In China, the commercial sex industry has reemerged since economic reform and the opening to the outside world in the early 1980s. According to the China public security agencies, there are an estimated 4 million female sex workers (FSWs) in China,16 although many public health experts believe that the actual number could reach 10 million.17 The National STD Surveillance System indicated that the majority of STIs were acquired through extramarital sex, including commercial sex.12 Existing studies on FSWs have relied largely on self-reported STI. Of limited studies that reported biologically confirmed STI, the prevalence ranged from 30% to 85%.17 FSWs recruited in STI clinics and detention centers (i.e., women's reeducation centers) reported extremely high rates of STI (as high as 85%).13,18,19 The high STI prevalence in FSWs has drawn increasing attention; FSWs and their clients are considered the most critical populations in the spread of STI and HIV in China.20 Nevertheless, given the large number of FSWs and the limited capacity of the current surveillance system in China, self-report of STI will continue to be used widely in studies among FSWs, especially in behavioral research of sexual risk and STI/HIV prevention. Therefore, there is a need to assess the accuracy of self-reported STI and the factors that contribute to underreporting.
In this study, by comparing self-reported history of STI (including both past and current STI) with biologically confirmed STI, we examine the occurrence of underreporting of STI; assess the relationship between underreporting of STI and FSWs' sexual history, sexual practices, and HIV/STI knowledge and awareness; and identify subgroups of FSWs who are more likely to underreport STI.
Materials and Methods
Study site
The data in the current study were drawn from the baseline assessment of a longitudinal STI/HIV intervention project, which was conducted in 2004–2005 in a rural county (H County) of the Guangxi Zhuang Autonomous Region.21 Guangxi, one of China's five autonomous and multiethnic regions, is located in the southern part of the country. It is bordered by Guangdong Province on the east, the Gulf of Tonkin on the south, and Vietnam on the southwest. Because of its central location in southwest China, Guangxi has historically been a transport hub for trade, commerce, and tourism in southwest China and South East Asia. Guangxi is along a drug trafficking route that originates from the Golden Triangle of Thailand, Myanmar, and Laos, passes through northern provinces of Vietnam and Guangxi, and finally enters Hong Kong and the rest of the world. Guangxi ranks second among China's 31 provinces in terms of reported HIV-seropositive cases.22 The prosperous economy, international contact, and tourism in Guangxi have created a demand and market for commercial sex. According to statistics from the local public security agency, there are at least 50,000 FSWs in Guangxi, although the actual number is believed to be substantially higher.22
H County, about 90 kilometers northeast from Nanning, the capital city of Guangxi, is the most populous county in the Nanning suburban area. H County has jurisdiction over 22 townships with a total population of 1.1 million (94.5% are rural residents). There were an estimated 200 entertainment establishments with more than 2000 women providing commercial sexual service in the county at the time of the study.
Participants
Participants in this study were recruited from restaurants, barbershops, and hair-washing rooms in H County. Because H County is a rural county, the majority of entertainment establishments that provide sex services are restaurants or barbershops (including hair-washing rooms). The research team and local health workers identified these entertainment establishments in H County through ethnographic targeted sampling strategies. The owners/managers of these establishments were contacted for permission to conduct research on their premises. Trained outreach health workers from the County Anti-Epidemic Station and local hospitals approached women in the establishments to ask for their participation. All participants were self-identified as sex workers. Among 582 women contacted, 454 (78%) agreed to participate in this study, provided written informed consent, and completed a self-administered questionnaire. Of 454 participants, 411 (91%) provided biological specimens for STI testing, and these women constituted the final sample of the current study.
Survey procedure
The survey procedure has been described in detail elsewhere.21 Briefly, the survey was conducted in separate rooms or private spaces in the establishments where participants were recruited. No one was allowed to stay with the participant during the survey except the interviewer who provided the participant with necessary assistance. For participants with limited literacy (approximately 10%), the interviewer read each question and response options from her copy of the questionnaire while the participant marked the response on her own copy (so that the interviewer would not see the participant's answers). The questionnaire took about 1 hour to complete. The study protocol was approved by the Institutional Review Boards at Wayne State University in the United States and Beijing Normal University and Guangxi CDC in China.
