Abstract
Objective
To describe the characteristics of wrestling injuries occurring in male athletes aged 7–17 treated in United States (U.S.) emergency departments (ED) from 2000–2006, and to compare injury patterns between younger & older youth wrestlers.
Methods
A stratified probability sample of U.S. hospitals providing emergency services in the National Electronic Injury Surveillance System was used for 2000–2006. ED visits for injuries sustained in organized wrestling were analyzed for male patients ages 7–17 years old (subdivided into 7–11 years old [youth group] and 12–17 years old [scholastic group]).
Results
During the study period, there were an estimated 167,606 ED visits for wrestling injuries in 7–17 years old U.S. males, with 152,710 (91.1%) occurring in the older (12–17 years old) group. The annual injury incidence was 6.49 injuries/1,000 wrestlers in the youth group and 29.57 injuries/1,000 wrestlers in the scholastic group. The distribution of diagnoses was similar in both age groups, with sprain/strain as the most common diagnosis, followed by fracture and contusion/abrasion. Distributions of injury by location were significantly different between groups (p=0.02), although both groups exhibited approximately 75% of all injuries from the waist up. Overexertion and struck by/against were the most common precipitating and direct mechanisms in both groups, respectively. Over 97% of all injured wrestlers were treated and released.
Conclusion
The types of injury in youth (7–11 years old) wrestlers are similar to those of scholastic (12–17 years old) wrestlers, although the distribution of body parts injured differs between the age groups. The majority of injuries occurs above the waist and may be a target for prevention strategies.
INTRODUCTION
Background
The origins of wrestling can be traced back to the Sumerians as early as 5000 B.C., and records of ancient Olympic wrestling date back to the Greeks in 708 B.C.1 Since those early days, wrestling has evolved into many different forms practiced all over the world with the major styles including freestyle, Greco-Roman and folkstyle. In the United States (U.S.), folkstyle is the style in which most athletes participate and involves younger athletes in youth programs as well as interscholastic wrestling teams at the middle school and high school levels. While overall participation has varied in recent years, U.S. wrestling participation has averaged 2.5 million participants per year over 2000–2006, with an average of 1.1 million participants wrestling greater than 50 days per year.2 Despite having only the sixth highest average annual participation of boys in high school sports, wrestling is second only to tackle football for frequency of injury in high school athletes.3–4
The risk of serious injury is significant in young athletes and includes permanent debilitation from fracture, traumatic brain injury and rarely, death.5–10 A number of these wrestling injuries can be categorized as major or catastrophic ensuring that wrestlers will frequently require emergency treatment while some injuries will require inpatient care or even surgery depending upon the diagnosis.5–6,9,11–13 Furthermore, the unique physical requirements and limb positions in wrestling also leads to rare but noteworthy injuries that have been reported in the medical literature.14–20
Because of its violent nature, wrestling has been a target of injury prevention efforts. These efforts have included regulations that cap excessive and rapid weight loss, mat and equipment engineering interventions, and revision of weight classes among others with effectiveness noted especially in the weight management interventions at the high school and collegiate levels.7,8,21–25
Importance
Our current knowledge of the distribution and nature of wrestling injuries is incomplete. While organizers, coaches and officials have made many efforts to ensure the safety of participants, injuries still occur, and the patterns of injury remain uncertain in the youngest athletes. Furthermore, the extent to which injuries at the youth level differ from those at the high school level is unknown. Overall, researchers have found that young athletes are more likely to suffer from physical injuries and avulsion fractures rather than ligament and tendon injuries like their older counterparts.26 Additionally, the larger body surface area to mass ratio and developing motor skills of younger athletes have been shown to result in more serious injuries in some sports.27
Goals of this Investigation
Existing data reflect patterns of wrestling injuries only on a local or regional level. To our knowledge, a national assessment of youth wrestling injuries has not been undertaken. Given the lack of knowledge concerning wrestling injuries in school-aged athletes, we set out to 1) describe injuries in competitive wrestlers at the youth, and the middle school/high school levels from a national perspective and 2) compare the patterns of injury between these age groups.
