Abstract
Current therapies for the autoimmune demyelinating disease multiple sclerosis (MS) target inflammation but do not directly address neuroprotection or lesion repair. Cytokines of the gp130 family regulate survival and differentiation of both neural and immune cells, and we recently identified expression of the family member interleukin-11 (IL-11) in active MS plaques. Here, we show that IL-11 regulates the clinical course and neuropathology of experimental autoimmune encephalomyelitis (EAE), a demyelinating model that mimics many of the clinical and pathologic features of MS. Importantly, the effects of IL-11 are achieved via a combination of immunoregulation and direct neuroprotection. IL-11 receptor-alpha null (IL-11Rα−/−) mice displayed a significant increase in clinical severity and neuropathology of EAE compared with wildtype littermates. Inflammation, demyelination, and oligodendrocyte and neuronal loss were all exacerbated in IL-11Ra−/− animals. Conversely, wildtype mice treated with IL-11 displayed milder clinical signs and neuropathology than vehicle-treated controls. In co-cultures of murine MOG35–55-specific CD4+ T lymphocytes and CD11c+ antigen-presenting cells (APCs), IL-11 treatment resulted in a significant decrease in T cell-derived effector cytokine production. This effect was generated via modulation of CD11c+ APC-mediated lymphocyte activation, and was associated with a decrease in the size of the CD11c+ cell population. Conversely, IL-11 strongly reduced apoptosis and potentiated mitosis in primary cultures of mouse oligodendrocyte progenitors (OPCs). Collectively, these data reveal that IL-11 regulates inflammatory demyelination via a unique combination of immunoregulation and neuroprotection. IL-11 signaling may represent a therapeutic avenue to restrict CNS inflammation and potentiate oligodendrocyte survival in autoimmune demyelinating disease.
Keywords: EAE/MS, Autoimmunity, Inflammation, Neuroimmunology, Cytokines
Introduction
Multiple sclerosis (MS) is an inflammatory disease of the central nervous system (CNS) primarily affecting young adults (1). Its pathology is characterized by leukocyte infiltration, demyelination and oligodendrocyte loss, axonal transection and a reactive astrogliosis (2, 3). It is believed that early neurologic disability in MS is effected by conduction block in demyelinated axons, whereas axonal transection underlies the more permanent deficits observed later in the disease (4). Remyelination of nascent lesions has been observed and is associated with recovery of axonal conduction, but often fails with disease progression (5, 6). Therapies for MS have focused primarily on the immune system, however novel approaches directed at CNS protection and regeneration, in concert with immunoregulation, are principal objectives of current research.
Analysis of cellular and molecular components of the MS lesion has led to significant advances in our understanding of disease pathogenesis. Notably, reactive astrocytes comprise the most prevalent cell type in MS plaques and have been shown to regulate both inflammation and CNS repair (7, 8). Recently, using a genomics-based approach we examined gene expression patterns of human astrocytes treated with cytokines relevant to MS lesion formation (9, 10). In these studies, cytokines including IL-1β, IFNγ and transforming growth factor β1 (TGFβ1) each elicited distinct changes in the astrocytic gene expression profile suggesting functional outcomes. Significantly, both IL-1β and TGFβ1 induced genes of the glycoprotein 130 (gp130) cytokine family (10). Members of this family have previously been implicated as mediators of neural and immune cell differentiation, suggesting potential relevance to autoimmune demyelination (11, 12).
IL-11 was one of the gp130 cytokines identified in our study and it shares characteristics with both immunoregulatory (IL-6) and neuroprotective (LIF, ciliary neurotrophic factor (CNTF)) members of the family. IL-11 has been shown to regulate mononuclear phagocyte activation and also stimulates megakaryocytopoiesis and thrombopoiesis (10, 13–15). In the CNS, IL-11 has been shown to promote neuronal differentiation, and our experiments demonstrated that IL-11 also enhanced oligodendrocyte numbers and myelin formation in vitro (10, 16). In MS lesions, we found that IL-11 was expressed by reactive astrocytes, corroborating our genomics data (10).
In this article, we describe studies investigating the role of IL-11 in experimental autoimmune encephalomyelitis (EAE), a widely accepted animal model of MS. Using loss-of-function and gain-of-function approaches we demonstrate that IL-11Rα−/− mice display exacerbated clinical and pathologic outcomes, whereas mice treated with exogenous IL-11 exhibit markedly milder disease. These effects are achieved via two distinct mechanisms. IL-11 displays potent immunomodulatory effects on CD11c+ APCs, and is also directly trophic for oligodendrocyte progenitors (OPCs). Thus, IL-11 exerts a unique spectrum of immunoregulation and neuroprotection. These effects suggest IL-11 signaling as a potential therapeutic avenue for inflammatory demyelinating disease.
Materials and Methods
Antibodies
A2B5 mouse hybridoma was obtained from the American Type Culture Collection (Manassas, VA), and supernatant (IgM) prepared by standard methods. Other antibodies used for immunocytochemistry and immunohistochemistry: rat anti-CD11b (Invitrogen, Carlsbad, CA), hamster anti-CD11c (BD Pharmingen, San Jose, CA), rabbit anti-fibrinogen (Dako Cytomation, Glostrup, Denmark), O4 mouse IgM (Dr. Peter Davies, AECOM, Bronx, NY); mouse anti-CNPase (IgG1), mouse anti-NeuN (IgG1), rabbit anti-Olig2 (Millipore Chemicon, Temecula, CA); mouse anti-myelin basic protein (MBP), mouse anti-neurofilament H nonphosphorylated (SMI 32, both Covance Sternberger, Berkeley, CA); rabbit anti-MAG (Dr. Jim Salzer, NYU); sheep anti-BrdU (Novus, Littleton, CO); rabbit anti-BrdU (Immunology Consultants, Newberg, OR); goat anti-IL-11 (Santa Cruz Biotechnology, Santa Cruz, CA); mouse anti-PDGFRα (IgG1) (R&D Systems); mouse CC-1, rabbit anti-CD3 (both Abcam, Cambridge, MA); mouse anti-actin (IgG1) (Sigma). Fluorescently-labeled antibodies used for flow cytometry: hamster anti-CD11c, rat anti-CD86, hamster anti-CD80rat anti-CD16/CD32, hamster IgG1, l1 (anti-TNP), rat IgG2a, l (anti-KLH), hamster IgG2, k (anti-KLH), I-A (all BD Bioscience, San Jose, CA). C57BL/6 mice do not express MHC II I-A/I-E, rather just I-A, however an I-A/I-E antibody was used to identify the I-A epitope.
Cytokines
Mouse and human IL-11 were purchased from Peprotech (Rocky Hill, NJ). Protein sequences of the two are 88.9% similar, and pilot experiments showed that both were equally effective in inducing responses in vivo and in all culture systems used in the project in vitro (data not shown). LPS from Salmonella minnesota was purchased from Alexis Biochemicals (Plymouth Meeting, PA).
Mice
IL-11Ra−/− mice backcrossed onto a C57BL/6 background for at least 12 generations were purchased from Jackson Laboratories (Bar Harbor, MN) and bred at MSSM. This genotype was originally generated by Drs. Harshal Nandurkar, Lorraine Robb and C. Glenn Begley (Walter and Eliza Hall Institute, Melbourne, Australia) (17, 18). Genotyping was carried out using PCR, using protocols shown on the JAX mice website (http://jaxmice.jax.org) and primer sequences provided by Dr. Lorraine Robb: IL11Ra-F3 5'-GGC TCC CGT CAT TAC CTA CA-3', IL11Ra-R3 5'-AGC AGT CCT ACC CGC TAC AA-3', IL11Ra-PGK1-R5 5'-ACT TGT GTA GCG CCA AGT GC-3'. C57BL/6 mice were also purchased from Jackson Laboratories.
Experimental Autoimmune Encephalomyelitis
All studies were approved by the MSSM Institutional Animal Care and Use Committee. EAE was induced in IL-11Ra−/− mice and littermate controls, or wildtype C57BL/6 mice (male, 8wk, at least 5 per group per experiment) using immunization with myelin oligodendrocyte glycoprotein (MOG35–55) peptide (MEVGWYRSPFSRVVHLYRNGK; Invitrogen) using a protocol similar to that previously reported (19). Briefly, animals were injected in the left and right rear flanks with 300µg of MOG35–55 (Invitrogen) in complete Freund’s adjuvant (CFA) and given 750ng of Bordetella pertussis toxin (Sigma Aldrich) i.v. at the base of the tail. The day after injection of MOG35–55 was considered day 1. On day 2 mice were given a second i.v. injection of 750ng pertussis toxin. In some experiments, C57BL/6 mice were treated with 50µg/kg recombinant mouse IL-11 (Peprotech) starting on the day when clinical signs were first observed in any animal in the experiment. EAE was scored as: 0, no symptoms; 1, floppy tail; 2, hind limb weakness; 3, hind limb paralysis; 4, forelimb weakness and hind limb paralysis; and 5, death (20).
Tissue culture
To establish cultures of CD11c+ cells or CD4+ cells, spleens from 8wk male C57BL/6 mice were homogenized and incubated for 30min in 2mg/ml collagenase D in DMEM at 37°C, then passed through 40µm mesh. Splenocytes were suspended in MACS Buffer (PBS pH7.2, 0.5% BSA 2mM EDTA) then subjected to magnetic cell sorting with mouse CD11c (N418) MicroBeads (Miltenyi Biotec, Auburn, CA), or untouched magnetic cell sorting with mouse CD4+ T Cell Isolation Kit MicroBeads (Miltenyi Biotec) according to the manufacturer's instructions. Following isolation, cells were cultured in RPMI1640, 10% FCS, 1mM sodium pyruvate 200µM NEAA, 20mM HEPES, 50µM β-mercaptoethanol, 50ug/ml gentamycin. Purity of isolation for both cell types was confirmed as >90% by flow cytometry (see below). For isolation and culture of OPCs, cerebral cortices of P0–P2 rats were homogenized, then A2B5+ Ran2− cells isolated by immunopanning and propagated or differentiated as described (21).
Co-culture studies
CD11c+ cells (2 × 104) were co-cultured with 5 × 104 CD4+ cells in 200µl medium in 96 well plates. Co-cultures were pulsed with 50µg/ml MOG35–55, 10ng/ml mouse IL-11, 5µg/ml PHA or vehicle control for 24–72h. In pre-treatment experiments, CD11c+ cells (2 × 104 cells in 100µl medium) or CD4+ cells (5 × 105 in 1ml medium) were treated with IL-11 (10ng/ml) 24h, then washed 3× with fresh medium. Treated CD11c+ cells were then co-cultured with vehicle-treated CD4+ cells, and vice versa. Co-cultures were treated with MOG35–55 (50ug/ml) upon plating, for 24–72h.