STI testing
Following the survey, participants received a gynecological examination that took about 15 minutes. Collection of blood specimen, cervical swabs, and screening of symptomatic STI (e.g., genital warts) were performed during the gynecological examination. STI screening and testing were conducted by trained STI clinicians and laboratory technicians for five common STI (Neisseria gonorrhoeae, Chlamydia trachomatis, trichomoniasis, syphilis, and genital warts). Blood specimens were drawn and assessed for syphilis using the Rapid Plasma Reagin (Xinjiang Xinde Co., China). Positive results were confirmed using the Serodia Treponema palladum Particle Agglutination procedure (Fujirebio, Inc., Japan). Cervical swab specimens were obtained from women to detect N. gonorrhoeae, C. trachomatis, and Trichomonas vaginalis. N. gonorrhoeae was identified using the standard culture procedure. Chlamydia infection was detected by rapid antigen test (Clearview, Unipath, U.K.). Trichomoniasis was diagnosed by detecting the motile parasite under a microscope. Genital warts were diagnosed by clinical examination performed by the STI clinician. All STI assays were conducted at the County Anti-Epidemic Station STD Laboratory. Investigators from the China CDC National Resource Centre for STI Control provided training, supervision, and quality control for all STI testing and diagnosis.
All participating FSWs who received free STI testing received individual pretesting and posttesting counseling.21 The results of STI testing were delivered by STI clinicians in private during the posttesting session. For those who tested positive for any STI, STI clinicians explained the test results and provided medical treatment during the posttest session. For those who had STI symptoms or a positive result but did not attend the second session, individual follow-up was conducted by the local research team and STI clinician to ensure appropriate counseling, referral, and treatment.
Measures
Demographic characteristics collected in this study included age, ethnicity (Han, Zhuang, or other ethnicities), years of formal schooling, marital status, length of being an FSW, workplace (restaurant or hair salon), number of FSWs at work, living arrangement (e.g., living with other FSWs), and monthly income (in Chinese currency, Yuan).
Social desirability might affect the response on self-report behaviors and medical history.23 We used the 5-item Marlowe-Crowne Social Desirability Scale,24 which has been validated in the Chinese population.25 The sample items include: I never took advantage from anyone; I am always happy to help others; and I have never said a bad word about anyone behind them. All items had a dichotomous response option (yes/no). A composite score (range 0–5) was created by summing up the positive responses to the 5 items, with a higher score indicating a higher level of social desirability. The Cronbach alpha for the scale was 0.46 for the current study sample.
Sexual history and sexual practices included the participant's age of sexual debut, number of clients per week, maximum number of clients per day, number of stable sexual partners (i.e., husband, boyfriend, or long-term client), number of pregnancies, and ever having had an abortion. Sexual risks were measured by asking FSWs the following 9 questions: if they had sex with clients with STI; if they ever used illicit drugs; if they had sex with clients during menses; if they had sex under the influence of alcohol; if they experienced sexual violence in the past 6 months; if they used condoms consistently with clients (i.e., always used a condom during sexual encounters with clients); if they used condoms consistently with stable partners; if they used condoms properly with clients (i.e., always put condom on before penetration); if they used condoms properly with stable partners. A composite sexual risk score (range 0–12) was created by summing up the dichotomous responses to these 12 items (with appropriate reverse coding or rescaling), with a higher score indicating a higher level of sexual risks.
HIV/STI-related knowledge and perceptions
HIV/AIDS knowledge items were adapted from the scales used in the 1992 U.S. National Health Interview Survey.26 Six items were employed to assess participants' knowledge of HIV transmission modes. All the items had likely/unlikely response choices. The internal consistency (Cronbach alpha) for the scale was 0.90. The sum of the correct answers (i.e., likely) to the six questions was retained as a composite score (range 0–6), with higher scores reflecting better knowledge about HIV transmission.
Knowledge of STI symptoms was assessed by asking participants to judge a possible STI symptom (yes, no, don't know) from a list of 10 symptoms. The Cronbach alpha for the 10 items was 0.88. A composite score was created by adding the correct responses to the 10 items, with a higher score reflecting a higher level of STI knowledge.
Knowledge of correct condom use was measured by asking participants to sort six preprinted pictorial cards describing major steps of condom use. Those participants who arranged the six cards in the correct order were considered as knowing how to use condoms correctly.
Participants' general awareness of HIV/STI was assessed by two separate questions on how much they know about STI and HIV (nothing, a little, some, a lot, almost everything). For the purpose of data analysis in the current study, responses were dichotomized into nothing/a little vs. some/a lot/everything.
Participants' vulnerability to STI was assessed by asking their perceived likelihood of acquiring STI in the future on a 5-point scale (1 = unlikely, 2 = somewhat likely, 3 = likely, 4 = very likely, and 5 = having already been infected). For the purpose of data analysis, the last four categories were combined to form one category (i.e., likely).
