Abstract
Objective
To study health care utilization patterns in patients with gout.
Methods
In a gout population from primary care and rheumatology clinics in three U.S. metropolitan cities, we collected data on gout-related utilization (primary care, rheumatology, urgent care, emergency room and other) in the past year. We evaluated the association of comorbidities, age, gender, gout characteristics (time since last gout attack and tophi) and gout severity ratings (mean of serum uric acid, patient-rated and physician-rated gout severity) and with emergency/urgent care and primary care utilization using regression and correlation analyses.
Results
Of the 296 patients who reported visiting at least one type of health practitioner for gout in the past year, percent of patients utilizing the service at least once and annual utilization rates among utilizers were: primary care physician, 60%, 3.0±3.4; nurse practitioner/physician assistant, 26%, 2.7±2.5; rheumatologist, 51%, 3.7±5.7; urgent care, 23%, 2.1±2.2; emergency room, 20%, 2.0±1.7; and hospitalization, 7%, 2.1±1.4. Higher overall gout severity was associated with greater use of each resource type and with overall gout-related utilization. Non- emergency/non-urgent care utilization (primary care physician, nurse practitioner, physician’s assistant and rheumatologist for gout) was the strongest predictor of gout-related emergency/urgent care utilization. Patients with more comorbidities had greater gout-related primary care utilization.
Conclusions
Overall gout severity was associated with all types of gout-related utilization. This may help to screen high utilizers for targeted behavioral and therapeutic interventions. Having a higher number of comorbid conditions was a risk factor for higher gout-related primary care utilization.
Keywords: Health care utilization, gout, predictors, resource utilization, gout severity
INTRODUCTION
With rapidly increasing health care costs in the U.S., health care policy makers have to assess resource utilization. Common conditions such as cardiovascular disease, diabetes, hypertension and arthritis contribute to significant utilization of health care resources. Gout is a common arthritis in adults, affecting approximately 5 million Americans (1), associated with an estimated health care cost of $27 million annually in the US for the new gout cases of acute gout (2). Costs for a gout patient versus a patient without gout are approximately $3,000 higher annually (3–4) or $134 (Canadian) higher monthly (5).
Although gout-related costs have been estimated (4–6), only a handful of studies have examined the specific types of health care resources utilized by gout patients (5–6) and none have examined the association of gout characteristics with health care utilization. One study reported the association of tophaceous gout (vs. non-tophaceous gout) with significantly higher 12-month all-cause and gout-related costs (4). Another study suggested that having a serum uric acid level ≥9 mg/dl was associated with significantly higher gout-related costs (4) and ≥6 mg/dl with higher gout flare cost (7).
The outcome of interest in these two studies was health care costs, not the underlying types of health care utilization. Veterans with gout have been shown to have more annual primary care visits and annual hospitalizations compared to veterans without gout after adjusting for differences in socio-demographics, comorbidities and health care access (6); however, disease characteristics were not examined. Thus, there is a lack of prospective studies describing the correlates of resource utilization in patients with gout. Identification of correlates will not only improve our understanding of gout’s impact on patients, the health care system, and society, but also identify potential areas of intervention that may reduce resource utilization and improve patients’ quality of life.
Our objective was to study health care utilization patterns and factors associated with higher health care utilization in patients with gout. Specifically, we studied primary care, rheumatology, and emergency/urgent health care utilization in patients with gout, and whether the following were associated with these types of gout-related utilization: patient and physician-rated gout severity, overall gout severity (composite measure), serum uric acid (sUA) concentration, gout characteristics such as time since last attack and presence or absence of tophi, and comorbidity characteristics.
METHODS
This study was conducted as part of a larger study validating a new gout-specific health related quality of life instrument (8). The sample was recruited from gout patients attending a variety of clinics (e.g. rheumatology, primary care) in three U.S. cities (San Diego, Cincinnati and Minneapolis) using physician in-office recruitment, patient response to clinic posters and local newspaper advertisements. Inclusion criteria were: age between 18 and 85, presence of gout as determined by physician (per American College of Rheumatology (ACR) preliminary criteria) (9) or reported by the patient, ability to read and/or understand patient informed consent and independently complete questionnaires in English, and provision of contact information for physician currently treating gout.
All consenting patients completed a series of questions regarding their gout (e.g. number of attacks, treatment), comorbidities, demographics, and gout-related health care utilization over the past year. Patients self-rated their gout severity on a 0–100 mm visual analog scale (VAS) ranging from “not severe at all” to “gout as severe as you can imagine.”
Physicians of participating patients were contacted via fax to confirm gout diagnosis and characterize the severity of their patient’s gout. Data collected from physicians included: date and method of gout diagnosis, presence or absence of tophi, most recent and the highest serum urate levels in the preceding year from laboratory records, flare frequency of gout in the past year, and a physician’s global assessment of patient’s overall gout severity using a VAS on a 1–5 Likert scale (very mild, mild, moderate, severe, very severe). All study procedures were approved by the University of California San Diego, San Diego Veterans Affairs Medical Center (VAMC), Cincinnati VAMC, University of Cincinnati and Minneapolis VAMC Human Research Protection Programs.
Data Analysis
For analysis, we divided gout-related health care utilization into the following four summary categories: (i) primary care (comprised of gout-related visits to any primary care physician, nurse practitioner, or physician’s assistant), (ii) rheumatology (visits to rheumatologist), (iii) emergency or urgent care and (iv) total utilization. The total utilization category includes visits to health care providers in the first three categories as well as the number of gout-related overnight hospital stays and visits made for gout to “other” health care providers (such as other non-rheumatology subspecialists etc.). We considered, but did not perform chart validation of utilization, since patients from different sources (referrals from private community clinics by calling the 800 number, University hospital practices in two cities, Cincinnati and San Diego, and three VA Medical centers). Validation of utilization in one health care system only would underestimate gout-related utilization and the ability to access records from each private community practice was limited due to limited resources. Each participant’s patient-rated, physician-rated and sUA gout severity variables were z-transformed (10), then averaged together to form a measure of overall gout severity (mean of 0 and standard deviation of 1).
We conducted univariate and multivariable analyses to investigate the factors associated with the frequency of health care utilization in patients with gout, as well as whether or not a specific resource type (e.g. primary care) was utilized. Outcomes of interest for these analyses were number of primary care visits, number of rheumatologist visits, number of emergency/urgent care visits, and total number of visits to any health practitioner for gout. Predictors of interest included gout severity ratings including: patient-rated, physician-rated, most recent sUA (long standing hyperuricemia has been linked to more frequent gout flares (11)), and overall severity, gout flare frequency in the past year, an overall gout severity composite measure, age, gender, time since the patient’s last gout attack, presence or absence of tophi, and self-reported comorbidities. Comorbid conditions recorded were heart disease (defined as heart attack or heart failure), kidney disease (defined as kidney stones, transplant, or other kidney problems), high blood pressure, high cholesterol, and diabetes.
