Abstract
Background
Aiming to align provider incentives toward improving quality and efficiency, the Center for Medicare and Medicaid Services is considering broader bundling of hospital and physician payments around episodes of inpatient surgery. Decisions about bundled payments would benefit from better information about how payments are currently distributed among providers of different perioperative services and how payments vary across hospitals.
Study Design
Using the national Medicare database, we identified patients undergoing one of four inpatient procedures in 2005 (coronary artery bypass [CABG], hip fracture repair, back surgery, and colectomy). For each procedure, price-standardized Medicare payments from the date of admission for the index procedure to 30 days postdischarge were assessed and categorized by payment type (hospital, physician, and postacute care) and subtype.
Results
Average total payments for inpatient surgery episodes varied from U.S.$26,515 for back surgery to U.S.$45,358 for CABG. Hospital payments accounted for the largest share of total payments (60–80 percent, depending on procedure), followed by physician payments (13–19 percent) and postacute care (7–27 percent). Overall episode payments for hospitals in the lowest and highest payment quartiles differed by U.S.$16,668 for CABG, U.S.$18,762 for back surgery, U.S.$10,615 for hip fracture repair, and U.S.$12,988 for colectomy. Payments to hospitals accounted for the largest share of variation in payments. Among specific types of payments, those associated with 30-day readmissions and postacute care varied most substantially across hospitals.
Conclusions
Fully bundled payments for inpatient surgical episodes would need to be dispersed among many different types of providers. Hospital payments—both overall and for specific services—vary considerably and might be reduced by incentives for hospitals and physicians to improve quality and efficiency.
Keywords: Surgery, Medicare, bundled payments
Efforts to curb the growth of health care spending in the United States, widely considered a national priority, will inevitably involve surgery. Extrapolating from our analyses of national Medicare data, costs related to procedures and other aspects of surgical care consume approximately 40 percent of all hospital and physician spending, or about U.S.$500 billion annually. Constraining growth in surgery costs will ultimately depend on slowing the growth in the number of procedures performed—over 45 million are performed annually in the United States (http://www.cdc.gov/nchs/fastats/insurg.htm). Controlling prices—payments per procedure—will also be essential. Toward this end, the Medicare Payment Advisory Commission (MedPAC) has recommended broader bundling of payments for surgical episodes, lumping reimbursements to hospitals, physicians, and other providers involved in care around a surgical episode into a single payment (Hackbarth, Reischauer, and Mutti 2008; MedPAC 2009;). The primary motivation underlying bundled payments is to align the often conflicting financial incentives of hospitals and surgeons around the common goal of coordinating care and improving quality and cost-efficiency.
Although conceptually straightforward, implementing this new reimbursement policy at the local level may be complex. Payments around inpatient surgery episodes are currently distributed among a diverse group of providers for a wide range of services. Some types of payments, including hospital payments for the index procedures (based on DRG assignments) and fees for surgeons and anesthesiologists, are obvious. The contributions of other types of payments, often for more discretionary services, may be under-appreciated, however. On the hospital side, these include outlier payments (for patients with particularly expensive hospital courses) and those related to readmissions for surgical complications. Postacute care, including both home health care and use of extended care facilities, may also contribute substantially to the overall cost of inpatient surgery.
A fuller accounting of current payments around surgical episodes would help inform the debate around bundled payments. On behalf of MedPAC Hackbarth, Reischauer, and Mutti (2008) described Medicare payments around hospitalizations for three common conditions and the extent to which payments vary across U.S. hospitals. However, this analysis focused only one type of surgical admission—coronary artery bypass surgery (CABG). It also considered only variation in payments among patients with the same DRG assignment and thus ignored variation in spending associated with hospital-level differences in how patients undergoing the same procedure are assigned to different DRG levels. Although variation in DRG distributions no doubt reflect differences in hospital case mix and procedure complexity, it may also occur as a result of different rates of postoperative complications or coding practices, both potentially leveraged by bundled payments.
In this context, we used national Medicare claims to examine payments around four expensive procedures performed commonly on the elderly. In addition to providing a more detailed description of how payments are currently dispersed, we explored the extent to which different types of payments vary across hospitals.
METHODS
Subjects and Databases
This study was based on complete Medicare claims data for a sample of patients undergoing selected inpatient procedures in 2005. Because services provided to Medicare managed care patients are not consistently captured in claims files, such patients (approximately 16 percent in 2005) were excluded from our study. We also excluded patients less than 65 years of age or over 99 and those not enrolled in both Medicare parts A and B at the time of their procedures (approximately 4 percent). Finally, to avoid skewing our accounting of payments for postacute care, we excluded the small percentage (<1 percent) of patients who were nursing home residents before surgery.
