Abstract
Differentiating intestinal tuberculosis from Crohn’s disease (CD) is an important clinical challenge of considerable therapeutic significance. The problem is of greatest magnitude in countries where tuberculosis continues to be highly prevalent, and where the incidence of CD is increasing. The final clinical diagnosis is based on a combination of the clinical history with endoscopic studies, culture and polymerase chain reaction for Mycobacterium tuberculosis, biopsy pathology, radiological investigations and response to therapy. In a subset of patients, surgery is required and intraoperative findings with pathological study of the resected bowel provide a definitive diagnosis. Awareness of the parameters useful in distinguishing these two disorders in each of the different diagnostic modalities is crucial to accurate decision making. Newer techniques, such as capsule endoscopy, small bowel enteroscopy and immunological assays for Mycobacterium tuberculosis, have a role to play in the differentiation of intestinal tuberculosis and CD. This review presents currently available evidence regarding the usefulness and limitations of all these different modalities available for the evaluation of these two disorders.
Keywords: Tuberculosis, Crohn’s disease, Clinical features, Endoscopy, Serology, Enteroscopy, Histology, Radiology, Surgery, Therapy
INTRODUCTION
Tuberculosis (TB) of the gastrointestinal tract and Crohn’s disease (CD) are chronic granulomatous disorders with similarities in their clinical presentation and pathology. The rising incidence of CD in countries like India where TB continues to be endemic has made the differentiation of these two disorders a diagnostic challenge[1-4]. Misdiagnosis leads to delays in initiating effective therapy with increased morbidity and mortality, hence the importance of making an accurate diagnosis at the earliest possible stage. Despite the similarities of these two disorders a number of studies have identified specific differences in their clinical, endoscopic, radiological and pathologic findings. Other laboratory tests such as culture and molecular testing for Mycobacterium tuberculosis (MTB) have also been described to be useful in distinguishing them, as has been their response to therapy[5,6]. In this review we present current evidence from the literature regarding conventional and new modalities that could be helpful in discriminating intestinal TB from CD.
CLINICAL FEATURES
Clinical features in both diseases include (1) constitutional symptoms such as fever, anorexia and weight loss; (2) symptoms due to mucosal ulceration such as diarrhea, hematochezia and malabsorption; (3) symptoms due to transmural involvement such as abdominal pain, and distention and vomiting due to luminal obstruction; a palpable lump; intestinal perforation and perianal and intestinal fistualization; (4) extra-intestinal manifestations such as arthritis and sclerosing cholangitis in the case of CD and involvement of other organs such as joints, lungs, peritoneum and lymph nodes in the case of TB; and (5) a family history of inflammatory bowel disease (IBD) in the case of CD or a history of family contacts in the case of TB[7,8].
In patients with CD the duration of illness is generally more than 12 mo while it is shorter, lasting around 6 to 7 mo, in intestinal TB[7]. Diarrhea and hematochezia are more commonly seen in CD while fever, ascites and co-existing TB at other sites are seen in gastrointestinal TB. Perianal disease, malabsorption and recurrence of disease after surgery are in favor of CD. A family history of IBD may be seen in 10% of patients with CD. Extra-intestinal involvement due to tuberculosis is seen in a third of patients with intestinal TB[7,9]. A high index of clinical suspicion is required, however, to differentiate between the two conditions clinically.
SEROLOGY
Abnormalities in routine blood tests such as total and differential leukocyte count, raised ESR, C-reactive protein and low hemoglobin are seen in the active phase of both intestinal TB and CD[5,7]. Platelet counts may be raised in the active phase of CD due to reversible hyposplenism and may increase the suspicion of CD over intestinal TB. One study on a small number of patients with intestinal TB showed that only one of 14 (7%) patients had a positive result to enzyme-linked immunosorbent assay (ELISA) against anti-Saccharomyces cerevisiae antibody (ASCA) in serum in contrast to 49% with CD[10], therefore, the authors recommended use of this test for differentiation between CD and intestinal TB. However, two studies from India involving a larger number of patients showed that ASCA was not useful in differentiating between CD and TB[11,12]. Almost half of the patients with intestinal TB in both studies were ASCA-positive, which was comparable to the frequency in patients with CD. ASCA is a non-specific antibody resulting from macromolecular transport of food antigens (including antigens contained in baker’s yeast), partly resulting from an increase in intestinal permeability. Since patients with intestinal TB have chronic inflammatory lesions of the small intestine, similar to patients with CD with increased small intestinal permeability, frequent positive results with the ASCA test in the former condition is quite expected[11].
CULTURES
The most reliable method to differentiate between intestinal TB and CD is demonstration of acid-fast bacilli (AFB) either in smears or by culture. However, smear and culture to demonstrate MTB have low sensitivity. Furthermore, Mycobacteria take a very long time (4-6 wk) to grow in culture. Identification of AFB on intestinal biopsies has been reported with variable frequency (25%-36%)[5,7,13]. MTB was cultured from mucosal biopsies only in one third of patients with colonic TB[14]. The use of fluorescent stain for the diagnosis of intestinal TB increases sensitivity but lacks specificity and results are still poor due to the pauci-bacillary nature of the disease[7]. The time to recovery of Mycobacteria from culture has been shortened to 2-3 wk by the use of automated culture systems such as BACTEC, Mycobacteria growth indicator tube (MGIT), MB/BacT mycobacterial detection system and the ESP culture system II[15]. The sensitivity of the BACTEC system was found to be poor, however, for the diagnosis of intestinal TB[7,8]. In the MGIT system, a fluorescent compound is embedded in silicone at the bottom of the tube. This compound is sensitive to dissolved oxygen in broth. As the actively growing bacteria consume the dissolved oxygen, the fluorescence is unmasked and can be observed in the tube under long wave UV light[16]. MB/BacT is a colorimetric, non-radiometric method of detection of mycobacterial growth, which uses Middlebrook 7H9 media in an atmosphere of CO2, H2 and O2 under vacuum. In ESP culture system II, each culture bottle is continuously monitored for any change in gas pressure due to metabolic activity of the microorganism[16]. These systems, however, need to be evaluated for the diagnosis of intestinal TB.
POLYMERASE CHAIN REACTION FOR MTB
The TB polymerase chain reaction (PCR) assay is based on augmenting oligonucleotides found in MTB chromosomes that are highly specific for the organism. TB PCR analysis of endoscopic biopsy specimens or surgical specimens can be done quickly and results can be obtained within 48 h[17]. This test is very specific for TB but occasionally may be positive in patients with CD[18,19]. Sensitivity of this test is modest and there is no correlation between PCR positivity and histological lesions such as caseation or granulomas[17,18]. In situ TB PCR and analysis of fecal samples of patients with gastrointestinal TB have been shown to be useful in small studies[14,20], but need validation in larger numbers of patients. The in situ TB PCR technique needs to be improved for better sensitivity. As currently used, TB PCR on biopsy samples has a high positive predictive value but a very low negative predictive value.
