Abstract
Objectives
To explore knowledge, awareness and attitudes among caregivers of hospitalized children regarding MRSA.
Study Design
We developed and administered a bedside questionnaire to caregivers of hospitalized children in contact isolation for MRSA colonization or infection.
Results
Out of 104 caregivers approached, 100 (96%) consented to participate. The caregivers’ children included 28 (28%) newly recognized as MRSA colonized or infected during the hospitalization and 72 (72%) previously identified as MRSA colonized or infected. Eighteen (18%) caregivers had no knowledge of MRSA. Twenty nine (29%) were unaware that their child had MRSA, including caregivers of 9 newly identified MRSA patients and 20 previously identified MRSA patients. Of the 71 caregivers aware of their child's MRSA status, 89% had concerns; 77% worried about risks of future MRSA infection, 51% worried about spreading MRSA, and 16% described a feeling of stigma. Worries were more common among caregivers of children with newly identified MRSA (P<0.05).
Conclusion
Caregivers of children hospitalized with MRSA are frequently unaware that their child has MRSA. Among those aware of their child's MRSA status, many have concerns and worries. Caregivers of children with newly identified MRSA more often are worried and may need additional education and reassurance.
Keywords: Staphylococcus aureus, Methicillin-resistance, Knowledge, Attitudes, Caregivers, Pediatrics
Introduction
The national prevalence of methicillin-resistant Staphylococcus aureus and the incidence of MRSA-related hospitalizations have increased.[1, 2] Identification and isolation of patients infected or colonized with MRSA in the hospital may prevent MRSA transmission and reduce MRSA infections.[3, 4] As a result, some states and national organizations recommend routine MRSA screening of selected hospitalized patients.[5] These MRSA control strategies are viewed as important patient safety measures. However, little is known about how being labeled as “MRSA positive” impacts a child and the family. [6, 7] The current study was designed to explore the knowledge, awareness and attitudes of caregivers regarding MRSA, and to assess whether there were negative consequences of identifying and labeling children with MRSA.
Patient & Methods
Setting & Participants
The 175 bed Johns Hopkins Children's Center (JHCC) is embedded within a large tertiary care referral medical center. Study participants included caregivers of children admitted to JHCC between August 2009 & January 2010 and identified as colonized or infected with MRSA. The institutional review board approved this study.
Surveillance protocol and patient management
The Johns Hopkins Hospital (JHH) Department of Hospital Epidemiology and Infection Control (HEIC) directs an MRSA screening program which includes collection and culture of nasal swabs for MRSA at the time of admission for patients in the pediatric intensive care unit (PICU) and those transferred to our neonatal intensive care unit (NICU) from an outside institution and weekly for patients in the PICU and NICU. HEIC uses a real-time infection surveillance software (Theradoc V4.1.1; Theradoc, Salt Lake City, UT) to identify and flag patients with a history of MRSA colonization or infection at JHCC, a known history of MRSA colonization or infection from an outside institution, and anyone with a clinical or surveillance culture that grows MRSA. Each unit's charge nurse is alerted by pager when a patient is newly identified. Per hospital policy, the nurse initiates contact isolation (a sign is placed on the door, gowns and gloves are used by healthcare providers and parents, and the patient either is relocated to a private room if available or cohorted). A nurse or physician informs caregivers of the child's MRSA status and need for contact precaution and isolation (contact isolation). A patient information sheet about MRSA is available to families.
Data Collection
After obtaining written informed consent, semi-structured interviews were conducted with the child's caregiver. Survey questions had a median Flesher-Kincaid grade level of five. Both quantitative and qualitative data were collected. Response to quantitative questions on knowledge and awareness were captured from all participants in a pre-coded scheme; qualitative data were collected only from caregivers who were aware that their child had MRSA. Open-ended questions included – ‘what were you told about MRSA the first time you were informed that your child had MRSA?’, ‘how are you concerned about your child's MRSA?’ (if the caregiver acknowledged concern in preceding questions), ‘how do you think people with MRSA are treated differently because they had MRSA?’, ‘what information was provided by the hospital about how you can reduce the risk of getting a MRSA infection’ and ‘what other information do you want to know about MRSA?’ Verbatim responses were transcribed during the interview.