Patients undergoing surgery were identified from the inpatient file based on the presence of the appropriate procedure codes from the International Classification of Diseases, version 9. We then identified the subset of these patients represented in the 20 percent carrier (i.e., physician) files. (Given the large size of these files, CMS only releases random samples of this database.) We then linked these patients' records to other CMS files containing claims potentially relevant to the surgical episode, including the outpatient, home health, skilled nursing facility, long stay hospital, and durable medical equipment files. Although this study was based entirely on patients undergoing surgery in 2005, we used information from January 2006 for patients undergoing surgery in December 2005.
This study was based on patients undergoing the following procedures: CABG, hip fracture repair, back surgery (including discectomy, laminectomy, and fusion), and colectomy. These procedures were selected because they are common in the elderly, very expensive, and likely to be associated with substantial costs related to discretionary peri- and postoperative services. Thus, they are the types of procedures likely to be selected by MedPAC or other policy makers for episode-based payment bundling. To enhance the homogeneity of our study cohorts, patients undergoing contemporaneous valve replacement were excluded from the CABG cohort. For similar reasons, the colectomy sample was restricted to patients with codes indicating colon cancer, the most common indication for this procedure.
Determination of Payments
For each patient, we assessed actual Medicare payments, not submitted charges. We extracted payment information for all services types from the date of hospital admission for the index procedure, to 30 days from the hospital discharge date. Although somewhat arbitrary, this payment window coincides with MedPAC's recommendations. It is also reasonable on empirical grounds. Based on our analyses, total payments drop to near patients' preoperative baselines by approximately 4–6 weeks after most inpatient procedures. All payments were price-standardized using methods described by Gottlieb et al. (2010).
In assessing hospital payments, we examined those related to both the index hospitalization (DRG payment plus outlier payments when present) and readmissions occurring within 30 days of discharge. In assessing DRG payments, we used the Medicare Price Amount, which reflects the actual hospital payment amount plus any applicable patient liability amounts. Pass-through amounts, used by CMS to cover certain capital expenses, education costs, and bad debt, were extremely small for the large majority of hospitals and were not included.
Physician payments were categorized according to the nature of the service provided, not the specialty type of the physician providing it. Thus, surgeon and anesthesia payments were extracted from claims containing current procedural terminology (CPT) codes corresponding to the index procedure and anesthetic services, respectively. Physician payments for imaging and laboratory services were assigned based on the presence of CPT codes specific to those services, as defined by the Berenson–Eggers Type of Service codes (http://www.cms.hhs.gov/hcpcsreleasecodesets/20_betos.asp). Payments for all other physician services—inpatient and outpatient—were collapsed under “other medical.”
In assessing costs related to postacute care, payments related to home health care and outpatient care were obtained directly from those respective files. We used the DRG price amount in assigning payments for stays in rehabilitation hospitals, prorated to include only payments occurring within our 30-day window. Payments to skilled nursing facilities and nursing homes were determined based on per diem payments occurring within the same time window.
Finally, we examined variation in payments across hospitals. We ranked hospitals from lowest to highest in price-standardized payments for overall payments and again for each type of service. Adopting the same convention as Hackbarth and colleagues, we then compared average payments between hospitals in the lowest and highest payment quartiles, respectively. To minimize chance variation, we limited this analysis to hospitals with at least 10 cases of each type of procedure.
This study was judged exempt from human subject review by the Institutional Review Board of the University of Michigan.
RESULTS
Average total payments around inpatient surgery episodes varied from U.S.$26,515 for back surgery to U.S.$45,358 for CABG. Hospital payments accounted for the largest share of total payments for each procedure, from 60 percent with hip fracture repair to 80 percent with CABG. Physician payments accounted for 13–19 percent, depending on procedure. Payments for postacute care varied most widely, from only 7 percent with CABG to 27 percent with hip fracture repair.
As expected, DRG payments were the single largest component of both hospital and overall payments around surgical episodes (Table 1). A substantial proportion (14–32 percent) of patients undergoing the four procedures was readmitted with 30 days of discharge from the index admission. For this reason, readmissions accounted for a substantial percentage of overall payments, ranging from 6.1 percent for colectomy (U.S.$12,023 per readmission, average U.S.$1,740 for all patients) to 16.2 percent for hip fracture repair (U.S.$14,073 per readmission, average U.S.$4,454 for all patients).