QUANTIFERON-TB GOLD
Quantiferon-TB Gold (QFT-G, Cellestis Limited, Carnegie, Victoria, Australia) is an in vitro ELISA which detects the release of interferon-gamma after stimulation by MTB antigen. The test, approved by the Food and Drug Administration (FDA) as an aid in diagnosing MTB infection, including both latent TB infection and TB disease, is performed by incubating fresh heparinized whole blood from sensitized persons with mixtures of synthetic peptides representing proteins present in M. tuberculosis: early secretory antigenic target-6 (ESAT-6) and culture filtrate protein-10 (CFP-10). The synthetic peptides used in QFT-G are absent from all BCG strains and most non-tuberculosis mycobacteria except M. kansasii, M. szulgai and M. marinum.
Advantages and limitations
The advantages of QFT-G include lack of cross-reaction with BCG and most nontuberculous mycobacteria, avoidance of reader bias and the need for only a single patient visit. It may also be useful in monitoring the clinical response to anti-TB therapy.
The limitations include the need for incubation within 12 h of blood collection and its inability to differentiate infection with TB from latent TB infection. Though the sensitivity of QFT-G for detecting MTB infection in individuals with untreated culture-confirmed TB is approximately 80% in published studies, its sensitivity for latent TB infection seems to be less than that of the tuberculin skin test. The ability of the test to predict the risk of progression to subsequent TB disease in latent TB has not been determined. The test should be interpreted with caution as a patient with a negative test may still have latent TB infection or active TB disease. In a study of HIV sero-negative pulmonary TB patients from Chennai, QFT-G and the tuberculin skin test yielded diagnostic sensitivities of 90.6% (95% CI: 86.3%-94.9%) and 68.9% (95% CI: 60.6%-77.2%), and specificities of 55% (95% CI: 35.2%-54.8%) and 75.5% (95% CI: 66.8%-84.2%), respectively. The higher sensitivity noted in this study may be due to the exclusion of HIV patients[21].
Role of QFT-G in intestinal tuberculosis
The role of QFT-G in intestinal tuberculosis is not clear. The test may have a possible role in follow up of patients on antituberculous therapy (ATT), in the diagnostic dilemma of CD vs TB and may be undertaken prior to starting biologicals in CD patients.
ENDOSCOPY
Gastrointestinal endoscopy - ileo-colonoscopy, device-assisted enteroscopy and gastro-duodenoscopy - plays a crucial role in the differentiation of intestinal TB from CD[6,22]. Endoscopy permits direct visualization and biopsy of lesions for histological and other studies from virtually the entire alimentary tract[23,24].
The ileo-cecal region is the most common site affected in either condition, and colonoscopy with retrograde intubation of the ileum is the initial procedure of choice. In patients with suspected or proven CD, ileo-colonoscopy provided similar sensitivity (67% vs 83%) but significantly higher specificity (100% vs 53%) compared to video capsule endoscopy[25]. The incremental diagnostic yield of ileoscopy, low at 3.7%, may yet be important in a given patient[26]. The diagnostic yield of histology increases with increasing number of biopsies from up to four segments in the colon[1]. Endoscopic biopsies from segments upstream after dilating a stricture, and also from the normal looking ileum, increase the yield in patients with suspected TB[27,28].
When the colon is spared, gastro-duodenoscopy and enteroscopy may be appropriate[6,22,24]. Balloon-assisted and spiral enteroscopy are preferred modalities for evaluating the small bowel today because of biopsy and therapeutic capability[23]. Biopsying small bowel lesions is important because the causes of ulcerating lesions cannot be differentiated based on endoscopic appearances alone[23]. Biopsies from normal appearing colonic or gastro-duodenal mucosa may provide diagnostic clues in suspected CD[1,29].
Characteristic endoscopic features have been described in intestinal TB and CD[6,22,24]. Transversely placed ulcers, nodularity and hypertrophic lesions resembling masses are characteristic of TB. Aphthoid or longitudinal, deep, fissuring ulcers and a cobblestone appearance are said to be more typical of CD. Very few studies have directly compared these or evaluated their diagnostic value and inter-observer agreement.
In a small comparative study, ano-rectal lesions, longitudinal ulcers, aphthous ulcers, and a cobblestone appearance were significantly more common in CD, and involvement of fewer than four segments, a patulous ileocecal valve, transverse ulcers, and pseudopolyps were more frequent in intestinal TB. Assuming that a diagnosis of one or the other disease could be made based on which parameters were more common in a given patient, the endoscopic diagnosis would have been proved correct in 77 of 88 (87.5%) patients[30]. These findings need to be validated before recommendation for routine use.
In a more recent prospective study, skip lesions in the colon were significantly more frequent in patients with CD compared to patients with intestinal TB (66% vs 17%)[31], as were aphthous ulceration (54% vs 13%), linear ulceration (30% vs 7%) and superficial ulceration (51% vs 17%). Cobblestoning of the colonic mucosa was seen only in CD (17% vs 0%). Nodularity of the colonic mucosa was significantly more common in patients with TB than in those with CD (49% vs 24.5%).
Capsule endoscopy
Capsule endoscopy has been established as a safe and non-invasive modality for the diagnosis of CD[32,33]. A meta analysis comparing capsule endoscopy with other imaging modalities of the small bowel for inflammatory bowel disease established that capsule endoscopy has an incremental diagnostic yield of 25%-40% over other modalities[34]. Capsule endoscopy has the unique ability to visualize small ulcers and early inflammatory lesions. Fidder et al[35] defined a positive capsule result for CD as presence of four or more ulcers, erosions, or a region with clear exudate and mucosal hyperemia and edema. A scoring index developed to quantify mucosal changes detected by capsule endoscopy in any inflammatory processes of the small bowel is based on three variables: villous appearance, ulceration and stenosis. Each variable is assessed by size and extent of change. The index does not diagnose or measure a disease and does not have the discriminatory ability to differentiate between illnesses, but only measures mucosal changes. The International Conference on Capsule Endoscopy consensus statement declared that capsule endoscopy may play an important role in the diagnosis and monitoring of patients with known or suspected CD[36]; playing a unique role in assessing mucosal healing after medical therapy, helping to assess early postoperative recurrence and guiding therapy. The consensus statement concluded that capsule endoscopy may identify sub-clinical markers in asymptomatic family members and contribute to the understanding of the natural history of IBD.
There are limited data regarding capsule endoscopy in intestinal TB. This can be attributed to non-affordability of capsule endoscopy in TB endemic countries and the inability of capsule endoscopy to take biopsies. A few case reports have described capsule endoscopic features of intestinal TB as multiple scattered short, oblique or transverse mucosal ulcers with a necrotic base in the jejunum and ileum[37]. Cello et al[38] also found that ulcers of the small bowel in intestinal TB were characteristically shallow with extensive irregular “geographic” borders, were usually not larger than 1-2 cm and were transverse rather than longitudinal. However, it is difficult to differentiate CD from TB based on capsule endoscopic features alone.
Small bowel enteroscopy
Double balloon and single balloon enteroscopy have the unique ability to visualize most of the small intestine by combined antegrade and retrograde approaches with biopsy capability and the possibility of therapeutic interventions[39,40]. However, they are more invasive than capsule endoscopy and need to be performed under sedation. A meta analysis compared capsule endoscopy and double balloon enteroscopy in patients with suspected inflammatory lesions and found no statistically significant difference in their diagnostic yield[41]. A few case reports have described the double balloon enteroscopic findings in intestinal TB. Nakamura et al[42] described multiple focal shallow irregular ulcers with necrotic bases of about 5 mm in the mid and distal ileum by double balloon enteroscopy through the retrograde route. In a series of 106 cases of single balloon enteroscopy, Ramchandani et al[43] diagnosed 13 cases of CD and 3 cases of intestinal TB, which were confirmed by mucosal biopsies. There were focal longitudinal and aphthous ulcers in the jejunum and ileum in CD, whereas ulcers in TB were oblique or transverse with a necrotic base. Focal ulcerated strictures were noted in the distal jejunum and ileum in four cases of CD.