We conducted correlation analyses for each predictor of interest and the frequency of primary care, rheumatology, emergency/urgent care and total utilization. We used multiple linear regression analyses to determine the relative weight and significance of gout-related severity measures and gout characteristics associated with the frequency of gout-related health care utilization, controlling for age, gender, and comorbidities. We created separate regression models with comorbidities included as individual conditions and as total number of comorbidities reported by each patient. Since the results of the regression analysis adjusting for individual conditions were very similar to the analyses adjusting for overall number of comorbidities, we only present the data for the former. We used logistic multiple regression to examine whether or not various health care services were utilized. For logistic regressions, we re-coded utilization types into dichotomous variables (yes/no).
We performed additional multivariable analyses, (i) to create a predictive model for Emergency Room and Urgent Care utilization and (ii) to examine the relationship between total number of comorbidities and primary care utilization. We used stepwise multiple regressions to determine the best predictive model for the amount (frequency) of Emergency Room and Urgent Care utilization. Variables entered were gout severity ratings (including sUA level), time since last gout attack, tophi, age, gender, individual comorbidities, and number of total visits over the previous year to any type of health practitioner for gout. We entered these same variables into logistic regressions using forward and backward likelihood ratio selection to determine the strongest predictors of whether or not the Emergency or Urgent Care departments were used for gout treatment. Hospitalizations were too few to be analyzed as a separate outcome. Linear regression was used to investigate the relative weight and significance of number of comorbidities associated with frequency of primary care utilization, controlling for rheumatologist utilization and gout severity. Correlations less than 0.30 were considered to be small, between 0.30 and 0.49 moderate, and greater than 0.50 large (12). We set statistical significance at p < 0.05 for group comparisons and performed all statistical analyses using SPSS software, Version 15.0 (Chicago, IL).
RESULTS
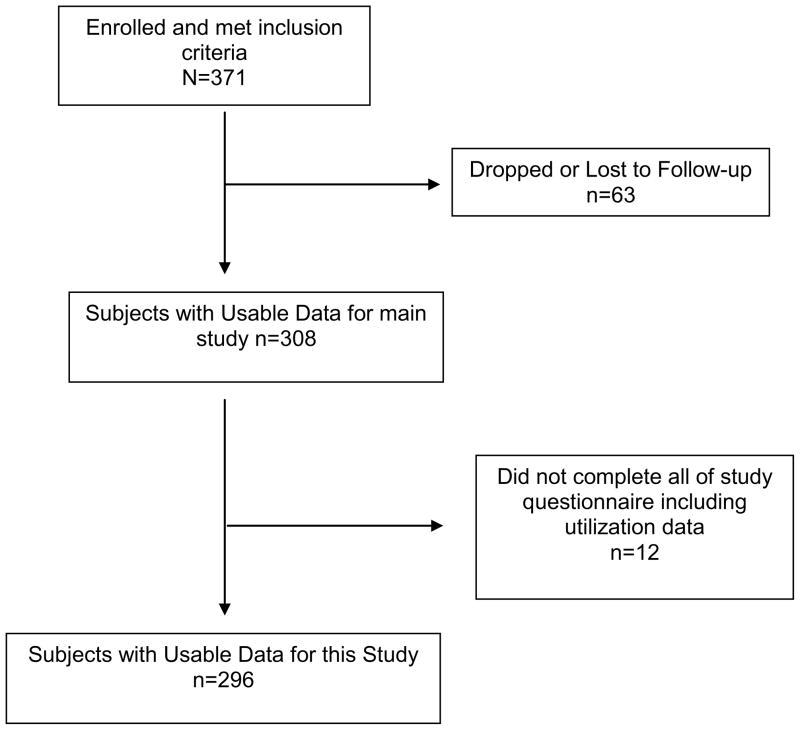
The original cohort consisted of a total of 298 patients who completed the study questionnaire. Of the original cohort, 296 (99.3%) provided utilization data and are included in the current study (Figure 1). Physicians responded for 224 patients, with gout diagnosis confirmed for 202 of the patients for whom physicians provided supporting data (90.2%). 60% of patients were recruited from the three VA medical centers and 40% from private practices.
Figure 1.
Flow chart of study population
Demographic and clinical information about the study participants including the gout severity ratings are included in Table 1. The mean age of participants was 62.3 (±11.8) the majority of patients were male (90.8%) and significant proportion (42.7%) were obese with a BMI of greater than 30. The race of the participants was mainly Caucasian at 76%, 13% African-American, 6% Asian and 5% other racial categories. The mean sUA level was 7.10 (±1.89) mg/dl, with 66.3% of patients having an sUA level between 6.0 and 10.0 mg/dl. The most frequently reported comorbidities were high blood pressure (73.9%), high cholesterol (58.8%) and kidney disease (35.4%). Diabetes and heart disease were reported by less than one-third of patients.
Table 1.
Demographics and clinical characteristics
| Number of Respondents | Mean ± SD or n (%) | |
|---|---|---|
| Age (mean ± SD) | 294 | 62.3 ±11.8 years |
| Gender [n (%)] | 294 | |
| Male | 267 (90.8%) | |
| Female | 27 (9.2%) | |
| Race [n (%)] | 287 | |
| Caucasian | 218 (76.0%) | |
