Abstract
The importance of X chromosome in the aetiology of premature ovarian failure (POF) is well-known but in many cases POF still remains idiopathic. Chromosome aneuploidy increase is a physiological phenomenon related to aging, but the role of low-level sex chromosome mosaicism in ovarian function is still undiscovered. Standard cytogenetic analysis was carried out in a total of 269 patients affected by POF: 27 chromosomal abnormalities were identified, including X chromosome and autosomal structural and numerical abnormalities. In 47 patients with 46,XX karyotype we performed interphase FISH using X alpha-satellite probe in order to identify X chromosome mosaicism rate. Aneuploidy rate in the patient group was significantly higher than the general population group. These findings underline the importance of X chromosome in the aetiology of POF and highlight the potential role of low-level sex chromosome mosaicism in ovarian aging that may lead to a premature onset of menopause.
1. Introduction
The increase of chromosome aneuploidy in human lymphocytes with aging has been described since early 1960s [1, 2]. Numerous reports confirmed the observations of Jacobs and colleagues and showed that hypodiploidy increases with age and is more common than hyperdiploidy [3–6]. Subsequent studies on metaphase spreads from peripheral blood lymphocytes demonstrated that there was a preferential loss of X and Y chromosomes in female and male, respectively [7–10], suggesting that loss of sex chromosomes follows an upward trend according to aging. An increase in micronucleus formation with age has been highlighted in many studies and in particular a high overrepresentation of the X chromosome in lymphocyte micronuclei of women [6, 11–14].
Premature ovarian failure (POF, OMIM 311360) is defined as the cessation of ovarian function before the age of 40, associated with elevated gonadotropins serum levels (FSH ≥ 40 UI/l) and affects at least 1%–3% of women of reproductive age [15]. The aetiology of POF is highly heterogeneous including genetic, autoimmune, metabolic and infectious causes, but in most cases the aetiology is still unknown [16, 17]. The most common genetic causes of POF are X chromosome abnormalities [18, 19], ranging from numerical defects, deletions, X-autosome translocations, and isochromosomes [17]. Turner syndrome, associated to X monosomy, leads to ovarian dysgenesis and accelerated follicular atresia, showing that two intact X chromosomes are essential for the maintenance of ovarian function as many genes, probably involved in ovarian function, escape X inactivation and are required for a normal ovarian development and maintenance [16, 20–22]. On the other hand, X trisomy seems to be related to ovarian dysfunction as 47,XXX women might experience oligomenorrhea, secondary amenorrhea, and early menopause [23]. Moreover the role of low-level sex chromosome mosaicism in ovarian function is still unknown, in most cases they escape diagnosis because they do not seem to cause any phenotypic effect [24, 25].
The aim of this work is to carry out a study on a group of 269 patients affected by POF, through a cytogenetic investigation, in order to identify chromosomal abnormalities. Moreover, we assessed an analysis on X chromosome aneuploidy, by means of FISH on interphase nuclei, to evaluate low-level sex chromosome mosaicism rate, trying to understand if there is a correlation between advanced and increased loss of X chromosome and POF.
2. Materials and Methods
2.1. Clinical Population
A total of 269 patients affected by POF referred to genetic laboratory for conventional cytogenetic analysis. A subpart of this case group has been already published in previous works by Vegetti et al. (1998); Tibiletti et al. (1999) and Marozzi et al. (2000) [26–28]. In this study all of the patients had the cessation of menses for a duration of 6 months or longer, with FSH levels ≥ of 40 IU/l, before or at the age of 40 (POF1), or between the age of 41 and 45 years (POF2). Also patients affected by primary amenorrhea were included in the study group, as this clinical condition can be considered the most severe cause of ovarian insufficiency [29, 30]. These patients did not show any typical features of Turner syndrome. All of the patients underwent a complete clinical assessment, including complete medical and gynaecological history, in order to exclude any other related pathology. Informed consent was obtained from all participants.
The general population group was composed by 357 uncultured female amniocytes derived from routinely diagnostic procedures, in order to establish the best unbiased reference group. All foetuses showed normal female karyotype after culture using standard cytogenetic techniques.
2.2. Conventional Cytogenetics
Metaphase-chromosome spreads were obtained from phytohaemagglutinin-stimulated peripheral blood lymphocytes using standard methods. The chromosomes were QFQ-banded using quinacrine mustard, and slides were mounted in McIlvaine buffer. A range of 30–50 cells were analyzed for karyotype following the guidelines of the International System for Chromosome Nomenclature 2009 (ISCN 2009) with the exclusion of mosaicism at 10%–6% grade, with 95% confidential level [31].
2.3. FISH Analysis on Interphase Nuclei
FISH analysis on interphase nuclei from lymphocytes was assessed on patients (n = 47) with normal constitutional karyotype and on uncultured amniocytes. The mean age of the patients at the time of the study was 34 years (range 12–45). FISH study was performed using alpha satellite probes of chromosomes X, Y, and 18 (AneuVysion Multicolor DNA Probe Kit, Vysis, Abbott Molecular) and performed according to the manufacturer's instructions. Chromosome 18 centromeric probe was used as reference signal in order to evaluate hybridization efficiency. A range of 40–210 nuclei was analyzed for each case. only monosomic and trisomic cells for X chromosome were taken into account to determine the aneuploidy rate, since other anomalous categories are small and so irrelevant [32].
2.4. Statistical Analysis
χ2 test was carried out on raw data using a Microsoft Excel spreadsheet (Microsoft Corporation, Redmond, WA). Data analysis between the two groups analyzed was considered significant, setting a threshold equal to P < .05.
