Abstract
Proton pump inhibitors (PPIs) are the gold standard treatment for gastroesophageal reflux disease. In clinical practice, failure of PPIs occurs frequently, and may affect up to 30% of patients in a typical gastroenterology practice. Multichannel impedance monitoring combined with pH monitoring helps to detect nonacid reflux, and if symptoms correlate with these nonacid reflux episodes, nonacid reflux disease can be diagnosed. In contrast to PPIs, reflux inhibitors target transient lower esophageal sphincter relaxations, which are involved in the pathophysiology of reflux disease and may be the appropriate future treatment for nonacid reflux disease. The present article discusses the current understanding of nonacid reflux disease, its diagnosis and treatment.
Keywords: Arbaclofen ADX 10059, GERD, Lesogaberan, Proton pump inhibitor, Reflux
Abstract
Les inhibiteurs de la pompe à protons (IPP) constituent le traitement de référence du reflux gastro-œsophagien pathologique. En milieu clinique, il est fréquent que les IPP ne fonctionnent pas, puisque jusqu’à 30 % des patients d’un cabinet de gastroentérologie classique peuvent être touchés. La surveillance d’impédance multivoie associée à la surveillance du pH contribue à déceler le reflux non acide, et si les symptômes sont liés à ces épisodes de reflux non acide, on peut diagnostiquer un reflux non acide pathologique. Contrairement aux IPP, les inhibiteurs du reflux ciblent les relâchements du sphincter inférieur de l’œsophage, qui participent à la physiopathologie du reflux pathologique et pourraient constituer le futur traitement du reflux non acide pathologique. Le présent article présente les connaissances actuelles du reflux non acide pathologique, de son diagnostic et de son traitement.
Gastroesophageal reflux (GER) is the term used to describe retrograde movement of gastric contents into the esophagus. Within certain limits, this is considered to be physiological, although a physiological relevance has yet to be established. The condition is named GER disease (GERD) when patients experience symptoms or when reflux results in esophageal damage (eg, esophagitis). There is no doubt that acid is the major aggressive component of the refluxate. GERD is a major burden to western societies and it was a major breakthrough when omeprazole – the first proton pump inhibitor (PPI) – was marketed in 1989. Since then, the acid component of GERD can be sufficiently treated; PPIs are the gold standard treatment for patients with GERD (1).
However, during the past two centuries, we learned that there is a subgroup of patients with typical reflux-indicating symptoms who respond insufficiently or not at all to PPI treatment, and in whom acid reflux does not seem to be the underlying disease. Present studies (2,3) estimate that this subgroup of PPI nonresponders may be as large as 20% to 30%. Due to a lack of diagnostic tools, it was not clear until recently to what extent weakly acidic reflux (pH 4 to 7), nonacidic reflux (pH greater than 4) or reasons not related to reflux contribute to the symptoms in these patients. Recent advances in technology now enable the detection of weakly acidic and nonacid reflux, as well as transient lower esophageal sphincter relaxations (TLESRs). Furthermore, we now know that nonacid reflux can cause symptoms, and that an increased number of TLESRs is the predominant pathophysiological mechanism that causes gastroesophageal junction incompetence and, consequently, GERD.
NONACID REFLUX DISEASE
GERD is diagnosed clinically according to the typical symptoms that respond to treatment with a PPI or by 24 h esophageal pH monitoring, in which a pH below 4.0 is regarded to indicate acid reflux, and the length of time in which esophageal mucosa is in contact with acid is used to diagnose GERD. On the other hand, pH monitoring is not helpful in diagnosing nonacid reflux because it monitors acidity as an indirect marker of reflux but not the actual reflux. Therefore, in a patient not responding to PPI treatment, pH monitoring is helpful in identifying individuals who still produce acid while being on a standard or double dose of a PPI, but in whom pH monitoring is not helpful to measure nonacid reflux episodes.
The recently introduced technique of multichannel intraluminal impedance monitoring combined with pH monitoring changed our understanding of GERD. From impedance monitoring we learned that nonacid reflux causes symptoms that may be indistinguishable from the symptoms of acid reflux disease and, furthermore, that, as in acid reflux disease, non-acid reflux may cause esophageal and extraesophageal symptoms. This applies to classical esophageal reflux symptoms and nonesophageal symptoms such as coughing (4–6). Whether the volume of the refluxate, esophageal sensitivity or other factors contribute to these symptoms is not clear and is the subject of ongoing investigation.