| African American | 37 (12.9%) | |
| Asian | 16 (5.6%) | |
| Native Hawaiian/Pacific Islander | 5 (1.7%) | |
| American Indian | 2 (0.7%) | |
| Other | 9 (3.1%) | |
| Ethnicity [n (%)] | 250 | |
| Hispanic/Latino | 9 (3.6%) | |
| Not Hispanic/Latino | 241 (96.4%) | |
| BMI (kg/m2) (mean ± SD) | 293 | 30.2 ± 6.2 |
| Comorbidities [n (%)] | ||
| Hypertension | 291 | 215 (73.9%) |
| Hyperlipidemia | 291 | 171 (58.8%) |
| Kidney Problems | 277 | 98 (35.4%) |
| Diabetes | 287 | 93 (32.4%) |
| Heart Attack or Heart Failure | 286 | 74 (25.9%) |
| Kidney Stones | 282 | 62 (22.0%) |
| Kidney Transplant | 283 | 8 (2.8%) |
| Medications (non-gout) [n (%)] | ||
| Diuretics Use | 292 | 161 (55.1%) |
| Low Dose Aspirin Use (≤ 325mg/d) | 290 | 148 (51.0%) |
| Alcohol Intake [Drinks/wk, n (%)] | 287 | |
| None | 135 (47.0%) | |
| 1 | 50 (17.4%) | |
| 2–3 | 29 (10.1%) | |
| 3–7 | 38 (13.2%) | |
| > 7 | 35 (12.2%) | |
| Years Since MD Diagnosis of Gout | 286 | 13.8 years ± 12.3 |
| Latest Serum Uric Acid (mean ± SD) | 166 | 7.10 ± 1.89 mg/dl (421 ± 113 mmol/l) |
| Presence of Tophi [n (% Yes)] | 167 | 44 (26.3%) |
| Number Gout Attacks in the Past Year [n (%)] | 287 | |
| 0 | 63 (22.0%) | |
| 1–2 | 99 (34.5%) | |
| 3–5 | 72 (25.2%) | |
| 6–10 | 26 (9.1%) | |
| > 10 | 27 (9.4%) | |
| Overall Gout Severity by Patient (mean ± SD) | 259 | 5.4 ± 3.2 |
| Overall Gout Severity by Patient [n (%)] | 259 | |
| 0–30 (very mild-mild) | 79 (30.5%) | |
| 31–70 (moderate) | 85 (32.8%) | |
| 71–100 (severe-very severe) | 95 (36.7%) | |
| Overall Gout Severity by MD [n (%)] | 178 | |
| Very mild-mild | 99 (55.6%) | |
| Moderate | 57 (32.0%) | |
| Severe-Very severe | 22 (12.4%) | |
| Provider Specialty [n (%)] | 214 | |
| Gout Treated by Rheumatologist | 129 (60.3%) | |
| Gout Treated by Primary Care Providers | 80 (37.4%) | |
| Other | 5 (2.3%) | |
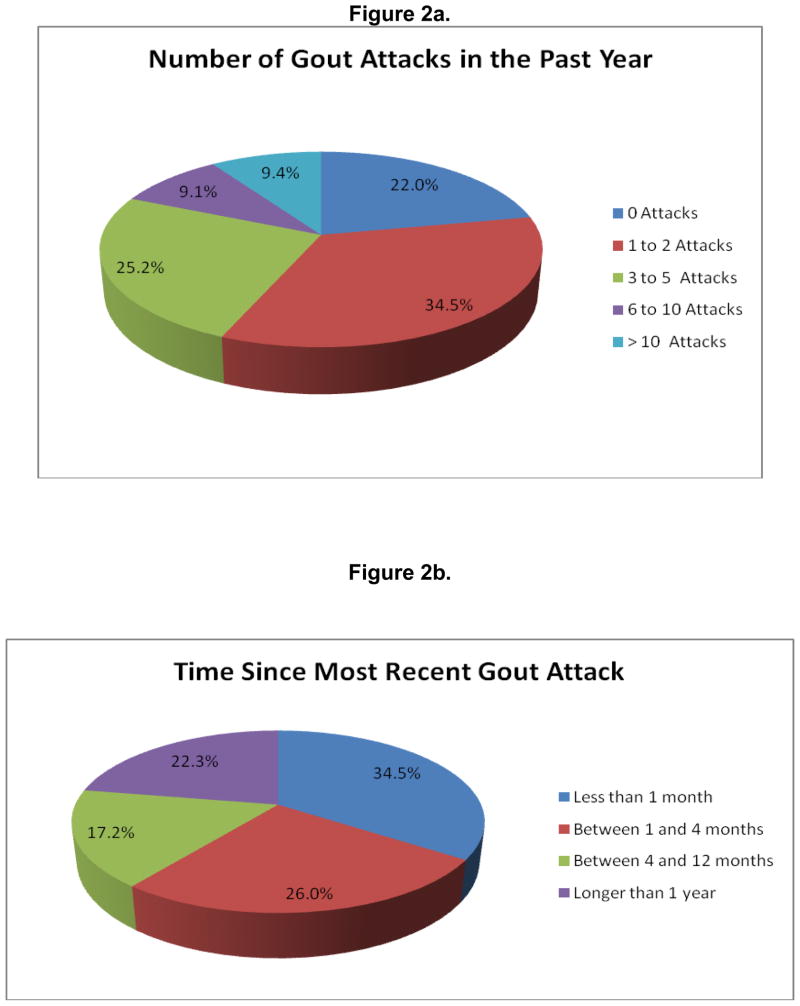
Most of the patients had a few to moderate number of gout attacks in the past year (34.5% had 1 or 2 attacks and 25.2% had 3–5 attacks). Slightly less than 20% of patients had more active gout, reporting 6 or more attacks in the past year. The remaining 22% of the population did not suffer any gout attacks in the past year. About one third of patients (34.5%) had experienced a gout attack within the month prior to completing the study questionnaire. One quarter of the patients (26.0%) had experienced their most recent gout attack between 1 and 4 months prior. Between 4 and 12 months had passed since the last gout attack for 17.2% of the population. The remainder of the patients (22.3%) reported that one or more years had passed since their last attack (Figure 2).
Figure 2.
Gout flares in the cohort, including the number of attacks in the past year (Figure 1a) and time since the most recent attack (Figure 1b).
Patient and physician-rated VAS severity assessments were available for 259 and 178 patients respectively. Patients were evenly distributed among mild, moderate and severe gout severity categories based on self-ratings (30.5%, 32.8%, 36.7%). Physician rated gout severity mild and moderate (55.6%, 32.0%) more often than severe (12.4%). Composite overall gout severity rating were 49.3% less than and 50.7% greater than median (Table 1).
Resource utilization by demographic, clinical and gout disease characteristics is summarized in Table 2. The most utilized gout-related health care resource in the past year was primary care physicians, used by 60.4% of patients with a mean annual utilization of 3.1 (± 3.4) visits (Table 3). Visits to rheumatologists were the next most commonly reported (50.7% of patients utilized with a mean annual number of visits of 3.7 ± 5.7). Nurse practitioner/physician assistant, urgent care and emergency department resources were each used by about one-quarter of patients, averaging approximately two visits each in the past year. Overnight hospitalization for gout was reported by less than 10% of patients.
Table 2.