3. Results
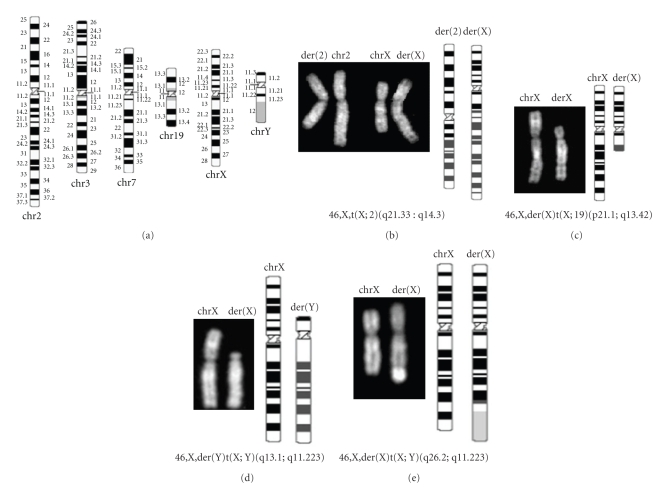
High-resolution cytogenetic analysis (QFQ banding) of peripheral blood lymphocytes from 269 patients revealed 27 chromosomal abnormalities (Table 1 and Figure 1). There were 13 nonmosaic X chromosome structural abnormalities (48.2% of detected abnormalities), including X-autosome translocations, X;Y translocations, Xq deletions, and pseudodicentric chromosomes. The 46,X,der(X)t(X;Y)(q26.2;q11.223) was a maternal inherited translocation and the mother ceased her menses at 40 years of age. The 46,X,der(X)t(X;19)(p21.1;13.42) case is a maternal inherited translocation, but the sister of this patient, who has inherited the same aberration is not affected by POF [33]. X chromosome was also involved in 3 (11.1%) cases of 45,X mosaic with the other cell line characterized by a pseudodicentric X chromosome. 6 (22.2%) patients showed X chromosome aneuploidy, in particular one patients was nonmosaic 47,XXX, one patient nonmosaic 45,X, 3 patients were 45,X/46,XX mosaic and one patient was 46,XX/47,XXX mosaic. In addition, 3 (11.1%) autosomal structural abnormalities were identified, one involving chromosomes 4 and 5 and a patient was mosaic for an isochromosome 9p. The patient with the 46,XX,t(3;7)(q23;p12) karyotype was characterized by primary amenorrhea and bilateral euryblepharon. The chromosome 3 breakpoint fell under the FOXL2 locus and she was not affected by the blepharophimosis-ptosis-epicanthus inversus syndrome. Autosomal numerical abnormalities were found in 2 patients (7.4%) including a 47,XX,+21 case and a 46,XX/47,XX+18 mosaic case successively described by Bettio et al. (2003) [34].
Table 1.
Summary of the chromosomal abnormalities found in the POF patient group.
| X chromosome structural abnormalities | nonmosaic | 46,X,t(X;2)(q21.33;q14.3) |
| nonmosaic | 46,X,der(X)t(X;9)(q21.33;p22.3)* | |
| nonmosaic | 46,X,der(X)t(X;19)(p21.1;13.42)# | |
| nonmosaic | 46,X,der(X)t(X,X)(q21.3;p21)* | |
| nonmosaic | 46,X,del(X)(q21.2→qter)* | |
| nonmosaic | 46,X,del(X)(q22.3→q27)* | |
| nonmosaic | 46,X,del(X)(q26.2→qter)* | |
| nonmosaic | 46,X,del(X)(p21→pter?) | |
| nonmosaic | 46,X,del(X)(p21.2) | |
| nonmosaic | 46,X,psudic(X)(q10;q10) | |
| nonmosaic | 46,X,del(X)(q21.1;q21.3) | |
| nonmosaic | 46,X,der(Y)t(X;Y)(q13.1;q11.223)† | |
| nonmosaic | 46,X,der(X)t(X;Y)(q26.2;q11.223) | |
| mosaic | 46,X,psudic(X)(q23;q23)[75]/45,X[25] | |
| mosaic | 45,X[97]/46,X,psudic(X)(q22;q22)[3]* | |
| mosaic | 45,X[29]/46,X,der(X)t(X;X)(q21.2;p22.33)[47] | |
| X chromosome numerical abnormalities | nonmosaic | 47,XXX |
| nonmosaic | 45,X | |
| mosaic | 46,XX[99]/45(X)[24] | |
| mosaic | 46,XX[96]/47,XXX[4] | |
| mosaic | 46,X[96]/45,X[4] | |
| mosaic | 46,X[96]/45,X[4] | |
| Autosomal structural abnormalities | nonmosaic | 46,XX,t(4;5) |
| nonmosaic | 46,XX,t(3;7)(q23;p12) | |
| mosaic | 47,XX,+i(9)(p10)[72]/46,XX[28] | |
| Autosomal numerical abnormalities | nonmosaic | 47,XX,+21 |
| mosaic | 46,XX[54]/47,XX+18[36]§ | |
*Marozzi et al. (2000) [28]; #Maraschio and Fraccaro (1983) [33]; §Bettio et al. (2003) [34]; †Lissoni et al. (2009) [35]. Square brackets, placed after the karyotype description, are used to designate the absolute number of cells in each clone, as stated by the International System for Human Cytogenetic Nomenclature 2009.
Figure 1.
Conventional cytogenetic analysis. (a) Ideograms of the normal chromosomes (550-band level). (b)–(f) Chromosomal abnormalities found in 5 patients affected by POF. Partial Q-banding karyotype on the left and ideograms of derivative chromosome on the right.