METHODS
Study Design
This was a retrospective study using data from the National Electronic Injury Surveillance System (NEISS) for patients treated from January 1, 2000, through December 31, 2006. Our institution’s Committee on the Protection of Human Subjects exempted the study protocol from institutional review board review.
Study Setting and Population
We obtained data from NEISS, which is a national probability sample of hospitals conducted by the U.S. Consumer Product Safety Commission. Data on injury-related visits are obtained from a national sample of 96 - 100 NEISS hospitals that was selected as a stratified probability sample of hospitals in the U.S. and its territories with a minimum of six beds and a 24-hour emergency department (ED). NEISS collects data on visits for consumer product-related injuries treated in U.S. EDs and provides data on approximately 350,000 injury-related ED visits annually. It is intended to provide national incidence estimates of consumer-product related nonfatal injuries and poisonings treated in U.S. hospital EDs. For purposes of the present study, all ED visits resulting from wrestling-associated injury were included. NEISS codes wrestling injuries as those resulting from wrestling activities, apparel or equipment. We reviewed the narrative portion of each record and included in our analysis only those ED visits for injuries resulting from organized wrestling activities. In addition, visits derived from wrestling activities other than Folkstyle/Scholastic, Freestyle or Greco-Roman wrestling were excluded (e.g., sumo wrestling, mud wrestling, etc.). Finally, because the injury numbers in female participants were very low and the NEISS estimates were therefore unstable, we restricted our analysis to male participants only.
Measurements
NEISS collects information on the date of treatment, patient age, diagnosis, body part injured, patient disposition, locale in which the injury occurred, the type of product associated with the injury and a brief narrative describing the circumstances of the injury event. Incident locale is coded by NEISS as: home, farm/ranch, street or highway, other public property (includes store, office building, restaurant, church, hotel, motel, hospital or other medical facility, nightclub, theater or other public property), mobile home, industrial place, school, place of recreation or sports, or not recorded. For the present study, only injuries that occurred at school or at a place of recreation or sports were included. Since deaths are not fully captured by NEISS, patients who were dead on arrival or died in the ED are excluded. Similarly, patient outcome subsequent to leaving the ED is not included in the NEISS data. Two age groupings were used for analysis: 7–11 years and 12–17 years. These were intended to approximate elementary school age and middle/high-school age. NEISS diagnosis was recoded as: contusion/abrasion, strain/sprain, fracture, dislocation, laceration, traumatic brain injury (TBI), and other. The diagnosis category TBI included NEISS diagnosis codes for concussion, for internal injury in which “head” was the body part affected, as well as NEISS diagnosis code for fracture in which “head” was the body part affected.28 NEISS body part categories were recoded in combination as: wrist/hand/finger, head/neck, shoulder, ankle/foot/toe, trunk/pubic region, arm (upper or lower), elbow, knee, and leg (upper or lower). Information in the narrative was used to code precipitating and direct mechanisms of injury as: fall/takedown, struck by/against, overexertion, other, or unknown/unspecified. Two researchers coded these variables independently, based upon the standard guidelines of the NEISS All Injury Program, defining the precipitating mechanism as the initiating mechanism that started the chain of events leading to the injury, and the direct mechanism as the most immediate mechanism that caused the actual injury.29 In accord with that program, overexertion was defined as “overexertion of one’s body or a body part, causing damage to muscle, tendon, ligament, cartilage, joint, or peripheral nerve (e.g., common cause of strains, sprains, and twisted ankles); overexertion from lifting, pushing, or pulling; damage to body parts of a person caused by exertion from excessive force such as pulling of a person’s arm, leg, or other body part by another person or an inanimate object, equipment or structure.” Differences in coding were initially resolved through discussion between the two reviewers. When differences could not be resolved in that manner, a third independent researcher helped to resolve the discrepancy.