Apoptosis Assay
Cultures were fixed in 4% paraformaldehyde 10min, then washed and permeabilized in PBS 0.3% Triton 10min, and subjected to a TUNEL assay using the In Situ Cell Death Kit (Roche-Applied-Science, Indianapolis, IN) according to the manufacturer's instructions. Cultures were imaged at 20× magnification and photographed using a Zeiss LSM 510 META laser scanning confocal system attached to an Axiovert 200 inverted microscope (Zeiss MicroImaging, Thornwood, NY). Apoptotic cells were counted in at least 5 fields per condition in each experiment by a blinded observer using ImageJ 1.30v software (NIH, Bethesda, MD). Results were expressed as percent of total 4',6'-diamidino-2-phenylindole (DAPI+) cells, and as number of positive cells, and were compared by statistics (see below).
Proliferation Assay
Mitosis was quantified using a CellTiter96 Aqueous One Solution Cell Proliferation Assay (Promega, Madison, WI) according to the manufacturer's instructions.
Multiplex ELISA
Supernatants taken at times shown from cultures or co-cultures treated as described in the text were assayed for the following cytokines using Milliplex mouse cytokine/chemokine multiplex ELISA panels (Millipore) according to the manufacturer's instructions. Milliplex 9-plex: GM-CSF, IFNγ, IL-2, IL-4, IL-5, IL-6, IL-10, TNFα, IL-17. Milliplex 6-plex: IL-1β, IL-6, IL-7, IL-12p40, IL-12p70, TNFα.Multiplex ELISA plates were read using a Luminex 100 multiplex plate reader (Luminex, Austin, TX).
Flow Cytometry
At times stated in the text, unfixed cultures were stained with fluorescently-conjugated antibodies as previously reported, using combinations described. Flow cytometry was performed on a Cytomics FC 500 machine (Beckman Coulter, Fullerton, CA) and analyzed using FlowJo software (Tree Star, Ashland, OR) (22).
Immunocytochemistry
OPC cultures were fixed 10min with 4% paraformaldehyde, and processed for single- or double-immunostaining for A2B5 (1:15), O4 (1:25), CNPase (1:100), Olig-2 (1:100), and BrdU (1:1000) as previously described using combinations described in the text (10). Immunostained cultures were examined and photographed using a Zeiss LSM 510 META laser scanning confocal system attached to an Axiovert 200 inverted microscope (as above), and Z series stacks collected using 1µm on the Z axis and assembled into projections using Zeiss LSM Image Browser software. Differentiation and proliferation of OPCs were quantified in Z-series stacks collected at 20× magnification from cultures immunostained for lineage or differentiation markers and BrdU. Cells positive for each marker were counted in at least 5 stacks per condition per marker in each experiment by a blinded observer using ImageJ 1.30v software. Results were expressed as percent of total (DAPI+) cells, and as number of positive cells, and were compared by statistics (see below).
Immunohistochemistry
At times specified in the text, mice with EAE (IL-11Ra−/−, littermates, and C57BL/6 mice treated as described) and age- and sex-matched controls without EAE were sacrificed by anesthetic overdose and perfused with 4% paraformaldehyde. Brain and spinal cord were removed and processed for cryostat or paraffin embedding. For immunostaining, 20µm sections of lumbar, thoracic and cervical spinal cord and cerebral cortex were rehydrated with PBS 10min, then immunostained using protocols previously described (23), and counterstained with DAPI. Immunostained sections were examined and photographed as above, and Z series stacks collected using 1 µm on the Z-axis and assembled into projections using Zeiss LSM Image Browser software. The number of cells positive for lineage and differentiation markers was counted in Z series stacks at 20× magnification by a blinded observer using ImageJ v1.30 software in lumbar, thoracic and cervical spinal cord sections, at least 5 fields at 20× magnification per animal, 3 animals per genotype or condition per time point, in at least 3 independent experiments per study. Data were expressed as number of cells positive for each marker per unit area (100µm2). To quantify demyelination, the MBP− area in each section was measured in Z series stacks at 10× magnification using ImageJ software v1.30, and expressed as absolute area and as percentage of entire section area. Results from different genotypes or conditions were compared using statistics (see below).
Histopathology
Paraffin-embedded 20µm sections of lumbar, thoracic and cervical spinal cord from animals sacrificed as described above were rehydrated with PBS 10min, stained with hematoxylin and eosin using standard protocols, and examined and photographed on a Zeiss Axioplan microscope (Zeiss MicroImaging) with a Q-Imaging MP3.3 RTV color camera and QED Capture software. Within each section, the area occupied by inflammatory infiltrates (defined as hypercellular perivascular or subpial accumulations of small mononuclear cells) was measured at 10× magnification by a blinded observer using ImageJ software v1.30. Results were expressed as absolute area and as percentage of entire section area. Results from different genotypes or conditions were compared using statistics (see below).
Statistical Analysis
Analyses were performed using Prism software v4.0 (GraphPad Inc., San Diego, CA). Datasets were tested to confirm a Gaussian distribution using D'Agostino and Pearson normality test. For multiple comparisons, one-way ANOVA followed by Bonferroni post-test was used. Student's t test was used to compare two groups of matched samples. Tests used for each experiment are specified in Figure Legends. In all cases, P<0.05 was considered significant.
Results
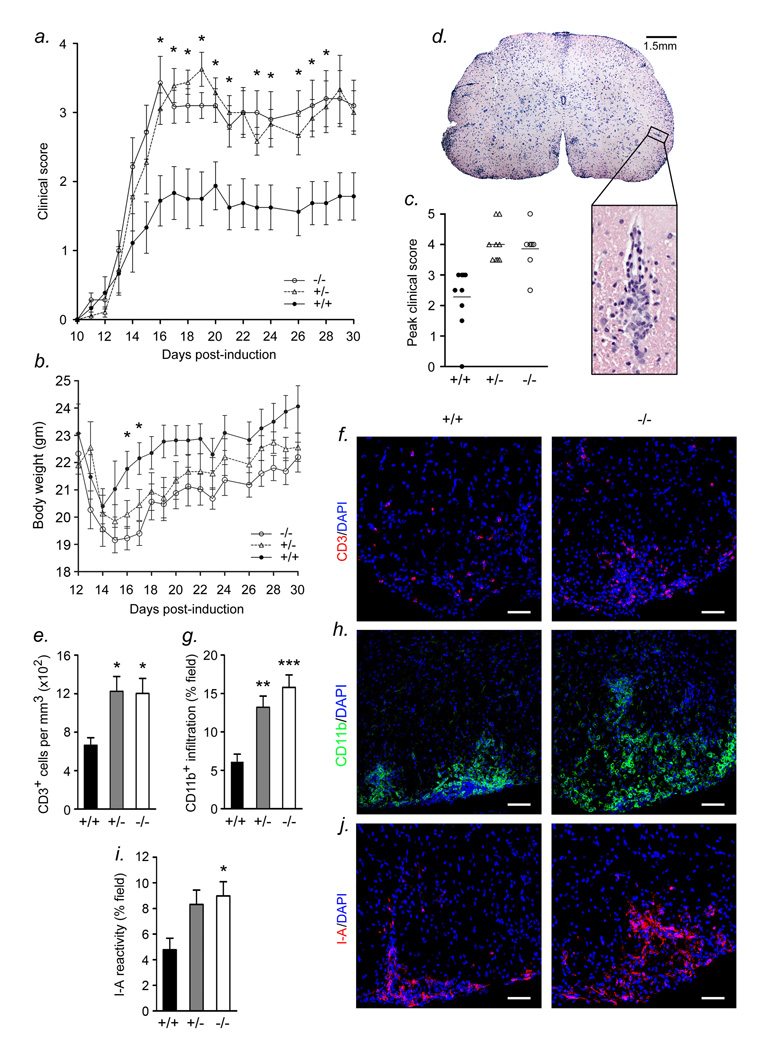
IL-11 signaling regulates the clinical severity and neuropathology of EAE
To investigate the role of IL-11 signaling in autoimmune demyelination, we induced EAE in mice with a selective deletion of IL-11Rα (IL-11Rα−/−) and littermate controls (Figures 1,2). When unchallenged by MOG35–55 sensitization, IL-11 receptor-null mice were healthy and showed no differences in CNS or peripheral immune system composition when compared to wildtype animals. In particular, IL-11Rα−/− and IL-11Rα+/+ animals had similar numbers of Olig2+ oligodendrocyte lineage cells, and both groups exhibited a normal pattern of CNS immunoreactivity for the myelin marker MBP (data not shown). No differences were observed in the number or activation of CD11c+ cells or CD4+ lymphocytes in spleens of mutant animals. However, upon EAE induction we observed significant contrasts between receptor-null and wildtype cohorts (Figure 1). Following sensitization with MOG35–55, mice were monitored daily for weight loss and clinical signs, which consisted of an ascending flaccid paralysis and were evaluated based upon a widely used five-point scoring paradigm (20). The resulting clinical profiles revealed that both IL-11Rα−/− mice and IL-11Rα+/− heterozygotes exhibited neurological signs starting at approximately the same time post-sensitization as wildtype littermates, but that their disease was significantly more severe (Fig. 1a, days 16–21 and 23–28, p<0.05, ANOVA followed by Bonferroni post test). This divergence in clinical scores was evident at 16 days post-sensitization and endured through the endpoint of the experiment (30d, Fig. 1a). Together with a worsened clinical profile, IL-11Ra−/− and IL-11Ra+/− mice exhibited more extensive weight loss than wildtype littermate controls (Fig. 1b days 16–17, p<0.05). Additionally, we compared the highest clinical score for each animal in all three genotypes during the course of the disease (Fig. 1c). Notably, we found that mice within the wildtype control group displayed a mean peak clinical score of 2.33, indicating hindlimb weakness, whereas heterozygotes and mutants scored 4.28 and 3.86 respectively, indicating severe paralysis (Fig. 1c, ANOVA plus Bonferroni post test, IL-11 Rα+/− p<0.01; IL-11Rα−/− p<0.01, at least 7 animals per group per experiment).
Figure 1. IL-11 signaling regulates clinical severity and neuroinflammation in EAE.