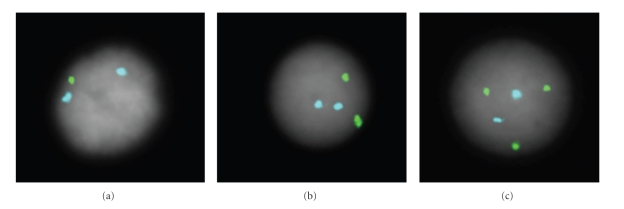
The distribution of aneuploidy rate for the patients and reference group is given in Tables 2 and 3. FISH analysis on interphase nuclei from amniocytes on the general population group revealed X chromosome monosomy in 2.7% (range 0%–11.4%) of cases and triple X signal in 0.6% (range 0%–6.1%) of cells. POF patient group showed higher aneuploidy values than reference group, in particular the percentage of cells with only one detectable signal was 7.5% (range 2.0%–19.2%), while a triple X chromosome signals were found in 3.3% (0%–12%) of cells. All these data were referred to cells with 2 visible 18 chromosome signals in order to evaluate only the cells with right hybridization efficiency. We established three 18:X categories and in detail: (i) 2:1 (two 18 signals and one X signal), (ii) 2:2, and (iii) 2:3 (Figure 2). All the cells that did not fall within these three categories were classified as “other” and their percentage was 5.1% and 4.8% for the reference and patient groups, respectively.
Table 2.
Detailed list of 18:X chromosome signals found in the patient group.
| Case no. | Diagnosis | Age at menopause | Number of signals (18:X) | Other | Total | ||
|---|---|---|---|---|---|---|---|
| 2: 1 | 2:2 | 2:3 | |||||
| 1 | POF2-FAM2 | 45 | 5 | 51 | 5 | 0 | 61 |
| 2 | PA | / | 7 | 54 | 3 | 0 | 64 |
| 3 | POF1-FAM2 | 40 | 11 | 69 | 10 | 0 | 90 |
| 4 | POF1 | 27 | 6 | 86 | 8 | 0 | 100 |
| 5 | POF1 | 33 | 13 | 99 | 7 | 0 | 119 |
| 6 | POF2 | 42 | 16 | 82 | 2 | 0 | 100 |
| 7 | POF1-FAM2 | 36 | 3 | 138 | 9 | 0 | 150 |
| 8 | PA-FAM1 | / | 12 | 56 | 11 | 20 | 99 |
| 9 | POF2-FAM1 | 41 | 7 | 81 | 3 | 9 | 100 |
| 10 | POF1-FAM2 | 35 | 16 | 72 | 3 | 8 | 99 |
| 11 | POF1-FAM1 | 34 | 12 | 76 | 3 | 8 | 99 |
| 12 | POF1 | 12 | 10 | 74 | 9 | 8 | 101 |
| 13 | POF2 | 42 | 17 | 74 | 2 | 11 | 104 |
| 14 | POF1-FAM1 | 33 | 8 | 72 | 3 | 13 | 96 |
| 15 | POF1-FAM1 | 38 | 19 | 62 | 3 | 15 | 99 |
| 16 | PA | / | 15 | 74 | 2 | 9 | 100 |
| 17 | POF1 | 32 | 5 | 83 | 2 | 11 | 101 |
| 18 | POF1 | 35 | 11 | 75 | 4 | 10 | 100 |
| 19 | POF1 | 37 | 10 | 74 | 6 | 9 | 99 |
| 20 | POF1-FAM1 | 25 | 4 | 88 | 6 | 2 | 100 |
| 21 | POF1 | 40 | 6 | 89 | 1 | 4 | 100 |
| 22 | POF1-FAM1 | 37 | 10 | 76 | 6 | 8 | 100 |
| 23 | POF1 | 34 | 6 | 32 | 8 | 54 | 100 |
| 24 | POF1-FAM2 | 34 | 4 | 35 | 6 | 5 | 50 |
| 25 | POF1 | 37 | 6 | 80 | 10 | 4 | 100 |
| 26 | POF1-FAM1 | 18 | 9 | 87 | 4 | 5 | 105 |
| 27 | POF1-FAM1 | 34 | 12 | 176 | 6 | 14 | 208 |
| 28 | POF1 | 30 | 11 | 167 | 0 | 6 | 184 |
| 29 | POF1-FAM2 | 35 | 16 | 167 | 5 | 12 | 200 |
| 30 | POF1 | 34 | 13 | 168 | 6 | 7 | 194 |
| 31 | POF1 | 27 | 9 | 180 | 7 | 3 | 199 |
| 32 | POF1 | 40 | 14 | 183 | 8 | 2 | 207 |
| 33 | POF1 | 40 | 6 | 190 | 4 | 3 | 203 |
| 34 | POF1-FAM1 | 40 | 13 | 182 | 4 | 5 | 204 |
| 35 | POF2 | 41 | 15 | 177 | 5 | 7 | 204 |
| 36 | POF1 | 26 | 12 | 182 | 4 | 5 | 203 |
| 37 | POF2 | 44 | 12 | 188 | 2 | 2 | 204 |
| 38 | POF1-FAM2 | 30 | 10 | 187 | 4 | 4 | 205 |
| 39 | POF1-FAM2 | 33 | 4 | 176 | 8 | 14 | 202 |
| 40 | PA | / | 23 | 177 | 2 | 3 | 205 |
| 41 | PA | / | 12 | 192 | 2 | 2 | 208 |
| 42 | POF1-FAM1 | 38 | 12 | 192 | 1 | 4 | 209 |
| 43 | POF1 | 38 | 13 | 191 | 5 | 5 | 214 |
| 44 | POF1-FAM1 | 18 | 10 | 190 | 2 | 3 | 205 |
| 45 | POF1 | 38 | 15 | 181 | 6 | 7 | 209 |
| 46 | POF1-FAM1 | 17 | 15 | 185 | 3 | 3 | 206 |
| 47 | POF1-FAM1/2 | 31 | 17 | 184 | 4 | 5 | 210 |
| % | 7.4 | 84.4 | 3.3 | 4.8 | |||
POF1: menopause before or at the age of 40; POF2: menopause between 41 and 45 years of age; PA: primary amenorrhea; FAM1: at least one relative with POF1; FAM2: at least one relative with POF2.