Definitions
Caregivers were individuals who lived with and cared for the child. A ‘newly identified’ MRSA patient was defined as someone identified for the first time as MRSA colonized or infected during the current hospitalization. A ’previously identified’ MRSA patient was defined as someone identified as MRSA colonized or infected during a previous hospitalization at JHCC or an outside institution. We categorized participants as ‘having no knowledge of MRSA’ if they offered that they had never heard of MRSA and they knew nothing about it. We determined a caregiver's awareness of their child's MRSA status by whether they stated having been informed in the current or a previous hospitalization that their child had MRSA.
Statistical Analysis
Quantitative data were analyzed using Fisher exact or Chi square test for proportion. For qualitative data, interview scripts were subjected to content analysis by the first author (A.S.) using grounded theory with inductive and deductive techniques.[8, 9] Data were extracted from each interview and coded into categories. The categories identified were collated and duplications removed. A cyclical process of collection of data, analysis, and development of provisional coding scheme was maintained and used for further sampling to identify emerging themes, subthemes and dimensions.[8, 9] Themes were concepts or ideas that persisted throughout the data, subthemes were common threads within a theme, and a dimension was a spectrum along which attributes or properties could be arranged. The principal investigator (A.M.) independently reviewed the data and generated codes to represent both a priori and emergent themes. A consensus was reached on final coding scheme and categories. Data was entered into NVIVO 8.0 software (QSR International PTY Ltd, Victoria, Australia) per the resulting coding scheme.
Results
Participant Characteristics
Out of 104 caregivers approached, 100 (96%) consented to participate in the study. Of the caregivers, 65 were mothers, 26 were fathers, and nine were grandparents; 72 were female, 55 were Caucasians and 41 were African-Americans. Fifty-four caregivers had one year or more of college education and another 38 had a high school degree. The participants’ children included 28 (28%) with newly identified MRSA and 72 (72%) with previously identified MRSA. Of those newly identified, 12 (43%) had an MRSA infection and 16 (57%) were colonized with MRSA without evidence of an infection. Of the children, 73 were admitted to the medical/surgical ward, 23 to the PICU and four to the NICU.
Knowledge Regarding MRSA and Awareness of Child's MRSA status
Eighteen (18%) caregivers reported having no knowledge about MRSA. Caregivers who had no knowledge about MRSA tended to be African-American (70% vs. 35%, P<0.01) and have an education level of twelfth grade or below (67% vs. 41%, P=.05) compared with those who had reported some knowledge. Many caregivers (29%) were unaware that their child had MRSA, including nine of 28 whose children were newly identified and 20 of 72 whose children were previously identified with MRSA (32 % vs. 28%, p=0.70) 148 (Table 1). Caregivers who were unaware of their child's MRSA status tended to be African-American (62% vs. 32%, P<.01) compared with those who were aware. Education level did not influence 150 caregiver awareness (P=0.47).
Table 1.