(a) IL-11Rα−/− and IL-11Rα+/− mice and wildtype C57BL/6 littermates were sensitized to MOG35–55 as described in the Methods section. Mice developed clinical signs of EAE starting at 10d post-sensitization, characterized by an ascending flaccid paralysis and were scored with widely used 5-point paradigm as described in the Methods section. The severity of disease in both IL-11Rα−/− and IL-11Rα+/− mice was significantly more severe than in controls (16–21d and 23–28d, p<0.05, ANOVA followed by Bonferroni post test). (b) Body weight was also measured daily. Mutants and heterozygotes exhibited greater weight loss during the course of disease when compared with wildtype controls (mutant, 16–17d, p<0.05). (c) Mutant and heterozygous animals also displayed mean peak clinical scores of EAE significantly higher than controls (IL-11 Rα+/− p<0.01; IL-11Rα−/− p<0.01, at least 7 animals per group per experiment). (d) Hematoxylin and eosin-stained section of lumbar spinal cord from 11wk wildtype C57BL/6 mouse 22d post-induction of EAE with MOG35–55 peptide. Typical perivascular mononuclear inflammatory infiltrates are observed in white matter areas, illustrated at higher magnification below. (e–j) Confocal Z-series projections of matched ventrolateral thoracic and lumbar spinal cord sections from 11wk IL-11Rα−/− animals with EAE 18d-22d post-induction (f,h,j, right panels), heterozygotes, or wildtype littermate controls (left panels), immunostained for CD3 (f), CD11b (h), or I-A (j) and quantitated by morphometric analysis as described in the Methods section (e,g,i). Sections from IL-11Rα−/− animals display more extensive inflammation than controls, including potentiated infiltration by CD3+ lymphocytes (e,f), and enhanced parenchymal immunoreactivity for the mononuclear phagocyte marker CD11b (g,h) and I-A (MHCII) (i,j). (a,b,e,g,i) *p<0.05, **p<0.01, ***p<0.001, ANOVA followed by Bonferroni post test. Results shown are from 3 animals per condition, at least 6 20× fields per animal, and are representative of at least 5 independent experiments. Scalebars, (f,h,j) 70µm.
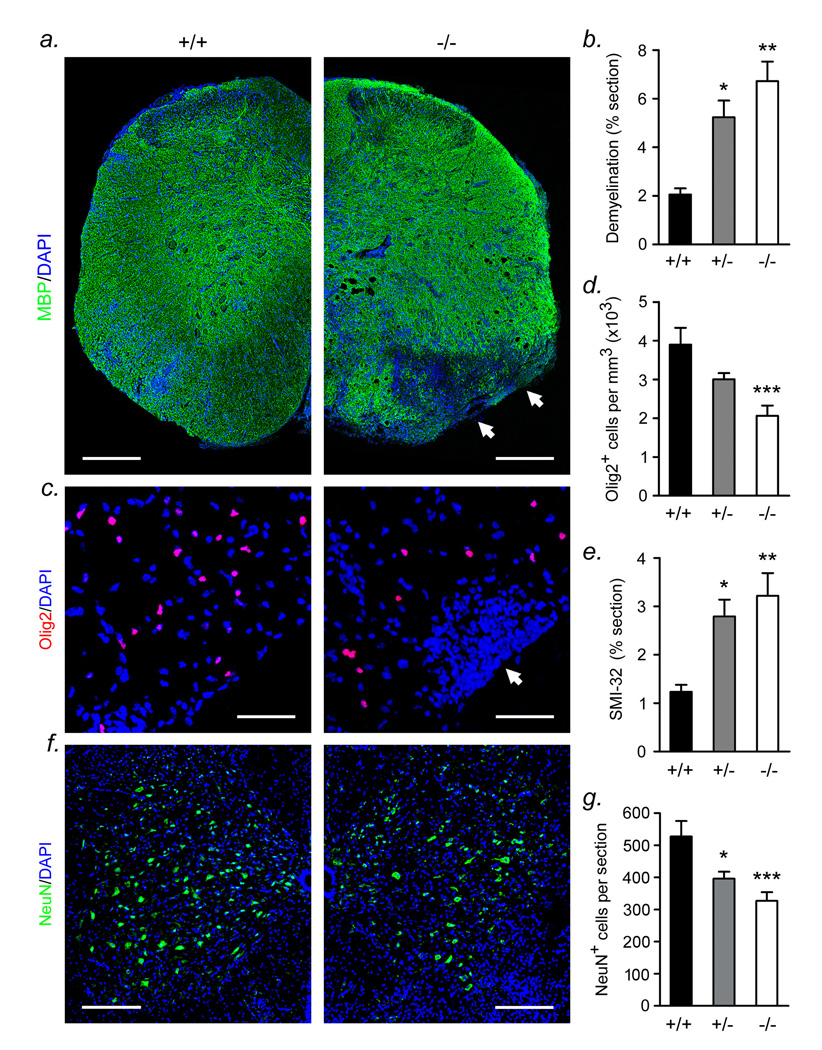
Figure 2. IL-11Rα−/− mice with EAE display exacerbated demyelination and oligodendrocyte and neuronal loss.
Confocal Z-series projections of spinal cord sections from the same IL-11Rα−/−, IL-11Rα+/− and wildtype control mice with EAE described in Figure 1 were immunostained for MBP (myelin), Olig2 (oligodendrocyte lineage), NeuN (neurons), and SMI-32 (axonal dystrophy). Projections were quantitated by morphometry as described in the Methods section (b,d,e,g). Sections from IL-11Rα−/− and heterozygous mice display more extensive demyelination than controls (a,b). Spinal cord sections from wildtype controls contained distinct areas of myelin loss, whereas mutant and heterozygous animals exhibited more confluent demyelination (a, arrows), which was typically observed in areas of hypercellularity corresponding to inflammatory cell infiltration. IL-11Rα−/− samples also exhibited more extensive oligodendrocyte loss than wildtype littermates (c,d), which similarly corresponded to hypercellular regions (c, arrows). Quantification of axonal dystrophy using SMI-32 immunostaining demonstrated that spinal cord sections from mutant and heterozygous animals displayed greater axonal damage than controls (e). Immunostaining for the neuronal marker NeuN also revealed a significant decrease in neuronal numbers in the spinal cord of IL-11Rα−/− and IL-11Rα+/− samples when compared with wildtype controls (f,g). (b,d,e,g) *p<0.05, **p<0.01, ***p<0.001, ANOVA followed by Bonferroni post test. Results shown are from 3 animals per condition, at least 6 20× fields per animal, and are representative of at least 5 independent experiments. Scalebars, (a) 200µm; (c) 50µm; (f) 100µm.
To investigate the pathology associated with these contrasting clinical deficits, the most severe animals from each cohort were sacrificed during the acute clinical episode of disease at 18–22d post-sensitization. Sections of thoracic and lumbar spinal cord from animals in each group were subjected to immunohistochemistry for markers of leukocyte infiltration and CNS inflammation (CD3, CD11b, I-A and fibrinogen). Sections were also immunostained for myelin (MBP), oligodendrocyte lineage cells (Olig2), neurons (NeuN) and SMI-32, a marker of axonal dystrophy (24). Stained sections were imaged using confocal microscopy and results were quantified by computer-assisted morphometry (see Materials and Methods, at least 3 animals per genotype, at least 3 sections per animal and 5 representative image fields per section).
Typical pathology of EAE was observed in IL-11Rα−/− and IL-11Rα+/+ CNS tissue, including perivascular infiltration of mononuclear inflammatory cells (Fig. 1d) and CNS demyelination (see Figure 2). Quantitative analysis of immunostained sections revealed that inflammation was significantly more extensive in IL-11Rα−/− mice and heterozygotes than in wildtype littermates (Figs. 1d–j). In mutant and heterozygote spinal cord sections, infiltration of CD3+ T lymphocytes was more pronounced than in controls (Figs. 1e,f, p<0.05, ANOVA plus Bonferroni post test). Activated mononuclear phagocytes (CD11b+) were also more numerous in both IL-11Rα−/− and IL-11Rα+/− spinal cord than in controls (Figs. 1g,h, mutant p<0.001, heterozygote p<0.01). Additionally, increased numbers of MHCII-expressing cells (assessed by I-A immunoreactivity), which are likely (although not conclusively) activated antigen presenting cells, were observed in mutant sections (Figs. 1i,j, p<0.05). A trend towards increased I-A immunoreactivity was also observed in heterozygotes but did not reach significance (Fig. 1i). Collectively, these studies revealed exacerbation of CNS inflammation in animals with defective IL-11 signaling. These changes included elements of both the innate and adaptive arms of the immune system.
In order to assess IL-11Rα expression in these animals, we performed immunocytochemistry on immune cells from IL-11Rα+/+, IL-11Rα+/−, and IL-11Rα−/− mice. CD11c+ APCs isolated from spleens of unchallenged 8 week old male mice of each genotype were stained for IL-11Rα, I-A, and DAPI (Supplementary Figure 1). IL-11Rα immunoreactivity localized to the surface of CD11c+ cells from wildtype mice (Suppl.Fig.1a). Conversely, compatible with previous reports, cells from heterozygotes displayed lower level expression of the receptor (Suppl.Fig.1b), and IL-11Rα immunoreactivity was absent from IL-11Rα−/− CD11c+ APCs (Suppl.Fig.1c) (17, 25). Cell surface expression of I-A was similar in all three genotypes (Suppl.Fig.1a–c).
Analysis of sections stained for lineage-specific and myelin markers revealed that the increase in CNS inflammation observed in IL-11Rα−/− and heterozygote animals was associated with exacerbated demyelination and oligodendrocyte loss, together with axonal transection and loss of neurons (Figure 2). Whereas wildtype thoracolumbar spinal cord contained distinct areas of myelin loss (as assessed by immunostaining for MBP) in subpial and perivascular white matter, spinal cord tissue from mutant and heterozygous animals exhibited more confluent demyelination (Figs. 2a,b), which was typically observed in areas of hypercellularity corresponding to inflammatory cell infiltration. Quantitation of these changes demonstrated that loss of myelin was significantly more extensive in IL-11Rα−/− and IL-11Rα+/− spinal cord tissue sections than in IL-11Rα+/+ littermates (Fig. 2b, mutant p<0.01, heterozygote p<0.05). Moreover, the number of Olig2+ oligodendrocytes per section was also reduced in IL-11Rα−/− spinal cord compared with controls (Figs. 2c,d, p<0.05), with loss of Olig2+ cells typically being observed in hypercellular areas of white matter (Fig. 2c). A trend towards decreased Olig2+ cells was also observed in heterozygotes, but did not reach significance (Fig. 2d). Moreover, staining of tissue sections with SMI-32, showed a greater extent of axonal damage in mutant and heterozygous animals compared with wildtype littermate controls (Fig. 2e, mutant p<0.01, heterozygote p<0.05). Staining for the neuronal marker NeuN also revealed a significant decrease in neuronal numbers in spinal cord tissue of IL-11Rα−/− and IL-11Rα+/− animals compared with wildtype controls (Figs. 2f,g, mutant p<0.001, heterozygote p<0.01). Collectively, these findings show that loss of IL-11 signaling is associated with intensified clinical deficits, heightened CNS inflammation, and more extensive demyelination and neurodegeneration.
IL-11 reduces apoptosis and potentiates mitosis in OPC cultures
To define the mechanisms underlying these effects, we performed parallel studies in vitro. Since demyelination and oligodendrocyte loss were potentiated in IL-11Rα−/− mice with EAE induced by MOG35–55 sensitization, we investigated whether IL-11 is directly protective for Olig2+ cells using primary cultures of OPCs (Figure 3). We also examined immunoregulatory effects of IL-11 in co-cultures of MOG35–55-specific CD4+ lymphocytes and CD11c+ APCs, since spinal cord infiltration of these cell types was enhanced in IL-11Rα−/− mice with EAE (Figure 4).