In contrast to pH monitoring, the multichannel impedance technique detects changes in resistance to electrical currents indicating the presence of intraluminal liquid (7). The multichannel capability of the recording catheter enables capturing the direction of this esophageal liquid, and enables us to clearly define antegrade bolus transit (food transport) and retrograde bolus transit as a marker of reflux. Because pH is monitored simultaneously, the information obtained enables the differentiation of acid reflux from nonacid reflux using a pH cut-off of 4.0 (Figure 1). Interestingly, one of the first things that was learned using this technique is that a PPI reduces the number of acid reflux episodes; however, the absolute number of reflux episodes remains unchanged – the reflux episodes in patients taking a PPI are simply turned into nonacidic episodes (8). Multichannel impedance monitoring enables the quantification of acid and nonacid reflux episodes, and contact time and, additionally, allows us to to distinguish liquid, gaseous and mixed reflux. Presently, different classifications are used. Whereas all of these classify acid reflux as episodes in which pH drops below 4.0, some of them use nonacid reflux for all other reflux episodes, and some classifications further distinguish weakly acidic reflux (pH 4 to 7) from weakly alkaline reflux (pH above 7) (9,10). The physiological significance of the classification of nonacid reflux into weakly acidic and weakly alkaline is unclear.
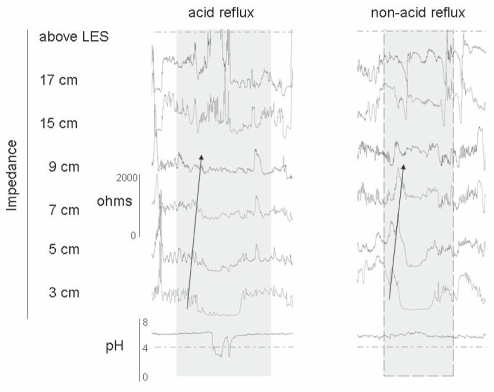
Figure 1.
Original recordings from a combined multichannel intraluminal impedance and pH (MII-pH) study. The impedance recording channels are located 3 cm, 5 cm, 7 cm, 9 cm, 15 cm and 17 cm above the lower esophageal sphincter (LES) and the pH recording sensor is located at 5 cm above the LES. In this image, impedance-pH monitoring identifies reflux episodes as declines in intraluminal impedance progressing from distal to proximal (arrow). The pH channel identifies acid (pH less than 4) and nonacid (pH greater than 4) reflux
Because our perception of nonacid reflux disease largely relies on studies performed during the preimpedance era, our current understanding is limited, especially because of the lack of epidemiological data and the undetermined impact of non-acid reflux disease. A recent multicentre trial (4) that used multichannel impedance combined with pH monitoring in patients with reflux-indicating symptoms despite being on a PPI twice daily, identified nonacid reflux in 37% and acidic reflux in 11%. Whereas the clinical approach to patients with persistent acid reflux seems evident, the approach to patients with nonacid reflux is less evolved.
DIAGNOSIS
In addition to patients not responding to PPI treatment being a significant problem, establishing the diagnosis is poorly developed and the tools needed to make this diagnosis are only available at tertiary referral centres. With new therapies on the horizon, this may change and require that nonacid reflux is confirmed before specific treatment is initiated. The clinical significance of multichannel impedance measurement combined with pH monitoring in patients who fail or insufficiently respond to PPI treatment is undoubted because it is currently the only technique that can reliably quantify nonacid reflux into the esophagus. Manometry, pH monitoring and radiological techniques cannot diagnose disease or quantify nonacid reflux and, thus, are used for other indications. pH monitoring is helpful in diagnosing acid reflux when the study is performed while the patient is off antacid medication, or in diagnosing ongoing acid reflux in patients who are on an antacid medication. The impedance technique is particularly useful in patients presenting with reflux symptoms while being on a PPI and, therefore, the studies are ideally performed with the patient being on a standard dose of twice daily PPI. The impedance results then report whether reflux is still the underlying cause of the symptoms and whether it is acidic or nonacidic. Additional information obtained during impedance monitoring, such as symptom reflux correlation, is considered to be an essential tool for interpreting the findings in the context of the patient’s symptoms and to direct treatment decisions. Presently, a symptom association probability of 50 or greater – indicating that 50% or more of symptoms are associated with reflux – is considered to be diagnostic for a positive study and acid reflux disease. Acid and nonacid reflux disease, or both, can be diagnosed based on a symptom association probability and the number of reflux episodes. Patients with reflux-indicating symptoms but a negative impedance study while on a twice daily PPI do not have significant acid or nonacid reflux disease and other causes should be considered.