Participation data were available through the Sports Business Research Network2 and are derived from annual reports provided by the National Sporting Goods Association (NSGA). The NSGA conducts annual mail based surveys of 30,000 pre-selected U.S. households, collecting self-reported sports participation data for U.S. residents. Eligible participants include household members ≥ 7 years of age who report participation in wrestling at least once during the 12-month period. Information collected includes age, sports participated in, and number of days participated during the previous twelve months. Participation numbers are grouped into age ranges and include the same age groups: 7–11 and 12–17 years. These data were available for the years 2001, 2003, 2004, and 2006.
Data Analysis
ED visits resulting from injuries involving organized wrestling were analyzed for patients 7 through 17 years of age. Data were analyzed with SAS (version 9.1.3; SAS Institute, Inc, Cary, NC) using the Survey Procedures (PROC SURVEYFREQ) to account for the complex sampling design and the weighting structure utilized by NEISS. Each case was assigned a sample weight by NEISS based on the inverse probability of selection. These weights were used to calculate national estimates of nonfatal injuries. Confidence intervals and coefficients of variation were calculated by using a direct variance estimation procedure that accounted for the sample weights. Consistent with the NEISS recommendations, we designated estimates as unstable when: computations were based on fewer than 20 NEISS cases (based on unweighted data), individual national estimates were less than 1,200 (based on weighted data), or the coefficient of variation (CV) of the estimate was greater than 30%. Univariate differences between the two age groups were examined using weighted chi-square testing for categorical variables. Annual injury incidence was calculated per 1,000 wrestlers based on NEISS estimates and average annual participation numbers for the study years using 2001, 2003, 2004, and 2006 participation data from the Sports Business Research Network.
RESULTS
Characteristics of Study Subjects
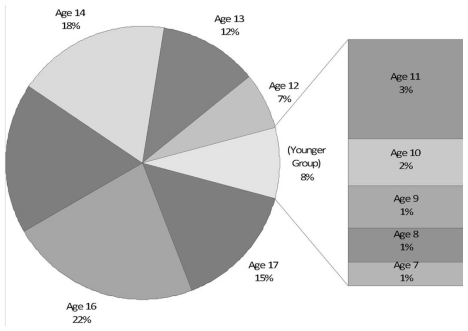
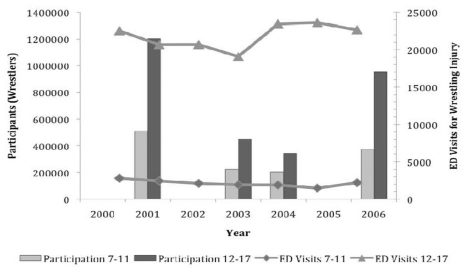
There were an estimated 173,604 ED visits for wrestling-related injuries in 7–17 year olds from 2000 through 2006. Of these 96.6% of the visits were by male patients, comprising an estimated 167,606 visits. Among male participants, 91.1% of all visits occurred in the 12–17 year age group. The gender and age distributions of these visits are depicted in Table 1 and Figure 1. Participation statistics were available for years 2001, 2003, 2004, and 2006 and are compared to annual ED visits for wrestling injuries in Figure 2.
Table 1.
Wrestling-related injuries in athletes presenting to emergency departments by age, United States, 2000–2006
| Characteristic | National Estimate* | % |
|---|---|---|
| Total | 173,604 | --- |
| Male | 167,606 | 96.5% |
| Female | 5,998 | 3.5% |
| 7–11 years | ||
| Male | 14,896 | 91.4% |
| Female | 1,409 | 8.6% |
| Total 7–11 | 16,305 | 100.00% |
| 12–17 years | ||
| Male | 152,710 | 97.1% |
| Female | 4,589 | 2.9% |
| Total 12–17 | 157,289 | 100.00% |
Based on NEISS-AIP weights
Figure 1.