Table 1.
Average Payments to Hospitals around Episodes of Four Common Inpatient Procedures
| CABG (N=18,392) | Back Surgery (N=14,892) | Hip Fracture Repair (N=34,298) | Colectomy (N=7,181) | |
|---|---|---|---|---|
| DRG payment for index hospitalization | ||||
| % with payment | 100.0 | 100.0 | 100.0 | 100 |
| Average payment, when present (U.S.$) | 31,329 | 15,487 | 11,844 | 19,484 |
| Average payment, overall (U.S.$) | 31,329 | 15,487 | 11,844 | 19,484 |
| % hospital payments/% total payments | 86.9/69.1 | 81.8/58.4 | 71.9/43.0 | 88.9/68.7 |
| Outliers | ||||
| % with payment | 7.1 | 4.7 | 1.5 | 3.9 |
| Average payment, when present (U.S.$) | 22,084 | 16,632 | 11,430 | 17,984 |
| Average payment, overall (U.S.$) | 1,559 | 783 | 168 | 696 |
| % hospital payments/% total payments | 4.3/3.4 | 4.1/3.0 | 1.0/0.6 | 3.2/2.5 |
| 30-day readmissions | ||||
| % with payment | 23.4 | 18.6 | 31.7 | 14.5 |
| Average payment, when present (U.S.$) | 13,526 | 14,294 | 14,073 | 12,023 |
| Average payment, overall (U.S.$) | 3,162 | 2,658 | 4,454 | 1,740 |
| % hospital payments/% total payments | 8.8/7.0 | 14.0/10.0 | 27.0/16.2 | 7.9/6.1 |
| Total | ||||
| Average payment, overall (U.S.$) | 36,049 | 18,928 | 16,467 | 21,920 |
| % total payments | 79.5 | 71.4 | 59.7 | 77.3 |
Based on 2005 National Medicare claims.
Of total payments around surgical episodes, only 4–13 percent (U.S.$1,248 for hip fracture repair to U.S.$3,466 for back surgery) went to the operating surgeon and less than 3 percent to anesthesiologists (Table 2). Physician payments for laboratory and imaging services accounted for less than 2 percent of total payments. Physician payments for other medical care, including inpatient consultative services, accounted for between 2.9 percent and 6.3 percent of total payments.
Table 2.
Average Payments to Physicians around Episodes of Four Common Inpatient Procedures
| CABG (N=18,392) | Back Surgery (N=14,892) | Hip Fracture Repair (N=34,298) | Colectomy (N=7,181) | |
|---|---|---|---|---|
| Surgeon | ||||
| % with payment | 98.8 | 97.0 | 96.8 | 97.5 |
| Average payment, when present (U.S.$) | 2,743 | 3,466 | 1,248 | 1,551 |
| Average payment, overall (U.S.$) | 2,712 | 3,364 | 1,208 | 1,512 |
| % physician payments/% total payments | 44.0/6.0 | 67.5/12.7 | 34.3/4.4 | 37.8/5.3 |
| Anesthesia | ||||
| % with payment | 97.2 | 97.0 | 97.4 | 97.2 |
| Average payment, when present (U.S.$) | 975 | 712 | 392 | 505 |
| Average payment, overall (U.S.$) | 948 | 690 | 382 | 491 |
| % physician payments/% total payments | 15.4/2.1 | 13.8/2.6 | 10.9/1.4 | 12.3/1.7 |
| Imaging | ||||
| % with payment | 98.9 | 91.4 | 99.2 | 78.7 |
| Average payment, when present (U.S.$) | 361 | 131 | 152 | 265 |
| Average payment, overall (U.S.$) | 357 | 120 | 150 | 209 |
| % physician payments/% total payments | 5.8/0.8 | 2.4/0.5 | 4.3/0.5 | 5.2/0.7 |
| Laboratory | ||||
| % with payment | 93.0 | 63.6 | 82.8 | 98.4 |
| Average payment, when present (U.S.$) | 105 | 75 | 57 | 286 |
| Average payment, overall (U.S.$) | 98 | 48 | 47 | 282 |
| % physician payments/% total payments | 1.6/0.2 | 1.0/0.2 | 1.3/0.2 | 7.0/1.0 |
| Other medical | ||||
| % with payment | 99.3 | 83.3 | 99.7 | 95.3 |
| Average payment, when present (U.S.$) | 2,056 | 915 | 1,736 | 1,581 |
| Average payment, overall (U.S.$) | 2,042 | 762 | 1,731 | 1,508 |
| % physician payments/% total payments | 33.2/4.5 | 15.3/2.9 | 49.2/6.3 | 37.7/5.3 |
| Total | ||||
| Average payment, overall (U.S.$) | 6,157 | 4,985 | 3,518 | 4,001 |
| % total payments | 13.6 | 18.8 | 12.8 | 14.1 |
Based on 2005 National Medicare claims.