Table 3.
FISH analysis on interphase nuclei data and statistical analysis.
| Number of signals (18:X) | |||||
|---|---|---|---|---|---|
| 2:1 | 2:2 | 2:3 | Other | Total | |
| Patients (n = 47) | 512 (7.5%) |
5754 (84.4%) |
224 (3.3%) |
329 (4.8%) |
6819 |
| Reference group (n = 357) | 596 (2.7%) |
20020 (91.5%) |
139 (0.6%) |
1121 (5.1%) |
21876 |
|
P-value* patients versus reference group |
.001 | .001 | .001 | .161 | / |
*χ2 test.
Figure 2.
FISH analysis on interphase nuclei. FISH was performed using alpha satellite probes of X (green) and 18 (aqua) chromosomes. The images show the three different categories of signals detected: (a) X monosomy (two 18 signals and one X signal); (b) X disomy and (c) X trisomy.
X chromosome aneuploidy comparison of raw data between the two groups by the means of statistical analysis using the χ2 test for variance showed a significant difference between the data distribution of the two groups (P < .001). Interestingly, there was no difference in the distribution of so-called “other” signals, so the difference of X chromosome aneuploidy between the two groups can not be attributed to different signal dispersion (Table 3).
4. Discussion
Cytogenetic analysis on blood lymphocytes derived from POF patients is an important tool in the detection of cytogenetic abnormalities that lead to premature ovarian insufficiency. In this study we identified 27 chromosomal abnormalities out of 269 cases of POF occurred to our attention. Cytogenetic findings include X chromosome and autosomal structural and numerical abnormalities. Our data show a prevalence of X structural abnormalities (16 chromosomal abnormalities out of 27 found, equal to 59.3%), highlighting the importance of X chromosome in ovarian function and POF aetiology as described in the literature [18, 19]. Conventional cytogenetic analysis through QFQ banding is a powerful tool for a first round of screening, but a wide range of POF cases remains defined as idiopathic. Some of these cases may be explained by FRAXA premutation or mutations in BMP15 or inhibin alpha gene [36–38] but a large group of cases still remains with unknown cause.
Turner syndrome is the chromosomal disorder most commonly associated with POF, but the correlation between ovarian function and karyotype is less clear [39, 40]. Nevertheless, the highest number of follicles were found in subjects with mosaic Turner syndrome and, above all, in subjects with the lowest percentage of cells with the 45,X karyotype [41]. These data strengthen the importance of X chromosome in ovarian function, showing that a double dose of some genes located on the X chromosome is essential in ovary maintenance, preventing follicle apoptosis and atresia [22]. Evaluating the implication of 45,X low level mosaicism in POF patients could give some clues in understanding the role of low level sex chromosome mosaicism in ovarian function even if the precise role is still unknown [24, 25].
In order to evaluate X chromosome aneuploidy we performed FISH analysis using alpha satellite probes on interphase cells because the exclusive analysis of metaphase chromosome may provide only partial information since the analysis is restricted to a specific type of cycling cells and in this way nondividing cells would remain undetected [42]. Moreover, FISH analysis on interphase cells is a sensitive method for detecting low-level sex chromosome mosaicism and also avoids artifacts and problems that may be associated to metaphase chromosome preparations [24, 43]. Indeed, metaphase chromosome spreads only allow the exclusion of 10 to 6% of mosaicism at confidence level of 95% [31] while the detection of low-level mosaicism increases from 30%–40% of cases to 74% using standard karyotyping and molecular techniques (FISHs), respectively [39].
Many reports describe the increase of X chromosome aneuploidy with aging and that the increasing age-related loss of sex chromosome loss associates with a higher level of micronuclei formation [6, 10, 13, 14, 33]. Instead, few works try to correlate X chromosome loss and POF [24, 25, 44] or at most, it is possible to find some studies that are more general and amenorrhea or aneuploidy only represent a secondary aspects [45, 46].
We studied a group of 47 POF patients with normal karyotype among our case group, using interphase FISH analysis, in order to detect low-level X chromosome mosaicism and to understand if there is a correlation between increased rate of sex chromosome aneuploidy and POF condition.
The identification of the suitable reference group is tricky both for the type of disorder itself (POF) and the kind of analysis (X chromosome aneuploidy). The study on the impact of X chromosome mosaicism on fertility is very difficult to assess due to the lack of a normal fertile reference group [47]. In the literature, the rate of X monosomy and aging has already been determined by several works [10, 25, 48] and so we decided to use a new reference group based on the most possible random and unbiased group. Thus we established a general population group composed by uncultured amniocytes derived from routinely diagnostic procedures and analyzed during the same period of POF patients. This group can be considered a sort of rational reference group (a general population) as, in this specific case, a real reference group can not be formed, due to the characteristics of the disease itself: POF can occur till the age of 40(POF1)-45(POF2) and does not show any early biochemical or phenotypic signal, furthermore using a general female population, other time-related variables should be considered, such as personal habits or occupational exposure. Thus, an age-matched female group could determine a pre-established bias [49]. Moreover, women with a regular ovarian function normally cease their menses between 45 and 55 years of age and so their lymphocytes are already predisposed to X chromosome aneuploidy as it is a physiological phenomenon related to aging [50].