RADIOLOGY
Imaging plays an important role in diagnosing and differentiating intestinal TB from CD[44-46]. Barium examination is the mainstay for the evaluation of the intestinal tract. Computed tomography (CT) is complementary to barium examination for the evaluation of extra-intestinal pathologies. CT enteroclysis is a hybrid technique that combines the advantages of both barium examination and CT.
In the vast majority of cases, differentiation of intestinal TB from CD is possible when radiological findings are correlated with clinical features, histopathological findings and response to treatment[47-49].
Various points of distinction are summarized as follows.
Distribution of disease
The ileo-cecal region is the most common site involved in intestinal TB (Figure 1)[49,50]. Isolated involvement of the ileo-cecal region is not seen in CD which typically involves the ileum with conspicuous sparing of the ileo-cecal valve. The cecum may rarely be involved in direct contiguity with the ileum or colonic disease.
Figure 1.
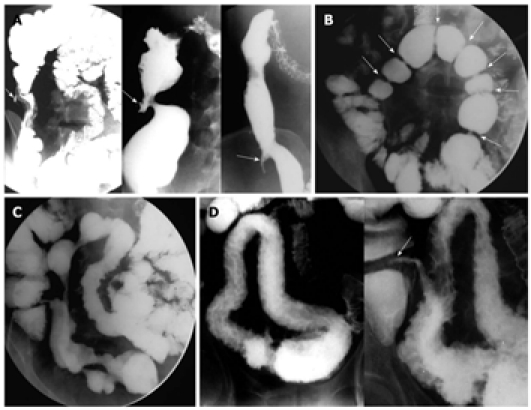
Findings on barium study of the small intestine. A: Barium study in three different patients with tuberculosis (TB) demonstrating shrunken, conical and retracted cecum (arrows); B: Multiple strictures (arrows) in ileal loops of a patient with TB. Note the short, concentric and smooth outline of the strictures; C: Multiple eccentric strictures seen in the ileum of a patient with Crohn's disease (CD). Note the normal ileo-cecal junction; D: Barium study showing an ulceronodular pattern involving a long segment of the ileum in a patient with CD. Note sparing of the ileo-cecal junction (arrow).
Colorectal involvement with small bowel disease is more often seen in CD than in TB whereas the ascending colon may be involved in direct contiguity with the ileo-cecal region in TB. Isolated colorectal involvement in TB is rare as compared to CD.
Barium findings (small bowel)
Strictures are the most common finding in intestinal TB and are typically short, concentric and smooth in outline with significant prestenotic dilatation (Figure 1A). In CD, strictures are usually long (the result of fibrosis, irritability and inflammation), eccentric with sacculations at the anti-mesenteric border and without significant prestenotic dilatation (Figure 1B). Aphthous ulcers and an ulceronodular pattern are almost pathognomonic in the appropriate clinical settings (Figure 1C). Tubercular ulcers are less common, longitudinally oriented and tend to be round to oval in configuration. Perforation and fistulae are more often encountered with CD, while enteroliths are more common in intestinal TB. Malignancy is a complication seen only with CD.
Barium findings (large bowel)
In TB, solitary or multiple strictures which are smooth and concentric are the most common finding (Figure 2A) while aphthous ulcers, segmental colitis and cobblestoning are the predominant findings in CD (Figure 2B and C).
Figure 2.
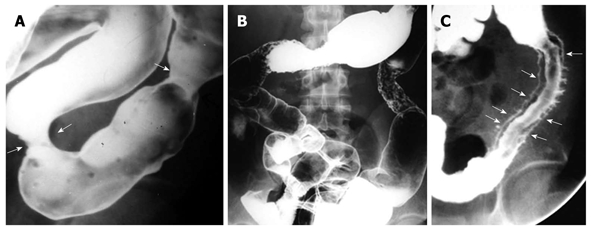
Findings on barium study of the colon in tuberculosis and Crohn's disease. A: Barium enema showing tubercular strictures (arrows) of the colon; B: Barium enema demonstrating skip lesions affecting descending and transverse colon as ulcers with areas of narrowing in a patient with Crohn's disease (CD); C: Deep ulcers with double tracking of sigmoid colon in a patient with CD (arrows).
Computed tomography
In CD, mural thickening with stratification is seen with active inflammation (Figure 3A) (Table 1). In addition, vascular engorgement of the mesentery (comb sign) and mesenteric fibrofatty proliferation are seen (Figure 3B and C). Mural thickening with contiguous ileo-cecal involvement is more often the presentation of intestinal TB (Figure 3D). Hypodense lymph nodes with peripheral enhancement in the mesentery and retro-peritoneum are characteristic of TB (Figure 3E), while in CD hypodense lymph nodes are seen.
Figure 3.
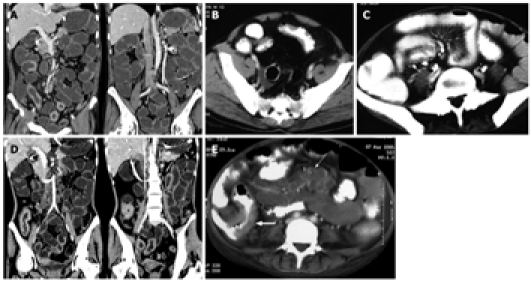
Findings on computed tomography. A: Computed tomography (CT) enteroclysis with negative oral contrast showing mural thickening of ileum with skip areas and sparing of cecum in a patient with Crohn's disease (CD); B: Contrast-enhanced CT scan (CECT) showing asymmetrical mural thickening in ileal loop with deep ulcerations. Note fibro-fatty proliferation of mesentery; C: CECT in another patient with CD showing mesenteric vascular engorgement (Comb sign) with fibro-fatty proliferation of the mesentery; D: CT enteroclysis with negative oral contrast showing contiguous mural thickening of the terminal ileum and cecum in a patient with tuberculosis (TB); E: CECT in a patient with TB showing mural thickening of the terminal ileum and cecum (thick arrow) with multiple enlarged mesenteric lymph nodes showing central hypoattenuating and peripherally enhancing rims (thin arrow).
Table 1.
Computed tomographic features of intestinal tuberculosis and Crohn’s disease
| Tuberculosis | Crohn’s disease |
| Mural thickening without stratification | Mural thickening with stratification in active inflammation |
| Strictures concentric | Strictures eccentric |
| Fibrofatty proliferation of mesentery very rare | Fibrofatty proliferation of mesentery |
| Mesenteric inflammation but no vascular engorgement | Hypervascular mesentery (comb sign) |
| Hypodense lymph nodes with peripheral enhancement | Mild lymphadenopathy |
| High density ascites | Abscesses |
PATHOLOGY
Surgical resections
Macroscopically, TB classically causes ulceration, short strictures, marked thickening of the bowel wall due to inflammation, fibrosis and adhesions, or a combination of these. The ulcers are transverse, often circumferential, with ill-defined, sloping or overhanging edges. The surrounding mucosa may show flattening of folds, ulcers, erosions and pseudopolyps. The cut section of the intestinal wall shows scarring and necrosis, often with loss of distinction of the different layers. The serosal surface may show 2-5 mm-sized nodules and adhesions. The regional lymph nodes are invariably enlarged and may show caseation[51].