Perceived barriers to condom use were measured by asking participants the barriers or negative consequences of condom use. The items included: If the police found you carrying a condom, you might be in trouble. Few men like to use condoms. If you insisted on using a condom, your partner might be suspicious that you had an STI. If you insisted on using a condom, your clients might get angry at you. If you insisted on using a condom, clients might not come to you any more. If you insisted on using a condom, you might make less money. The participants were asked to indicate if they agreed or disagreed with the statements. The Cronbach alpha for the six items was 0.56. A composite score was created by summing the agree responses.
Self-efficacy of condom use assessed one's belief in her own ability to obtain and to use a condom (e.g., I will refuse to have sex if my partner does not want to use a condom). The two-item scale had a Cronbach alpha of 0.58. A sum score was obtained as a composite score, with higher scores indicating higher levels of self-efficacy.
Perceived peer risk involvement was assessed by asking participants to estimate how many (1 = none, 2 = few, 3 = some, and 4 = most) of their peers had engaged in a number of HIV/STI risk behaviors, such as having multiple sexual partners and having STI. The internal consistency (Cronbach alpha) of the four items was 0.82. A composite score was created by averaging the responses, with a higher score indicating a higher level of perceived peer sexual risk involvement.
Measures of STI
Self-report history of STI was measured by asking a participant if she ever had an STI or if she was currently infected with an STI. Biologically confirmed STI was measured by testing for five common STIs, including Chlamydia, N. gonorrhoeae, syphilis, Trichomonas, and genital warts. Underreporting of STI referred to the situation in which a participant did not self-report an STI but tested positive for at least one STI.
Data analysis
First, we compared the number and percentage of people who self-reported having a history of STI and who tested positive for a STI. We calculated the percentage of FSWs who provided consistent reports and inconsistent reports and graphically depicted the proportions. We also calculated the proportion of five biologically confirmed STIs among all the infected participants and among those who underreported STI. Second, participants' demographic and work-related information and social desirability were compared between their self-reported STI status and biologically confirmed STI status. Chi-square (for categorical variables) or analysis of variance (ANOVA) (for continuous variables) was employed to assess the associations of STI underreporting with participant characteristics. Third, Kruskal-Wallis test and chi-square tests were employed to assess the relationship between underreporting of STI and sexual history and practice as well as STI/HIV-related knowledge and perceptions.
Finally, multivariate logistic regression analysis was employed to assess the relative importance and independent contribution of various factors that were associated with STI underreporting. All variables that were significantly associated with underreporting (p < 0.05) in binary analyses were selected as the independent variables in the multivariate logistic regression model. Key demographic factors (age, social desirability, schooling, and marital status) were forcedly entered into the model to control for potential confounding effect. Sexual history, sexual practice, and HIV-related knowledge and perceptions were entered into the model in a stepwise manner. Adjusted odds ratio (aOR) and 95% confidence intervals (95% CI) were used to assess the association between independent variables and STI underreporting.
Results
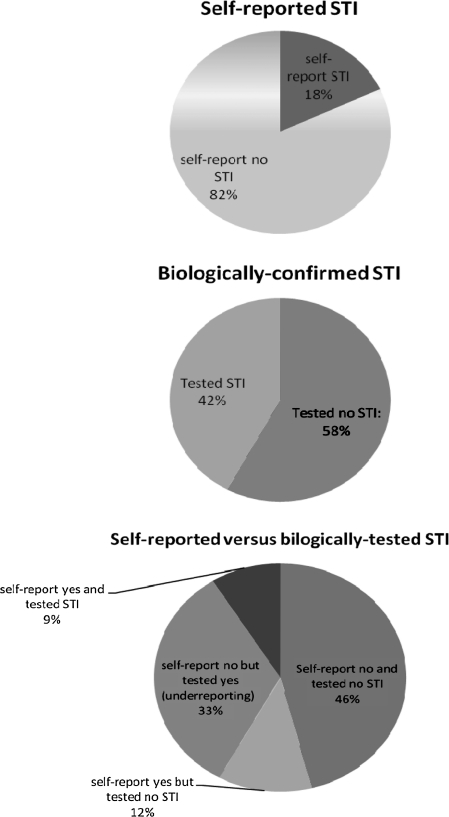
Self-reported STI and biologically confirmed STI
Of 411 participants, 42% tested positive for at least one STI. However, only 9% of these women reported having a history of STI (either past or current). Therefore, about 33% of women were considered to be underreporting their STI status (Fig. 1). About 12% of women reported a history of STI but showed negative results on the test for five STIs. As shown in Table 1, of 171 participants with biologically confirmed STI (or acute STI), 20% had syphilis, 38% had gonorrhea neisseria, 44% had Chlamydia infection, 17% had trichomoniasis, and 4% had genital warts. Of 134 underreported cases, 22% had syphilis, 39% had gonorrhea, 41% had Chlamydia infection, 18% had trichomoniasis, and 3% had genital warts.