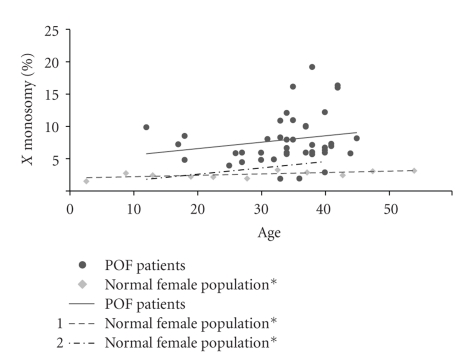
In this study we report a higher percentage of X aneuploidy rate in the POF patient group than in the general population group and we found also that the percentage of monosomic nuclei is much higher than trisomic nuclei. In particular, in the general population group, the percentage of 45,X cells was 2.7% and 47,XXX was 0.6%. POF group showed a statistical significant higher percentage rate equal to 7.5% and 3.3%, respectively (P < .001, χ2 test). We compared also the percentage of one X chromosome signal in interphase cells between our patient group and two normal female population described in the literature in two reports by Guttenbach and colleagues in 1995 and Lakhal et al. (2010) (Figure 3). Guttenbach et al. analyzed X chromosome mosaicism in a group of female aged 1 week to 91 years and in particular they found that the percentage of X monosomy in female aged 16–50 years was 3,13% [10, 25, 48]. The comparison between this literature age-matched control group and our patient group showed a significant increase of X monosomy in POF patient group (7.5% of X monosomy, P < .001). Similar results were obtained comparing our patient control group and the control group described by Lakhal and colleagues (2.33% of X monosomy) [25]. These data suggest that low-level X chromosome mosaicism may contribute to POF pathology and these findings are very interesting because POF is a premature cessation of ovarian function and probably the lack of adequate number of follicles may be due to an earlier oocyte aging in these patients that could lead to premature follicular atresia [24, 25]. In particular, Lakhal and colleagues found a correlation between X chromosome monosomy and the age of POF installation in a subgroup (11.5%) of patients, suggesting that mosaicism in these patients was pathological and linked to POF [25].
Figure 3.
Percentage of X monosomy related to aging. The graph shows the linear trend of X monosomy both in POF patient group and in two different reference groups described in two reports from the literature: *(1) Guttenbach et al. (1995) [10] and (2) Lakhal et al. (2010) [25].
Many studies suggest that the incidence of cells lacking sex chromosome, however, might be caused by a preferential cell survival rate than preferential X chromosome loss. In fact, the loss of sex chromosomes (late replicating X chromosome for female and Y chromosome for male) should not affect cell survival as these chromosomes should not play a critical role in lymphocyte survival [6, 49, 50]. X chromosome loss could be accounted by aneuploidy of the late replicating X [51, 52]. Anyway, even if X chromosome is not fundamental for lymphocyte or other type of cell survival, it might have an essential role in the ovary, since various X chromosome abnormalities are associated with POF and many studies suggest that two intact X chromosome are essential for proper ovarian function [16, 20–22]. X chromosome has a pivotal role in ovarian development and maintenance, so the 45,X mosaicism may influence survival rate and be related to accelerated aging of ovarian cells. Follicular deficit of POF patients may be explained by decreased germ cell number, accelerated oocyte atresia, and postnatal destruction of germ cells [53]. The X chromosome appears to play an essential role in the mechanism that leads to POF phenotype, as females lacking an X chromosome, or showing extra copies of the X chromosome, are predisposed to developing POF [54]. In this regard, even trisomy seems to be related to ovarian dysfunction: although normal ovarian function and fertility are reported in most 47,XXX females, some of these patients experience delayed menarche or premature ovarian failure, late onset menarche, and oligomenorrhea [23, 55].
The prevalence of X monosomy can not be attributed to culture artifacts since this phenomenon has been described both in vitro and in vivo [11–13, 56] and it is unlikely that the observed hypodiploidy can be due primarily to technical factors, considering X loss rate in the younger and older age groups [57]. Peripheral blood lymphocytes still remain the standard method in cytogenetic diagnosis procedures because of their accessibility, but it is important to highlight that the karyotypic pattern of the gonad may be different [46]. Anyway, blood lymphocytes provide the best indicator in the detection of senescence, and the increasing of chromosome aneuploidy with aging was assessed also in skin fibroblasts (reviewed in [48]). So it is reasonable to use blood lymphocytes as a model to study chromosome aneuploidy as the specific tissue of interest is often not available.
Fitzgerald in 1975 suggested a mechanism for X chromosome loss based on premature centromeric division (PCD), linked to a subsequent chromosome nondisjunction that may result in cells with an extra X chromosome or with only one sex chromosome, with a great majority of 45,X cells [58]. Burgoyne and Baker in 1984 suggested that 45,X/46,XX/47,XXX mosaicism may accelerate follicular atresia by different mechanisms: (i) aberrant chromosome pairing during meiosis; (ii) deficiency or overexpression of specific gene products on the X chromosome may influence oocyte quality; (iii) an overall impaired genetic control could be related to X chromosome mosaicism leading to defects in meiosis-mitosis process, resulting in gonadal damage, aberrant meiosis, and oocyte atresia [59].
Considering the high rate of X chromosome loss in POF patients, it is reasonable to hypothesize that POF represents a disease spectrum with various degrees, maybe related to X chromosome mosaicism. In fact, considering our data it is possible to suggest that women with X chromosome mosaicism can experience premature menopause [24, 25, 44]. The underling pathological mechanism may be explained by accelerated oocyte aging due to increased mosaicism rate that leads to premature follicular atresia.