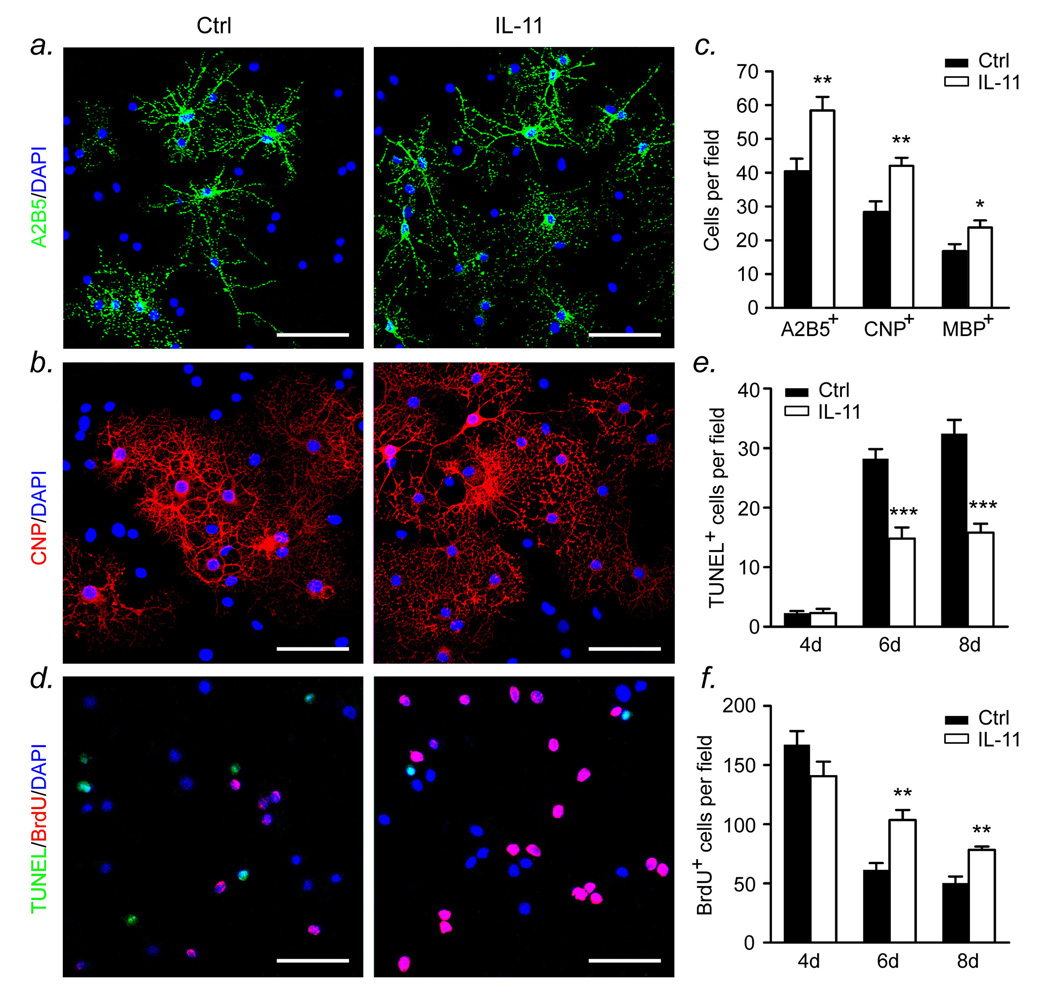
Figure 3. IL-11 reduces apoptosis and potentiates mitosis in OPC cultures.
(a–c) Rat OPCs (A2B5+, Ran2−) were purified from P1 cortices as described in the Methods section. Cultures were left to differentiate in serum-free medium for 5d in the presence of 10ng/ml IL-11 or vehicle control, then fixed and immunostained for differentiation markers. Morphometric analysis, as described in the Methods section, revealed that after 5d, IL-11-treated cultures contained more oligodendrocyte lineage cells of all differentiation stages than controls, including A2B5+ OPCs (a,c), CNPase+ arborized oligodendrocytes (b,c), and mature MBP+ cells (c). *p<0.05, **p<0.01, ***p<0.001, Student’s t test. (d–f) Rat P1 OPCs were purified as above, then left to differentiate for 4, 6 or 8d in the presence of 10ng/ml IL-11 or vehicle control. Cultures were then fixed, and apoptosis was quantified by TUNEL immunostaining (d,e) and proliferation was quantified using BrdU labeling in parallel studies on the same cultures (d,f). Data shown in panel (d) are from 6d. In control cultures, at 4d few cells were TUNEL+ (e) whereas large numbers of cells were mitotic as assessed by BrdU labeling (f). Conversely, at 6d and 8d apoptosis was more prevalent, whereas proliferation was less extensive (e,f). Treatment with IL-11 was associated with significantly reduced apoptosis and potentiated mitosis at both 6d and 8d (e, 6d and 8d p<0.001; f, 6d and 8d p<0.01, Student’s t test). Scale bars, (a,b,d) 40µm. Data for all panels are representative of findings from at least 3 independent experiments using separate cultures.
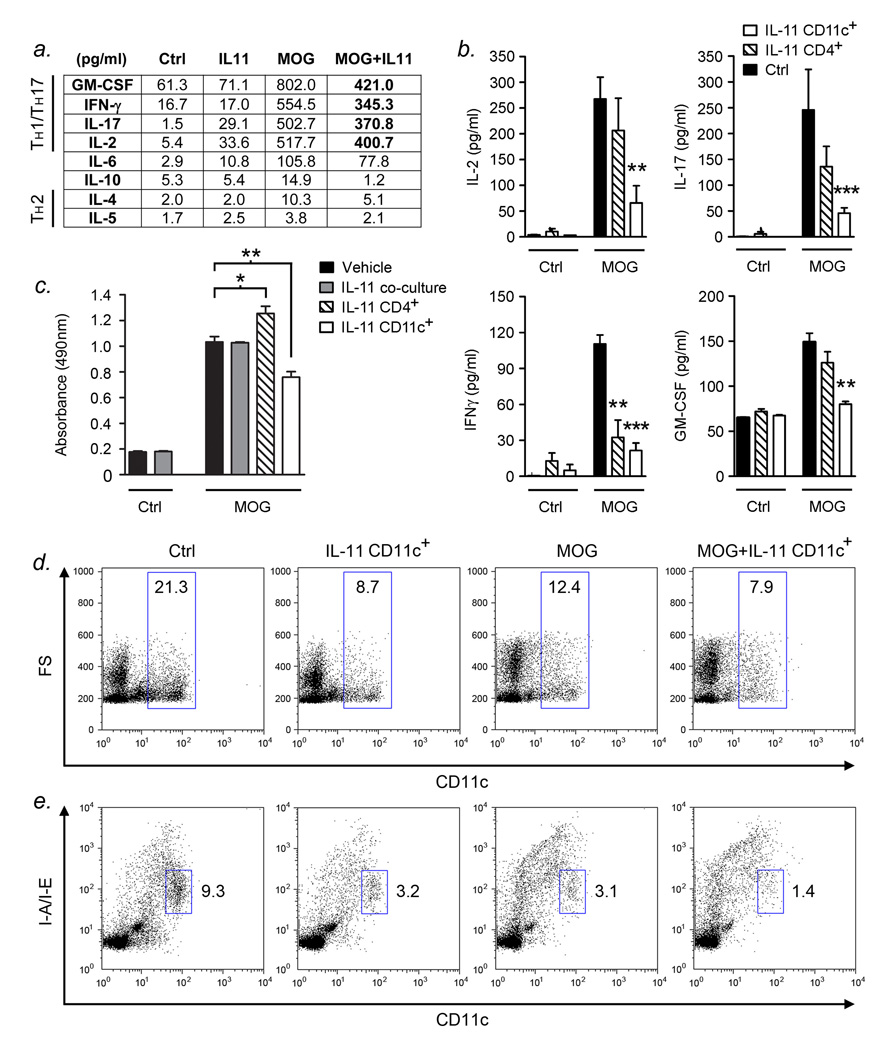
Figure 4. IL-11 reduces CD4+ lymphocyte activation via inhibitory effects on CD11c+ cells.
(a) CD4+ lymphocytes and CD11c+ cells were isolated as described in the Methods section and co-cultured for 72h. MOG35–55-pulsed cultures exhibited a significant increase in production of the TH1/TH17 cytokines GM-CSF, IFNγ, IL-17, and IL-2, but no induction of IL-10 or the TH2 cytokines, IL-4 and IL-5. Treatment with 10ng/ml IL-11 reduced MOG35–55-driven production of all TH1/TH17 cytokines assayed by approximately 25–50%. (b) Co-cultures containing IL-11 pretreated CD11c+ cells and vehicle pretreated CD4+ lymphocytes exhibited a pronounced reduction of all TH1/TH17 cytokines assayed (b, *p<0.05, **p<0.01, ***p<0.001, ANOVA plus Bonferroni post test). In contrast, the effect of IL-11 pretreatment of CD4+ lymphocytes was weaker and reached significance only for IFN-γ (b, IFN-γ p<0.05). (c) In the absence of IL-11 treatment, MOG35–55-pulsed co-cultures displayed a significant increase in cell number after 72h as assessed by MTS tetrazolium reduction assay. No difference in proliferation was observed in co-cultures co-treated with IL-11. Conversely, IL-11 pretreatment of CD11c+ cells resulted in significantly decreased proliferation (IL-11 CD11c+ p<0.01, ANOVA plus Bonferroni post test), while CD4+ lymphocyte pretreatment yielded an increase in cell number (IL-11 CD4+ p<0.05). (d,e) Co-cultures containing IL-11 pretreated CD11c+ cells were analyzed at 48h using flow cytometry. CD11c+ cells made up a smaller percentage of the total cell population in MOG35–55-pulsed cultures compared with unstimulated controls (12.4%, versus 21.3%), due to clonal expansion of MOG35–55-specific memory T lymphocytes (d). IL-11 pretreatment of CD11c+ cells in stimulated co-cultures was associated with a further decrease in the relative number of CD11c+ cells (7.9%, versus 12.4%) (d). In co-cultures absent of MOG35–55, IL-11 pretreatment of CD11c+ APCs also resulted in a significant reduction in the relative number of CD11c+ cells in resulting cultures (8.7% of co-culture cells) compared to untreated controls (21.3%) (d). Analysis of I-A expression in these co-cultures similarly demonstrated that IL-11 pretreatment of CD11c+ cells was associated with a decrease in the relative number of I/A-I/E+ CD11c+ cells in both unstimulated and MOG35–55-pulsed co-cultures (e). Data for all panels are representative of findings from at least 3 independent experiments using separate cultures.