Payments for postacute care varied widely, ranging from U.S.$2,431 (colectomy) to U.S.$7,585 (hip fracture repair) (Table 3). Between 29 percent and 50 percent of patients undergoing the four procedures received home health care afterward, adding U.S.$388–718 to the average bill. Average payments to skilled nursing facilities were of comparable magnitude for most procedures, but particularly high for hip fracture repair (U.S.$5,219 per patient overall).
Table 3.
Average Payments for Postacute Care around Episodes of Four Common Inpatient Procedures
| CABG (N=18,392) | Back Surgery (N=14,892) | Hip Fracture Repair (N=34,298) | Colectomy (N=7,181) | |
|---|---|---|---|---|
| Outpatient care | ||||
| % with payment | 56.1 | 33.7 | 40.8 | 43.4 |
| Average payment, when present (U.S.$) | 426 | 235 | 418 | 414 |
| Average payment, overall (U.S.$) | 239 | 79 | 171 | 180 |
| % postacute care payments/% total payments | 7.6/0.5 | 3.0/0.3 | 2.2/0.6 | 7.4/0.6 |
| Home health | ||||
| % with payment | 50.4 | 28.8 | 33.0 | 29.2 |
| Average payment, when present (U.S.$) | 1,425 | 1,728 | 1,526 | 1,331 |
| Average payment, overall (U.S.$) | 718 | 498 | 504 | 388 |
| % postacute care payments/% total payments | 22.8/1.6 | 19.1/1.9 | 6.6/1.8 | 16.0/1.4 |
| Skilled nursing | ||||
| % with payment | 17.5 | 15.6 | 69.5 | 21.8 |
| Average payment, when present (U.S.$) | 5,323 | 5,331 | 7,510 | 5,625 |
| Average payment, overall (U.S.$) | 931 | 829 | 5,219 | 1,227 |
| % postacute care payments/% total payments | 29.5/2.1 | 31.9/3.1 | 68.9/18.9 | 50.5/4.3 |
| Rehabilitation | ||||
| % with payment | 2.9 | 5.5 | 8.1 | 0.8 |
| Average payment, when present (U.S.$) | 13,190 | 13,165 | 14,887 | 15,423 |
| Average payment, overall (U.S.$) | 380 | 727 | 1,203 | 120 |
| % postacute care payments/% total payments | 12.1/0.8 | 27.9/2.7 | 15.9/4.4 | 4.9/0.4 |
| Nursing homes | ||||
| % with payment | 2.6 | 0.8 | 1.7 | 1.4 |
| Average payment, when present (U.S.$) | 31,572 | 25,751 | 23,215 | 29,142 |
| Average payment, overall (U.S.$) | 814 | 195 | 396 | 406 |
| % postacute care/% total payments | 25.8/1.8 | 7.5/0.7 | 5.2/1.4 | 16.7/1.4 |
| Hospice | ||||
| % with payment | 0.2 | 0.2 | 1.7 | 1.6 |
| Average payment, when present (U.S.$) | 878 | 1,301 | 1,381 | 2,068 |
| Average payment, overall (U.S.$) | 1 | 2 | 24 | 34 |
| % postacute care/% total payments | 0.0/0.0 | 0.1/0.0 | 0.3/0.1 | 1.4/0.1 |
| DME | ||||
| % with payment | 29.7 | 40.5 | 34.7 | 25.3 |
| Average payment, when present (U.S.$) | 229 | 671 | 201 | 303 |
| Average payment, overall (U.S.$) | 68 | 272 | 70 | 77 |
| % post-acute care/% total payments | 2.2/0.1 | 10.4/1.0 | 0.9/0.3 | 3.2/0.3 |
| Subtotal for postacute care | ||||
| Average payment, overall (U.S.$) | 3,152 | 2,602 | 7,585 | 2,431 |
| % total payments | 6.9 | 9.8 | 27.5 | 8.6 |
Based on 2005 National Medicare claims.