The histological hallmarks of TB are confluent, caseating granulomas containing acid fast bacilli and surrounded by a lymphoid cuff. These are found in all layers of the intestinal wall and in regional lymph nodes, but sometimes only in the latter[51]. Early granulomas are usually found within lymphoid tissue[52]. There may be extensive pyloric metaplasia. Occasional superficial fissuring ulcers that extend into the submucosa may be seen. Healing occurs by fibrosis, and epithelial regeneration begins at the edge of ulcers. Healing granulomas are surrounded by a rim of fibrous tissue in lymph nodes, but not in the intestinal wall[51].
Macroscopically, CD also shows bowel wall thickening, skip lesions and strictures, but the latter are longer than in TB. Fat wrapping is common, as are adhesions, fistulae, sinuses and extra-intestinal abscesses[53]. Mucosal aphthous ulcers are seen at an early stage, and coalesce to form larger stellate ulcers. Deep, longitudinal, fissuring ulcers are characteristic of CD, as well as smaller longitudinal ulcers separating edematous or uninvolved mucosa to create a cobblestone appearance[54].
Microscopically, common features are aphthous ulcers over lymphoid follicles, fissuring ulcers that extend into the muscularis propria or deeper, distortion of the mucosal architecture, pyloric metaplasia, cryptitis and crypt abscess formation with moderate to severe chronic inflammation. These changes are often segmental or patchy and extend transmurally. Prominent lymphoid follicles in the submucosa and serosa are another characteristic feature of CD. Granulomas, characteristically small, are seen in 50%-60% of resection specimens and may be found in the regional lymph nodes in about 25% of cases[54].
Mucosal biopsies
With the increasing use of endoscopic procedures to visualize the intestinal lumen and obtain targeted biopsies from diseased areas, the histological differentiation of intestinal TB and CD is most commonly made on mucosal biopsies. One of the limitations of mucosal biopsies is that granulomas, the primary differentiating feature of TB from CD, are found in only 50%-80% of intestinal mucosal biopsies from patients with clinically confirmed TB[31,55,56] and in 15%-65% of mucosal biopsies from patients with CD[57]. Caseation and AFB, the diagnostic features of TB, are found in only 18%-33% of cases[56,58] and in as low as 5% of cases[58], respectively. Other features suggestive of TB include confluent granulomas (Figure 4A), a lymphoid cuff around granulomas, granulomas larger than 400 μm in diameter (Figure 4B), 5 or more granulomas in biopsies from one segment, granulomas located in the submucosa or in granulation tissue, often as palisaded epithelioid histiocytes, and disproportionate submucosal inflammation[1,3]. Features that favor a diagnosis of CD on mucosal biopsies include infrequent (< 5), small (< 200 μm in size) granulomas that are poorly organized and discrete or isolated. Granulomas are located more commonly in the mucosa than in other sites in CD. Microgranulomas, or aggregates of histiocytes (Figure 4C), and crypt-centered inflammation such as pericryptal granulomas (Figure 4D) and focally enhanced colitis are also features of CD[1,3,59].
Figure 4.
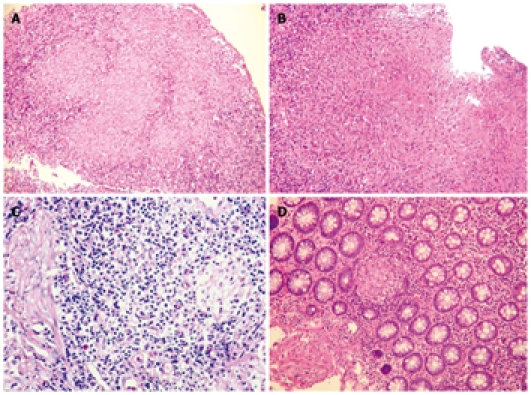
Histological features. A: Confluent granulomas in inflammatory granulation tissue from ulcerated colonic mucosa of a patient with tuberculosis (TB) [Hematoxylin and eosin (HE), 100 ×]; B: Large granuloma in the ulcerated mucosa of a patient with TB (HE, 100 ×); C: Microgranuloma composed of a small aggregate of macrophages in a lymphoid follicle from the mucosa of a patient with Crohn's disease (CD) (HE, 400 ×); D: Small pericryptal granuloma in the colonic mucosa of a patient with CD (HE, 100 ×).
SURGERY
In India, due to a high prevalence of TB, the diagnosis of CD is often delayed. In one report nearly a quarter of patients with CD were being treated as tuberculosis[60]. In a study published from India of 28 patients undergoing surgery for CD, elective surgery was performed in 23 and emergency intervention was required in 5. The commonest indication was subacute intestinal obstruction (53%), followed by enteroenteric and enterocutaneous fistulae (10.7%), chronic gastrointestinal blood loss (7%) and protein losing enteropathy (7%). The emergency indications included perforation and peritonitis (14%) and massive GI bleed (4%). Two patients required surgery for gastric outlet obstruction (4%). Eleven patients had combinations of pathology, such as stricture with fistula or perforations. Table 2 shows the clinical and operative findings of 68 patients who underwent surgery for CD and 41 patients for TB in a tertiary referral centre in South India. Indications for surgery in TB were diagnosis and relief of intestinal obstruction. In this study as in previous studies[7], fever, altered bowel habits, clinical presentation as recurrent intestinal obstruction, diffuse small bowel involvement with multiple strictures and deep linear ulcers/cobblestone appearance of bowel were significantly more common in CD than in TB. Conversely, pulmonary involvement, abdominal distension, ascites, peritoneal nodules and terminal ileal/ileocolic involvement without multiple strictures were significantly more common in TB.
Table 2.