In experiments investigating effects on oligodendrocyte lineage cells, primary cultures of A2B5+Ran2− OPCs were purified from P1 mouse cortex as previously described, then left to differentiate in serum-free medium in the presence of recombinant IL-11 (1–100ng/ml, most commonly 10ng/ml) or vehicle control for up to 5d (21) (Figure 3). Previous work in our laboratory has shown that IL-11Rα is expressed by both rodent and human oligodendrocyte lineage cells, localizing primarily to A2B5+ OPCs (10). In initial studies, IL-11-treated cultures and controls were immunostained for the stage-specific differentiation markers A2B5 (OPCs), CNPase (oligodendrocytes), and MBP (mature oligodendrocytes), and imaged using confocal microscopy. Random 20× Z-series stacks were captured (at least 5 per condition) and cells positive for each marker counted and compared (see Methods section).
These studies showed that after differentiation for 5d, vehicle-treated control cultures contained A2B5+ and CNPase+ cells, together with arborized MBP+ oligodendrocytes (Figs. 3a–c). Cells positive for the OPC marker A2B5 were the most abundant population, while MBP+ oligodendrocytes were the least prominent fraction (Fig. 3c). Treatment with 10–100ng/ml IL-11 was associated with increased numbers of oligodendrocyte lineage cells of all maturational stages, and these differences were significant for each marker tested (Fig. 3c, 10ng/ml illustrated, A2B5 p<0.01, CNPase p<0.01, MBP p<0.05, Student's t test). These findings suggested that IL-11 potentiated survival and/or proliferation within the oligodendrocyte lineage, and in subsequent studies we analyzed both parameters (Figs. 3d–f). Purified primary OPCs left to mature in serum-free medium for 4, 6 or 8d were fixed and apoptosis quantified by TUNEL immunostaining (Figs. 3d,e). Proliferation was quantified using BrdU labeling in parallel studies on the same cultures (Figs. 3d,f). These studies showed that, at 4d, control cultures contained very few TUNEL+ cells (Fig. 3e) whereas large numbers of cells were mitotic as assessed by BrdU labeling (Fig. 3f). Previous work has shown that A2B5+ OPCs comprise the mitotic population in these cultures (26). Conversely, at 6d and 8d apoptosis was more prevalent, whereas proliferation was less extensive (Figs. 3e,f). Treatment with IL-11 was associated with significantly reduced apoptosis and potentiated mitosis at both 6d and 8d (Fig. 3e, 6d and 8d p<0.001; Fig. 3f, 6d and 8d p<0.01, Student’s t test).
Collectively, these experiments reveal that IL-11 is directly trophic for the oligodendrocyte lineage. Recombinant IL-11 slows the increase in apoptosis normally observed over time in OPC cultures, and results in a significant increase in the number of cells of all maturational stages, including proliferating A2B5+ OPCs and mature MBP+ oligodendrocytes.
IL-11 reduces CD4+ lymphocyte activation via inhibitory effects on CD11c+ cells
In parallel with studies on cultured oligodendrocytes, we carried out mechanistic in vitro experiments focused on immune cells relevant to autoimmune demyelination (Figure 4). CD4+ TH1/TH17 lymphocytes are known to play a prominent role in the pathogenesis of EAE and MS, and the importance of CD11c+ APCs in autoimmunity is underscored by their capacity to prime, activate, and even induce tolerance in the CD4+ lymphocyte population (27–30). We co-cultured murine MOG35–55-specific CD4+ lymphocytes with MOG35–55-pulsed CD11c+ APCs, and investigated the effects of IL-11 treatment. CD4+ lymphocytes and CD11c+ cells were isolated from spleens of sensitized and unchallenged 8wk C57BL/6 mice respectively (see Methods section) and co-cultured in the presence of MOG35–55 and 10ng/ml IL-11 or vehicle control for 48–72h. Cytokine production, proliferation and surface molecule expression were then quantified.
We initially examined the cytokine content of co-culture supernatants using a multiplex ELISA assay system (see Methods section), focusing on a panel of TH1/TH17 and TH2 effector cytokines (Fig. 4a). Sensitization with MOG35–55 in complete Freund’s adjuvant results in a delayed-type hypersensitivity response, the production of TH1/TH17 cytokines, and induction of EAE. Thus, these studies showed that, compared with unstimulated controls, MOG35–55-treated cultures exhibited a significant increase in the production of IL-17 and the TH1 cytokines GM-CSF, IL-2 and IFNγ (Fig. 4a). Also assayed were IL-10 and the TH2 cytokines IL-4 and IL-5, however, as expected we found no significant induction of these factors in MOG35–55-pulsed cultures (Fig. 4a). Importantly, in the presence of treatment with 10ng/ml IL-11, production of all TH1/TH17 cytokines assayed (IL-17, GM-CSF, IL-2 and IFNγ) was reduced by approximately 25–50% (Fig. 4a).
To determine whether this change resulted from IL-11-mediated effects on CD11c+ cells or CD4+ lymphocytes, we repeated these studies using a pretreatment paradigm (Fig. 4b). CD4+ lymphocytes and CD11c+ cells isolated as above were independently treated with 10ng/ml IL-11 or vehicle control for 24h. Each population was then washed and resuspended in fresh medium before being co-cultured in the presence of MOG35–55. The design of these experiments provided a means for us to study the effects of IL-11 signaling on co-cultures in the context of lymphocyte versus CD11c+ APC exposure. We observed generally lower cytokine induction in these experiments, presumably due to the pretreatment paradigm. However, these studies clearly showed that both CD11c+ cell pretreatment and CD4+ lymphocyte pretreatment resulted in reduced production of IL-17, GM-CSF, IL-2, and IFN-γ compared with vehicle-treated controls (Fig. 4b). Notably, the CD11c+ pretreated cultures exhibited a much more pronounced reduction (50–80%) of inflammatory cytokines than the CD4+ lymphocyte pretreated cultures (Fig. 4b). The effect of IL-11 CD11c+ pretreatment reached significance for all four of the aforementioned cytokines (GM-CSF, p<0.001; IFNγ, p<0.001; IL-2, p<0.05; IL-17, p<0.05, ANOVA plus Bonferroni post test). By contrast, CD4+ pretreatment reached significance only in the case of IFNγ (p<0.01) (Fig. 4b). Neither CD11c+ pretreatment nor CD4+ pretreatment resulted in effects on the cytokines IL-4, IL-5 and IL-10 (data not shown).
To investigate whether these effects were associated with changes in lymphocyte proliferation, we carried out MTS tetrazolium reduction assays in co-cultures treated with IL-11 using both co-treatment and pretreatment paradigms as described above (Fig. 4c). CD11c+ APCs are terminally differentiated non-proliferating cells, thus increases in cell number in these co-cultures were attributable to clonal expansion of MOG35–55-specific CD4+ lymphocytes (31). In the absence of IL-11 treatment, MOG35–55-pulsed co-cultures displayed a significant increase in cell number after 72h compared with unstimulated controls (Fig. 4c). Interestingly, although co-treatment with IL-11 was associated with reduced production of TH1/TH17 cytokines, we detected no differences in proliferation in co-cultures treated according to this paradigm. Conversely, IL-11 pretreatment of CD11c+ APCs and CD4+ lymphocytes generated differential effects on cell number. When compared with MOG35–55-stimulated untreated co-cultures, IL-11 pretreatment of CD11c+ cells resulted in significantly decreased proliferation (Fig. 4c, p<0.01, ANOVA plus Bonferroni post test), compatible with data from our multiplex ELISA studies. Interestingly, pretreatment of CD4+ lymphocytes resulted in an additional increase in cell number compared with MOG35–55-pulsed controls (Fig. 4c, p<0.05), despite its subtle downregulatory effects on inflammatory cytokine production (compare Figs. 4b, 4c).
To define the nature of IL-11 signaling effects on CD11c+ cells, we repeated CD11c+ pretreatment experiments and analyzed the resulting co-cultures after 48h using flow cytometry (Figs. 4d,e). Co-cultures were stained for CD11c, I-A (MHCII), and the co-stimulatory molecules CD80 and CD86, then subjected to analysis by flow cytometry (see Methods section). In MOG35–55-pulsed cultures, CD11c+ cells made up a smaller percentage of the total cell population (12.4%, versus 21.3%), due to clonal expansion of MOG35–55-specific memory T lymphocytes (Fig. 4d). However, we found that IL-11 pretreatment of CD11c+ cells was associated with a further decrease in the relative number of CD11c+ cells (7.9% versus 12.4%), even though proliferation was reduced in these cultures compared with MOG35–55-pulsed controls (Fig. 4d, compare with Fig. 4c). In co-cultures absent of MOG35–55, IL-11 pretreatment of CD11c+ APCs also resulted in a significant reduction in the relative number of CD11c+ cells (8.7% of co-culture cells) compared to untreated controls (21.3%) (Fig. 4d). Upon analyzing I-A expression in these co-cultures, we observed a similar pattern (Fig. 4e). We found that IL-11 pretreatment of CD11c+ cells was associated with a decrease in the relative number of I-A+ CD11c+ cells, and this finding was observed in both unstimulated and MOG35–55-pulsed cultures (Fig. 4e). Interestingly, although the percentage of I-A+ cells was reduced in cultures exposed to IL-11, we did not detect significant alterations in I-A levels in expressing cells (data not shown). Similar results were observed for the costimulatory molecules CD80 and CD86 (data not shown).
Collectively, these findings demonstrate that IL-11 signaling has potent effects on both CD4+ lymphocytes and CD11c+ APCs. Most notably, IL-11 regulates production of TH1/TH17 effector cytokines, via both direct and indirect pathways. The indirect pathway is the more effectual of the two and results from effects on CD11c+ APCs.