Overall episode payments between hospitals in the lowest and highest payment quartiles differed by U.S.$16,668 for CABG, U.S.$18,762 for back surgery, U.S.$10,615 for hip fracture repair, and U.S.$12,988 for colectomy (Figure 1). With the exception of hip fracture repair (which is associated with a single DRG level), differences in DRG assignment and thus payments related to the index hospitalization accounted for the single largest share of variation in payments. Differences in payments for readmissions accounted for at least U.S.$3,000 in average payments between the lowest and highest cost hospitals. Differences in payments for physician services and postacute care were substantial but accounted for a smaller proportion of variation in average payments across hospitals.
Figure 1.
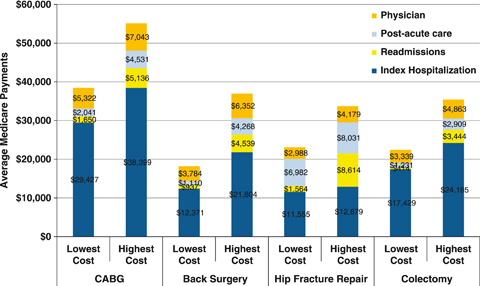
Differences in Price-Adjusted Medicare Payments around Episodes of Four Different Types of Inpatient Procedures between Hospitals in the Lowest and Highest Quartiles of Overall Payments. Based on 2005 National Medicare Data
DISCUSSION
Although hospitals have long received a fixed amount for a given hospital admission (based on DRG assignment), this mechanism alone provides inadequate incentives for improving quality and cost-efficiency with inpatient surgery. Hospitals pay little penalty for poor quality, as patients with adverse outcomes get “bumped up” to higher paying DRGs or trigger outlier payments. Costs associated with adverse outcomes get shifted to settings for which payments are not bundled, such as readmissions and postacute care. Finally, the current prospective payment system fails to align incentives between hospitals and their physicians, who continue to be paid for each unit of service and remain largely shielded from the financial consequences of their quality of care or utilization decisions. Under a fully bundled payment system, however, hospitals, surgeons, and all other providers involved in treating patients during and after inpatient surgery would share a single lump sum payment. All would have “skin the game,” sharing in the higher margins associated with uneventful, cost-efficient surgical care (Dimick et al. 2006), but suffering financially from poor outcomes and excess utilization.
Bundled payments around inpatient surgery are not a brand new idea. Over 25 years ago, the Texas Heart Institute began charging a single lump sum for CABG (Miller 2009). Geisinger Health System followed suit in 2007, receiving considerable media attention (Abelson 2007). For organ transplantation, similar “case rate” payments have been common among private payers for several years. In 2008, the MedPAC made several recommendations aimed a charting a path toward broader implementation of bundled payments around hospital episodes, including surgical admissions (Hackbarth, Reischauer, and Mutti 2008). These include providing hospitals and physicians with relevant information about how their cost per episodes compare with those of their peers. Second, MedPAC recommended that payments be reduced for hospitals with high risk-adjusted readmission rates for selection conditions. Finally, it recommended that Congress initiate a pilot test of bundled payments for a small number of conditions involving hospitalization, which is now underway.
The results of our study suggest several types of payments associated with inpatient surgery that might be leveraged by bundled payments. Hospital payments not only accounted for the largest share of overall payments but also comprised the largest source of variation in payments across hospitals. Variation associated with payments for index hospitalization, outliers, and 30-day readmissions were considerable for each of the four procedures studied. To the extent that such payments are strongly associated with patients with adverse outcomes and hospital quality (Baser et al. 2009), bundled payments should provide strong incentives toward quality improvement. Echoing the results of the MedPAC analysis, payments for postacute care were substantial and varied widely across hospitals. Such payments would be reduced by incentives for both minimizing postoperative complications and avoiding the use of home health care and extended care facilities in patients who do not truly require them.
Although our analysis identifies areas of variation and services requiring further scrutiny, it does not identify how much savings might be achieved by episode-based bundled payments for inpatient surgery. Because hospital-specific sample sizes were limited, hospital payments—both overall and for specific types of payments—will vary by chance alone. Because claims data provided limited clinical detail for risk adjustment, some of the variation in hospital payments observed in this analysis are no doubt attributable to differences in case mix. Finally, we made no attempt to link payment levels to patient outcomes. Thus, we can make no inference about the extent to which variation in hospital payments reflects underuse or overuse of specific services.