TREATMENT
Currently, GERD is best treated with a PPI and provides adequate symptom relief for the majority of patients. However, targeting acid reflux does not target the cardinal mechanism underlying GER. Our current understanding is that an increased number of TLESRs is the main pathophysiological mechanism underlying GERD. A new group of drugs, known as reflux inhibitors, is emerging that targets TLESRs and, thus, the main mechanism of GER. Gamma aminobutyric acid receptor (GABAB) agonists and metabotropic glutamate receptor 5 (MGLUR5) antagonists are such reflux inhibitors and are currently being tested in clinical trials. They may not have the potential to replace PPIs, but may be future treatment options in patients in whom PPIs provide incomplete or no symptomatic benefit. The number of such PPI nonresponders should not be underestimated. Presently, there is no formal, established treatment for nonacid reflux. Intensifying lifestyle changes including weight loss, small meals, avoiding nicotine and alcohol, eliminating late meals and sleeping with the head of the bed elevated are frequently recommended. This is entirely based on our knowledge of acid reflux disease in which, aside from losing weight and poor elevation of the head of the bed evidence, efficacy of these measures in nonacid reflux disease is assumed but has yet to be confirmed.
Medical treatment specifically tested in nonacid reflux is not yet available, but some approaches are established. The GABAB agonist baclofen is known to decrease the number of TLESRs and was studied in a significant number of clinical trials in volunteers and patients with GER (11). In these trials, baclofen reduced reflux, especially postprandial reflux of acidic and nonacidic composition. In one placebo-controlled trial (12) in which baclofen (10 mg four times per day) or placebo were given over four weeks, baclofen reduced GER, which led to a significant improvement of symptoms. This was confirmed in a previous study of acute GER (13), in which a single dose of baclofen (40 mg) or placebo was given before a refluxogenic meal. In this study, baclofen significantly reduced both acid and nonacid reflux, as well as associated symptoms. Because this approach was tested on a small number of patients, further data from larger trials are needed before recommending baclofen for routine clinical use in the treatment of nonacid reflux disease; however, a trial of baclofen (10 mg four times per day) in selected patients may be considered. Due to the side effects associated with baclofen, its overall usefulness is somewhat limited. Its use is likely to diminish with the introduction of alternative options.
One alternative in clinical development is lesogaberan, a GABAB receptor agonist developed by AstraZeneca (Sweden). In a recent placebo-controlled clinical trial (14), lesogaberan reduced the number of TLESRs due to underlying GER, increased lower esophageal sphincter pressure and reduced the number of GER episodes in healthy volunteers. Lesogaberan has a more favourable side effect profile than baclofen and is presently being assessed in many clinical trials focusing on manometry and impedance changes in patients with GERD (NCT00743444), on acid and nonacid reflux episodes in patients with GERD (NCT01043185), and on symptomatic improvement in patients with GERD with lesogaberan as an add-on therapy to PPI in GERD patients with partial response to PPI (NCT00394472 and NCT01005251). Another GABAB agonist developed by AstraZeneca, AZD9343, reduced TLESRs and the number of acid reflux episodes in healthy volunteers; however, the reported side effect profile makes further development unlikely (15). Arbaclofen-placarbil, the R-isomer of baclofen, is under investigation by XenoPort Pharma (USA). In a multicentre, randomized, double-blind crossover study of patients with GERD (16), it was well tolerated and reduced the number of GER episodes and heartburn. Arbaclofen-placarbil is currently being tested in a multicentre clinical trial (NCT00978016) as adjunctive therapy in subjects with GERD who are incomplete responders to a PPI. The MGLUR5 antagonist ADX10059 (Addex Pharma, Switzerland) was investigated in a randomized, double-blind, placebo-controlled study on healthy volunteers in whom it significantly reduced esopha-geal acid exposure and weakly acidic reflux. The efficacy of ADX10059 is presently being studied in a multicentre trial (NCT00810485) as an add-on therapy to PPI in patients with GERD.