Awareness about Children's Methicillin-Resistant Staphylococcus aureus (MRSA) Status among Caregivers whose Children were in Contact Isolation for MRSA
| New MRSA Carriera [N= 28] | Known MRSA Carrierb [N=72] | All MRSA Carriers [N=100] | |
|---|---|---|---|
| “During this hospital stay were you told that your child has a MRSA infection or MRSA on their body?” | |||
| Yes (%) | 19 (68) | 20 (28) | 39 (39) |
| “Have you ever been told that your child has a MRSA infection or MRSA on their body?” | |||
| Yes (%) | - | 32 (44) | 32 (32) |
| Caregivers with no recollection of being informed during the current or a previous hospitalization that their child had an MRSA infection or MRSA on their body | |||
| Yes (%) | 9 (32) | 20 (28) | 29 (29) |
N – number of respondents
Child identified for the first time as MRSA colonized or infected during the current hospitalization
Child identified as MRSA colonized or infected during a previous hospitalization at JHCC or an outside institution
Attitudes of caregivers
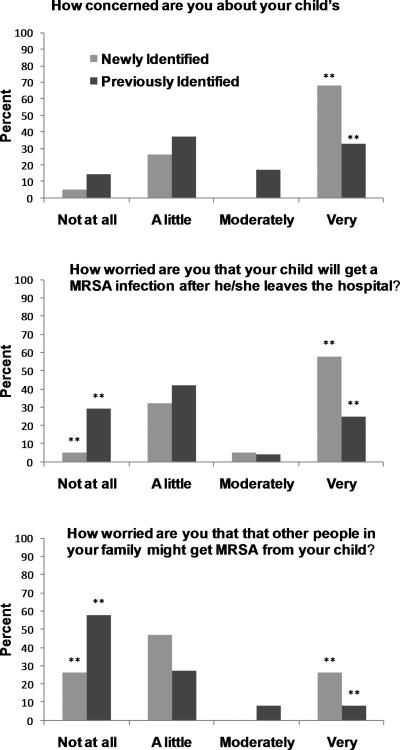
Of the 71 caregivers who knew their child had MRSA, 63 (89%) had concerns; 55 (77%) worried about the risk of future MRSA infection in their child, and 36 (51%) worried about their child spreading MRSA to others. Of the caregivers, 24 (34%) had a relative with MRSA. There was no difference in concerns or worries comparing those who had a relative with MRSA and those who did not have a relative with MRSA. Caregivers of children with newly identified MRSA (68%) were more likely to be ‘very concerned’ than caregivers of children with previously identified MRSA (33%) (p<0.01) (Figure1). Similarly caregivers of children with newly identified MRSA were more likely to be ‘very worried’ about the perceived threat of a future MRSA infection to their child (p<0.01) or about their child spreading MRSA to others (p<0.05) than caregivers of children with previously identified MRSA. Among caregivers of children with newly identified MRSA, we did not find a difference in concerns or worries between those whose children were infected or colonized with MRSA. There were no differences in the caregiver's concerns or worries among those with children of different ages.
Figure 1.
Caregivers of children with MRSA were asked about their concerns and worries. Responses were captured using a Likert scale and stratified by caregivers of children newly identified with MRSA and caregivers of children previously identified with MRSA. ** denotes responses that had a statistically significant difference (P<0.05).
Themes, Subthemes, & Dimensions Revealed through Qualitative Analysis (Table 2)
Table 2.
Identified Themes, Subthemes, and Dimensions in Knowledge, Awareness and Attitudes among Caregivers of Children with Methicillin-Resistant Staphylococcus aureus
| Theme | Subtheme | Dimension |
|---|---|---|
| Delay in disclosure | Displeasure | Discontent |
| Dismay | Disappointment | |
| Gaps in knowledge | Feeling of incomplete briefing by healthcare providers | Frustration |
| Lack of sharing information among caregivers | Need to share knowledge | |
| Concern and Anxiety | Protection of children and family members | Helplessness |
| Persistence and recurrence of MRSA | Uncertainty | |
| Relationship with healthcare providers | Apprehension | |
| Accurate information reassures | Reassurance | |
| Inadequate knowledge drives anxiety | Vulnerability | |
| Experience reduces concern & anxiety | Value of experience | |
| Social stigma | Isolation | Fear |
| Coping | Adaptation | |
| Eagerness for information | Simple language, relevant information | Eagerness |
Questions were only asked of caregivers who knew their child had MRSA
Delayed disclosure
Several caregivers described delays in alerting them that their child had MRSA . The caregiver of a five year old child expressed her displeasure in this regard: “If she had MRSA in 2005 as I was told today, why the hospital made no effort to let us know this before?” Parents may become upset and frustrated with this delayed disclosure. The mother of a three year old child articulated: “Docs didn't tell me about it the first time they diagnosed it, I found out about MRSA in a follow-up visit when I saw doctors taking precautions while examining him. It was really upsetting. I couldn't believe they wouldn't tell me to begin with and (then) still take precautions!”