Clinical parameters and operative findings of 68 surgical patients with Crohn’s and 41 patients with intestinal tuberculosis n (%)
| Parameter | Crohn’s disease (n = 68) | Intestinal Tuberculosis (n = 41) | P value1 |
| Clinical parameters | |||
| Male:female | 38:30 | 28:13 | NS |
| Mean age (yr) | 31.2 (16-52) | 36.8 (23-64) | NS |
| Fever | 17 (25) | 28 (68) | < 0.010 |
| Pain | 50 (73) | 26 (63) | NS |
| Altered bowel habits | 46 (67) | 14 (34) | < 0.001 |
| Fistula in ano | 7 (12) | 1 (2.4) | NS |
| Anemia | 34 (50) | 28 (68) | NS |
| Edema | 22 (32) | 14 (34) | NS |
| Growth retardation | 14 (20) | 4 (9.7) | NS |
| Treated as tuberculosis | 18 (26) | 8 (19) | NS |
| Pulmonary involvement | 6 (8.2) | 14 (34) | < 0.010 |
| Abdominal distension | 18 (26) | 19 (46) | < 0.050 |
| Abdominal lump | 7 (12) | 8 (19) | NS |
| Recurrent intestinal obstruction | 40 (59) | 14 (34) | < 0.020 |
| Operative findings | |||
| Peritoneal nodules | 15 (22) | 32 (78) | < 0.001 |
| Ascites | 19 (27) | 28 (68) | < 0.001 |
| Nodules over bowel/mesentery | 14 (20) | 14 (34) | NS |
| Site of involvement: | |||
| Diffuse small bowel | 22 (32) | 6 (14.6) | < 0.050 |
| Jejunum | 14 (20) | 6 (14.6) | NS |
| Ileum | 44 (64) | 32 (78) | NS |
| Colon | 6 (8.8) | 2 (4.8) | NS |
| Small bowel and colon | 18 (26) | 3 (7.3) | < 0.020 |
| Multiple strictures | 44 (64) | 4 (9.7) | < 0.001 |
| Skip lesions | 17 (25) | 4 (9.7) | NS |
| Internal fistula | 14 (20) | 1 (2.4) | < 0.01 |
| Mesenteric fat creeping | 44 (64) | 28 (51) | NS |
| Shortened mesentery | 18 (26) | 14 (34) | NS |
| Aphthoid ulcers | 32 (47) | 15 (36) | NS |
| Deep linear ulcers | 40 (59) | 8 (19) | < 0.001 |
| Cobblestone appearance | 44 (64) | 7 (17) | < 0.001 |
| Stricture | 40 (59) | 18 (44) | NS |
P value: by χ2. NS: Not significant.
ROLE OF THERAPY AND FOLLOW UP
Even when the best available diagnostic modalities are utilized, the differentiation of TB from CD remains a problem in 10%-15% of patients in India. Four decades ago, it was usual for these patients to have received antituberculous treatment (ATT) for two years and the individuals who did not respond to such treatment were then diagnosed as having CD. However, advances in diagnosis and increasing experience have allowed Indian gastroenterologists to make a diagnosis of CD in the first instance. Today, nearly half of our patients with CD continue to have received ATT prior to the establishment of the diagnosis of CD. Clearly, a good response to ATT, confirmed by endoscopic and histological clearance of disease, establishes and confirms the diagnosis of TB. Conversely, a poor response to ATT could indicate that the diagnosis is really CD, but could also represent non-responsive TB or drug-resistant TB. An understanding of the intestinal response to therapy of TB and of CD is therefore basic to the use of therapy in differentiating these two diseases.
Use of the directly observed treatment, short course (DOTS) strategy for 6 mo has become standard in the treatment of TB in India. In patients with newly diagnosed pulmonary TB, the “cure” rate after DOTS ranges from 75%-92%[61,62]. Treatment success in extrapulmonary TB was 91% in one study, but this study did not further categorize extrapulmonary TB[62]. In a study from Kerala of 47 patients treated with either DOTS or daily chemotherapy, complete mucosal healing was noted at colonoscopy in 35 at 2 mo and in all 47 at 6 mo[63]. However, biopsies were not taken from these patients during follow up nor was there any long term follow up of the treated individuals. Similar observations have been made of mucosal healing soon after commencement of ATT in colonic TB, but the lack of long term follow up - to ensure that disease does not recur - is a drawback of these studies[64]. In our anecdotal experience, it is common for a proportion of patients to have recurrent disease one to five years after cessation of ATT. At this point it is often difficult to decide whether the patient has recurrence of TB or whether the patient is actually suffering from CD. Drug resistance is increasingly common in strains of MTB and may contribute to recurrent or persistent disease in patients correctly diagnosed as having TB but not showing clinical, endoscopic or histological response to treatment with first line chemotherapy for TB. Multi-drug resistance (MDR) has been observed in 2.4% to 13.2% of strains of MTB isolated from newly diagnosed pulmonary TB patients and in 17.4% to 25.5% of previously treated patients[65,66]. Extensive drug resistance (XDR) is found almost exclusively in previously treated patients and accounts for about 6% of MDR TB[67]. Statistics regarding prevalence of MDR and XDR strains in intestinal TB are not available from India; however, in one series of 30 patients with colonic TB in Taiwan, 4 (13%) had MDR TB[68].
Studies carried out in the last three decades clearly demonstrate that CD does not respond to conventional ATT including isoniazid, rifampicin and ethambutol[69,70]. Prolonged treatment for Mycobacterium avium subsp. paratuberculosis with clarithromycin, rifabutin and clofazimine did lead to improvements in disease activity in patients with CD, but such improvement was not sustained[71].
In summary, the response to an adequate course of ATT should differentiate patients with TB from CD in instances when this becomes necessary. Such response should be assessed by clinical and biochemical parameters, but also by evidence of mucosal healing at endoscopy and on segmental mucosal biopsies. A proportion of patients with intestinal TB (amounting in our experience to about 10%) will not show the desired response and may then be incorrectly diagnosed as having CD. Longer term follow up in these patients will eventually reveal the correct diagnosis.
CONCLUSION
In conclusion, differentiating intestinal TB from CD in countries like India, where both diseases are prevalent, is an important clinical problem. A combination of a good clinical history with colonoscopy, biopsies, cultures, and barium or simple CT studies can be utilized to make a diagnosis in the majority of cases. This article has highlighted important parameters that differentiate intestinal TB from CD in each of these diagnostic modalities. The role of newer techniques, such as capsule endoscopy, single and double balloon enteroscopy, CT enteroclysis, PCR and immunological assays for MTB, has also been highlighted. An adequate course of antituberculous therapy and longer term follow up may become necessary to differentiate patients with TB from CD in some instances. An understanding of the intestinal response to treatment of TB and of CD is, however, fundamental to the use of therapy in differentiating these two diseases.
Acknowledgments
Ghoshal U would like to acknowledge the help of Ghoshal UC, Phillip M would like to acknowledge the help of Prakash K and Zacharias P, and Reddy DN would like to acknowledge the contribution of Rajesh Gupta towards the preparation of the manuscript.