Mean utilization by subject characteristics
| Physician + Nurse | Rheumatologist | Emergency + Urgent Care | Total Utilization | |||||
|---|---|---|---|---|---|---|---|---|
| Mean (SD) | n | Mean (SD) | n | Mean (SD) | n | Mean (SD) | n | |
| Age (years) | ||||||||
| <50 | 2.76 (4.56) | 37 | 1.33 (2.32) | 36 | 1.11 (1.78) | 35 | 5.41 (7.23) | 37 |
| 50–65 | 2.53 (3.92) | 135 | 2.49 (6.04) | 132 | 1.08 (2.30) | 129 | 6.74 (11.63) | 136 |
| 66–80 | 2.10 (3.54) | 102 | 1.21 (1.96) | 104 | 0.44 (1.00) | 94 | 3.83 (5.26) | 108 |
| >80 | 2.77 (4.23) | 13 | 1.85 (3.08) | 13 | 1.09 (3.62) | 11 | 5.85 (8.79) | 13 |
| Gender | ||||||||
| Male | 2.36 (3.91) | 259 | 1.95 (4.62) | 257 | 0.92 (2.04) | 245 | 5.51 (9.48) | 267 |
| Female | 2.89 (3.68) | 27 | 0.85 (1.70) | 27 | 0.25 (.53) | 24 | 4.78 (4.89) | 27 |
| Patient-rated Severity (0–100) | ||||||||
| Mild (0–30) | 1.71 (3.60) | 76 | 1.97 (7.08) | 76 | 0.70 (2.20) | 73 | 4.70 (10.67) | 79 |
| Moderate (30–70) | 2.07 (3.68) | 81 | 1.11 (1.67) | 82 | 0.49 (0.98) | 77 | 3.95 (5.69) | 85 |
| Severe (71–100) | 3.38 (4.10) | 93 | 2.68 (3.88) | 94 | 1.40 (2.38) | 88 | 7.87 (10.47) | 95 |
| Physician-rated Severity (1–5) | ||||||||
| Mild (1&2) | 1.94 (3.18) | 96 | 1.32 (2.17) | 96 | 0.66 (1.34) | 90 | 4.07 (5.29) | 99 |
| Mod (3) | 2.31 (3.30) | 55 | 2.16 (2.77) | 55 | 0.88 (2.12) | 50 | 5.40 (6.86) | 57 |
| Severe (4&5) | 4.09 (3.58) | 22 | 6.38 (13.19) | 21 | 2.29 (4.17) | 21 | 13.32 (18.32) | 22 |
| Serum Uric Acid Level | ||||||||
| <6.0 | 3.06 (4.58) | 48 | 1.85 (2.45) | 48 | 0.75 (1.97) | 44 | 5.90 (7.40) | 48 |
| 6.0–10 | 2.19 (2.66) | 105 | 2.70 (6.38) | 106 | 1.09 (2.37) | 96 | 6.05 (9.68) | 110 |
| >10 | 4.38 (5.37) | 8 | 3.88 (4.76) | 8 | 2.50 (3.21) | 8 | 10.88 (10.40) | 8 |
| Overall Severity (Median =0.024) | ||||||||
| <Median | 1.70 (3.11) | 137 | 1.15 (1.89) | 135 | 0.45 (1.41) | 128 | 3.43 (5.24) | 141 |
| >Median | 3.10 (4.26) | 136 | 2.66 (6.01) | 137 | 1.27 (2.29) | 128 | 7.48 (11.41) | 141 |
| Number of Attacks in the past year | ||||||||
| 0 | 0.54 (0.97) | 56 | 0.55 (1.49) | 56 | 0.02 (.14) | 55 | 1.22 (2.21) | 58 |
| 1–2 | 2.28 (3.57) | 88 | 1.99 (6.56) | 88 | 0.87 (1.96) | 82 | 5.26 (9.99) | 91 |
| 3–5 | 2.39 (2.88) | 84 | 1.83 (2.60) | 83 | 0.84 (1.43) | 82 | 5.43 (5.54) | 86 |
| 6–10 | 3.33 (5.64) | 24 | 1.75 (1.87) | 24 | 1.00 (1.69) | 20 | 6.33 (7.87) | 24 |
| >10 | 5.26 (6.10) | 34 | 3.82 (5.07) | 34 | 2.33 (3.71) | 30 | 12.14 (15.67) | 36 |
| Time Since Last Gout Attack | ||||||||
| <1 week | 4.42 (5.70) | 45 | 3.09 (4.47) | 47 | 2.28 (3.31) | 43 | 9.94 (13.90) | 50 |
| 1–4 weeks | 3.44 (5.01) | 52 | 2.18 (3.04) | 51 | 0.77 (1.26) | 44 | 7.00 (8.02) | 52 |
| 1–3 months | 2.15 (2.58) | 75 | 1.35 (1.96) | 75 | 0.61 (1.21) | 71 | 4.30 (4.57) | 77 |
| 4–6 months | 2.04 (3.30) | 24 | 3.83 (12.37) | 23 | 1.52 (3.30) | 23 | 8.08 (17.12) | 24 |
| 7–12 months | 1.93 (3.19) | 27 | 1.41 (1.91) | 27 | 0.54 (0.81) | 26 | 3.93 (4.70) | 27 |
| >1 yr | 0.84 (1.69) | 64 | 0.75 (1.72) | 63 | 0.11 (.41) | 63 | 1.77 (2.93) | 66 |
| Tophi | ||||||||
| Yes | 3.61 (4.07) | 44 | 3.90 (3.88) | 42 | 1.36 (3.17) | 39 | 8.82 (9.07) | 44 |
| No | 2.08 (3.16) | 119 | 1.97 (5.83) | 119 | 0.90 (1.85) | 112 | 5.14 (8.96) | 123 |
| Heart Disease | ||||||||
| Yes | 3.69 (5.73) | 70 | 1.94 (3.11) | 72 | 1.45 (2.44) | 62 | 7.59 (11.75) | 74 |
| No | 2.04 (2.99) | 209 | 1.83 (4.87) | 206 | 0.65 (1.74) | 199 | 4.74 (8.09) | 212 |
| Kidney Disease | ||||||||
| Yes | 2.94 (5.02) | 124 | 2.53 (6.20) | 123 | 1.20 (2.63) | 114 | 7.04 (12.47) | 127 |
| No | 2.03 (2.67) | 159 | 1.34 (2.22) | 158 | 0.58 (1.15) | 151 | 4.26 (5.16) | 163 |
| High Blood Pressure | ||||||||
| Yes | 2.85 (4.31) | 209 | 2.13 (5.03) | 207 | 0.98 (2.16) | 197 | 6.34 (10.27) | 215 |
| No | 1.28 (2.00) | 75 | 1.19 (2.01) | 75 | 0.45 (1.05) | 69 | 3.09 (4.19) | 76 |
| High Cholesterol | ||||||||
| Yes | 2.75 (4.16) | 168 | 1.55 (2.65) | 165 | 1.01 (1.96) | 154 | 5.74 (8.78) | 171 |
| No | 1.95 (3.43) | 116 | 2.26 (6.14) | 117 | 0.61 (1.94) | 111 | 5.04 (9.77) | 120 |
| Diabetes | ||||||||
| Yes | 3.08 (5.08) | 90 | 2.89 (7.15) | 88 | 1.29 (2.65) | 84 | 7.85 (13.82) | 93 |
| No | 2.12 (3.19) | 190 | 1.39 (2.25) | 88 | 0.64 (1.50) | 179 | 4.35 (5.60) | 194 |
Table 3.
Gout-related health care resource utilization
| Health Practitioner | % Utilizing Past Year | Number Utilizing/Total Respondents | Mean # Visits per year (SD)* |
|---|---|---|---|
| Primary Care Physician | 60.4 | 172/285 | 3.0 (3.4) |
| Nurse/Physician Assistant | 26.0 | 65/250 | 2.7 (2.5) |
| Rheumatologist | 50.7 | 145/286 | 3.7 (5.7) |
| Walk-in/Urgent Care | 23.3 | 59/253 | 2.1 (2.2) |
| Emergency Room | 20.3 | 53/261 | 2.0 (1.7) |
| Overnight Hospitalizations | 7.2 | 18/249 | 2.1 (1.4) |
| Other | 15.1 | 26/172 | 4.5 (4.7) |
| Any Utilization | 78.4 | 232/296 | 6.9 (9.8) |
Calculated for patients using particular resource for gout at least once in past year. SD, standard deviation
Our composite measure of overall gout severity was significantly associated with whether or not patients utilized each resource category, with the exception of rheumatologist utilization (OR: 2.11 to 2.59) (Table 4); however, its association with the number of times a resource was utilized was small (correlation coefficient: 0.15 to 0.19). This association was due largely to the physician-rated gout severity component of the composite measure. Patient-rated gout severity and most recent sUA level had only a small association with the frequency of resource utilization (correlation coefficient: 0.02 to 0.16). Time since last gout attack was significantly inversely associated with whether or not patients utilized each resource category (OR: 0.59 to 0.78) and had a small association with the number of times a resource was utilized (correlation coefficient: -0.13 to −0.24). Whether or not a patient had a gout attack within the past three months was strongly associated with whether or not each resource category was utilized (OR: 2.11 to 4.70). The association with frequency of primary care, emergency, and overall utilization was significant yet small (correlation coefficient: 0.18 to 0.24). Presence of tophi was strongly associated with whether or not a rheumatologist was seen (OR = 7.92) but the association with the number of primary care and overall visits for gout was small (correlation coefficient: 0.19 to 0.20). Gender was only associated significantly with whether or not a rheumatologist was seen, with females being almost five times as likely to see a rheumatologist than males (OR=4.85). It is important to note, however, that this study population was heavily male-dominated, as would be expected for gout patients. Age and comorbidity factors were not significantly related and were only weak predictors of gout-related resource utilization (correlation coefficient: 0.01 to 0.18).