Awareness of gaps in knowledge
Despite knowing that their child had MRSA, some caregivers acknowledged an incomplete understanding of MRSA. Reflecting upon what they were told when their child was first identified as having MRSA , one mother said: “I was told she has MRSA; that is all”, and another said: “[I was told] that she has MRSA and they need to take precaution”. The father of a six month old child said: “we were told that the baby's test has come (back) positive for MRSA. They talked to my wife and I have not seen her yet. So I do not know the fine details.”
Concern and anxiety among caregivers
Learning that a child has MRSA can be an alarming experience for a caregiver. One father said: “For us, everything was fine until today when they told us he has MRSA. We don't know what to do!” Three major areas of concern and anxiety emerged. First, caregivers worried about how to protect the child and other family members at home from getting infected with MRSA. One caregiver said: “I do not know anything about it. I have children in my house and people with heart disease.” Another exclaimed: “Is it bad to go home with it? What (can we) do in home to prevent infections from MRSA?” Second, caregivers were concerned about the uncertainty of persistence and recurrence of MRSA. One mother stated: “Repeated admissions and coming back and forth to hospitals are troubling. The infection keeps coming back. If something can be done to stop this, it will be helpful.” Third, caregivers worried how sharing information about their child's MRSA would affect their relationship with healthcare providers. One mother said: “Would it be a problem for me to let his future health providers know that he has MRSA?” Another mother said: “Should we tell her nurse (at) home that she has MRSA?” A subtheme emerged that caregivers who thought they knew and understood more about MRSA were less concerned and anxious. One mother said: “We were told that she had MRSA on the skin. It is not that serious, (and) can be treated. They told us to be careful and to keep clean and practice hand washing”. Another mother said: “We are only a little concerned; they said he is just a carrier.” On the other hand, caregivers who perceived that they had an incomplete understanding of MRSA were more vulnerable to anxiety. One mother said: “I want to know about MRSA in detail. What is it? Where it comes from? Can it be gotten rid of? Is it deadly? Can others get it? Is it airborne? Right now we only know scary things about MRSA. We want to know exactly what kind of threat it is”. Open ended questioning suggested that caregivers’ experience with MRSA over time reduced concern and anxiety. One mother said: “I am only a little concerned; not a lot since it's been a long time and she never got an infection from it till now”. Another mother said: “Only a little since she had it before without any problem.”
Social Stigma
Caregivers reported social stigma attached to MRSA. Eleven caregivers (16%) revealed behavior outside of the hospital that can be perceived as a consequence of social stigma. One mother said: “Some people think people with MRSA are dirtier because they have MRSA. There is a stigma attached to it.” Another mother said: “Yes there is social isolation. People would not be around someone after knowing he has MRSA“. One father said: “People have scary perceptions about MRSA; (they) want to keep away from people who have MRSA“. Another father said: “When my wife tested positive for MRSA, the plastic surgeon refused to do surgery on her”. One mother said: “Once a person asked me if MRSA was an STD. I think uneducated people get freaked out when they know someone has MRSA.” Caregivers may change their behaviors to adapt to this social stigma. When asked if people treat her child differently because she had MRSA, one mother said: “Within the hospitals, they apply precautions and isolation. I do not let other people (outside the hospital) know she has MRSA.” Another said: “She is fine outside because I tell nobody she has MRSA.” Social stigma concerns some caregivers who fear repercussions. One caregiver said: “We cannot tell the school that he has MRSA; that may have consequences. So instead we want to know what to do to prevent (its) spread and protect others“. Caregivers think that being informed helps to cope. One mother said: “I think the best way to de-stigmatize MRSA is to inform the parent and the child what MRSA is and what their exact status is. That makes life easier”.
Caregivers seek more information
Caregivers frequently have questions and want to learn more about MRSA (Table 3). One father said: “Explain what it is; what needs to be done in addition to normal childcare; in simple language”.
Table 3.