Footnotes
Peer reviewer: Jorgen Rask-Madsen, MD, FRCP, Professor of Gastroenterology, Department of Gastroenterology, Herlev Hospital, Skodsborg Strandvej 280A, 2942, Herlev, DK-2730, Denmark
S- Editor Tian L L- Editor Logan S E- Editor Ma WH
References
- 1.Pulimood AB, Peter S, Ramakrishna B, Chacko A, Jeyamani R, Jeyaseelan L, Kurian G. Segmental colonoscopic biopsies in the differentiation of ileocolic tuberculosis from Crohn's disease. J Gastroenterol Hepatol. 2005;20:688–696. doi: 10.1111/j.1440-1746.2005.03814.x. [DOI] [PubMed] [Google Scholar]
- 2.Lakatos PL. Recent trends in the epidemiology of inflammatory bowel diseases: up or down? World J Gastroenterol. 2006;12:6102–6108. doi: 10.3748/wjg.v12.i38.6102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Pulimood AB, Ramakrishna BS, Kurian G, Peter S, Patra S, Mathan VI, Mathan MM. Endoscopic mucosal biopsies are useful in distinguishing granulomatous colitis due to Crohn's disease from tuberculosis. Gut. 1999;45:537–541. doi: 10.1136/gut.45.4.537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Pai CG, Khandige GK. Is Crohn's disease rare in India? Indian J Gastroenterol. 2000;19:17–20. [PubMed] [Google Scholar]
- 5.Almadi MA, Ghosh S, Aljebreen AM. Differentiating intestinal tuberculosis from Crohn's disease: a diagnostic challenge. Am J Gastroenterol. 2009;104:1003–1012. doi: 10.1038/ajg.2008.162. [DOI] [PubMed] [Google Scholar]
- 6.Epstein D, Watermeyer G, Kirsch R. Review article: the diagnosis and management of Crohn's disease in populations with high-risk rates for tuberculosis. Aliment Pharmacol Ther. 2007;25:1373–1388. doi: 10.1111/j.1365-2036.2007.03332.x. [DOI] [PubMed] [Google Scholar]
- 7.Amarapurkar DN, Patel ND, Rane PS. Diagnosis of Crohn's disease in India where tuberculosis is widely prevalent. World J Gastroenterol. 2008;14:741–746. doi: 10.3748/wjg.14.741. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Patel N, Amarapurkar D, Agal S, Baijal R, Kulshrestha P, Pramanik S, Gupte P. Gastrointestinal luminal tuberculosis: establishing the diagnosis. J Gastroenterol Hepatol. 2004;19:1240–1246. doi: 10.1111/j.1440-1746.2004.03485.x. [DOI] [PubMed] [Google Scholar]
- 9.Hou JK, El-Serag H, Thirumurthi S. Distribution and manifestations of inflammatory bowel disease in Asians, Hispanics, and African Americans: a systematic review. Am J Gastroenterol. 2009;104:2100–2109. doi: 10.1038/ajg.2009.190. [DOI] [PubMed] [Google Scholar]
- 10.Kim BG, Kim YS, Kim JS, Jung HC, Song IS. Diagnostic role of anti-Saccharomyces cerevisiae mannan antibodies combined with antineutrophil cytoplasmic antibodies in patients with inflammatory bowel disease. Dis Colon Rectum. 2002;45:1062–1069. doi: 10.1007/s10350-004-6361-3. [DOI] [PubMed] [Google Scholar]
- 11.Ghoshal UC, Ghoshal U, Singh H, Tiwari S. Anti-Saccharomyces cerevisiae antibody is not useful to differentiate between Crohn's disease and intestinal tuberculosis in India. J Postgrad Med. 2007;53:166–170. doi: 10.4103/0022-3859.33857. [DOI] [PubMed] [Google Scholar]
- 12.Makharia GK, Sachdev V, Gupta R, Lal S, Pandey RM. Anti-Saccharomyces cerevisiae antibody does not differentiate between Crohn's disease and intestinal tuberculosis. Dig Dis Sci. 2007;52:33–39. doi: 10.1007/s10620-006-9527-0. [DOI] [PubMed] [Google Scholar]
- 13.Leung VK, Law ST, Lam CW, Luk IS, Chau TN, Loke TK, Chan WH, Lam SH. Intestinal tuberculosis in a regional hospital in Hong Kong: a 10-year experience. Hong Kong Med J. 2006;12:264–271. [PubMed] [Google Scholar]
- 14.Balamurugan R, Venkataraman S, John KR, Ramakrishna BS. PCR amplification of the IS6110 insertion element of Mycobacterium tuberculosis in fecal samples from patients with intestinal tuberculosis. J Clin Microbiol. 2006;44:1884–1886. doi: 10.1128/JCM.44.5.1884-1886.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Morgan MA, Horstmeier CD, DeYoung DR, Roberts GD. Comparison of a radiometric method (BACTEC) and conventional culture media for recovery of mycobacteria from smear-negative specimens. J Clin Microbiol. 1983;18:384–388. doi: 10.1128/jcm.18.2.384-388.1983. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Winn W Jr AS, Janda W, Koneman E, Procop G, Schreckenberger P, Woods G. Koneman’s color atlas and textbook of diagnostic Microbiology. Philadelphia: Lippincott Williams & Wilkins; 2006. pp. 1064–1124. [Google Scholar]
- 17.Gan H, Ouyang Q, Bu H, Li S, Chen D, Li G, Yang X. Value of polymerase chain reaction assay in diagnosis of intestinal tuberculosis and differentiation from Crohn's disease. Chin Med J (Engl) 1995;108:215–220. [PubMed] [Google Scholar]
- 18.Amarapurkar DN, Patel ND, Amarapurkar AD, Agal S, Baigal R, Gupte P. Tissue polymerase chain reaction in diagnosis of intestinal tuberculosis and Crohn's disease. J Assoc Physicians India. 2004;52:863–867. [PubMed] [Google Scholar]
- 19.Li JY, Lo ST, Ng CS. Molecular detection of Mycobacterium tuberculosis in tissues showing granulomatous inflammation without demonstrable acid-fast bacilli. Diagn Mol Pathol. 2000;9:67–74. doi: 10.1097/00019606-200006000-00001. [DOI] [PubMed] [Google Scholar]
- 20.Pulimood AB, Peter S, Rook GW, Donoghue HD. In situ PCR for Mycobacterium tuberculosis in endoscopic mucosal biopsy specimens of intestinal tuberculosis and Crohn disease. Am J Clin Pathol. 2008;129:846–851. doi: 10.1309/DKKECWQWMG4J23E3. [DOI] [PubMed] [Google Scholar]
- 21.Kabeer BS, Sikhamani R, Raja A. Comparison of interferon gamma and interferon gamma-inducible protein-10 secretion in HIV-tuberculosis patients. AIDS. 2010;24:323–325. doi: 10.1097/QAD.0b013e328334895e. [DOI] [PubMed] [Google Scholar]
- 22.Ouyang Q, Tandon R, Goh KL, Pan GZ, Fock KM, Fiocchi C, Lam SK, Xiao SD. Management consensus of inflammatory bowel disease for the Asia-Pacific region. J Gastroenterol Hepatol. 2006;21:1772–1782. doi: 10.1111/j.1440-1746.2006.04674.x. [DOI] [PubMed] [Google Scholar]
