Abstract
We report the case of a 58-year-old Caucasian woman with severe symptoms attributable to hypertrophic obstructive cardiomyopathy (HOCM). When supine there was no significant left ventricular outflow tract (LVOT) gradient on echocardiography or cardiac catheter measurements—despite provocation with supine leg exercise and right ventricular pacing. However, semi-supine bicycle exercise induced a marked increase in the LVOT gradient, which helped guide successful percutaneous alcohol septal ablation. This case report demonstrates the usefulness of bicycle exercise echocardiography in diagnosing HOCM with latent LVOT obstruction.
BACKGROUND
Hypertrophic cardiomyopathy (HCM) is a familial disease and symptomatic patients with obstructive disease may benefit from either cardiac surgery or septal ablation. There is, however, a group of patients who do not show obstruction at rest, which can be provoked by exercise, and who also benefit from intervention.
CASE PRESENTATION
A 58-year-old woman with HCM presented with presyncope and exertional dyspnoea (NYHA class II). She was treated with verapamil without any improvement and was subsequently referred for alcohol septal ablation. She also suffered from hypertension and arthritis, and had a strong family history of HCM with three of her six sisters having the disease.
Physical examination revealed a grade 3/6-ejection systolic murmur in the aortic region. A trans-thoracic echocardiogram showed an end-diastolic inter-ventricular septal thickness (IVS) of 2.2 cm, posterior wall thickness of 1.2 cm, systolic anterior motion of the anterior mitral valve leaflet, mild mitral regurgitation, and a peak instantaneous left ventricular outflow gradient (LVOTG) of 45 mmHg. This increased to 65 mmHg when a straight leg raises exercise was done. The left atrium was not dilated and left ventricular systolic function was good. A 24 h ambulatory ECG was normal and a Bruce protocol exercise test time was limited to only 2 min and 29 s as a result of dyspnoea.
She was referred for coronary angiography with a view to subsequent alcohol septal ablation. However, a repeat echocardiogram during the procedure showed a maximal LVOTG of only 30 mmHg. Right ventricular pacing did not induce any significant gradient change. Supine exercise only induced a gradient of 30 mmHg that fell to 10 mmHg with rest. For this reason septal ablation was not performed. A semi-supine bicycle stress echocardiogram was undertaken after a month. The LVOTG gradient increased to 88 mmHg from a baseline of 30 mmHg (figs 1 and 2), which was associated with severe breathlessness and dizziness.
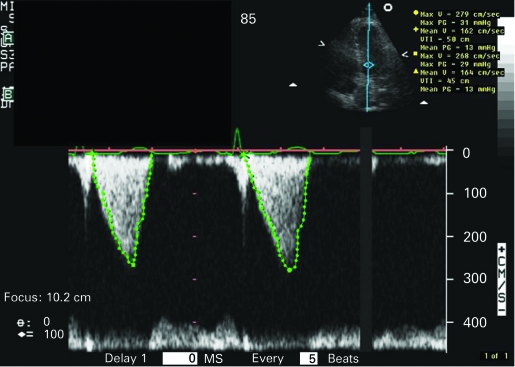
Figure 1.
Baseline left ventricular outflow gradient.
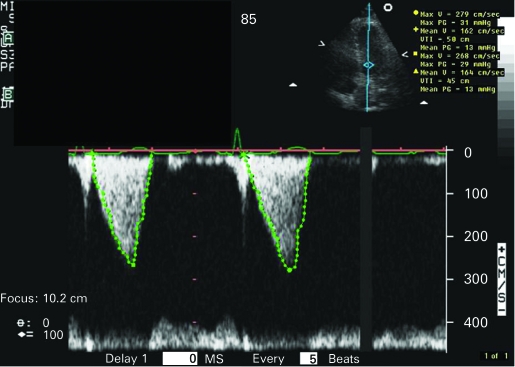
Figure 2.
Peak stress left ventricular outflow gradient.
TREATMENT
Alcohol septal ablation was subsequently performed as per the unit protocol. Postablation LVOTG decreased to 12 mmHg with reduction in septal thickness to 1.6 cm from 2.5 cm.
OUTCOME AND FOLLOW-UP
The mitral regurgitation became trivial, with akinesis of the mid-interventricular septal segment. On repeat stress echocardiogram 6 months postablation, the maximum LVOTG was 10 mmHg and the IVS thickness 1.6 cm. Septal akinesis was present, but the overall systolic function was good with no LV dilatation. Symptomatically, she improved remarkably and was in NYHA functional class I.
DISCUSSION
HCM is a familial cardiac disease affecting 1 in 500 of the population worldwide. It is characterised by a hypertrophied and non-dilated left ventricle, and is a common cause of sudden death particularly in young people. In a quarter of patients it may be associated with dynamic outflow obstruction. An LVOT gradient greater than 30 mmHg has pathophysiological and prognostic importance.1–3
Alcohol septal ablation is a percutaneous catheter-based interventional procedure for the treatment of symptomatic and medically unresponsive patients.4–6 It reduces the basal septal thickness, enlarges LVOT flow tract and reduces LVOTG. Patient selection for this procedure remains crucial. A gradient of more than 30–50 mmHg either at basal conditions or after provocation during exercise is an acceptable criterion in the presence of symptoms.1,7 Stress echocardiography has been used to provoke LVOT gradient. Semi-supine bicycle stress echocardiography is preferred over dobutamine as the latter has been shown to increase gradients even in normal hearts and in diseases other than HCM.8–12 It can also detect left ventricular dysfunction, and can be utilised to monitor the efficacy of treatment.13
In this patient, there was difficulty in eliciting an LVOT gradient despite right ventricular pacing and supine leg-raising exercise. Semi-supine stress echocardiography with bicycle ergometry was able to provoke the LVOT gradient, after which septal ablation was successfully undertaken. There was an instantaneous decrease in the LVOT gradient after ablation, with no provocable gradient 6 months post-ablation. This correlated with a decrease in symptoms similar to those reported by others.6,14,15
This case report re-emphasises the importance of semi-supine bicycle stress echocardiography in provoking a significant gradient in symptomatic patients with latent HCM, where other methods have failed.