Information Sought by Caregivers of Children Hospitalized with Methicillin-Resistant Staphylococcus aureus (MRSA)
| What is MRSA? |
| Where does it come from? |
| Is having MRSA the same as having an infection from MRSA? |
| Is the chance of infection higher in people who carry it? |
| What are the risk factors to get a future infection from MRSA? |
| Why are hospitals so concerned about MRSA? |
| What is the rationale for precautions and isolation? |
| Should I be worried to have a child with MRSA at home? |
| How to prevent future MRSA infection in the child? |
| How to prevent the spread of MRSA to others? |
| How to know if my child has an infection from MRSA and what to do? |
| Is it going to persist forever? |
| Is it necessary to treat with antibiotics? |
| Is there any way to get rid of it? |
| How would sharing information with healthcare providers about the child's MRSA affect them? |
Discussion
Increasingly, children are hospitalized with MRSA colonization or infections.[1] In an attempt to prevent MRSA transmission, some institutions screen patients to identify those colonized with MRSA.[10, 11] As a result, more caregivers are informed that their child has MRSA. To our knowledge, no studies have examined how effectively this information is conveyed to families and the impact it has on children and their caregivers. Our findings suggest that many caregivers whose hospitalized children were kept in contact isolation had no knowledge of MRSA and were unaware that their child had MRSA. Among those aware of their child's MRSA status, many were concerned, anxious, and wanting more information about MRSA in order to protect their child and family members.
In this study, we did not try to quantify caregiver's knowledge of MRSA; rather we assessed caregiver's perception of their knowledge of MRSA. Many caregivers felt that their knowledge was lacking and this perception often fueled concern and anxiety. These findings are similar to studies of perceptions of adult patients with MRSA.[12, 13] Caregivers who perceived a better understanding of MRSA were less concerned and anxious. Caregivers were eager for information beyond their child's MRSA status and the need for contact isolation. They wanted to learn how to protect their children and others in the household from MRSA infections. When a child is identified as being infected or colonized with MRSA, caregivers should be notified and the disclosure of information needs to be timely, personal, and comprehensive, yet individualized to the patient's context, recognizing unique risks to the child and other family members.
Most previous studies on patient perceptions regarding MRSA have involved adults.[12, 13] When counseling adult patients about MRSA, healthcare providers can reference data from relevant studies on the duration of MRSA colonization, long-term risk of MRSA infection, and intervention strategies to prevent MRSA infection.[14-17] Similar studies are needed among children, so caregivers can be counseled and reassured with data from pediatric studies instead of extrapolation from adult literature and speculation.[18]
Our study consistently identified caregivers who recognized a stigma from MRSA that affected the lives of their children and their families. This stigma extended to interactions in the hospital, at home, at school, and with other healthcare providers. Similar to patients with leprosy, human immunodeficiency virus (HIV) and sexually transmitted diseases, caregivers often did not share their child's MRSA status with others in fear of social isolation. [7, 19, 20] Healthcare providers should be aware of the potential for a feeling of stigma when counseling families. Media descriptions of MRSA are often sensationalized and focus on contagiousness, severe disease and death. Community education campaigns and other strategies may help to allay unnecessary fears that provokes stigma surrounding MRSA.[20, 21]
Certain limitations should be considered when interpreting our data. Caregivers were mostly Caucasian or African American race, limiting the conclusions generalizability to other populations in the United States. Whether or not caregivers present at their child's bedside represent a group that is more or less likely to be concerned or worried about their child's care is unknown. Many of the important findings in our study emerged from qualitative data analysis. These findings may not be representative or quantifiable, but we provided the frequency of key themes wherever possible. Recognizing limitations of qualitative studies, we also accounted for our analytic process and included context for each quote, so that readers can assess our interpretations. To ensure reliability, two researchers independently evaluated the data to reach consensus.
Conclusion
Our findings suggest that the way in which we communicate about MRSA has the potential to alleviate or create concern and anxiety among caregivers of children with MRSA. Healthcare providers need to be equipped with accurate information to reassure caregivers and the community at large. Excellent resources, including fact sheets, are available from the Centers for Disease Control and Prevention.[22] More research is needed to determine how to best inform and reassure caregivers about MRSA and how to protect children and family members from the stigma associated with MRSA.