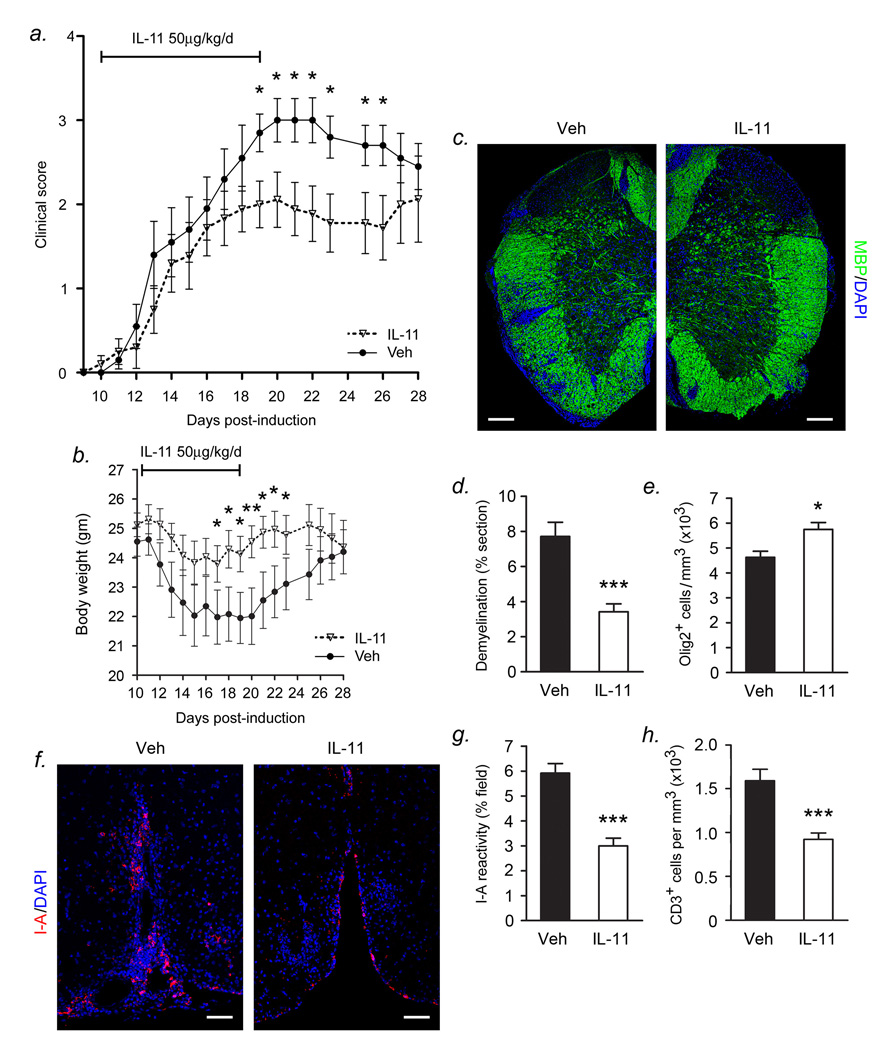
Interleukin-11 treatment mitigates disease severity in EAE
To investigate effects of IL-11 gain-of-function in vivo, we employed a treatment paradigm in which recombinant IL-11 was administered to 8wk C57BL/6 mice sensitized with MOG35–55 (Figure 5). Mice were injected intraperitoneally with IL-11 (25 or 50µg/kg/day) or vehicle control daily for 10d (days 10–19) starting at clinical onset of EAE. Clinical disease and weight loss were evaluated daily as above. These studies showed that treatment with 50µg/kg/day IL-11 was associated with significantly reduced disease severity as assessed by motor deficit (Fig. 5a) and improved retention of body weight (Fig. 5b) compared with vehicle-treated littermate controls (clinical score: days 19–26, p<0.05; body weight:: days 17–19, 21–23, p<0.05, day 20, p<0.01; Students t-test). Noticeable therapeutic effects of IL-11 were observed from day 17 (day 9 of treatment) and these effects endured to day 26 (7 days following cessation of treatment). At day 27 (8 days following cessation of treatment) the mean score of the IL-11 treated group began to increase and converge with that of the control group, suggesting that IL-11 exerts its protective effects in a treatment-dependent fashion (Fig. 5a). Lower doses of IL-11 did not produce significant protection (data not shown).
Figure 5. Interleukin-11 treatment mitigates disease severity in EAE.
(a) C57BL/6 mice, sensitized with MOG35–55 at 8 wks were injected intraperitoneally with IL-11 (50µg/kg/day) or vehicle control daily for 10d (days 10–19) starting at clinical onset of EAE. Clinical deficits were evaluated based upon a widely used scoring paradigm detailed in the Methods section. Treatment with 50µg/kg/day IL-11 was associated with significantly reduced disease severity as assessed by neurologic deficit, compared with vehicle-treated littermate controls (days 19–26, p<0.05; Students t-test). Noticeable therapeutic effects of IL-11 were observed from day 17 (day 9 of treatment) and these effects endured to day 26 (7 days following cessation of treatment). (b) Animals treated with IL-11 also exhibited significantly improved retention of body mass during the course of disease when compared with vehicle treated controls (days 17–19, 21–23, p<0.05, day 20, p<0.01). (c–h) Animals from each cohort were sacrificed during the acute clinical episode (20–22d post-sensitization) and immunohistochemistry was performed on spinal cord tissue sections as in Figure 1 and quantitated by morphometry described in the Methods section. IL-11 treatment was associated with a striking reduction in the extent of demyelination in MBP-immunostained sections when compared with vehicle-treated controls (c,d p<0.001, Student’s t test). IL-11-treated animals also displayed a minor but significant decrease in the loss of Olig2+ oligodendrocyte lineage cells in the spinal cord (e). (f–h) The observed changes in neuropathology accompanied significantly attenuated inflammation in samples from IL-11-treated mice. The presence of I-A+ APCs was significantly reduced in spinal cord sections of IL-11-treated mice compared with vehicle treated controls (f,g p<0.001). Numbers of CD3+ lymphocytes were also significantly decreased (h p<0.001). Results shown are from 3 animals per condition, at least 6 20× fields per animal, and are representative of at least 5 independent experiments. Scalebars, (c) 150µm; (f) 70µm.
To investigate the effects of IL-11 treatment on autoreactive inflammation and CNS pathology, animals from each cohort were sacrificed during the acute clinical episode (20–22d post-sensitization), and immunohistochemistry performed on spinal cord tissue sections as above. As suggested by our functional studies in vitro, we found a striking reduction in the extent of demyelination per section in IL-11-treated animals compared with vehicle-treated controls (Figs. 5c,d, p<0.001, Student’s t test). This was associated with a small but significant effect on the number of Olig2+ oligodendrocyte lineage cells, which were observed in slightly higher numbers in spinal cord from IL-11-treated animals (Fig. 5e). These changes accompanied a significant decrease in inflammation in samples from IL-11-treated mice with EAE (Figs. 5f–h). The presence of I-A+ APCs was significantly reduced in spinal cord sections of IL-11-treated mice compared with vehicle treated controls (Figs. 5f,g, p<0.001). Numbers of CD3+ lymphocytes were also significantly decreased (Fig. 5h, p<0.001). Collectively, the findings of these gain-of-function studies in vivo are compatible with the results of our experiments in vitro. They demonstrate that administration of IL-11 to mice with EAE is associated with amelioration of neurological disease, and diminished inflammation and CNS demyelination.
Discussion
In this study, we have investigated the functional significance of IL-11 signaling in the context of autoimmune demyelinating disease. Our data establish that IL-11 exerts protective effects in EAE via immune system modulation as well as trophic effects on oligodendrocytes. MOG35–55-sensitized IL-11Rα−/− mice displayed significantly worsened clinical signs of EAE compared with IL-11Rα+/+ littermates (Figure 1). This exacerbated clinical outcome was accompanied by heightened CNS inflammation and neuropathology (Figures 1,2). Conversely, IL-11 (50µg/kg/day) treatment of wildtype MOG35–55-sensitized animals resulted in the amelioration of clinical EAE and pathology consistent with disease attenuation (Figure 5). Our in vitro studies revealed that OPCs treated with IL-11 exhibited reduced apoptosis and potentiated mitosis (Figure 3). In contrast to these trophic effects on oligodendrocytes, we found that IL-11 treatment of CD11c+ APCs, when co-cultured with MOG35–55-specific CD4+ lymphocytes, resulted in diminished lymphocyte proliferation and reduced production of TH1/TH17 effector cytokines. This inverse relationship, supportive effects on oligodendroglia versus inhibitory effects on leukocytes, positions IL-11 as a potentially protective factor in inflammatory disease of the mammalian CNS.
IL-11 is member of the gp130 family, a pleiotropic group of cytokines known to modulate proliferation, maturation, and survival in multiple cell lineages (32). Members of the family include IL-6, IL-11, LIF, CNTF, and oncostatin M and all bind to cell surface receptors containing the common signal-transducing subunit gp130 (33). Family members have pro- as well as anti-inflammatory properties and are important regulators of hematopoiesis, as well as innate and adaptive immune responses (32). For example, IL-6 has a mixed history of both promoting and inhibiting inflammation, and is also known as an acute phase reactant that produces fever (34–36). In addition, recent work has shown that IL-6 acts in combination with TGFβ1, a cytokine previously believed to be predominantly anti-inflammatory, to induce TH17 effector cells (37, 38). While IL-6 is known for its potent effects on cells of the immune system, reports of gp130-driven neuroprotection have further encouraged research focus on this family of mediators. CNTF has been shown to promote survival in oligodendrocytes and neurons in addition to preventing BBB disruption (12, 39), and LIF is also known to enhance oligodendrocyte viability in animal models of autoimmune demyelination (11).
IL-11 was originally isolated from bone marrow stromal cells and early studies revealed its potent effects on hematopoiesis (40, 41). In particular, IL-11 stimulates megakaryocytopoiesis and thrombopoiesis, which has resulted in its therapeutic use in patients exhibiting chemotherapy-driven thrombocytopenia (13, 15, 42). In related studies, over-expression of IL-11 in transgenic mice resulted in stimulation of long bone formation with increased cortical thickness and decreased bone loss over time (43). Additional reports have revealed the anti-inflammatory properties of IL-11 in conditions such as mucositis and periodontitis (44, 45). Work by Robb and colleagues has also demonstrated that IL-11 signaling is required for normal uterine decidualization, and that female mice lacking IL-11Rα are infertile (18). Finally, research into CNS neurogenesis has shown that neuronal progenitors within the hippocampus differentiate in response to IL-11 treatment in vitro. This collection of studies, amongst others, illustrates the pleiotropy of IL-11 signaling in mammalian biology.
Employing functional genomics data, we recently discovered that expression of IL-11, along with other gp130 cytokines, was strongly induced in cultures of human astrocytes in response to IL-1β or TGFβ1 (10). Both of these cytokines have previously been implicated in lesion formation in inflammatory CNS diseases including MS (46, 47). We therefore examined brain tissue samples from MS patients and controls and discovered that IL-11 was present at the border of both chronic active and silent MS lesions and that IL-11 immunoreactivity localized to reactive astrocytes in vivo. We also found IL-11Rα expression to co-localize with oligodendrocyte markers in the same tissue sections (10). In the current study, we have examined the functional relevance of these findings in the context of autoimmune demyelinating disease in vivo. Our results are compatible with our initial in vitro findings, which showed that IL-11 potentiates oligodendrocyte survival and maturation in human cultures (10). However, our current data also clearly demonstrate a role for IL-11 in functional regulation of leukocytes relevant to autoreactive inflammation of the CNS. Of particular interest are our results showing modulation of CD11c+ APC function, which support and extend a previous report that IL-11 exerts anti-inflammatory effects on cells of the innate immune system (14).