In addition to medical treatment, interventional and surgical treatments may be options for patients with nonacid reflux disease. Antireflux surgery was previously shown to be a treatment for GERD patients who respond well to PPI treatment. It was reported that patients who do not respond to PPI will have a poor response to antireflux surgery and should, therefore, not be offered this option. In the impedance era, this notion needs to be revised because a recent study (17) clearly showed that patients with nonacid reflux and a positive symptom index in a preoperative impedance-pH study while being on PPI had a 94% chance of achieving a good symptomatic response or to be asymptomatic with a Nissen fundoplication. Although larger, ideally multicentre, trials still need to confirm this observation, this extends our current knowledge and may direct the treatment of patients with nonacid reflux disease.
Although there are no data available to support the notion that endoscopic antireflux procedures are helpful for the treatment of nonacid reflux, these procedures may experience a revival in nonacid reflux disease because voluminous reflux may be a better target than acid reflux in patients in whom these endoscopic procedures previously failed. Combined impedance-pH monitoring may be helpful in facilitating ideal patient selection for future clinical trials. Furthermore, it is not established whether prokinetics, such as metoclopramide and domperidone, or mucoprotective agents are helpful in patients with nonacid reflux disease. For acid reflux disease and functional gastrointestinal diseases, these compounds provide symptomatic benefit and, to some extent, heal esophagitis, but they are inferior to the gold standard PPI treatment. These drugs were not tested for the treatment of nonacid reflux disease, but studies in reflux patients who failed standard PPI therapy are underway (NCT00777439, NCT00761254).
SUMMARY AND OUTLOOK
A significant number of patients with typical reflux-indicating symptoms do not respond to PPI treatment; nonacid reflux disease may be underlying in these patients. Nonacid reflux is common and causes symptoms very similar to the classical symptoms of GERD. Combined impedance-pH monitoring helps us to diagnose nonacid reflux disease, and patients with insufficient response to high-dose PPI should undergo impedance-pH monitoring where available. In contrast to pH monitoring alone, the combination of pH monitoring with multichannel impedance testing is a powerful tool to detect acid and nonacid reflux when performed while the patient continues to take a PPI twice daily.
Current treatment approaches are limited; however, promising clinical trials are underway. The contemporary approach includes intensifying the same lifestyle modifications recommended for GERD. Baclofen (10 mg four times per day) before meals may be tried as suggested by small clinical trials. If both approaches fail and the patient requires a more definite therapy, a surgical approach may be considered. A requirement for surgery is that nonacid reflux be diagnosed with an impedance study because, until previously, failure of PPI treatment was considered to be a negative predictor of symptom improvement following antireflux surgery. It is presently unclear to what extent drug development will add further options in the near future – the clinical trial activity, however, appears promising.
References
- 1.Storr M, Meining A, Allescher HD. Pharmacoeconomic issues of the therapy of gastroesophageal reflux disease. Exp Opin Pharmacother. 2001;2:1099–108. doi: 10.1517/14656566.2.7.1099. [DOI] [PubMed] [Google Scholar]
- 2.Armstrong D, Pare P, Pericak D, Pyzyk M. Symptom relief in gastroesophageal reflux disease: A randomized, controlled comparison of pantoprazole and nizatidine in a mixed patient population with erosive esophagitis or endoscopy-negative reflux disease. Am J Gastroenterol. 2001;96:2849–57. doi: 10.1111/j.1572-0241.2001.4237_a.x. [DOI] [PubMed] [Google Scholar]