Acknowledgements
We would like to thank Kathleen Speck MPH, Claire Beers RN MSN, Alicia Budd MPH, the JHH Department of Hospital Epidemiology and Infection Control, and the JHCC nurses for their support of this study. This study was supported by K23AI081752 from the National Institute of Allergy and Infectious Diseases (NIAID) to A.M.M.. The content is solely the responsibility of the authors and does not necessarily represent the official views of NIAID or the NIH.
Financial Disclosures and Conflict of Interest: This study was supported by NIH/NIAID 1 K23 AI081752-01 (A.M.M.). A.M. and T.M.P. receive grant support from Sage Products, Inc. T.P. was on an advisory board and received honorarium from Pfizer and BioMerieux, was on an advisory panel for Theradoc Inc., and received an honorarium from 3M. A.S. and C.R. report no disclosures.
Abbreviations
- MRSA
Methicillin-Resistant Staphylococcus aureus
- JHCC
Johns Hopkins Children's Center
- JHH
Johns Hopkins Hospital
- HEIC
Hospital Epidemiology and Infection Control
- PICU
Pediatric Intensive Care Unit
- NICU
Neonatal Intensive Care Unit
- STD
Sexually Transmitted Disease
Footnotes
Disclosures: This study was supported by NIH/NIAID K23AI081752. A.M. and T.M.P. receive grant support from Sage Products, Inc. T.P. was on a advisory board and received honorarium from Pfizer and BioMerieux, was on an advisory panel for Theradoc Inc., and received an honorarium from 3M. A.S. and C.R. reports no disclosures.
References
- 1.Gerber JS, Coffin SE, Smathers SA, Zaoutis TE. Trends in the incidence of methicillin-resistant Staphylococcus aureus infection in children's hospitals in the United States. Clin Infect Dis. 2009;49:65–71. doi: 10.1086/599348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Gorwitz RJ, Kruszon-Moran D, McAllister SK, McQuillan G, McDougal LK, Fosheim GE, et al. Changes in the prevalence of nasal colonization with Staphylococcus aureus in the United States, 2001-2004. The Journal of infectious diseases. 2008;197:1226–34. doi: 10.1086/533494. [DOI] [PubMed] [Google Scholar]
- 3.Henderson DK. Managing methicillin-resistant staphylococci: a paradigm for preventing nosocomial transmission of resistant organisms. American journal of infection control. 2006;34:S46–54. doi: 10.1016/j.ajic.2006.05.228. discussion S64-73. [DOI] [PubMed] [Google Scholar]
- 4.Robicsek A, Beaumont JL, Paule SM, Hacek DM, Thomson RB, Jr., Kaul KL, et al. Universal surveillance for methicillin-resistant Staphylococcus aureus in 3 affiliated hospitals. Annals of internal medicine. 2008;148:409–18. doi: 10.7326/0003-4819-148-6-200803180-00003. [DOI] [PubMed] [Google Scholar]
- 5.Calfee DP, Salgado CD, Classen D, Arias KM, Podgorny K, Anderson DJ, et al. Strategies to prevent transmission of methicillin-resistant Staphylococcus aureus in acute care hospitals. Infect Control Hosp Epidemiol. 2008;29(Suppl 1):S62–80. doi: 10.1086/591061. [DOI] [PubMed] [Google Scholar]
- 6.Kirkland KB. Taking off the gloves: toward a less dogmatic approach to the use of contact isolation. Clin Infect Dis. 2009;48:766–71. doi: 10.1086/597090. [DOI] [PubMed] [Google Scholar]
- 7.Mozzillo KL, Ortiz N, Miller LG. Patients with methicillin-resistant Staphylococcus aureus infection: twenty-first century lepers. The Journal of hospital infection. 2010;75:132–4. doi: 10.1016/j.jhin.2009.10.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Green J, Thorogood N. Qualitative Methods for Health Research. First ed Sage Publications Ltd; 2007. [Google Scholar]