Table 4.
Relationships of gout-related health care resource utilization with gout severity, demographics, gout characteristics and comorbidities
| Primary Care | Rheumatologist | Emergency/Urgent Care | Total Utilization | |
|---|---|---|---|---|
| Odds Ratioa [95% CI] p-value | Odds Ratioa [95% CI] p-value | Odds Ratioa [95% CI] p-value | Odds Ratioa [95% CI] p-value | |
|
Gout Characteristics | ||||
| Overall Gout Severity composite | 2.11** [1.46–3.05] p<.0001 | 1.35 [0.96–1.89] p=.082 | 2.59** [1.71–3.92] P<.0001 | 2.16** [1.42–3.29] P<.0001 |
| Patient-rated Gout Severity | 1.02** [1.01–1.03] p<.0001 | 1.01* [1.00–1.02] p=.043 | 1.02** [1.01–1.03] P<.0001 | 1.02** [1.01–1.04] P<.0001 |
| Physician-rated Gout Severity | 1.46* [1.02–2.08] p=.037 | 1.52* [1.08–2.14] p=.018 | 1.65* [1.12–2.42] p=.012 | 1.74* [1.12–2.70] p=.014 |
| sUA level | 1.09 [0.91–1.31] p=.357 | 0.93 [0.78–1.12] p=.442 | 1.18 [0.97–1.43] p=.092 | 1.09 [0.87–1.37] p=.443 |
| Time Since Last Attack | 0.65** [0.55–0.76] P<.0001 | 0.78** [0.67–0.91] p=.001 | 0.66** [0.55–0.79] p<.0001 | 0.59** [0.49–0.72] p<.0001 |
| Attack in the last 3 months (yes/no) | 3.48** [1.84–6.58] P<.0001 | 2.11** [1.22–3.65] p=.008 | 3.15** [1.75–5.68] P<.0001 | 4.70** [2.02–10.97] P<.0001 |
| Tophi | 1.56 [0.69–3.55] p=.290 | 7.92** [2.81–22.34] p<.0001 | 1.45 [0.64–3.31] p=.376 | 5.21* [1.13–23.92] p=.034 |
|
Demographics and Comorbidity | ||||
| Age | 1.00 [0.98–1.02] p=.892 | 1.00 [0.97–1.02] p=.496 | 0.96** [0.94–0.99] p=.003 | 0.98 [0.96–1.01] p=.215 |
| Gender | 0.99 [0.40–2.42] p=.976 | 4.85** [1.72–13.68] p=.003 | 2.11 [0.72–6.19] p=.172 | 1.02 [0.36–2.95] p=.967 |
| Heart Disease | 0.72 [0.36–1.45] p=.361 | 0.99 [0.52–1.88] p=.964 | 0.35** [0.17–0.69] p=.003 | 0.56 [0.25–1.29] p=.175 |
| Kidney Disease | 0.89 [0.52–1.52] p=.663 | 0.68 [0.40–1.15] p=.145 | 0.85 [0.48–1.50] p=.568 | 0.54 [0.29–1.03] p=.059 |
| High Blood Pressure | 0.68 [0.38–1.21] p=.191 | 0.65 [0.36–1.17] p=.151 | 0.50 [0.25–1.01] p=.054 | 0.55 [0.29–1.06] p=.072 |
| High Cholesterol | 0.58 [0.33–1.01] p=.054 | 1.57 [0.90–2.73] p=.111 | 0.70 [0.38–1.30] p=.262 | 1.07 [0.57–2.01] p=.846 |
| Diabetes | 0.84 [0.45–1.56] p=.578 | 0.87 [0.48–1.60] p=.661 | 1.06 [0.56–2.00] p=.868 | 1.07 [0.52–2.20] p=.859 |
Odds ratio whether use or not use particular health care services using logistic regression adjusted for age, gender and individual comorbidities.
Significant odds ratios are in bold-
Significant at the 0.05 level (2-tailed);
Significant at the 0.01 level (2-tailed).
Slightly more than one-third (34.8%) of patients reported using an Emergency/Urgent Care facility for gout treatment within the past year. Of patients utilizing these facilities, most did so only once (53.2%) or twice (24.5%). The number of visits for the remaining 22.3% of utilizers ranged between 3–16 visits in the past year. Table 5 presents results from the stepwise multiple regression analysis for the frequency of gout-related Emergency/Urgent Care utilization. The predictors included in the model explained 44.6% of the variation. Non-emergency/Urgent Care utilization (i.e. number of primary care physician, nurse practitioner, physician’s assistant or rheumatologist visits, and outpatient visits to other health practitioners for gout) was significantly associated with Emergency/Urgent Care utilization rate and accounted for 40.6% of the variance. History of heart disease (heart attack or failure) and sUA level were also significantly associated and accounted for an additional 3.2% and 2.5% of variance, respectively.
Table 5.
Predicting frequency of gout-related emergency department and/or urgent care utilization for patients with at least one emergency/urgent care visit (n=97) and of gout-related primary care utilization (n=264).
| B (Unstd.) | Std. Error of B | Beta (Std.) | p-value | |
|---|---|---|---|---|
| Predictors of frequency of gout-related emergency department and/or urgent care Utilizationa | ||||
| Non-Emergency/urgent Care Utilization* | 0.183 | 0.022 | 0.624 | <0.001 |
| Heart Disease | 1.176 | 0.508 | 0.176 | 0.023 |
| Recent SUA | 0.224 | 0.109 | 0.157 | 0.042 |
| Constant | −1.491 | 0.785 | n/a | 0.061 |
| Predictors of frequency of gout-related primary care utilizationb | ||||
| Rheumatologist Utilization | 0.232 | 0.048 | 0.278 | <0.001 |
| Total Number of Comorbidities | 0.428 | 0.154 | 0.160 | 0.006 |
| Overall Standardized Gout Severity | 0.791 | 0.281 | 0.163 | 0.005 |
| Constant | 1.003 | 0.416 | n/a | 0.017 |
Dependent Variable: Number of visits patients made to emergency or urgent care departments for gout over the preceding year;
Non-Emergency/urgent Care = total gout-related primary care physician, nurse practitioner, physician’s assistant and rheumatologist visits, and visits to other health practitioners for gout. Unstd, unstandardized; Std., standardized
The t-test and significance values express significance of each unstandardized B coefficient.