Implementation of bundled payments will be associated with numerous challenges. In addition to contentiousness around how bundled payments are divvied up among the many providers involved in a surgical episode, there will be considerable gray area in determining which services go in the bundle. For example, readmission for a complication unambiguously related to the operation (e.g., surgical site infection) would clearly be bundled. But what about patients readmitted 3 weeks after CABG with pneumonia or congestive heart failure, conditions that might have occurred in the absence of surgery? Second, bundled payments may provide incentives for hospitals and providers to skimp on necessary care, for example, home health care in patients who really need it. Hospitals could minimize investments in resources associated with safer surgery (e.g., quality and quantity of nursing staffing, intensivist-managed ICUs) or better long-term outcomes (e.g., more expensive but superior joint prostheses) (Aiken et al. 2002; Pronovost et al. 2002;). The need for safeguards against such unintended consequences is widely recognized, but whether existing quality measures and monitoring systems are sufficient for this task remains a matter of debate.
As efforts to bundle payments for surgical episodes gain momentum, hospitals and physicians should be prepared. Hospitals should implement better systems for monitoring, benchmarking, and improving their quality and cost-efficiency with inpatient surgery. Physicians, the primary drivers of utilization, should redouble their efforts to eliminate clinical waste—practices that generate additional expense at little value to patients. Hospitals and physicians will need to collaborate on strategies for enhancing care coordination as surgical patients leave the hospital. For their part, payers and policy makers will need to recognize that improving technical quality and cost-efficiency with inpatient surgery is only a start. More “upstream” strategies aimed at reducing unwanted variation in the use of surgery will also be essential in improving outcomes and controlling costs with surgical care.
Acknowledgments
Joint Acknowledgment/Disclosure Statement: This work was supported by funding from the National Institute on Aging (P01AG019783-07S1).
Disclosures: None.
Disclaimers: None.
Supporting Information
Additional supporting information may be found in the online version of this article:
Appendix SA1: Author Matrix.
Please note: Wiley-Blackwell is not responsible for the content or functionality of any supporting materials supplied by the authors. Any queries (other than missing material) should be directed to the corresponding author for the article.
REFERENCES
- Abelson R. “In Bid for Better Care, Surgery with a Warranty.”New York Times 2007: A1.
- Aiken LH, Clarke SP, Sloane DM, Sochalski J, Silber JH. Hospital Nurse Staffing and Patient Mortality, Nurse Burnout, and Job Dissatisfaction. Journal of American Medical Association. 2002;288(16):1987–93. doi: 10.1001/jama.288.16.1987. [DOI] [PubMed] [Google Scholar]
- Baser O, Fan Z, Dimick JB, Staiger DO, Birkmeyer JD. Outlier Payments for Cardiac Surgery and Hospital Quality. Health Affairs. 2009;28:1154–60. doi: 10.1377/hlthaff.28.4.1154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dimick JB, Weeks WB, Karia RJ, Das S, Campbell DAJ. Who Pays for Poor Surgical Quality? Building a Business Case for Quality Improvement. Journal of the American College of Surgeons. 2006;202:933–7. doi: 10.1016/j.jamcollsurg.2006.02.015. [DOI] [PubMed] [Google Scholar]
- Gottlieb DJ, Zhou W, Sung Y, Sutherland JM, Andrews K, Skinner JS. Adjusting Medicare Expenditures for Regional Differences in Prices. Medical Care. 2010 (in press) [Google Scholar]
- Hackbarth JD, Reischauer R, Mutti A. Collective Accountability for Medical Care—Toward Bundled Medicare Payments. New England Journal of Medicine. 2008;359:3–5. doi: 10.1056/NEJMp0803749. [DOI] [PubMed] [Google Scholar]
- Medicare Payment Advisory Commission (MedPAC) 2009. Report to the Congress: Improving Incentives in the Medicare Program” [accessed on September 25, 2009]. Available at http://www.medpac.gov/documents/Jun09_EntireReport.pdf.
- Miller HD. From Volume to Value: Better Ways to Pay for Health Care. Health Affairs. 2009;28:1418–28. doi: 10.1377/hlthaff.28.5.1418. [DOI] [PubMed] [Google Scholar]
- Pronovost PJ, Angus DC, Dorman T, Robinson KA, Dremsizov TT, Young TL. Physician Staffing Patterns and Clinical Outcomes in Critically Ill Patients: A Systematic Review. Journal of the American Medical Association. 2002;288(17):2151–62. doi: 10.1001/jama.288.17.2151. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