- 9.Miles MB, Huberman M. Qualitative Data Analysis. Second ed Sage Publications Ltd.; 1994. [Google Scholar]
- 10.Milstone AM, Carroll KC, Ross T, Shangraw KA, Perl TM. Community-associated methicillin-resistant Staphylococcus aureus strains in pediatric intensive care unit. Emerging infectious diseases. 2010;16:647–55. doi: 10.3201/eid1604.090107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Milstone AM, Perl TM. Fact, fiction, or no data: what does surveillance for methicillin-resistant Staphylococcus aureus prevent in the intensive care unit? Clin Infect Dis. 2008;46:1726–8. doi: 10.1086/587902. [DOI] [PubMed] [Google Scholar]
- 12.Newton JT, Constable D, Senior V. Patients’ perceptions of methicillin-resistant Staphylococcus aureus and source isolation: a qualitative analysis of source-isolated patients. The Journal of hospital infection. 2001;48:275–80. doi: 10.1053/jhin.2001.1019. [DOI] [PubMed] [Google Scholar]
- 13.Tarzi S, Kennedy P, Stone S, Evans M. Methicillin-resistant Staphylococcus aureus: psychological impact of hospitalization and isolation in an older adult population. The Journal of hospital infection. 2001;49:250–4. doi: 10.1053/jhin.2001.1098. [DOI] [PubMed] [Google Scholar]
- 14.Ridenour G, Lampen R, Federspiel J, Kritchevsky S, Wong E, Climo M. Selective use of intranasal mupirocin and chlorhexidine bathing and the incidence of methicillin-resistant Staphylococcus aureus colonization and infection among intensive care unit patients. Infect Control Hosp Epidemiol. 2007;28:1155–61. doi: 10.1086/520102. [DOI] [PubMed] [Google Scholar]
- 15.Simor AE, Phillips E, McGeer A, Konvalinka A, Loeb M, Devlin HR, et al. Randomized controlled trial of chlorhexidine gluconate for washing, intranasal mupirocin, and rifampin and doxycycline versus no treatment for the eradication of methicillin-resistant Staphylococcus aureus colonization. Clin Infect Dis. 2007;44:178–85. doi: 10.1086/510392. [DOI] [PubMed] [Google Scholar]
- 16.Robicsek A, Beaumont JL, Peterson LR. Duration of colonization with methicillin-resistant Staphylococcus aureus. Clin Infect Dis. 2009;48:910–3. doi: 10.1086/597296. [DOI] [PubMed] [Google Scholar]
- 17.Huang SS, Platt R. Risk of methicillin-resistant Staphylococcus aureus infection after previous infection or colonization. Clin Infect Dis. 2003;36:281–5. doi: 10.1086/345955. [DOI] [PubMed] [Google Scholar]
- 18.Hersh AL, Cabana MD, Gonzales R, Shenkin BN, Cho CS. Pediatricians’ perspectives on the impact of MRSA in primary care: a qualitative study. BMC pediatrics. 2009;9:27. doi: 10.1186/1471-2431-9-27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Cunningham SD, Tschann J, Gurvey JE, Fortenberry JD, Ellen JM. Attitudes about sexual disclosure and perceptions of stigma and shame. Sexually transmitted infections. 2002;78:334–8. doi: 10.1136/sti.78.5.334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Emlet CA. Experiences of stigma in older adults living with HIV/AIDS: a mixed-methods analysis. AIDS patient care and STDs. 2007;21:740–52. doi: 10.1089/apc.2007.0010. [DOI] [PubMed] [Google Scholar]
- 21.Cao X, Sullivan SG, Xu J, Wu Z. Understanding HIV-related stigma and discrimination in a “blameless” population. AIDS Educ Prev. 2006;18:518–28. doi: 10.1521/aeap.2006.18.6.518. [DOI] [PubMed] [Google Scholar]
- 22.2010 http://www.cdc.gov/ncidod/dhqp/ar_mrsa_ca.html.