Dependent Variable: Number of visits patients made to a primary care (primary care physician, nurse, or physician’s assistant) for gout over the preceding year.
Patients with more comorbid conditions, more rheumatologist visits and higher overall gout severity composite score, each tended to have higher primary care utilization in multivariable-adjusted analyses (Table 5). Hence, when overall gout severity and rheumatologist utilization are controlled for, number of comorbidities still predicts a higher number of primary care visits for gout treatment.
A logistic regression performed using forward likelihood ratio selection showed that composite gout severity ratings, heart disease and non-emergency/urgent care utilization were the three most significant predictors of whether or not Emergency or Urgent Care department services were used for gout treatment (any vs. none) (Table 6). The same logistic regression performed using the backward likelihood selection method also yielded composite gout severity ratings, heart disease, and non-emergency/urgent care utilization as the top three predictors, with the addition of time since last gout attack as a fourth significant predictor (Table 6).
Table 6.
Predicting likelihood of gout-related emergency department and/or urgent care utilization (n=97)
| Beta | Std. Error | Odds Ratio | Sig. | |
|---|---|---|---|---|
| Forward likelihood ratio selection | ||||
| Overall Standardized Gout Severity | 1.579 | 0.510 | 9.590 | 0.002 |
| Heart Disease | −1.926 | 0.690 | 7.784 | 0.005 |
| Non-Emergency/urgent Care Utilization* | 0.200 | 0.069 | 8.408 | 0.004 |
| Constant | 0.089 | 0.692 | 0.016 | 0.898 |
| Backward likelihood ratio selection | ||||
| Overall Standardized Gout Severity | 1.259 | 0.545 | 5.346 | 0.021 |
| Heart Disease | −1.918 | 0.689 | 7.747 | 0.005 |
| Non-Emergency/urgent Care Utilization* | 0.186 | 0.071 | 6.895 | 0.009 |
| Time Since Last Gout Attack | −0.330 | 0.198 | 2.785 | 0.095 |
| Constant | 1.176 | 0.949 | 1.537 | 0.215 |
Dependent Variable: Whether or not patients visited emergency or urgent care departments for gout over the preceding year.
Non-Emergency/urgent Care = total gout-related primary care physician, nurse practitioner, physician’s assistant and rheumatologist visits, and visits to other health practitioners for gout. Unstd, unstandardized; Std., standardized
DISCUSSION
In our study, primary care physician visits were the most frequently cited health care resource for gout treatment and rheumatologist visits were the second most frequently used resource. Patients used each of these visit types an average of three times in the year prior to the survey. Slightly more than one-third of patients had used Emergency Room or Urgent Care facilities for their gout treatment, which is more costly than outpatient care. Our overall gout severity composite measure, physician-rated gout severity, time since a patient’s last gout attack, and occurrence of an attack in the past three months were associated with whether or not patients utilized each resource category (primary care, rheumatologist or Emergency/urgent care). Presence of tophi was associated with greater likelihood of a rheumatology visit, which is consistent with the current practice of referring patients with severe gout to the rheumatologists. Utilization of non-emergency/urgent care was a significant predictor of whether or not patients used Emergency/urgent care and the frequency of Emergency/urgent care usage. We also found that after controlling for the number of rheumatology visits and gout severity, patients with more comorbidities have more primary care visits for their gout than those with a lower number of comorbidities.
Recently, a few studies have examined the impact of gout on health care costs including medication costs and health care utilization. Population-based studies comparing patients with gout to those without gout reported significantly higher adjusted primary care clinic utilization and hospitalization rates in veterans with gout (6) and in elderly adults with gout (5). Gout patients incur higher adjusted medication costs than those without gout; among those with gout, presence of tophaceous gout was significantly associated with higher costs (4). Serum uric acid ≥9 mg/dl (4) and ≥6 mg/dl (7) has been shown to be associated with higher costs. Brook et al. reported that 0.9% of the gout patients were responsible for 20% of the gout-specific medication and prescription costs, signifying that those with higher disease load/severity consume the most resources (3). Previous studies were limited since most focused on costs, not utilization, most compared gout to non-gout populations, all used claims databases (which have inherent limitations) and none examined correlates of gout-specific health care utilization. This study was conducted due to the lack of prospective studies examining correlates of gout-related health care utilization.
Our finding of association of an overall severity composite measure and physician-rated gout severity with each type of and overall utilization is novel and interesting. These simple (and inexpensive) measures of gout severity can be easily documented by clinicians to help them identify patients who are likely high-users of resources. Creation of the severity composite measure requires only a patient perceived severity rating, physician’s perceived severity rating and most recent sUA. The association of “time since last gout attack” and “attack in past three months” with each type of and overall resource utilization is logical and suggests identification of these patients for more intensive therapy and better monitoring of their gout may reduce health care costs.
Our findings of correlates of Emergency/urgent care and primary care utilization deserve some discussion. Utilization of other health care services was the strongest correlate of emergency/urgent care, explaining almost half of the variability. This should not be surprising, since it likely represents the correlation that one might expect between different types of utilization due to other characteristics such as socio-demographics, health care access/insurance, health attitudes and behaviors. However, it also suggests that emergency/urgent care services are not solely being used as a substitute for non-emergency/urgent gout care resources, but instead are used in addition to non-emergency/urgent services by many patients. Addressing the reasons for this additional usage could help to reduce health costs in the future.
Presence of a higher number of co-morbidities was associated with higher primary care use by patients to treat their gout even when controlling for use of rheumatologists to treat gout. There may be many reasons patients require primary and specialty care for their gout: (1) drug-drug interactions due to poly-pharmacy requiring frequent clinical and laboratory monitoring of gout and limiting the use/dose of anti-gout medications; (2) medications used for comorbidity, such as diuretics for heart failure, leading to difficulty in optimally controlling gout and preventing gout flares; and (3) presence of renal failure requiring more frequent laboratory monitoring, leading to more patient visits. That higher overall and physician-rated gout severity was associated with higher primary care utilization is reassuring, since it indicates that more severe disease gets the well-deserved attention from treating physicians, primary care providers and rheumatologists.
With an increasing incidence of gout in the general population, especially in the elderly (13), and high medical comorbidity in patients with gout, we speculate that gout-related utilization is likely to increase significantly in the next few years. It is important to distinguish what proportion of the gout-related utilization is appropriate and which part is related to inappropriate treatment (under- or over-treatment) and/or poor patient compliance. We speculate that much of the emergency/urgent care utilization may be decreased by reducing recurrent acute flares of gout. Studies have shown that many interventions are effective at reducing frequency and/or severity of acute flares in patients with gout. These include maintaining target serum uric acid levels at 6 mg/dl or lower (11), taking allopurinol continuously instead of intermittently (14) and using colchicine prophylaxis when initiating allopurinol and continuing past allopurinol initiation (15–16). Further studies should examine if interventions targeting these factors can reduce gout-related utilization.