FIG. 1.
Self-report vs. biologically confirmed sexually transmitted infection (STI).
Table 1.
Biologically Confirmed Sexually Transmitted Infection Among Female Sex Workers by Status of Underreporting (n = 411)
| Total | Underreporting | |
|---|---|---|
| n (%) | 171 (100) | 134 (33) |
| Syphilis | 34 (20) | 29 (22) |
| Neisseria gonorrhoeae | 65 (38) | 52 (39) |
| Chlamydia trachomatis | 75 (44) | 55 (41) |
| Trichomonas vaginalis | 29 (17) | 24 (18) |
| Genital warts | 7 (4) | 4 (3) |
Demographic characteristics and work-related information
The participants were young, with a mean age of 23.5 years, and they received an average of 5.7 years of formal schooling. About four fifths of the women worked in restaurants, and the rest worked in hair salons. A majority of these women (60%) were never married, and most of them (76%) lived with other FSWs. The average length of working as an FSW was 12.6 months, with a range of 6 days–66 months. On average, they made 570 yuan (approximately US$82 at the time of the survey) a month, with a range of 50–4000 yuan. The mean social desirability score was 3.41 (on a scale of 0–5).
As shown in Table 2, women who had less education, worked in larger commercial sex venues, had worked in commercial sex longer, had a higher monthly income, and had a lower level of social desirability were more likely to self-report STI. Women who were younger, never married, and had a lower level of social desirability were more likely to have biologically confirmed STI. STI underreporting was significantly associated with being of the Zhuang ethnic minority, being less educated, living with other FSWs, working in smaller commercial sex venues, having worked in commercial sex for a shorter period of time, having a lower income, and having a higher level of social desirability (Table 2).
Table 2.
Demographic Characteristics and Work Information of Participants by Self-Reported Sexually Transmitted Infection and Biologically Confirmed Sexually Transmitted Infection
| |
|
Self-reported STI |
Clinic-tested STI |
|
||
|---|---|---|---|---|---|---|
| Total | Yes | No | Yes | No | Underreporting | |
| n (%) | 411 (100) | 79 (18) | 332 (82) | 171 (42) | 240 (58) | 134 (33) |
| Age, mean (SD) | 23.50 (5.09) | 23.96 (4.75) | 23.39 (5.21) | 22.82 (4.57) | 23.99 (5.44)* | 22.80 (4.66) |
| Ethnicity | ||||||
| Han | 57% | 68% | 54%* | 55% | 58% | 49%* |
| Zhuang | 31% | 24% | 33% | 36% | 28% | 41% |
| Others | 12% | 8% | 14% | 10% | 14% | 10% |
| Years of school, mean (SD) | 5.74 (3.24) | 6.46 (2.93) | 5.57 (3.30)* | 5.47 (3.17) | 5.94 (3.29) | 5.36 (3.15)* |
| Marital status | ||||||
| Never married | 60% | 62% | 60% | 68% | 55%* | 66% |
| Married | 40% | 18% | 40% | 32% | 45% | 34% |
| Living with other FSW | 76% | 65% | 79%** | 78% | 75% | 81%** |
| Workplace | ||||||
| Restaurant | 83% | 80% | 83% | 84% | 82% | 85% |
| Hair salon | 17% | 20% | 17% | 16% | 18% | 15% |
| N. of FSWs at work, mean (SD) | 16.46 (9.93) | 18.97 (11.00) | 15.85 (9.58)* | 15.48 (9.32) | 17.16 (10.31) | 14.97 (9.14)** |
| Length being FSW, months, mean (SD) | 12.60 (12.48) | 18.59 (13.96) | 11.16 (11.67)**** | 11.24 (12.16) | 13.58 (12.64) | 9.65 (11.21)**** |
| Monthly income in RMB, mean (SD) | 570 (504) | 766 (710) | 524 (431)**** | 564 (507) | 574 (504) | 492 (380)**** |
| Social desirability, mean (SD) | 3.41 (1.26) | 3.05 (1.26) | 3.50 (1.24)** | 2.23 (1.27) | 3.54 (1.24)* | 3.37 (1.27) |
p < 0.05; **p < 0.01; ***p < 0.001; ****p < 0.0001.