Age distribution of male emergency department visits for wrestling-related injuries, 2000–2006 (n=167,606).
Figure 2.
Wrestling participation and United States emergency department visits for wrestling injuries, by age group, 2000–2006.
Main Results
The characteristics of U.S. ED visits for wrestling-related injuries are illustrated in Table 2. There were approximately 10 times more injuries in the scholastic (12–17 years) age group than in the youth (7–11 years) group over the seven-year study period. In contrast, the number of wrestling participants over the study period for the scholastic group was only slightly more than twice that of the youth group, with an average of approximately 330,000 participants/year in the youth group and 740,000 participants/year in the scholastic group. The annual injury incidence for our study period was nearly 5 times higher in the scholastic group, equaling 29.57 injuries/1,000 wrestlers/year (95% CI 26.74–32.40) versus 6.49 injuries/1,000 wrestlers/year in the youth group (95% CI 4.97–8.03).
Table 2.
Wrestling-related injury characteristics of male athletes presenting to emergency departments by age group, United States, 2000–2006
| Males | |||||
|---|---|---|---|---|---|
| Age 7–11 | Age 12–17 | ||||
| Characteristic | n* | % (95% CL) | n* | % (95% CL) | p |
| Total Injuries | 14896 | -- | 152710 | -- | -- |
| Injuries by Diagnosis | 0.28 | ||||
| Sprain/Strain | 5757 | 38.7 (32.4–44.9) | 55910 | 36.6 (34.7–38.5) | |
| Fracture | 3858 | 25.9 (20.3–31.5) | 33764 | 22.1 (20.5–23.7) | |
| Contusion/Abrasion | 2422 | 16.3 (11.5–21.1) | 22843 | 15.0 (13.6–16.4) | |
| Other/Not Stated | 1088† | 7.3 (4.1–10.5) | 13103 | 8.6 (7.5–9.7) | |
| Traumatic Brain Injury | 676† | 4.5 (1.9–7.2) | 9437 | 6.2 (5.3–7.1) | |
| Laceration | 424† | 2.9 (0.8–4.9) | 9063 | 5.9 (5.0–6.9) | |
| Dislocation | 671† | 4.5 (1.8–7.2) | 8590 | 5.6 (4.7–6.5) | |
| Injuries by Location§ | 0.02 | ||||
| Wrist/Hand/Finger | 2772 | 18.6 (13.6–23.6) | 28193 | 18.5 (16.9–20.0) | |
| Head/Neck | 2352 | 15.8 (11.2–20.4) | 22169 | 14.5 (13.2–15.9) | |
| Shoulder | 1776 | 11.9 (7.7–16.1) | 22839 | 15.0 (13.6–16.4) | |
| Ankle/Foot/Toe | 1661 | 11.2 (7.1–15.3) | 14350 | 9.4 (8.3–10.5) | |
| Trunk/Pubic Region | 1625 | 10.9 (6.9–14.9) | 15480 | 10.1 (9.0–11.3) | |
| Arm, Upper or Lower | 1581 | 10.6 (6.6–14.7) | 8087 | 5.3 (4.4–6.2) | |
| Elbow | 1148† | 7.7 (4.5–10.9) | 9476 | 6.2 (5.3–7.2) | |
| Knee | 994† | 6.7 (3.5–9.9) | 12876 | 8.4 (7.4–9.5) | |
| Face/Ear/Eye/Mouth | 669† | 4.5 (1.9–7.1) | 15073 | 9.9 (8.7–11.1) | |
| Leg, Upper or Lower | 257† | 1.7 (0.0–3.5) | 3481 | 2.3 (1.7–2.8) | |
| Injuries by Precipitating Mechanism | 0.29 | ||||
| Overexertion | 4900 | 32.9 (26.9–38.9) | 53519 | 35.0 (33.2–36.9) | |
| Struck By/Against | 4686 | 31.5 (25.5–37.5) | 51903 | 34.0 (32.1–35.8) | |
| Fall/Takedown | 3387 | 22.7 (17.4–28.1) | 26134 | 17.1 (15.7–18.6) | |
| Unknown | 1764 | 11.8 (7.8–15.9) | 19061 | 12.5 (11.2–13.8) | |