Strengths and Limitations
This is the first study of a large multi-center gout cohort investigating gout-related utilization. We examined the impact of gout severity (patient-rated, physician-rated and sUA) and comorbidities on the rate of healthcare utilization categorized into primary care, rheumatology, emergency/urgent care visits using multivariable-adjusted analysis. Our study recruited patients from arthritis or primary care clinics in three U.S. metropolitan areas. Our study has several limitations. The measures of utilization are self-reported, therefore subject to recall bias. Self-reported utilization has been shown to be a valid measure in many studies (17–20), while others found inaccuracy (21), usually under-reporting (22). Use of self-reported comorbidity may be prone to error, with the possibility of over- or under-reporting (23–29). Study findings may not be generalizable to gout patients who do not see physicians for gout or those in other healthcare settings. Our composite measure of gout severity will need further validation. However, it is quite intuitive in concept and easy to calculate. Most recent serum urate likely represents long-standing hyperuricemia in patients without a recent gout flare, but may have been low in those with a recent gout flare, which may have impacted its association with outcomes.
In summary, we report health care utilization patterns for gout and their correlates in a large well-defined multi-center cohort of gout patients. Our findings that physician-rated and overall gout severity, time since last gout attack and comorbidity are significant correlates of emergency/urgent care, primary care, rheumatologist and overall health care utilization, add to the current literature. Future studies should investigate whether we can use these measures to prospectively identify high resource-utilizers in gout populations and whether targeting this group of patients improves their quality of care, satisfaction and decreases resource utilization.
Take Home Message.
More severe gout is associated with greater gout-related utilization.
In patients with gout, greater use of non- emergent care strongly predicts emergent/urgent care utilization for gout care.
Gout patients with higher medical comorbidity have higher gout-related primary care utilization.
Acknowledgments
Grant Support: Supported by the Takeda Pharmaceutical Products, Inc., VA Research Service and the University of California, San Diego General Clinical Research Center Program, M01 RR00827, National Center for Research Resources, National Institutes of Health. D.K was also supported by a National Institutes of Health Award (NIAMS K23 AR053858-01A1) during this period. J.A.S was supported by a National Institutes of Health CTSA Award 1 KL2 RR024151-01 (Mayo Clinic Center for Clinical and Translational Research).
This work was supported in part by an investigator-initiated research grant from Takeda Pharmaceutical Products, Inc., VA Research Service and the University of California, San Diego General Clinical Research Center Program, M01 RR00827, National Center for Research Resources, National Institutes of Health.
Appendix
Appendix 1.
Additional clinical characteristics of the study population
| Number of Respondents | Mean ± SD or n (%) | |
|---|---|---|
| Weight (kg) (mean ± SD) | 293 | 95.2 kg ± 22.1 |
| Body Mass Index [BMI, n (%)] | 293 | |
| BMI < 18.5 (Underweight) | 2 (0.7%) | |
| BMI 18.5–24.9 (Normal) | 54 (18.4%) | |
| BMI 25–29.9 (Overweight) | 112 (38.2%) | |
| BMI ≥ 30 (Obese) | 125 (42.7%) | |
| Employment [n (%)] | 292 | |
| Full Time Employment | 63 (21.6%) | |
| Part Time Employment | 28 (9.6%) | |
| Unemployed/Other | 54 (18.5%) | |
| Retired | 147 (50.3%) | |
| Years Since MD Diagnosis of Gout | ||
| Mean ± SD | 286 | 13.8 years ± 12.3 |
| Median | 286 | 10.0 years |
| Interquartile Range (IQR) | 25%=4; 50%=10; 75%=23 | |
| Current Gout Medications [n (% Yes)] | 194 | |
| Patients on Allopurinol Alone | 102 (52.6%) | |
| Patients on Colchicine Alone | 36 (18.6%) | |
| Patients on Both Allopruinol and Colchicine | 57 (29.4%) | |
| Time Since Most Recent Gout Attack | 296 | |
| Less than 1 month | 102 (34.5%) | |
| Between 1 and 4 months | 77 (26.0%) | |
| Between 4 and 12 months | 51 (17.2%) | |
| Longer than 1 year | 66 (22.3%) | |
| Number of Joints Involved During an Attack (mean ± SD) | 168 | 5.2± 6.4 |
| Severity of Typical Gout Attack Pain (mean ±SD) | 160 | 6.71 ± 2.57 |
| Family History of Gout n (%)] | 284 | 103 (36.3%) |
Footnotes
Disclosure Statement: J.A.S. has received speaker honoraria from Abbott, research grants from Department of Veterans Affairs, National Institute of Health, Arthritis Foundation, University of Minnesota, Cochrane centers, Minnesota Medical Foundation, research and travel grants from Allergan, Takeda, Savient, Wyeth and Amgen and consultant fees from Savient, URL pharmaceuticals and Novartis. J.D.H. has received a research grant from TAP and Takeda pharmaceuticals and consultant fees from Regeneron. R.T. is a consultant for Takeda, Savient, EnzymeRx, Altus, BioCryst, Regeneron, Novartis, Pfizer, URL Pharma, and Proctor & Gamble and has received grants from the Research Service of the Department of Veterans Affairs and Takeda Pharmaceuticals. D.K. has received consultant fees and research grants from Takeda Pharmaceuticals. A.K. has received consultant fees from URL pharmaceuticals. All other authors have declared no conflicts of interest.
“The views expressed in this article are those of the authors and do not necessarily reflect the position or policy of the Department of Veterans Affairs.”