- 23.Bourreille A, Ignjatovic A, Aabakken L, Loftus EV Jr, Eliakim R, Pennazio M, Bouhnik Y, Seidman E, Keuchel M, Albert JG, et al. Role of small-bowel endoscopy in the management of patients with inflammatory bowel disease: an international OMED-ECCO consensus. Endoscopy. 2009;41:618–637. doi: 10.1055/s-0029-1214790. [DOI] [PubMed] [Google Scholar]
- 24.Leighton JA, Shen B, Baron TH, Adler DG, Davila R, Egan JV, Faigel DO, Gan SI, Hirota WK, Lichtenstein D, et al. ASGE guideline: endoscopy in the diagnosis and treatment of inflammatory bowel disease. Gastrointest Endosc. 2006;63:558–565. doi: 10.1016/j.gie.2006.02.005. [DOI] [PubMed] [Google Scholar]
- 25.Solem CA, Loftus EV Jr, Fletcher JG, Baron TH, Gostout CJ, Petersen BT, Tremaine WJ, Egan LJ, Faubion WA, Schroeder KW, et al. Small-bowel imaging in Crohn's disease: a prospective, blinded, 4-way comparison trial. Gastrointest Endosc. 2008;68:255–266. doi: 10.1016/j.gie.2008.02.017. [DOI] [PubMed] [Google Scholar]
- 26.Jeong SH, Lee KJ, Kim YB, Kwon HC, Sin SJ, Chung JY. Diagnostic value of terminal ileum intubation during colonoscopy. J Gastroenterol Hepatol. 2008;23:51–55. doi: 10.1111/j.1440-1746.2007.05151.x. [DOI] [PubMed] [Google Scholar]
- 27.Misra SP, Misra V, Dwivedi M. Ileoscopy in patients with ileocolonic tuberculosis. World J Gastroenterol. 2007;13:1723–1727. doi: 10.3748/wjg.v13.i11.1723. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Misra SP, Misra V, Dwivedi M, Arora JS, Kunwar BK. Tuberculous colonic strictures: impact of dilation on diagnosis. Endoscopy. 2004;36:1099–1103. doi: 10.1055/s-2004-826046. [DOI] [PubMed] [Google Scholar]
- 29.Danelius M, Ost A, Lapidus AB. Inflammatory bowel disease-related lesions in the duodenal and gastric mucosa. Scand J Gastroenterol. 2009;44:441–445. doi: 10.1080/00365520802647426. [DOI] [PubMed] [Google Scholar]
- 30.Lee YJ, Yang SK, Byeon JS, Myung SJ, Chang HS, Hong SS, Kim KJ, Lee GH, Jung HY, Hong WS, et al. Analysis of colonoscopic findings in the differential diagnosis between intestinal tuberculosis and Crohn's disease. Endoscopy. 2006;38:592–597. doi: 10.1055/s-2006-924996. [DOI] [PubMed] [Google Scholar]
- 31.Makharia GK, Srivastava S, Das P, Goswami P, Singh U, Tripathi M, Deo V, Aggarwal A, Tiwari RP, Sreenivas V, et al. Clinical, endoscopic, and histological differentiations between Crohn's disease and intestinal tuberculosis. Am J Gastroenterol. 2010;105:642–651. doi: 10.1038/ajg.2009.585. [DOI] [PubMed] [Google Scholar]
- 32.Reddy DN, Kaffes AJ, Sriram PVJ, Rao GV. Capsule endoscopic features of Crohn's disease. Dig Endosc. 2004;16:138–142. [Google Scholar]
- 33.Sriram PV, Rao GV, Reddy DN. Wireless capsule endoscopy: experience in a tropical country. J Gastroenterol Hepatol. 2004;19:63–67. doi: 10.1111/j.1440-1746.2004.03220.x. [DOI] [PubMed] [Google Scholar]
- 34.Triester SL, Leighton JA, Leontiadis GI, Gurudu SR, Fleischer DE, Hara AK, Heigh RI, Shiff AD, Sharma VK. A meta-analysis of the yield of capsule endoscopy compared to other diagnostic modalities in patients with non-stricturing small bowel Crohn's disease. Am J Gastroenterol. 2006;101:954–964. doi: 10.1111/j.1572-0241.2006.00506.x. [DOI] [PubMed] [Google Scholar]
- 35.Fidder HH, Nadler M, Lahat A, Lahav M, Bardan E, Avidan B, Bar-Meir S. The utility of capsule endoscopy in the diagnosis of Crohn's disease based on patient's symptoms. J Clin Gastroenterol. 2007;41:384–387. doi: 10.1097/01.mcg.0000225621.02094.8a. [DOI] [PubMed] [Google Scholar]
- 36.Delvaux M, Friedman S, Keuchel M, Hagenmüller F, Weinstein M, Cave D, de Franchis R, Gay G, Korman LY. Structured terminology for capsule endoscopy: results of retrospective testing and validation in 766 small-bowel investigations. Endoscopy. 2005;37:945–950. doi: 10.1055/s-2005-870266. [DOI] [PubMed] [Google Scholar]
- 37.Reddy DN, Sriram PV, Rao GV, Reddy DB. Capsule endoscopy appearances of small-bowel tuberculosis. Endoscopy. 2003;35:99. doi: 10.1055/s-2003-36415. [DOI] [PubMed] [Google Scholar]
- 38.Cello JP. Capsule endoscopy features of human immunodeficiency virus and geographical diseases. Gastrointest Endosc Clin N Am. 2004;14:169–177. doi: 10.1016/j.giec.2003.10.008. [DOI] [PubMed] [Google Scholar]
- 39.Tsujikawa T, Saitoh Y, Andoh A, Imaeda H, Hata K, Minematsu H, Senoh K, Hayafuji K, Ogawa A, Nakahara T, et al. Novel single-balloon enteroscopy for diagnosis and treatment of the small intestine: preliminary experiences. Endoscopy. 2008;40:11–15. doi: 10.1055/s-2007-966976. [DOI] [PubMed] [Google Scholar]
- 40.Yamamoto H, Sekine Y, Sato Y, Higashizawa T, Miyata T, Iino S, Ido K, Sugano K. Total enteroscopy with a nonsurgical steerable double-balloon method. Gastrointest Endosc. 2001;53:216–220. doi: 10.1067/mge.2001.112181. [DOI] [PubMed] [Google Scholar]
- 41.Pasha SF, Leighton JA, Das A, Harrison ME, Decker GA, Fleischer DE, Sharma VK. Double-balloon enteroscopy and capsule endoscopy have comparable diagnostic yield in small-bowel disease: a meta-analysis. Clin Gastroenterol Hepatol. 2008;6:671–676. doi: 10.1016/j.cgh.2008.01.005. [DOI] [PubMed] [Google Scholar]
- 42.Nakamura M, Niwa Y, Ohmiya N, Arakawa D, Honda W, Miyahara R, Matsuura T, Ando T, Maeda O, Itoh A, et al. Small bowel tuberculosis diagnosed by the combination of video capsule endoscopy and double balloon enteroscopy. Eur J Gastroenterol Hepatol. 2007;19:595–598. doi: 10.1097/MEG.0b013e3280ec544c. [DOI] [PubMed] [Google Scholar]
- 43.Ramchandani M, Reddy DN, Gupta R, Lakhtakia S, Tandan M, Rao GV, Darisetty S. Diagnostic yield and therapeutic impact of single-balloon enteroscopy: series of 106 cases. J Gastroenterol Hepatol. 2009;24:1631–1638. doi: 10.1111/j.1440-1746.2009.05936.x. [DOI] [PubMed] [Google Scholar]
- 44.Marshall JB. Tuberculosis of the gastrointestinal tract and peritoneum. Am J Gastroenterol. 1993;88:989–999. [PubMed] [Google Scholar]
- 45.Nagi B, Kochhar R, Bhasin DK, Singh K. Colorectal tuberculosis. Eur Radiol. 2003;13:1907–1912. doi: 10.1007/s00330-002-1409-z. [DOI] [PubMed] [Google Scholar]
- 46.Wills JS, Lobis IF, Denstman FJ. Crohn disease: state of the art. Radiology. 1997;202:597–610. doi: 10.1148/radiology.202.3.9051003. [DOI] [PubMed] [Google Scholar]