| Other | 159† | 1.1 (0.0–2.3) | 2093 | 1.4 (0.9–1.8) | |
| Injuries by Direct Mechanism | 0.92 | ||||
| Struck By/Against | 6924 | 46.5 (40.1–52.9) | 67886 | 44.5 (42.5–46.4) | |
| Overexertion | 4918 | 33.0 (27.0–39.0) | 54283 | 35.5 (33.7–37.4) | |
| Unknown | 1758 | 11.8 (7.7–15.9) | 18783 | 12.3 (11.0–13.6) | |
| Fall/Takedown | 1062† | 7.1 (3.9–10.4) | 9622 | 6.3 (5.4–7.2) | |
| Other | 235† | 1.6 (0.0–3.2) | 2135 | 1.4 (1.0–1.9) | |
| Disposition | 0.28 | ||||
| Admit/Transfer/Observation | 436† | 2.9 (0.8–5.1) | 2883 | 1.9 (1.4–2.4) | |
| Treated and Released | 14460 | 97.1 (94.9–99.3) | 149421 | 98.1 (97.6–98.6) | |
Based on National Electronic Injury Surveillance System - AIP weights
Known body parts analyzed only
National estimates less than 1,200 cases are considered unstable by National Electronic Injury Surveillance System
The distribution of diagnoses was similar in both age groups, with sprain/strain as the most common diagnosis, followed by fracture and contusion/abrasion. There was no significant difference between the two age groups. Greater than 97% of all injuries were treated in the ED and released.
The distribution of body parts injured was significantly different between the youth and scholastic groups (p=0.02). In the youth group, wrist/hand/finger injuries were most common (18.6%, 95% CL 13.6–23.6%), followed by head/neck injuries (15.8%, 11.2–20.4%) and shoulder injuries (11.9%, 7.7–16.1%). In the scholastic group, wrist/hand/finger injuries were also most common (18.5%, 16.9–20.0%), followed closely by shoulder injuries (15.0%, 13.6–16.4%) and head/ neck injuries (14.5%, 13.2–15.9%). In both groups, approximately 75% of all injuries occurred above the waist.
Overexertion and struck by/against were the top two precipitating mechanisms for both age groups and the distribution of mechanism for both age groups was statistically similar. For direct mechanism, both groups again had the same ranking of categories, although struck by/against supplanted overexertion as the most common mechanism in both groups. Nearly 80% of all injuries directly occurred via struck by/ against and overexertion in both groups.
DISCUSSION
Our investigation is the first to compare ED treated wrestling injuries of youth participants with those of middle and high school wrestlers on a national level. We found that the overall patterns of injury were similar between both groups. This could be due to comparable rules, competition structure, and practice regimens at both levels. However, our findings are especially interesting given the overall differences in injury patterns that Yard et al.30 described when they compared high school wrestlers with their collegiate counterparts. This disparity might be explained by the fact that the rules and level of competition are more comparable for youth wrestlers and middle/high-school wrestlers than for the high school and collegiate levels.