LEARNING POINTS
The latent and variable nature of LVOT gradients can create management difficulties in HCM.
Identifying latent gradients by bicycle exercise echocardiography can help in decision making and should be strongly considered.
Footnotes
Competing interests: none.
Patient consent: Patient/guardian consent was obtained for publication.
REFERENCES
- 1.Maron BJ, McKenna WJ, Danielson GK, et al. ACC/ESC Clinical Expert Consensus Document on Hypertrophic Cardiomyopathy. J Am Coll Cardiol 2003; 42: 1–27 [DOI] [PubMed] [Google Scholar]
- 2.Maron MS, Olivotto I, Betocchi, et al. Effect of left ventricular outflow tract obstruction on clinical outcome in hypertrophic cardiomyopathy. N Engl J Med 2003; 348: 295–303 [DOI] [PubMed] [Google Scholar]
- 3.Gietzen FH, Leuner CJ, Obergassel L, et al. Role of trans-coronary septal ablation of septal hypertrophy in patients with hypertrophic cardiomyopathy, NYHA functional class III or IV and outflow obstruction under provocable conditions. Circulation 2002; 106: 454–9 [DOI] [PubMed] [Google Scholar]
- 4.Faber L, Meissener A, Ziemssen P, et al. Percutaneous trans-luminal septal myocardial ablation for hypertrophic obstructive cardiomyopathy: long term follow up of the first series of 25 patients. Heart 2000; 83: 326–31 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Gietzen FH, Leuner CJ, Raute-Kreinsen U, et al. Acute and long term results after trans-coronary ablation of septal hypertrophy (TASH). Catheter interventional treatment for hypertrophic obstructive cardiomyopathy. Eur Heart J 1999; 20: 1342–54 [DOI] [PubMed] [Google Scholar]
- 6.Nagueh SF, Lakkis NM, He ZX, et al. Role of myocardial contrast echocardiography during non-surgical septal reduction therapy for hypertrophic obstructive cardiomyopathy. J Am Coll Cardiol 1998; 32: 225–9 [DOI] [PubMed] [Google Scholar]
- 7.Maron BJ. Role of alcohol septal ablation in treatment of obstructive hypertrophic cardiomyopathy. Lancet 2000; 355: 425–6 [DOI] [PubMed] [Google Scholar]
- 8.Firoozi S, Elliott PM, Sharma S. Septal myotomy-myectomy and transcoronary septal septal ablation in hypertrophic cardiomyopathy. A comparison of clinical, haemodynamic and exercise outcomes. Eur Heart J 2002; 20: 1617–24 [DOI] [PubMed] [Google Scholar]
- 9.Bocketegers P, Steinbigler P, Molanar A, et al. Pressure-guided non-surgical reduction by septal infarctions in hypertrophic cardiomyopathy. J Am Coll Cardiol 2001; 38: 846–53 [DOI] [PubMed] [Google Scholar]
- 10.Okicic K, Shimuzu M, Yoshio H, et al. Left ventricular systolic dysfunction during exercise and dobutamine stress in patients with hypertrophic cardiomyopathy. J Am Coll Cardiol 2000; 36: 856–63 [DOI] [PubMed] [Google Scholar]
- 11.Luria D, Klustein MW, Rosenmann D, et al. Prevalence and significance of left ventricular outflow gradient during dobutamine echocardiography. Eur Heart J 1999; 20: 386–92 [DOI] [PubMed] [Google Scholar]
- 12.Pellikka PA, Oh JK, Bailey KR, et al. Dynamic intra-ventricular obstruction during dobutamine stress echocardiogram. A new observation. Circulation 1992; 82: 1429–32 [DOI] [PubMed] [Google Scholar]
- 13.Wu WC, Bhavsar JH, Aziz GF, et al. An overview of stress echocardiography in the study of patients with dilated or hypertrophic cardiomyopathy. Echocardiography 2004; 21: 467–75 [DOI] [PubMed] [Google Scholar]
- 14.Shamim W, Yousufuddin M, Wang D, et al. Non-surgical reduction of the inter-ventricular septum in patients with hypertrophic cardiomyopathy. N Engl J Med 2000; 347: 1326–8 [DOI] [PubMed] [Google Scholar]
- 15.Lakkis NM, Nagueh SF, Dunn JK, Killip D, Spencer WH., 3rd Nonsurgical septal reduction therapy for hypertrophic obstructive cardiomyopathy: one-year follow-up. J Am Coll Cardiol 2000; 36: 852–5 [DOI] [PubMed] [Google Scholar]