- 3.Meineche-Schmidt V, Juhl HH, Ostergaard JE, Luckow A, Hvenegaard A. Costs and efficacy of three different esomeprazole treatment strategies for long-term management of gastro-oesophageal reflux symptoms in primary care. Aliment Pharmacol Ther. 2004;19:907–15. doi: 10.1111/j.1365-2036.2004.01916.x. [DOI] [PubMed] [Google Scholar]
- 4.Mainie I, Tutuian R, Shay S, et al. Acid and non-acid reflux in patients with persistent symptoms despite acid suppressive therapy: A multicentre study using combined ambulatory impedance-pH monitoring. Gut. 2006;55:1398–402. doi: 10.1136/gut.2005.087668. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Sifrim D, Dupont L, Blondeau K, Zhang X, Tack J, Janssens J. Weakly acidic reflux in patients with chronic unexplained cough during 24 hour pressure, pH, and impedance monitoring. Gut. 2005;54:449–54. doi: 10.1136/gut.2004.055418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Tutuian R, Mainie I, Agrawal A, Adams D, Castell DO. Nonacid reflux in patients with chronic cough on acid-suppressive therapy. Chest. 2006;130:386–91. doi: 10.1378/chest.130.2.386. [DOI] [PubMed] [Google Scholar]
- 7.Nguyen HN, Silny J, Matern S. Multiple intraluminal electrical impedancometry for recording of upper gastrointestinal motility: Current results and further implications. Am J Gastroenterol. 1999;94:306–17. doi: 10.1111/j.1572-0241.1999.00847.x. [DOI] [PubMed] [Google Scholar]
- 8.Vela MF, Camacho-Lobato L, Srinivasan R, Tutuian R, Katz PO, Castell DO. Simultaneous intraesophageal impedance and pH measurement of acid and nonacid gastroesophageal reflux: Effect of omeprazole. Gastroenterology. 2001;120:1599–606. doi: 10.1053/gast.2001.24840. [DOI] [PubMed] [Google Scholar]
- 9.Smout AJ. The measurement of non-acid gastro-oesophageal reflux. Aliment Pharmacol Ther. 2007;26(Suppl 2):7–12. doi: 10.1111/j.1365-2036.2007.03527.x. [DOI] [PubMed] [Google Scholar]
- 10.Sifrim D, Castell D, Dent J, Kahrilas PJ. Gastro-oesophageal reflux monitoring: Review and consensus report on detection and definitions of acid, non-acid, and gas reflux. Gut. 2004;53:1024–31. doi: 10.1136/gut.2003.033290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lidums I, Lehmann A, Checklin H, Dent J, Holloway RH. Control of transient lower esophageal sphincter relaxations and reflux by the GABA(B) agonist baclofen in normal subjects. Gastroenterology. 2000;118:7–13. doi: 10.1016/s0016-5085(00)70408-2. [DOI] [PubMed] [Google Scholar]
- 12.Ciccaglione AF, Marzio L. Effect of acute and chronic administration of the GABA B agonist baclofen on 24 hour pH metry and symptoms in control subjects and in patients with gastro-oesophageal reflux disease. Gut. 2003;52:464–70. doi: 10.1136/gut.52.4.464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Vela MF, Tutuian R, Katz PO, Castell DO. Baclofen decreases acid and non-acid post-prandial gastro-oesophageal reflux measured by combined multichannel intraluminal impedance and pH. Aliment Pharmacol Ther. 2003;17:243–51. doi: 10.1046/j.1365-2036.2003.01394.x. [DOI] [PubMed] [Google Scholar]
- 14.Boeckxstaens GE, Rydholm H, Lei A, Adler J, Ruth M. Effect of lesogaberan, a novel GABA-receptor agonist, on transient lower esophageal sphincter relaxations in male subjects. Aliment Pharmacol Ther. 2010;11:1208–17. doi: 10.1111/j.1365-2036.2010.04283.x. [DOI] [PubMed] [Google Scholar]
- 15.Beaumont H, Smout A, Aanen M, et al. The GABA(B) receptor agonist AZD9343 inhibits transient lower oesophageal sphincter relaxations and acid reflux in healthy volunteers: A phase I study. Aliment Pharmacol Ther. 2009;30:937–46. doi: 10.1111/j.1365-2036.2009.04107.x. [DOI] [PubMed] [Google Scholar]
- 16.Gerson LB, Huff FJ, Hila A, et al. Arbaclofen Placarbil decreases postprandial reflux in patients with gastroesophageal reflux disease. Am J Gastroenterol. 2010;105:1266–75. doi: 10.1038/ajg.2009.718. [DOI] [PubMed] [Google Scholar]
- 17.Mainie I, Tutuian R, Agrawal A, Adams D, Castell DO. Combined multichannel intraluminal impedance-pH monitoring to select patients with persistent gastro-oesophageal reflux for laparoscopic Nissen fundoplication. Br J Surg. 2006;93:1483–7. doi: 10.1002/bjs.5493. [DOI] [PubMed] [Google Scholar]