The mechanism underlying the effects of IL-11 on CD11c+ APCs is presently an area of active research in our laboratory. While the direct impact of IL-11 on CD4+ lymphocyte cytokine production in our experiments was subtle, pretreatment of CD11c+ APCs evoked much more potent suppression of lymphocyte cytokine production in co-cultures. To define the changes elicited by IL-11 on CD11c+ function, we are currently examining three distinct hypotheses. First, our present findings show a reduction in the size of the CD11c+ population in co-cultures containing IL-11-pretreated CD11c+ cells. This may result from directly apoptotic effects of the cytokine, or from the observed reduction in survival factors, such as GM-CSF, in these experiments. Second, IL-11 may suppress activation of CD11c+ APCs, resulting in altered production of cytokines required for amplification of effector CD4+ lymphocytes. Studies to test this hypothesis are planned. Finally, IL-11 may regulate expression of stimulatory, costimulatory or adhesion molecules relevant to efficient antigen presentation by CD11c+ cells. These hypotheses are currently under investigation in our laboratory.
The neuropathologic phenotype of IL-11Rα−/− mice with EAE was also of particular interest to us in the current work. Loss of IL-11Rα expression and signaling was associated with a significant increase in CNS demyelination, potentiated loss of Olig2+ oligodendrocytes, increased axonal dystrophy and extensive neurodegeneration. Whereas loss of myelin in wild-type littermates occurred in discrete perivascular and subpial white matter areas, in IL-11Rα−/− animals we observed more confluent areas of demyelination. Notably, deficiency of just one allele of IL-11Rα in heterozygotes was sufficient to generate comparable effects to that observed in receptor-null mutants, suggesting that partial loss of IL-11 signaling may be nearly as deleterious as complete inactivation. Defining the relative contributions of immunoregulatory versus directly protective effects of IL-11 to the phenotype of IL-11Rα−/− mice and heterozygotes will require refinement of our current experimental paradigm to include the use of cell-type specific loss-of-function studies, and this we are currently pursuing this approach.
A cell type-specific approach would also contribute to our understanding of the results of our gain-of-function studies in vivo, which were compatible with but not the exact converse of the phenotype observed in IL-11Rα−/− animals. Specifically, while we observed a striking reduction in demyelination in mice with EAE that received IL-11 treatment, protection of oligodendrocyte lineage cells in these animals only appeared partial, albeit statistically significant. Although at 19kD IL-11 would not be expected to pass freely through the BBB, mice sensitized to develop EAE using our chosen protocol are known to display extensive histamine-driven BBB disruption (48), providing peripheral factors a potential means of entry into the CNS parenchyma. However, it is difficult to estimate the extent to which systemically administered cytokine entered the CNS in our gain-of-function study. Thus, efficient delivery of therapies based on the IL-11 pathway may require a small molecular weight agonist designed to emulate the receptor binding kinetics of IL-11 while passing freely through the BBB.
Potential therapeutic strategies for MS can be divided into two main areas. In the first are immunomodulatory treatments designed to reduce or prevent the formation of new CNS lesions and hence new clinical episodes. In the second are neuroprotective or regenerative therapies aimed at repairing pre-existing damage. Avenues combining both approaches may represent novel and efficacious treatments for inflammatory CNS demyelination. Our results show that IL-11 has potent anti-inflammatory properties and also acts to support oligodendrocyte populations directly, a spectrum of biological action clearly relevant to the clinical course and neuropathology of EAE. On the basis of our previous findings and the work described in the current manuscript, we suggest that manipulation of IL-11 signaling may represent a potential means of therapy for inflammatory diseases of the CNS, including MS.
Supplementary Material
Spleens were taken from unchallenged male 8wk IL-11Rα−/−, IL-11Rα+/− and IL-11Rα+/+ mice. CD11c+ APCs were isolated from splenocytes and immunostained for IL-11Rα, I-A, and DAPI (a–c). CD11c+ cells from wildtype animals displayed cell surface expression of both IL-11Rα and I-A (a). Cells from heterozygotes exhibited a lower level of IL-11Rα expression than wildtype mice (b). IL-11Rα was absent from the surface of CD11c+ cells from IL-11Rα−/− mice (c). Scalebars, 5µm.
Acknowledgements
We thank Dr. Lorraine Robb of the Walter and Eliza Hall Institute of Medical Research, (Parkville, Victoria Australia) for generating the IL-11Rα−/− strain of mice and Dr. Trevelyan Menheniott of the Murdoch Children’s Research Institute (Parkville, Victoria Australia) for providing a genotyping protocol. We thank Prof. Celia Brosnan at Albert Einstein College of Medicine for EAE induction training and manuscript input. We thank Dr. Antonio Borderia-Giner of the Mount Sinai School of Medicine (MSSM) Department of Microbiology for Milliplex ELISA training. We also thank Dr. Victor Friedrich, Rumana Huq, and Timothy Kang of the MSSM Microscopy Shared Resource Facility.
Abbreviations used in this paper
- BBB
blood-brain barrier
- CNTF
ciliary neurotrophic factor
- DAPI
4',6'-diamidino-2-phenylindole
- EAE
experimental autoimmune encephalomyelitis
- gp130
glycoprotein 130
- IL-11Rα
interleukin-11 receptor alpha
- MBP
myelin basic protein
- MOG35–55
myelin oligodendrocyte glycoprotein 35–55
- MS
multiple sclerosis
- OPC
oligodendrocyte progenitor cell
- TGFβ1
transforming growth factor beta-1
Footnotes
This work was supported by U.S. Public Health Service Grants R01 NS056074 and R01 NS046620 (to G.R.J.), R21 AI077007 (to T.M.M. and C.B.L.), R01 AI041111 (to T.M.M. and C.B.L.), T32-GM-008553-13 (to B.T.G.), National Multiple Sclerosis Society Fellowship FG-1739 (to Y.Z.) and Research Grant RG-3874 (to G.R.J.), and the Jayne and Harvey Beker Foundation (to G.R.J.). The Mount Sinai School of Medicine/Microscopy Shared Resource Facility is supported, in part, with funding from National Institutes of Health/National Cancer Institute Shared Resources Grant R24 CA095823.
Disclosures
The authors declare no conflicts of interest.
References
- 1.Keegan BM, Noseworthy JH. Multiple sclerosis. Annu Rev Med. 2002;53:285–302. doi: 10.1146/annurev.med.53.082901.103909. [DOI] [PubMed] [Google Scholar]
- 2.Hauser SL, Oksenberg JR. The neurobiology of multiple sclerosis: genes, inflammation, and neurodegeneration. Neuron. 2006;52:61–76. doi: 10.1016/j.neuron.2006.09.011. [DOI] [PubMed] [Google Scholar]
- 3.Ridet JL, Malhotra SK, Privat A, Gage FH. Reactive astrocytes: cellular and molecular cues to biological function. Trends. Neurosci. 1997;20:570–577. doi: 10.1016/s0166-2236(97)01139-9. [DOI] [PubMed] [Google Scholar]
- 4.Bruck W, Stadelmann C. The spectrum of multiple sclerosis: new lessons from pathology. Curr. Opin. Neurol. 2005;18:221–224. doi: 10.1097/01.wco.0000169736.60922.20. [DOI] [PubMed] [Google Scholar]
- 5.Prineas JW, Barnard RO, Kwon EE, Sharer LR, Cho ES. Multiple sclerosis: remyelination of nascent lesions. Ann Neurol. 1993;33:137–151. doi: 10.1002/ana.410330203. [DOI] [PubMed] [Google Scholar]
- 6.Smith KJ, Blakemore WF, McDonald WI. The restoration of conduction by central remyelination. Brain. 1981;104:383–404. doi: 10.1093/brain/104.2.383. [DOI] [PubMed] [Google Scholar]
- 7.Bush TG, Puvanachandra N, Horner CH, Polito A, Ostenfeld T, Svendsen CN, Mucke L, Johnson MH, Sofroniew MV. Leukocyte infiltration, neuronal degeneration, and neurite outgrowth after ablation of scar-forming, reactive astrocytes in adult transgenic mice. Neuron. 1999;23:297–308. doi: 10.1016/s0896-6273(00)80781-3. [DOI] [PubMed] [Google Scholar]
- 8.Faulkner JR, Herrmann JE, Woo MJ, Tansey KE, Doan NB, Sofroniew MV. Reactive astrocytes protect tissue and preserve function after spinal cord injury. J. Neurosci. 2004;24:2143–2155. doi: 10.1523/JNEUROSCI.3547-03.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.John GR, Shankar SL, Shafit-Zagardo B, Massimi A, Lee SC, Raine CS, Brosnan CF. Multiple sclerosis: re-expression of a developmental pathway that restricts oligodendrocyte maturation. Nat. Med. 2002;8:1115–1121. doi: 10.1038/nm781. [DOI] [PubMed] [Google Scholar]
- 10.Zhang Y, Taveggia C, Melendez-Vasquez C, Einheber S, Raine CS, Salzer JL, Brosnan CF, John GR. Interleukin-11 potentiates oligodendrocyte survival and maturation, and myelin formation. J. Neurosci. 2006;26:12174–12185. doi: 10.1523/JNEUROSCI.2289-06.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Butzkueven H, Zhang JG, Soilu-Hanninen M, Hochrein H, Chionh F, Shipham KA, Emery B, Turnley AM, Petratos S, Ernst M, Bartlett PF, Kilpatrick TJ. LIF receptor signaling limits immune-mediated demyelination by enhancing oligodendrocyte survival. Nat Med. 2002;8:613–619. doi: 10.1038/nm0602-613. [DOI] [PubMed] [Google Scholar]
- 12.Linker RA, Maurer M, Gaupp S, Martini R, Holtmann B, Giess R, Rieckmann P, Lassmann H, Toyka KV, Sendtner M, Gold R. CNTF is a major protective factor in demyelinating CNS disease: a neurotrophic cytokine as modulator in neuroinflammation. Nat. Med. 2002;8:620–624. doi: 10.1038/nm0602-620. [DOI] [PubMed] [Google Scholar]
- 13.Goldman SJ. Preclinical biology of interleukin 11: a multifunctional hematopoietic cytokine with potent thrombopoietic activity. Stem Cells. 1995;13:462–471. doi: 10.1002/stem.5530130503. [DOI] [PubMed] [Google Scholar]