In general, we found that the frequency of injury in scholastic (12–17 years) wrestlers was approximately ten times greater than that of youth (7–11 years) wrestlers across most categories. This is particularly noteworthy given that participation rates in the older group were only about two times higher over the entire study period suggesting that there may be differences in the rate of injury between the age groups. Strauss and Lanesse31 examined wrestling injuries in several tournaments and found that the youngest wrestlers (8–14 year olds) were injured at a rate of 3.78/100 tournament participants, whereas the high school wrestlers’ rate was 11.15/100 tournament participants. Although many studies have attempted to quantify these injury rates in various wrestling settings (multiple seasons, individual tournaments, high school and collegiate)12,30–35 and have tried to characterize the rates in different manners (player-matches, player-seasons),12,30,31,33 there is still considerable variability in the reported data, making comparison difficult. It is likely that the older wrestlers in our study faced a much greater time of wrestling exposure, participating in daily practices and more matches, whereas youth wrestlers often practice once or twice weekly with matches only on the weekend. This might explain the difference in injury rates. It is also possible that older wrestlers are stronger, more violent, or less flexible than the younger wrestlers, accounting for the difference in injury incidence. Additional evaluation of the level of injury exposure in the younger wrestlers may be warranted.
In our study, we found the annual cumulative injury incidence to be 6.49 injuries/1,000 wrestlers/year for the youth group and 29.57 injuries/1,000 wrestlers/year in the scholastic group. While significantly lower than that reported by Lanesse et al., this likely reflects the level of injury that presents to the ED. However, finding that almost 3% of the older wrestlers will require ED evaluation annually suggests that wrestling continues to have a very high rate of injury. When compared to our previously published results on football injury36, the younger athletes’ injury rates in the two sports are nearly identical (6.49/1,000 for wrestling vs. 6.1/1,000 for football), while the older wrestlers rates are almost 3 times those of football players (29.57/1,000 for wrestling vs. 11.0/1,000 for football). Future investigation is necessary to determine why the scholastic wrestlers are experiencing a higher rate of injury requiring ED evaluation.
The distribution of diagnoses in our two groups was similar, supporting what has previously been reported in the wrestling literature regarding individual tournaments, single seasons and collegiate wrestling.12,30,33,35 The distribution of diagnoses in our study was also similar to that reported for other high school sports such as football, basketball, and baseball.11 37,38 However, when compared to results from these and other sports, it is apparent that our results contain a higher representation of more severe injuries, especially fractures. This is likely due to the fact that our data include only injuries presenting to EDs and represents a higher level of medical acuity than reported in many other studies of practice or competition.
Our youth and scholastic groups were significantly different when comparing body parts injured. Youth wrestlers experienced a greater proportion of finger/wrist/hand injuries and head/neck injuries. In contrast, scholastic wrestlers injured large joints, such as the shoulder, proportionally more than the younger wrestlers. Although differences in body part groupings make it somewhat difficult to directly compare our findings with those reported by others, the high proportion of upper extremity injuries and head/neck injuries that we report is consistent with previous studies.8,12,30–33,35 Notably, this pattern of higher rates of head/neck and upper extremity injuries is more similar to sports like baseball or softball, and distinct from those of sports such as basketball or soccer, where lower extremity injuries predominate. 11,38–40 This is probably due to the unique athletic movements required in each of these individual sports. It is interesting to note that in our investigation, approximately 75% of all injuries occurred above the waist. This suggests possible preventative interventions such as equipment or rule changes as the target of further investigation.
The injury mechanisms in our study were also similar between the younger and the scholastic-aged groups. Again, the overall preponderance of contact injuries (our struck by/ against category) is consistent with existing literature.12,30,33,35,41 Where our study differs is through re-coding the dataset to involve both a precipitating and a direct mechanism. By doing this, we attempted to describe more accurately the complex interaction between the athlete and his or her competitive environment, an approach that has not been undertaken in previous wrestling research. Whereas most wrestling injuries involve direct contact with the opponent and the mat, many injury processes originate with overexertion (as defined by NEISS-AIP) in both age groups. This might suggest the need for new or different methods of training, stretching and/or conditioning.
Finally, although our findings over-represent serious injuries by looking specifically at ED data, wrestlers, coaches, parents and fans can be reassured by our finding that 97% injuries were treated and released from the ED did not require inpatient treatment. However, it must be noted that our data do not fully characterize the time loss and rehabilitation costs of the wrestling injuries seen in the ED, a major consequence of any athletic injury.