5. Conclusion
We performed a study on a large group of POF patients and we identified 27 chromosomal abnormalities associated with POF. Moreover, we assessed a higher frequency of X chromosome aneuploidy rate in POF patients than in the general population group, in particular an increased rate of X chromosome loss, observed by FISH on interphase nuclei. These findings confirm the importance of X chromosome in POF aetiology and the incidence of low-level X chromosome mosaicism in POF patients, as sex chromosome mosaicism may account for some “idiopathic” POF cases.
Acknowledgment
The authors gratefully acknowledge Telethon Foundation, Italy (Grant no. GGP09126 to Professor A. Marozzi).
References
- 1.Jacobs PA, Court Brown WM, Doll R. Distribution of human chromosome counts in relation to age. Nature. 1961;191(4794):1178–1180. doi: 10.1038/1911178a0. [DOI] [PubMed] [Google Scholar]
- 2.Jacobs PA, Brunton M, Brown WMC, Doll R, Goldstein H. Change of human chromosome count distributions with age: evidence for a sex difference. Nature. 1963;197(4872):1080–1081. doi: 10.1038/1971080a0. [DOI] [PubMed] [Google Scholar]
- 3.Kleisner De Galán EH. Age and chromosomes. Nature. 1966;211(5055):1324–1325. doi: 10.1038/2111324b0. [DOI] [PubMed] [Google Scholar]
- 4.Fang JS, Jagiello G, Ducayen M, Graffeo J. Aging and X chromosome loss in the human ovary. Obstetrics and Gynecology. 1975;45(4):455–458. [PubMed] [Google Scholar]
- 5.Martin JM, Kellett JM, Kahn J. Aneuploidy in cultured human lymphocytes: I. Age and sex differences. Age and Ageing. 1980;9(3):147–153. doi: 10.1093/ageing/9.3.147. [DOI] [PubMed] [Google Scholar]
- 6.Bukvic N, Gentile M, Susca F, et al. Sex chromosome loss, micronuclei, sister chromatid exchange and aging: a study including 16 centenarians. Mutation Research. 2001;498(1-2):159–167. doi: 10.1016/s1383-5718(01)00279-0. [DOI] [PubMed] [Google Scholar]
- 7.Neurath P, Deremer K, Bell B, Jarvik L, Kato T. Chromosome loss compared with chromosome size, age and sex of subjects. Nature. 1970;225(5229):281–282. doi: 10.1038/225281a0. [DOI] [PubMed] [Google Scholar]
- 8.Fitzgerald PH, McEwan CM. Total aneuploidy and age-related sex chromosome aneuploidy in cultured lymphocytes of normal men and women. Human Genetics. 1977;39(3):329–337. doi: 10.1007/BF00295428. [DOI] [PubMed] [Google Scholar]
- 9.Richard F, Aurias A, Couturier J, et al. Aneuploidy in human lymphocytes: an extensive study of eight individuals of various ages. Mutation Research. 1993;295(2):71–80. doi: 10.1016/0921-8734(93)90003-l. [DOI] [PubMed] [Google Scholar]
- 10.Guttenbach M, Koschorz B, Bernthaler U, Grimm T, Schmid M. Sex chromosome loss and aging: in situ hybridization studies on human interphase nuclei. American Journal of Human Genetics. 1995;57(5):1143–1150. [PMC free article] [PubMed] [Google Scholar]
- 11.Hando JC, Nath J, Tucker JD. Sex chromosomes, micronuclei and aging in women. Chromosoma. 1994;103(3):186–192. doi: 10.1007/BF00368011. [DOI] [PubMed] [Google Scholar]
- 12.Richard F, Muleris M, Dutrillaux B. The frequency of micronuclei with X chromosome increases with age in human females. Mutation Research. 1994;316(1):1–7. doi: 10.1016/0921-8734(94)90002-7. [DOI] [PubMed] [Google Scholar]
- 13.Catalán J, Autio K, Kuosma E, Norppa H. Age-dependent inclusion of sex chromosomes in lymphocyte micronuclei of man. American Journal of Human Genetics. 1998;63(5):1464–1472. doi: 10.1086/302092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Wojda A, Zietkiewicz E, Witt M. Effects of age and gender on micronucleus and chromosome nondisjunction frequencies in centenarians and younger subjects. Mutagenesis. 2007;22(3):195–200. doi: 10.1093/mutage/gem002. [DOI] [PubMed] [Google Scholar]
- 15.Coulam CB. Premature gonadal failure. Fertility and Sterility. 1982;38(6):645–655. doi: 10.1016/s0015-0282(16)46688-4. [DOI] [PubMed] [Google Scholar]
- 16.Laml T, Preyer O, Umek W, Hengstschlager M, Hanzal E. Genetic disorders in premature ovarian failure. Human Reproduction Update. 2002;8(5):483–491. doi: 10.1093/humupd/8.5.483. [DOI] [PubMed] [Google Scholar]
- 17.Goswami D, Conway GS. Premature ovarian failure. Human Reproduction Update. 2005;11(4):391–410. doi: 10.1093/humupd/dmi012. [DOI] [PubMed] [Google Scholar]
- 18.Devi A, Benn PA. X-chromosome abnormalities in women with premature ovarian failure. Journal of Reproductive Medicine for the Obstetrician and Gynecologist. 1999;44(4):321–324. [PubMed] [Google Scholar]
- 19.Schlessinger D, Herrera L, Crisponi L, et al. Genes and translocations involved in POF. American Journal of Medical Genetics. 2002;111(3):328–333. doi: 10.1002/ajmg.10565. [DOI] [PubMed] [Google Scholar]