FSW, female sex worker; SD, standard deviation; STI, sexually transmitted infection; RMB, renminbi, or Chinese yuan.
Sexual history and sexual practices
The participating FSWs initiated sex at a mean age of 18 years and had an average of 2.14 clients per week, with a maximum of 1.28 clients per day. They had an average of 1.3 stable partners and 2.23 pregnancies. About 55% of them had had an abortion, and the mean score of sexual risk was 4.13 (out of 12 items). STI underreporting was significantly associated with all these variables except age of sexual debut (Table 3). Specifically, women who underreported STI had fewer clients each week, had a lower number of daily maximum of clients, had more stable partners, had less pregnancies and abortion, and had a lower level of sexual risk.
Table 3.
Relationship of Sexually Transmitted Infection Underreporting and Sexual History and Practices
| |
|
STI underreporting |
|
|---|---|---|---|
| Total | No | Yes | |
| Age of sex debut (SD) | 18.28 (1.95) | 18.33 (2.03) | 18.25 (1.90) |
| No. of clients/week (SD) | 2.14 (1.91) | 2.61 (2.08) | 1.83 (1.72)** |
| Maximum number of clients/day (SD) | 1.28 (0.67) | 1.42 (0.84) | 1.18 (0.51)** |
| Having stable partner | 1.30 (0.46) | 1.20 (0.41) | 1.36 (0.48)* |
| No. of pregnancies | 2.23 (1.21) | 2.72 (1.33) | 1.90 (1.00)**** |
| Had abortion | 118 (55%) | 61 (71%) | 57 (45%)**** |
| Sexual risk score (12 items) | 4.13 (2.10) | 5.34 (1.99) | 3.33 (1.75)**** |
p < 0.05; **p < 0.01; ****p < 0.0001.
STI/HIV-related knowledge and perception
Table 4 shows the mean scores of the measures of STI/HIV-related knowledge and perceptions. STI underreporting was significantly associated with lower level of HIV/AIDS knowledge, lower level of knowledge of STI symptoms, knowing nothing/little about STI, perceived lower vulnerability of STI infection, and lower level of perceived peer sexual risk involvement.
Table 4.
Relationship of Sexually Transmitted Infection Underreporting and Female Sex Workers' HIV/Sexually Transmitted Infection Knowledge and Attitudes
| |
|
STI underreporting |
|
|---|---|---|---|
| Total | No | Yes | |
| HIV knowledge | 4.39 (2.11) | 4.87 (1.90) | 4.04 (2.19)** |
| Knowledge of STI symptoms | 3.35 (2.84) | 4.67 (2.67) | 2.49 (2.61)**** |
| Knowledge of correct condom use | 4.80 (1.58) | 4.99 (1.48) | 4.66 (1.64) |
| Knowing nothing/little about STI | 124 (56%) | 37 (42%) | 87 (65%)**** |
| Knowing nothing/little about HIV | 159 (72%) | 58 (67%) | 101 (75%) |
| Perceived STI vulnerability | 51 (23%) | 34 (39%) | 17 (13%)**** |
| Perceived barriers to condom use | 2.65 (1.57) | 2.58 (1.61) | 2.69 (1.55) |
| Self-efficacy of condom use | 3.16 (1.47) | 3.36 (1.38) | 3.02 (1.51) |
| Peer risk involvement | 2.23 (1.68) | 2.98 (1.70) | 1.74 (1.47)**** |
p < 0.01; ****p < 0.0001.
Multivariate model
The results of the final multivariate logistic regression model are presented in Table 5. Among the demographic factors, age was a significant predictor, with younger women more likely to underreport their STI status (aOR 0.87, 95% CI 0.76-0.99). After controlling for demographic factors, STI underreporting was independently associated with a shorter duration of commercial sex engagement (aOR 0.97, 95% CI 0.94-0.99), poorer knowledge of STI symptoms (aOR 0.81, 95% CI 0.70-0.94), perceived lower risks of STI (aOR 0.63, 95% CI 0.40-0.99), and a lower level of self-reported sexual risks (aOR 0.52, 95% CI 0.41-0.66).
Table 5.