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Kramer HM, Curhan G. The association between gout and nephrolithiasis: the National Health and Nutrition Examination Survey III, 1988–1994. Am J Kidney Dis. 2002 Jul;40(1):37–42. doi: 10.1053/ajkd.2002.33911. [DOI] [PubMed] [Google Scholar]
- 2.Kim KY, Ralph Schumacher H, Hunsche E, Wertheimer AI, Kong SX. A literature review of the epidemiology and treatment of acute gout. Clin Ther. 2003 Jun;25(6):1593–617. doi: 10.1016/s0149-2918(03)80158-3. [DOI] [PubMed] [Google Scholar]
- 3.Brook RA, Kleinman NL, Patel PA, Melkonian AK, Brizee TJ, Smeeding JE, et al. The economic burden of gout on an employed population. Curr Med Res Opin. 2006 Jul;22(7):1381–9. doi: 10.1185/030079906X112606. [DOI] [PubMed] [Google Scholar]
- 4.Wu EQ, Patel PA, Yu AP, Mody RR, Cahill KE, Tang J, et al. Disease-related and all-cause health care costs of elderly patients with gout. J Manag Care Pharm. 2008 Mar;14(2):164–75. doi: 10.18553/jmcp.2008.14.2.164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hanly JG, Skedgel C, Sketris I, Cooke C, Linehan T, Thompson K, et al. Gout in the elderly -- a population health study. J Rheumatol. 2009 Apr;36(4):822–30. doi: 10.3899/jrheum.080768. [DOI] [PubMed] [Google Scholar]
- 6.Singh JA, Strand V. Gout is associated with more comorbidities, poorer health related quality of life and higher health care utilization in US veterans. Ann Rheum Dis. 2008 Jan 4; doi: 10.1136/ard.2007.081604. [DOI] [PubMed] [Google Scholar]
- 7.Halpern R, Fuldeore MJ, Mody RR, Patel PA, Mikuls TR. The effect of serum urate on gout flares and their associated costs: an administrative claims analysis. J Clin Rheumatol. 2009 Feb;15(1):3–7. doi: 10.1097/RHU.0b013e3181945d2c. [DOI] [PubMed] [Google Scholar]
- 8.Hirsch JD, Lee SJ, Terkeltaub R, Khanna D, Singh J, Sarkin A, et al. Evaluation of an Instrument Assessing Influence of Gout on Health-Related Quality of Life. J Rheumatol. 2008 Oct 15; doi: 10.3899/jrheum.080506. [DOI] [PubMed] [Google Scholar]
- 9.Wallace SL, Robinson H, Masi AT, Decker JL, McCarty DJ, Yu TF. Preliminary criteria for the classification of the acute arthritis of primary gout. Arthritis Rheum. 1977 Apr;20(3):895–900. doi: 10.1002/art.1780200320. [DOI] [PubMed] [Google Scholar]
- 10.Ragazzini JR, Bergen AR. A Mathematical Technique for the Analysis of Linear Systems. Proceedings of the IRE. 1954;42(11):1645–51. [Google Scholar]
- 11.Shoji A, Yamanaka H, Kamatani N. A retrospective study of the relationship between serum urate level and recurrent attacks of gouty arthritis: evidence for reduction of recurrent gouty arthritis with antihyperuricemic therapy. Arthritis Rheum. 2004 Jun 15;51(3):321–5. doi: 10.1002/art.20405. [DOI] [PubMed] [Google Scholar]
- 12.Cohen J, Cohen P, West S, Aiken L. Applied multiple regression/correlation analysis for the behavioral scienceS. 2. Hillsdale, NJ: Lawrence Erlbaum Associates; 2003. [Google Scholar]
- 13.Arromdee E, Michet CJ, Crowson CS, O’Fallon WM, Gabriel SE. Epidemiology of gout: is the incidence rising? J Rheumatol. 2002 Nov;29(11):2403–6. [PubMed] [Google Scholar]
- 14.Bull PW, Scott JT. Intermittent control of hyperuricemia in the treatment of gout. J Rheumatol. 1989 Sep;16(9):1246–8. [PubMed] [Google Scholar]
- 15.Borstad GC, Bryant LR, Abel MP, Scroggie DA, Harris MD, Alloway JA. Colchicine for prophylaxis of acute flares when initiating allopurinol for chronic gouty arthritis. J Rheumatol. 2004 Dec;31(12):2429–32. [PubMed] [Google Scholar]
- 16.Becker MA, Schumacher HR, Jr, Wortmann RL, MacDonald PA, Eustace D, Palo WA, et al. Febuxostat compared with allopurinol in patients with hyperuricemia and gout. N Engl J Med. 2005 Dec 8;353(23):2450–61. doi: 10.1056/NEJMoa050373. [DOI] [PubMed] [Google Scholar]
- 17.Clarke AE, Esdaile JM, Bloch DA, Lacaille D, Danoff DS, Fries JF. A Canadian study of the total medical costs for patients with systemic lupus erythematosus and the predictors of costs. Arthritis Rheum. 1993 Nov;36(11):1548–59. doi: 10.1002/art.1780361109. [DOI] [PubMed] [Google Scholar]
- 18.Lubeck DP, Brown BW, Holman HR. Chronic disease and health system performance. Care of osteoarthritis across three health services. Med Care. 1985 Mar;23(3):266–77. doi: 10.1097/00005650-198503000-00008. [DOI] [PubMed] [Google Scholar]
- 19.Lubeck DP, Spitz PW, Fries JF, Wolfe F, Mitchell DM, Roth SH. A multicenter study of annual health service utilization and costs in rheumatoid arthritis. Arthritis Rheum. 1986 Apr;29(4):488–93. doi: 10.1002/art.1780290405. [DOI] [PubMed] [Google Scholar]
- 20.Reijneveld SA, Stronks K. The validity of self-reported use of health care across socioeconomic strata: a comparison of survey and registration data. Int J Epidemiol. 2001 Dec;30(6):1407–14. doi: 10.1093/ije/30.6.1407. [DOI] [PubMed] [Google Scholar]
- 21.Cleary PD, Jette AM. The validity of self-reported physician utilization measures. Med Care. 1984 Sep;22(9):796–803. doi: 10.1097/00005650-198409000-00003. [DOI] [PubMed] [Google Scholar]
- 22.Roberts RO, Bergstralh EJ, Schmidt L, Jacobsen SJ. Comparison of self-reported and medical record health care utilization measures. J Clin Epidemiol. 1996 Sep;49(9):989–95. doi: 10.1016/0895-4356(96)00143-6. [DOI] [PubMed] [Google Scholar]
- 23.Bergmann MM, Byers T, Freedman DS, Mokdad A. Validity of self-reported diagnoses leading to hospitalization: a comparison of self-reports with hospital records in a prospective study of American adults. Am J Epidemiol. 1998 May 15;147(10):969–77. doi: 10.1093/oxfordjournals.aje.a009387. [DOI] [PubMed] [Google Scholar]
- 24.Fisher MA, Taylor GW, Shelton BJ, Debanne SM. Sociodemographic characteristics and diabetes predict invalid self-reported non-smoking in a population-based study of U.S. adults. BMC Public Health. 2007;7:33. doi: 10.1186/1471-2458-7-33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Manuel DG, Lim JJ, Tanuseputro P, Stukel TA. How many people have had a myocardial infarction? Prevalence estimated using historical hospital data. BMC Public Health. 2007;7:174. doi: 10.1186/1471-2458-7-174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Margolis KL, Lihong Q, Brzyski R, Bonds DE, Howard BV, Kempainen S, et al. Validity of diabetes self-reports in the Women’s Health Initiative: comparison with medication inventories and fasting glucose measurements. Clin Trials. 2008;5(3):240–7. doi: 10.1177/1740774508091749. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Rosamond WD, Sprafka JM, McGovern PG, Nelson M, Luepker RV. Validation of self-reported history of acute myocardial infarction: experience of the Minnesota Heart Survey Registry. Epidemiology. 1995 Jan;6(1):67–9. doi: 10.1097/00001648-199501000-00013. [DOI] [PubMed] [Google Scholar]
- 28.Simpson CF, Boyd CM, Carlson MC, Griswold ME, Guralnik JM, Fried LP. Agreement between self-report of disease diagnoses and medical record validation in disabled older women: factors that modify agreement. J Am Geriatr Soc. 2004 Jan;52(1):123–7. doi: 10.1111/j.1532-5415.2004.52021.x. [DOI] [PubMed] [Google Scholar]
- 29.Tisnado DM, Adams JL, Liu H, Damberg CL, Chen WP, Hu FA, et al. What is the concordance between the medical record and patient self-report as data sources for ambulatory care? Med Care. 2006 Feb;44(2):132–40. doi: 10.1097/01.mlr.0000196952.15921.bf. [DOI] [PubMed] [Google Scholar]