- 20.Davison RM, Davis CJ, Conway GS. The X chromosome and ovarian failure. Clinical Endocrinology. 1999;51(6):673–679. doi: 10.1046/j.1365-2265.1999.00926.x. [DOI] [PubMed] [Google Scholar]
- 21.Conway GS. Premature ovarian failure. British Medical Bulletin. 2000;56(3):643–649. doi: 10.1258/0007142001903445. [DOI] [PubMed] [Google Scholar]
- 22.Zinn AR. The X chromosome and the ovary. Journal of the Society for Gynecologic Investigation. 2001;8(1, supplement):S34–S36. doi: 10.1016/s1071-5576(00)00104-0. [DOI] [PubMed] [Google Scholar]
- 23.Holland CM. 47,XXX in an adolescent with premature ovarian failure and autoimmune disease. Journal of Pediatric and Adolescent Gynecology. 2001;14(2):77–80. doi: 10.1016/s1083-3188(01)00075-4. [DOI] [PubMed] [Google Scholar]
- 24.Devi AS, Metzger DA, Luciano AA, Benn PA. 45,X/46,XX mosaicism in patients with idiopathic premature ovarian failure. Fertility and Sterility. 1998;70(1):89–93. doi: 10.1016/s0015-0282(98)00122-8. [DOI] [PubMed] [Google Scholar]
- 25.Lakhal B, Braham R, Berguigua R, et al. Cytogenetic analyses of premature ovarian failure using karyotyping and interphase fluorescence in situ hybridization (FISH) in a group of 1000 patients. Clinical Genetics. 2010;78(2):181–185. doi: 10.1111/j.1399-0004.2009.01359.x. [DOI] [PubMed] [Google Scholar]
- 26.Vegetti W, Tibiletti MG, Testa G, et al. Inheritance in idiopathic premature ovarian failure: analysis of 71 cases. Human Reproduction. 1998;13(7):1796–1800. doi: 10.1093/humrep/13.7.1796. [DOI] [PubMed] [Google Scholar]
- 27.Tibiletti MG, Testa G, Vegetti W, et al. The idiopathic forms of premature menopause and early menopause show the same genetic pattern. Human Reproduction. 1999;14(11):2731–2734. doi: 10.1093/humrep/14.11.2731. [DOI] [PubMed] [Google Scholar]
- 28.Marozzi A, Manfredini E, Tibiletti M, et al. Molecular definition of Xq common-deleted region in patients affected by premature ovarian failure. Human Genetics. 2000;107(4):304–311. doi: 10.1007/s004390000364. [DOI] [PubMed] [Google Scholar]
- 29.Mumm S, Herrera L, Waeltz PW, et al. X/autosomal translocations in the Xq critical region associated with premature ovarian failure fall within and outside genes. Genomics. 2001;76(1–3):30–36. doi: 10.1006/geno.2001.6611. [DOI] [PubMed] [Google Scholar]
- 30.Portnoï MF, Aboura A, Tachdjian G, et al. Molecular cytogenetic studies of Xq critical regions in premature ovarian failure patients. Human Reproduction. 2006;21(9):2329–2334. doi: 10.1093/humrep/del174. [DOI] [PubMed] [Google Scholar]
- 31.Hook EB. Exclusion of chromosomal mosaicism: tables of 90%, 95%, and 99% confidence limits and comments on use. American Journal of Human Genetics. 1977;29(1):94–97. [PMC free article] [PubMed] [Google Scholar]
- 32.Mukherjee AB, Thomas S. A longitudinal study of human age-related chromosomal analysis in skin fibroblasts. Experimental Cell Research. 1997;235(1):161–169. doi: 10.1006/excr.1997.3673. [DOI] [PubMed] [Google Scholar]
- 33.Maraschio P, Fraccaro M. Citogenetica of the Mammalian X Chromosome—part B: X Chromosome Anomalies and Their Clinical Manifestations. New York, NY, USA: Alan R. Liss; 1983. Phenotypic effects of X-chromosome deficiencies; pp. 359–369. [Google Scholar]
- 34.Bettio D, Levi Setti P, Bianchi P, Grazioli V. Trisomy 18 mosaicism in a woman with normal intelligence. American Journal of Medical Genetics. 2003;120(2):303–304. doi: 10.1002/ajmg.a.20213. [DOI] [PubMed] [Google Scholar]
- 35.Lissoni S, Baronchelli S, Villa N, et al. Chromosome territories, X;Y translocation and premature ovarian failure: is there a relationship? Molecular Cytogenetics. 2009;2:p. 19. doi: 10.1186/1755-8166-2-19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Marozzi A, Vegetti W, Manfredini E, et al. Association between idiopathic premature ovarian failure and fragile X premutation. Human Reproduction. 2000;15(1):197–202. doi: 10.1093/humrep/15.1.197. [DOI] [PubMed] [Google Scholar]
- 37.Marozzi A, Porta C, Vegetti W, et al. Mutation analysis of the inhibin alpha gene in a cohort of Italian women affected by ovarian failure. Human Reproduction. 2002;17(7):1741–1745. doi: 10.1093/humrep/17.7.1741. [DOI] [PubMed] [Google Scholar]
- 38.Rossetti R, Pasquale ED, Marozzi A, et al. BMP15 mutations associated with primary ovarian insufficiency cause a defective production of bioactive protein. Human Mutation. 2009;30(5):804–810. doi: 10.1002/humu.20961. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Hanson L, Bryman I, Barrenäs ML, et al. Genetic analysis of mosaicism in 53 women with Turner syndrome. Hereditas. 2001;134(2):153–159. doi: 10.1111/j.1601-5223.2001.00153.x. [DOI] [PubMed] [Google Scholar]