Multivariate Logistic Regression Model
| |
Dependent variables: underreporting of STI |
||
|---|---|---|---|
| Independent variables | aOR (95%CI) | Wald | p |
| Age | 0.87 (0.76-0.99) | 4.41 | 0.036 |
| Social desirability | 1.30 (0.94-1.78) | 2.57 | 0.109 |
| Years of schooling | 1.05 (0.92-1.20) | 0.50 | 0.481 |
| Years being FSW | 0.97 (0.94-0.99) | 4.61 | 0.032 |
| Sexual risk | 0.52 (0.41-0.66) | 29.60 | 0.000 |
| Knowledge of STI symptoms | 0.81 (0.70-0.94) | 7.57 | 0.006 |
| Perceived STI vulnerability | 0. 63 (0.40-0.99) | 3.90 | 0.048 |
aOR, adjusted odds ratio; CI, confidence interval.
Discussion
Our data reveal that in a sample of FSWs recruited from commercial sex venues in a rural county of Guangxi, 42% of the FSWs tested positive for STI, with 33% of them underreporting STI. The STI rate in our sample was similar to that in previous studies of FSWs in China.13,18 Because there was no prior study that compared self-reported and biologically tested STI in FSWs in China, it is difficult to judge the extent of underreporting. However, a study conducted in drug-using FSWs in Amsterdam reported 34% underreporting of STI,11 and a study with sexually active adolescents recruited from clinics in the United States found underreporting of STI to be 21%–47%.7 Our study confirms the inaccuracy of self-reported STI, particularly in the high-risk group of FSWs in China. Behavioral studies on FSWs have largely relied on self-reported STI. For instance, in our recent systematic review of the existing literature on FSWs, of 18 quantitative studies published in English journals, only 8 reported biologically tested STI. The other 10 studies either provided self-report data or did not report STI.17 The high rate of underreporting of STI in the current study underscores the importance of STI testing in future studies of FSWs. As voluntary counseling and testing (VCT) are gradually scaled up in many areas of China,27 having culturally appropriate programs to promote STI testing in high-risk groups, such as FSWs, is urgently needed.
Our findings suggested that underreporting was not significantly associated with social desirability. The underreporting in the current study might be largely due to low perceived STI risk or low awareness of STI symptoms in this group. Our data showed that FSWs who were newer to the commercial sex industry, had lower level of knowledge of STI symptoms, had a perceived lower risk of STI, and had lower level of sexual risks were more likely to underreport STI. These findings suggest that FSWs with the perception of lower risks and engaged in less sexual risks were less likely to be tested for STI and more likely to be unaware of their infectious status. A recent qualitative study of FSWs' access to free VCT services reported that low use of VCT among FSWs was due to misunderstanding about STI/HIV transmission, low perceived risk of infection, and anxiety about the implications of possible test results.28 Another major deterrent to STI testing was the strong stigma associated with commercial sex, as previous studies suggested that self-perceived stigma has led to increased sexual risks, including delayed testing or treatment.29 Therefore, interventions aimed at reducing the STI epidemic in FSWs should not only focus on reducing sexual risks among FSWs and their clients but also increase their awareness and motivation to access STI/HIV testing. Structural interventions at a society level are needed to reduce the stigma against FSWs and create a positive environment for them to seek preventive care and treatment.
There are several limitation in the current study. First, our participants were recruited from entertainment establishments through community outreach; there might be self-selection bias in the sampling. However, demographic characteristics reported by our participants were similar to those observed in previous studies with different sampling methods.13,17,18 Second, data about the history of STI testing were not available in the current study. Therefore, we could not further break down underreporting subjects into those who were tested before and those who were never tested. Third, some of the measures used in the current study did not have good internal consistency estimates (low Cronbach alpha). Further studies are necessary on the development of culturally appropriate measures for such socially marginalized populations as FSWs. Finally, the study was conducted in a multiethnic rural county of Guangxi. Our ability to generalize the findings to other areas or other groups of FSWs in China may be limited.
Despite these limitations, the current study was the first to examine the inaccuracy of self-reported STI and the factors associated with STI underreporting in FSWs in China. The fact that a substantial proportion of these women were infected with at least one STI indicates that most of the women practiced unprotected sex and were at great risk of STI. However, the majority of the FSWs who had STI did not report their infection; underreporting was associated with younger age, poor knowledge of STI symptoms, and perceived lower risk of infection as well as lower perceived sexual risks. These women deserve more attention in STI prevention intervention. As commercial sex plays a critical role in China's escalating HIV and STI epidemics, comprehensive and appropriate prevention programs to increase these women's awareness of their risk of STI and to promote effective STI testing and treatment services for FSWs are urgently needed.