- 47.Chernish SM, Maglinte DD, O'Connor K. Evaluation of the small intestine by enteroclysis for Crohn's disease. Am J Gastroenterol. 1992;87:696–701. [PubMed] [Google Scholar]
- 48.Maglinte DD, Gourtsoyiannis N, Rex D, Howard TJ, Kelvin FM. Classification of small bowel Crohn's subtypes based on multimodality imaging. Radiol Clin North Am. 2003;41:285–303. doi: 10.1016/s0033-8389(02)00117-3. [DOI] [PubMed] [Google Scholar]
- 49.Nagi B, Sodhi KS, Kochhar R, Bhasin DK, Singh K. Small bowel tuberculosis: enteroclysis findings. Abdom Imaging. 2004;29:335–340. doi: 10.1007/s00261-003-0115-x. [DOI] [PubMed] [Google Scholar]
- 50.Lundstedt C, Nyman R, Brismar J, Hugosson C, Kagevi I. Imaging of tuberculosis. II. Abdominal manifestations in 112 patients. Acta Radiol. 1996;37:489–495. doi: 10.1177/02841851960373P213. [DOI] [PubMed] [Google Scholar]
- 51.Tandon HD, Prakash A. Pathology of intestinal tuberculosis and its distinction from Crohn's disease. Gut. 1972;13:260–269. doi: 10.1136/gut.13.4.260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Gaffney EF, Condell D, Majmudar B, Nolan N, McDonald GS, Griffin M, Sweeney EC. Modification of caecal lymphoid tissue and relationship to granuloma formation in sporadic ileocaecal tuberculosis. Histopathology. 1987;11:691–704. doi: 10.1111/j.1365-2559.1987.tb02683.x. [DOI] [PubMed] [Google Scholar]
- 53.Price AB, Morson BC. Inflammatory bowel disease: the surgical pathology of Crohn's disease and ulcerative colitis. Hum Pathol. 1975;6:7–29. doi: 10.1016/s0046-8177(75)80107-9. [DOI] [PubMed] [Google Scholar]
- 54.Lockhart-Mummery HE, Morson BC. Crohn’s disease of the large intestine. Gut. 1964;5:493–509. doi: 10.1136/gut.5.6.493. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Pettengell KE, Larsen C, Garb M, Mayet FG, Simjee AE, Pirie D. Gastrointestinal tuberculosis in patients with pulmonary tuberculosis. Q J Med. 1990;74:303–308. [PubMed] [Google Scholar]
- 56.Shah S, Thomas V, Mathan M, Chacko A, Chandy G, Ramakrishna BS, Rolston DD. Colonoscopic study of 50 patients with colonic tuberculosis. Gut. 1992;33:347–351. doi: 10.1136/gut.33.3.347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Tanaka M, Riddell RH. The pathological diagnosis and differential diagnosis of Crohn's disease. Hepatogastroenterology. 1990;37:18–31. [PubMed] [Google Scholar]
- 58.Alvares JF, Devarbhavi H, Makhija P, Rao S, Kottoor R. Clinical, colonoscopic, and histological profile of colonic tuberculosis in a tertiary hospital. Endoscopy. 2005;37:351–356. doi: 10.1055/s-2005-861116. [DOI] [PubMed] [Google Scholar]
- 59.Kirsch R, Pentecost M, Hall Pde M, Epstein DP, Watermeyer G, Friederich PW. Role of colonoscopic biopsy in distinguishing between Crohn's disease and intestinal tuberculosis. J Clin Pathol. 2006;59:840–844. doi: 10.1136/jcp.2005.032383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Prakash K, Varma D, Mahadevan P, Narayanan RG, Philip M. Surgical treatment for small bowel Crohn's disease: an experience of 28 cases. Indian J Gastroenterol. 2008;27:12–15. [PubMed] [Google Scholar]
- 61.Gopi PG, Chandrasekaran V, Subramani R, Santha T, Thomas A, Selvakumar N, Narayanan PR. Association of conversion & cure with initial smear grading among new smear positive pulmonary tuberculosis patients treated with Category I regimen. Indian J Med Res. 2006;123:807–814. [PubMed] [Google Scholar]
- 62.Tahir M, Sharma SK, Rohrberg DS, Gupta D, Singh UB, Sinha PK. DOTS at a tertiary care center in northern India: successes, challenges and the next steps in tuberculosis control. Indian J Med Res. 2006;123:702–706. [PubMed] [Google Scholar]
- 63.Tony J, Sunilkumar K, Thomas V. Randomized controlled trial of DOTS versus conventional regime for treatment of ileocecal and colonic tuberculosis. Indian J Gastroenterol. 2008;27:19–21. [PubMed] [Google Scholar]
- 64.Park YS, Jun DW, Kim SH, Lee HH, Jo YJ, Song MH, Kim NI, Lee JS. Colonoscopy evaluation after short-term anti-tuberculosis treatment in nonspecific ulcers on the ileocecal area. World J Gastroenterol. 2008;14:5051–5058. doi: 10.3748/wjg.14.5051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Jain A, Mondal R, Prasad R, Singh K, Ahuja RC. Prevalence of multidrug resistant Mycobacterium tuberculosis in Lucknow, Uttar Pradesh. Indian J Med Res. 2008;128:300–306. [PubMed] [Google Scholar]
- 66.Ramachandran R, Nalini S, Chandrasekar V, Dave PV, Sanghvi AS, Wares F, Paramasivan CN, Narayanan PR, Sahu S, Parmar M, et al. Surveillance of drug-resistant tuberculosis in the state of Gujarat, India. Int J Tuberc Lung Dis. 2009;13:1154–1160. [PubMed] [Google Scholar]
- 67.Jain A, Mondal R. Extensively drug-resistant tuberculosis: current challenges and threats. FEMS Immunol Med Microbiol. 2008;53:145–150. doi: 10.1111/j.1574-695X.2008.00400.x. [DOI] [PubMed] [Google Scholar]
- 68.Lin PY, Wang JY, Hsueh PR, Lee LN, Hsiao CH, Yu CJ, Yang PC. Lower gastrointestinal tract tuberculosis: an important but neglected disease. Int J Colorectal Dis. 2009;24:1175–1180. doi: 10.1007/s00384-009-0721-3. [DOI] [PubMed] [Google Scholar]
- 69.Peyrin-Biroulet L, Neut C, Colombel JF. Antimycobacterial therapy in Crohn's disease: game over? Gastroenterology. 2007;132:2594–2598. doi: 10.1053/j.gastro.2007.04.027. [DOI] [PubMed] [Google Scholar]
- 70.Thomas GA, Swift GL, Green JT, Newcombe RG, Braniff-Mathews C, Rhodes J, Wilkinson S, Strohmeyer G, Kreuzpainter G. Controlled trial of antituberculous chemotherapy in Crohn's disease: a five year follow up study. Gut. 1998;42:497–500. doi: 10.1136/gut.42.4.497. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Selby W, Pavli P, Crotty B, Florin T, Radford-Smith G, Gibson P, Mitchell B, Connell W, Read R, Merrett M, et al. Two-year combination antibiotic therapy with clarithromycin, rifabutin, and clofazimine for Crohn's disease. Gastroenterology. 2007;132:2313–2319. doi: 10.1053/j.gastro.2007.03.031. [DOI] [PubMed] [Google Scholar]