Further analysis of wrestling injuries could be improved with better information on the duration of athlete exposure, especially in the youth wrestlers and would enable quantification of risk facing these athletes. The ED is certainly a good location to capture injury data on a national basis, but future research on national wrestling injuries might explore a point of surveillance closer to the athletic competition. Additional studies might benefit from more complete or universal classifications for injury mechanisms or body parts involved, enabling better comparison and reproducibility in the literature.
In summary, our national study of wrestling injuries in young and scholastic-aged athletes disclosed many similarities between both the diagnoses and mechanisms involved. We did, however, find significant differences between groups when examining the part of the body involved in injury. While further study of this relationship is necessary, we suggest that patterns of wrestling injury in younger athletes are likely different than those of their older counterparts, and may benefit from targeted prevention efforts. Furthermore, the finding that 75% of injuries occur above the waist may signal the need for youth and high school wrestling governing bodies to consider prevention strategies including re-examination of the rules of competition for opportunities to reduce head and neck, trunk and upper extremity injuries.
LIMITATIONS
There are several limitations to our study. While the NEISS captures injuries presenting to U.S. EDs, it does not address minor wrestling injuries that are seen in a non-acute care setting or managed by coaches or trainers. These minor injuries likely make up the majority of wrestling injury encounters, making our description a significant underestimate of overall injury incidence. These minor injuries are frequently an important cause of loss of participation, as well as pain and suffering. As such, our analysis likely overemphasizes the most severe injuries seen in wrestling participation and may not be directly comparable to individual teams’ experiences.
An additional limitation of using NEISS is that it codes for only the most severe injury in the case of a multiply injured patient, thereby possibly excluding minor injuries. As mentioned earlier, catastrophic injuries involving death are excluded from NEISS and would be missed in our analysis. While death is a rare occurrence in competitive wrestling, we are unable to discuss that outcome in our study.5
Our age grouping approximated a youth wrestling (amateur club) population and compared it to an interscholastic wrestling (middle and high-school) population. Additionally, these groupings are consistent with existing participation data. However, it is possible that these age groupings overlap somewhat and may confound our data.
We attempted to restrict our analysis to only competitive wrestling (practice and competition) through two methods. First, by restricting location codes to school and place of recreation or sport, we attempted to minimize non-organized wrestling settings. Second, by review of the NEISS narrative descriptions, we were able to exclude additional records that did not involve athletic competition or training. Despite these two facets to our methodology, a few cases may have been erroneously omitted or included.
Our analysis was limited to descriptive data only. Accurate exposure (gym classes, practices and matches) data are difficult to obtain for these participants, especially at the youth wrestling level. While the National Federation of High School Sports maintains detailed annual participation data, the organizational structure at the middle school and youth levels makes it difficult to obtain similar data. However, generalized participation numbers were available for several years of our study and provided an overall comparison.
The annual injury incidence enables comparison of our results to reported injury rates in other wrestling studies and data from additional sports. Because participation statistics were not available for all study years, an average yearly participation was calculated using the four years of data out of the seven study years. With significant participation variability over the study period, the injury incidence may not accurately reflect the true exposure of athletes to wrestling injury. However, because the NSGA defines a participant as one who has participated in wrestling “at least once in the last 12 months,” the number of participants is likely an overestimate of competition level wrestlers. This would cause our calculation to be a significant underestimate of the true injury incidence.
Finally, because females make up such a small portion of the population in question, approximately 7% of all participants in our study period, we eliminated females from our analysis and our conclusions are limited to male athletes only.2
Footnotes
Reprints available through open access at http://escholarship.org/uc/uciem_westjem.
Conflicts of Interest: By the WestJEM article submission agreement, all authors are required to disclose all affiliations, funding sources, and financial or management relationships that could be perceived as potential sources of bias. The authors disclosed none.