Acknowledgments
This research is supported by grants from the NIMH (R01MH064878) and NIH Office of AIDS Research (R01MH064878-3S1). Dr. Guojun Liang, Dr. Ping Yang, and other investigators from the China CDC National Resource Center for STD Control provided assistance in staff training and quality control for STI testing, counseling, and treatment. Many dedicated individuals from the Guangxi Zhuang Autonomous Region CDC and H County Anti-Epidemic Station assisted in field data collection and intervention implementation.
Disclosure Statement
The authors have no conflicts of interest to report.
References
- 1.Fishbein M. Pequegnat W. Evaluating AIDS prevention interventions using behavioral and biological outcome measures. Sex Transm Dis. 2000;27:101–110. doi: 10.1097/00007435-200002000-00008. [DOI] [PubMed] [Google Scholar]
- 2.Pequegnat W. Fishbein M. Celentano D, et al. NIMH/APPC workgroup on behavioral and biological outcomes in HIV/STD prevention studies: A position statement. Sex Transm Dis. 2000;27:127–132. doi: 10.1097/00007435-200003000-00001. [DOI] [PubMed] [Google Scholar]
- 3.Van Ameijden EJC. van den Hoek JAR. van Haastrecht HJA. Coutinho RA. Trends in sexual behavior and the incidence of sexually transmitted diseases and HIV among drug using prostitutes, Amsterdam 1986–1992. AIDS. 1994;8:213–221. [PubMed] [Google Scholar]
- 4.Fleischer JM. Minkoff HL. Senie RT. Endias RE. Assessing prior history of sexually transmitted diseases. JAMA. 1991;266:1646–1647. [PubMed] [Google Scholar]
- 5.Kleyn J. Schwebke J. Holmes KK. The validity of injecting drug users' self-reports about sexually transmitted diseases: A comparison of survey and serological data. Addiction. 1993;88:673–690. doi: 10.1111/j.1360-0443.1993.tb02080.x. [DOI] [PubMed] [Google Scholar]
- 6.Nelson KE. Vlahov D. Cohn S, et al. Sexually transmitted diseases in a population of injecting drug users: Association with seropositivity to the human immunodeficiency virus (HIV) J Infect Dis. 1991;164:457–463. doi: 10.1093/infdis/164.3.457. [DOI] [PubMed] [Google Scholar]
- 7.Niccolai LM. Kershaw TS. Lewis JB. Cicchetti DV. Ethier KA. Ickovics JR. Data collection for sexually transmitted disease diagnoses: A comparison of self-report, medical record reviews, and state health department reports. Ann Epidemiol. 2005;15:236–242. doi: 10.1016/j.annepidem.2004.07.093. [DOI] [PubMed] [Google Scholar]
- 8.Harrington KF. DiClemente RJ. Wingood GM, et al. Validity of self-reported sexually transmitted diseases among African American female adolescents participating in an HIV/STD prevention intervention trial. Sex Transm Dis. 2001;28:468–471. doi: 10.1097/00007435-200108000-00009. [DOI] [PubMed] [Google Scholar]
- 9.Clark LR. Brasseux C. Richmond D. Getson P. D'Angelo LJ. Are adolescents accurate in self-report of frequencies of sexually transmitted diseases and pregnancies? J Adolesc Health. 1997;21:91–96. doi: 10.1016/s1054-139x(97)00042-6. [DOI] [PubMed] [Google Scholar]
- 10.Hornberger LL. Rosenthal SL. Biro FM. Stanberry LR. Sexual histories of adolescent girls: Comparison between interview and chart. J Adolesc Health. 1995;16:235–239. doi: 10.1016/1054-139X(94)00074-O. [DOI] [PubMed] [Google Scholar]
- 11.Fennema JS. van Ameijden EJ. Coutinho RA. van den Hoek JA. Validity of self-reported sexually transmitted diseases in a cohort of drug-using prostitutes in Amsterdam: Trends from 1986 to 1992. Int J Epidemiol. 1995;24:1034–1041. doi: 10.1093/ije/24.5.1034. [DOI] [PubMed] [Google Scholar]
- 12.Chen XS. Gong XD. Liang GJ. Zhang GC. Epidemiologic trends of sexually transmitted diseases in China. Sex Transm Dis. 2000;27:138–142. doi: 10.1097/00007435-200003000-00003. [DOI] [PubMed] [Google Scholar]