- 14.Trepicchio WL, Wang L, Bozza M, Dorner AJ. IL-11 regulates macrophage effector function through the inhibition of nuclear factor-kappaB. J. Immunol. 1997;159:5661–5670. [PubMed] [Google Scholar]
- 15.Weich NS, Wang A, Fitzgerald M, Neben TY, Donaldson D, Giannotti J, Yetz-Aldape J, Leven RM, Turner KJ. Recombinant human interleukin-11 directly promotes megakaryocytopoiesis in vitro. Blood. 1997;90:3893–3902. [PubMed] [Google Scholar]
- 16.Mehler MF, Rozental R, Dougherty M, Spray DC, Kessler JA. Cytokine regulation of neuronal differentiation of hippocampal progenitor cells. Nature. 1993;362:62–65. doi: 10.1038/362062a0. [DOI] [PubMed] [Google Scholar]
- 17.Nandurkar HH, Robb L, Tarlinton D, Barnett L, Kontgen F, Begley CG. Adult mice with targeted mutation of the interleukin-11 receptor (IL11Ra) display normal hematopoiesis. Blood. 1997;90:2148–2159. [PubMed] [Google Scholar]
- 18.Robb L, Li R, Hartley L, Nandurkar HH, Koentgen F, Begley CG. Infertility in female mice lacking the receptor for interleukin 11 is due to a defective uterine response to implantation. Nat. Med. 1998;4:303–308. doi: 10.1038/nm0398-303. [DOI] [PubMed] [Google Scholar]
- 19.Chen L, Brosnan CF. Exacerbation of experimental autoimmune encephalomyelitis in P2X7R−/− mice: evidence for loss of apoptotic activity in lymphocytes. J Immunol. 2006;176:3115–3126. doi: 10.4049/jimmunol.176.5.3115. [DOI] [PubMed] [Google Scholar]
- 20.Brosnan CF, Goldmuntz EA, Cammer W, Factor SM, Bloom BR, Norton WT. Prazosin, an alpha 1-adrenergic receptor antagonist, suppresses experimental autoimmune encephalomyelitis in the Lewis rat. Proc. Natl. Acad. Sci. USA. 1985;82:5915–5919. doi: 10.1073/pnas.82.17.5915. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Caporaso GL, Chao MV. Telomerase and oligodendrocyte differentiation. J. Neurobiol. 2001;49:224–234. doi: 10.1002/neu.1077. [DOI] [PubMed] [Google Scholar]
- 22.Yount JS, Kraus TA, Horvath CM, Moran TM, Lopez CB. A novel role for viral-defective interfering particles in enhancing dendritic cell maturation. J. Immunol. 2006;177:4503–4513. doi: 10.4049/jimmunol.177.7.4503. [DOI] [PubMed] [Google Scholar]
- 23.Argaw AT, Zhang Y, Snyder BJ, Zhao ML, Kopp N, Lee SC, Raine CS, Brosnan CF, John GR. IL-1beta regulates blood-brain barrier permeability via reactivation of the hypoxia-angiogenesis program. J. Immunol. 2006;177:5574–5584. doi: 10.4049/jimmunol.177.8.5574. [DOI] [PubMed] [Google Scholar]
- 24.Sternberger LA, Sternberger NH. Monoclonal antibodies distinguish phosphorylated and nonphosphorylated forms of neurofilaments in situ. Proc. Natl. Acad. Sci. USA. 1983;80:6126–6130. doi: 10.1073/pnas.80.19.6126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Robb L, Hilton DJ, Brook-Carter PT, Begley CG. Identification of a second murine interleukin-11 receptor alpha-chain gene (IL11Ra2) with a restricted pattern of expression. Genomics. 1997;40:387–394. doi: 10.1006/geno.1996.4579. [DOI] [PubMed] [Google Scholar]
- 26.Barres BA, Raff MC, Gaese F, Bartke I, Dechant G, Barde YA. A crucial role for neurotrophin-3 in oligodendrocyte development. Nature. 1994;367:371–375. doi: 10.1038/367371a0. [DOI] [PubMed] [Google Scholar]
- 27.Komiyama Y, Nakae S, Matsuki T, Nambu A, Ishigame H, Kakuta S, Sudo K, Iwakura Y. IL-17 plays an important role in the development of experimental autoimmune encephalomyelitis. J. Immunol. 2006;177:566–573. doi: 10.4049/jimmunol.177.1.566. [DOI] [PubMed] [Google Scholar]
- 28.Vaknin-Dembinsky A, Balashov K, Weiner HL. IL-23 is increased in dendritic cells in multiple sclerosis and down-regulation of IL-23 by antisense oligos increases dendritic cell IL-10 production. J. Immunol. 2006;176:7768–7774. doi: 10.4049/jimmunol.176.12.7768. [DOI] [PubMed] [Google Scholar]
- 29.Banchereau J, Fay J, Pascual V, Palucka AK. Dendritic cells: controllers of the immune system and a new promise for immunotherapy. Novartis Found. Symp. 2003;252:226–235. discussion 235–228, 257–267. [PubMed] [Google Scholar]
- 30.Mellman I, Steinman RM. Dendritic cells: specialized and regulated antigen processing machines. Cell. 2001;106:255–258. doi: 10.1016/s0092-8674(01)00449-4. [DOI] [PubMed] [Google Scholar]
- 31.Steinman RM, Kaplan G, Witmer MD, Cohn ZA. Identification of a novel cell type in peripheral lymphoid organs of mice. V. Purification of spleen dendritic cells, new surface markers, and maintenance in vitro. J. Exp. Med. 1979;149:1–16. doi: 10.1084/jem.149.1.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Heinrich PC, Behrmann I, Haan S, Hermanns HM, Muller-Newen G, Schaper F. Principles of interleukin (IL)-6-type cytokine signalling and its regulation. Biochem. J. 2003;374:1–20. doi: 10.1042/BJ20030407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Ernst M, Jenkins BJ. Acquiring signalling specificity from the cytokine receptor gp130. Trends. Genet. 2004;20:23–32. doi: 10.1016/j.tig.2003.11.003. [DOI] [PubMed] [Google Scholar]
- 34.Di Marco R, Khademi M, Wallstrom E, Iacobaeus E, Salvaggio A, Caracappa S, Papoian R, Nicoletti F, Olsson T. Curative effects of recombinant human Interleukin-6 in DA rats with protracted relapsing experimental allergic encephalomyelitis. J. Neuroimmunol. 2001;116:168–177. doi: 10.1016/s0165-5728(01)00301-0. [DOI] [PubMed] [Google Scholar]
- 35.Samoilova EB, Horton JL, Hilliard B, Liu TS, Chen Y. IL-6-deficient mice are resistant to experimental autoimmune encephalomyelitis: roles of IL-6 in the activation and differentiation of autoreactive T cells. J. Immunol. 1998;161:6480–6486. [PubMed] [Google Scholar]
- 36.Steinman L. Elaborate interactions between the immune and nervous systems. Nat. Immunol. 2004;5:575–581. doi: 10.1038/ni1078. [DOI] [PubMed] [Google Scholar]
- 37.Bettelli E, Carrier Y, Gao W, Korn T, Strom TB, Oukka M, Weiner HL, Kuchroo VK. Reciprocal developmental pathways for the generation of pathogenic effector TH17 and regulatory T cells. Nature. 2006;441:235–238. doi: 10.1038/nature04753. [DOI] [PubMed] [Google Scholar]
- 38.Veldhoen M, Hocking RJ, Atkins CJ, Locksley RM, Stockinger B. TGFbeta in the context of an inflammatory cytokine milieu supports de novo differentiation of IL-17-producing T cells. Immunity. 2006;24:179–189. doi: 10.1016/j.immuni.2006.01.001. [DOI] [PubMed] [Google Scholar]
- 39.Kuhlmann T, Remington L, Cognet I, Bourbonniere L, Zehntner S, Guilhot F, Herman A, Guay-Giroux A, Antel JP, Owens T, Gauchat JF. Continued administration of ciliary neurotrophic factor protects mice from inflammatory pathology in experimental autoimmune encephalomyelitis. Am. J. Pathol. 2006;169:584–598. doi: 10.2353/ajpath.2006.051086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Musashi M, Yang YC, Paul SR, Clark SC, Sudo T, Ogawa M. Direct and synergistic effects of interleukin 11 on murine hemopoiesis in culture. Proc. Natl. Acad. Sci. USA. 1991;88:765–769. doi: 10.1073/pnas.88.3.765. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Paul SR, Bennett F, Calvetti JA, Kelleher K, Wood CR, O'Hara RM, Jr., Leary AC, Sibley B, Clark SC, Williams DA, et al. Molecular cloning of a cDNA encoding interleukin 11, a stromal cell-derived lymphopoietic and hematopoietic cytokine. Proc. Natl. Acad. Sci. USA. 1990;87:7512–7516. doi: 10.1073/pnas.87.19.7512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Tepler I, Elias L, Smith JW, 2nd, Hussein M, Rosen G, Chang AY, Moore JO, Gordon MS, Kuca B, Beach KJ, Loewy JW, Garnick MB, Kaye JA. A randomized placebo-controlled trial of recombinant human interleukin-11 in cancer patients with severe thrombocytopenia due to chemotherapy. Blood. 1996;87:3607–3614. [PubMed] [Google Scholar]
- 43.Takeuchi Y, Watanabe S, Ishii G, Takeda S, Nakayama K, Fukumoto S, Kaneta Y, Inoue D, Matsumoto T, Harigaya K, Fujita T. Interleukin-11 as a stimulatory factor for bone formation prevents bone loss with advancing age in mice. J. Biol. Chem. 2002;277:49011–49018. doi: 10.1074/jbc.M207804200. [DOI] [PubMed] [Google Scholar]
- 44.Sonis ST, Van Vugt AG, McDonald J, Dotoli E, Schwertschlag U, Szklut P, Keith J. Mitigating effects of interleukin 11 on consecutive courses of 5-fluorouracil-induced ulcerative mucositis in hamsters. Cytokine. 1997;9:605–612. doi: 10.1006/cyto.1997.0208. [DOI] [PubMed] [Google Scholar]
- 45.Yucel OO, Berker E, Gariboglu S, Otlu H. Interleukin-11, interleukin-1beta, interleukin-12 and the pathogenesis of inflammatory periodontal diseases. J. Clin. Periodontol. 2008;35:365–370. doi: 10.1111/j.1600-051X.2008.01212.x. [DOI] [PubMed] [Google Scholar]
- 46.Hauser SL, Doolittle TH, Lincoln R, Brown RH, Dinarello CA. Cytokine accumulations in CSF of multiple sclerosis patients: frequent detection of interleukin-1 and tumor necrosis factor but not interleukin-6. Neurology. 1990;40:1735–1739. doi: 10.1212/wnl.40.11.1735. [DOI] [PubMed] [Google Scholar]
- 47.Steinman L. Nuanced roles of cytokines in three major human brain disorders. J. Clin. Invest. 2008;118:3557–3563. doi: 10.1172/JCI36532. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Linthicum DS, Munoz JJ, Blaskett A. Acute experimental autoimmune encephalomyelitis in mice. I. Adjuvant action of Bordetella pertussis is due to vasoactive amine sensitization and increased vascular permeability of the central nervous system. Cell Immunol. 1982;73:299–310. doi: 10.1016/0008-8749(82)90457-9. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Spleens were taken from unchallenged male 8wk IL-11Rα−/−, IL-11Rα+/− and IL-11Rα+/+ mice. CD11c+ APCs were isolated from splenocytes and immunostained for IL-11Rα, I-A, and DAPI (a–c). CD11c+ cells from wildtype animals displayed cell surface expression of both IL-11Rα and I-A (a). Cells from heterozygotes exhibited a lower level of IL-11Rα expression than wildtype mice (b). IL-11Rα was absent from the surface of CD11c+ cells from IL-11Rα−/− mice (c). Scalebars, 5µm.