- 40.Cameron M, Grover S, Moore P, Jayasinghe Y. Non-chromosomal, non-iatrogenic premature ovarian failure in an adolescent population: a case series. Journal of Pediatric and Adolescent Gynecology. 2008;21(1):3–8. doi: 10.1016/j.jpag.2007.07.003. [DOI] [PubMed] [Google Scholar]
- 41.Hreinsson JG, Otala M, Fridström M, et al. Follicles are found in the ovaries of adolescent girls with Turner’s syndrome. Journal of Clinical Endocrinology and Metabolism. 2002;87(8):3618–3623. doi: 10.1210/jcem.87.8.8753. [DOI] [PubMed] [Google Scholar]
- 42.Mukherjee AB, Alejandro J, Payne S, Thomas S. Age-related aneuploidy analysis of human blood cells in vivo by fluorescence in situ hybridization (FISH) Mechanisms of Ageing and Development. 1996;90(2):145–156. doi: 10.1016/0047-6374(96)01762-9. [DOI] [PubMed] [Google Scholar]
- 43.Mukherjee AB, Thomas S, Schmitt E. Chromosomal analysis in young vs. senescent human fibroblasts by fluorescence in situ hybridization: a selection hypothesis. Mechanisms of Ageing and Development. 1995;80(1):11–23. doi: 10.1016/0047-6374(94)01544-v. [DOI] [PubMed] [Google Scholar]
- 44.Wu RC, Kuo PL, Lin SJ, Liu CH, Tzeng CC. X chromosome mosaicism in patients with recurrent abortion or premature ovarian failure. Journal of the Formosan Medical Association. 1993;92(11):953–956. [PubMed] [Google Scholar]
- 45.Nowinski GP, Van Dyke DL, Tilley BC, et al. The frequency of aneuploidy in cultured lymphocytes is correlated with age and gender but not with reproductive history. American Journal of Human Genetics. 1990;46(6):1101–1111. [PMC free article] [PubMed] [Google Scholar]
- 46.Kuo PL, Guo HR. Mechanism of recurrent spontaneous abortions in women with mosaicism of X-chromosome aneuploidies. Fertility and Sterility. 2004;82(6):1594–1601. doi: 10.1016/j.fertnstert.2004.06.042. [DOI] [PubMed] [Google Scholar]
- 47.Moore AK, Lynch K, Arny MJ, Grow DR. Turner mosaicism (45,X/46,XX) diagnosed in a young woman subsequent to low oocyte maturity and failed ICSI. Fertility and Sterility. 2008;90(5):2012.e13–2012.e15. doi: 10.1016/j.fertnstert.2008.03.063. [DOI] [PubMed] [Google Scholar]
- 48.Wojda A, Witt M. Manifestations of ageing at the cytogenetic level. Journal of Applied Genetics. 2003;44(3):383–399. [PubMed] [Google Scholar]
- 49.Bolognesi C, Abbondandolo A, Barale R, et al. Age-related increase of baseline frequencies of sister chromatid exchanges, chromosome aberrations, and micronuclei in human lymphocytes. Cancer Epidemiology Biomarkers and Prevention. 1997;6(4):249–256. [PubMed] [Google Scholar]
- 50.Stone JF, Sandberg AA. Sex chromosome aneuploidy and aging. Mutation Research. 1995;338(1–6):107–113. doi: 10.1016/0921-8734(95)00016-y. [DOI] [PubMed] [Google Scholar]
- 51.Abruzzo MA, Mayer M, Jacobs PA. Aging and aneuploidy: evidence for the preferential involvement of the inactive X chromosome. Cytogenetics and Cell Genetics. 1985;39(4):275–278. doi: 10.1159/000132157. [DOI] [PubMed] [Google Scholar]
- 52.Tucker JD, Nath J, Hando JC. Activation status of the X chromosome in human micronucleated lymphocytes. Human Genetics. 1996;97(4):471–475. doi: 10.1007/BF02267069. [DOI] [PubMed] [Google Scholar]
- 53.Pal L, Santoro N. Premature ovarian failure (POF): discordance between somatic and reproductive aging. Ageing Research Reviews. 2002;1(3):413–423. doi: 10.1016/s1568-1637(02)00009-0. [DOI] [PubMed] [Google Scholar]
- 54.Villanueva AL, Rebar RW. Triple-X syndrome and premature ovarian failure. Obstetrics and Gynecology. 1983;62(supplement 3):70s–73s. [PubMed] [Google Scholar]
- 55.Brambila-Tapia AJL, Rivera H, García-Castillo H, Domínguez-Quezada MG, Dávalos-Rodríguez IP. 47,XXX/45,X/46,XX mosaicism in a patient with Turner phenotype and spontaneous puberal development. Fertility and Sterility. 2009;92(5):1747.e5–1747.e7. doi: 10.1016/j.fertnstert.2009.07.1008. [DOI] [PubMed] [Google Scholar]
- 56.Guttenbach M, Schakowski R, Schmid M. Aneuploidy and ageing: sex chromosome exclusion into micronuclei. Human Genetics. 1994;94(3):295–298. doi: 10.1007/BF00208287. [DOI] [PubMed] [Google Scholar]
- 57.Ford JH, Russel JA. Differences in the error mechanisms affecting sex and autosomal chromosomes in women of different ages within the reproductive age group. American Journal of Human Genetics. 1985;37(5):973–983. [PMC free article] [PubMed] [Google Scholar]
- 58.Fitzgerald PH. A mechanism of X chromosome aneuploidy in lymphocytes of aging women. Humangenetik. 1975;28(2):153–158. doi: 10.1007/BF00735748. [DOI] [PubMed] [Google Scholar]
- 59.Burgoyne PS, Baker TG. Meiotic pairing and gametogenic failure. Symposia of the Society for Experimental Biology. 1984;38:349–362. [PubMed] [Google Scholar]