- 13.Chen XS. Yin YP. Liang GJ, et al. Sexually transmitted infections among female sex workers in Yunnan, China. AIDS Patient Care STDS. 2005;19:853–860. doi: 10.1089/apc.2005.19.853. [DOI] [PubMed] [Google Scholar]
- 14.China Center for Disease Control and Prevention. Reports of National STD and HIV/AIDS Surveillance Systems, 2004. Beijing: China Center for Disease Control and Prevention; 2005. [Google Scholar]
- 15.Parish WL. Laumann EO. Cohen MS, et al. Population-based study of chlamydial infection in China: A hidden epidemic. JAMA. 2003;289:1265–1273. doi: 10.1001/jama.289.10.1265. [DOI] [PubMed] [Google Scholar]
- 16.Huang Y. Henderson GE. Pan S. Cohen MS. HIV/AIDS risk among brothel-based female sex workers in China: Assessing the terms, content, and knowledge of sex work. Sex Transm Dis. 2004;31:695–700. doi: 10.1097/01.olq.0000143107.06988.ea. [DOI] [PubMed] [Google Scholar]
- 17.Hong Y. Li X. Behavioral studies of female sex workers in China: A literature review and recommendation for future research. AIDS Behav. 2008;12:623–636. doi: 10.1007/s10461-007-9287-7. [DOI] [PubMed] [Google Scholar]
- 18.Ruan Y. Cao X. Qian HZ, et al. Syphilis among female sex workers in southwestern China: Potential for HIV transmission. Sex Transm Dis. 2006;33:719–723. doi: 10.1097/01.olq.0000218881.01437.99. [DOI] [PubMed] [Google Scholar]
- 19.Gil VE. Wang MS. Anderson AF. Lin GM. Wu ZO. Prostitutes, prostitution and STD/HIV transmission in mainland China. Soc Sci Med. 1996;42:141–152. doi: 10.1016/0277-9536(95)00064-x. [DOI] [PubMed] [Google Scholar]
- 20.Qian HZ. Vermund SH. Wang N. Risk of HIV/AIDS in China: Subpopulations of special importance. Sex Transm Infect. 2005;81:442–447. doi: 10.1136/sti.2004.014258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Li X. Wang B. Fang X, et al. Short-term effect of a cultural adaptation of voluntary counseling and testing among female sex workers in China: A quasi-experimental trial. AIDS Educ Prev. 2006;18:406–419. doi: 10.1521/aeap.2006.18.5.406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Guangxi Center for Disease Control and Prevention. Update on HIV/AIDS epidemic in Guangxi.; Paper presented at Workshop of NIAAA Venue-based HIV and Alcohol Risk Reduction among Female Sex Workers in China; Jul 19–21;2009 ; Guilin, Guangxi. [Google Scholar]
- 23.Crowne DP. Marlowe D. A new scale of social desirability independent of psychopathology. J Consult Psychol. 1960;24:349–354. doi: 10.1037/h0047358. [DOI] [PubMed] [Google Scholar]
- 24.Holtgrave T. Social desirability and self-reports: Testing models of socially desirable responding. Pers Soc Psychol Bull. 2004;30:161–172. doi: 10.1177/0146167203259930. [DOI] [PubMed] [Google Scholar]
- 25.Cuixia L. Jian X. Zhongfang Y. A compromise between self-enhancement and honesty: Chinese self-evaluations on social desirability scales. Psychol Rep. 2003;92:291–298. doi: 10.2466/pr0.2003.92.1.291. [DOI] [PubMed] [Google Scholar]
- 26.Schoenborn CA. Marsh SL. Hardy AM. AIDS knowledge and attitudes for 1992. Data from the National Health Interview Survey. Adv Data. 1994;23:1–16. doi: 10.1037/e608982007-001. [DOI] [PubMed] [Google Scholar]
- 27.Shen J. Zhang Y. Yang P. Shanghai: Shanghai Scientific and Technical Publishers; 2006. Practice manual of voluntary consulting and testing for AIDS. [Google Scholar]
- 28.Wang Y. Li B. Zheng J, et al. Factors related to female sex workers' willingness to utilize VCT service: A qualitative study in Jinan city, northern China. AIDS Behav. 2009;13:866–872. doi: 10.1007/s10461-008-9446-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Hong Y. Hong Y. Li X. Fang X. Zhao R. Depressive symptoms and condom use with clients among female sex workers in China. Sex Health. 2007;4:99–104. doi: 10.1071/sh06063. [DOI] [PMC free article] [PubMed] [Google Scholar]