REFERENCES
- 1.Roots and History of Olympic Wrestling. FILA Wrestling- Federation Internationale des Luttes Associees; 2009. [Google Scholar]
- 2.Sports Business Research Network. Wrestling Market Research Results: Participation. 2008. [Google Scholar]
- 3.Sports Business Research Network. High School Participation: Boys Athletics; Number of Part./Schools with Prog., By Sport. 2008. Market Research Results. [Google Scholar]
- 4.Comstock RD, Knox C, Yard E, et al. Sports-related injuries among high school athletes--United States, 2005–06 school year. MMWR Morb Mortal Wkly Rep. 2006 Sep 29;55:1037–40. [PubMed] [Google Scholar]
- 5.Boden BP, Lin W, Young M, et al. Catastrophic injuries in wrestlers. Am J Sports Med. 2002;30:791–5. doi: 10.1177/03635465020300060601. [DOI] [PubMed] [Google Scholar]
- 6.Boden BP, Jarvis CG. Spinal injuries in sports. Neurol Clin. 2008;26:63–78. viii. doi: 10.1016/j.ncl.2007.12.005. [DOI] [PubMed] [Google Scholar]
- 7.Halloran L. Wrestling injuries. Orthop Nurs. 2008;27:189–92. doi: 10.1097/01.NOR.0000320548.20611.16. [DOI] [PubMed] [Google Scholar]
- 8.Hewett TE, Pasque C, Heyl R, et al. Wrestling injuries. Med Sport Sci. 2005;48:152–78. doi: 10.1159/000084288. [DOI] [PubMed] [Google Scholar]
- 9.Luckstead EF, Patel DR. Catastrophic pediatric sports injuries. Pediatr Clin North Am. 2002;49:581–91. doi: 10.1016/s0031-3955(02)00006-8. [DOI] [PubMed] [Google Scholar]
- 10.Powell JW, Barber-Foss KD. Traumatic brain injury in high school athletes. JAMA. 1999;282(10):958–63. doi: 10.1001/jama.282.10.958. [DOI] [PubMed] [Google Scholar]
- 11.Powell JW, Barber-Foss KD. Injury patterns in selected high school sports: A review of the 1995–1997 seasons. J Athl Train. 1999;34:277–84. [PMC free article] [PubMed] [Google Scholar]
- 12.Jarret GJ, Orwin JF, Dick RW. Injuries in collegiate wrestling. Am J Sports Med. 1998;26:674–80. doi: 10.1177/03635465980260051301. [DOI] [PubMed] [Google Scholar]
- 13.Yang J, Peek-Asa C, Allareddy V, et al. Patient and hospital characteristics associated with length of stay and hospital charges for pediatric sports-related injury hospitalizations in the United States, 2000–2003. Pediatrics. 2007;119:e813–20. doi: 10.1542/peds.2006-2140. [DOI] [PubMed] [Google Scholar]
- 14.Devgan LL, Gill HS, Faustin C, et al. Posterior dislocation in a voluntary subluxator: a case report. Med Sci Sports Exerc. 2006;38:613–617. doi: 10.1249/01.mss.0000210210.40694.df. [DOI] [PubMed] [Google Scholar]
- 15.Giombini A, Di Cesare A, Sardella F, et al. Myositis ossificans as a complication of a muscle tendon junction strain of long head of biceps. A case report. J Sports Med Phys Fitness. 2003;43:75–7. [PubMed] [Google Scholar]
- 16.Johnson R. Abdominal wall injuries: rectus abdominis strains, oblique strains, rectus sheath hematoma. Curr Sports Med Rep. 2006;5:99–103. doi: 10.1007/s11932-006-0038-8. [DOI] [PubMed] [Google Scholar]
- 17.Ozcakar L, Erol O, Kara M, et al. Accessory nerve injury during amateur wrestling: silent but not overlooked. Br J Sports Med. 2003;37:372. doi: 10.1136/bjsm.37.4.372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Pearsall AWt, Russell GV., Jr Ipsilateral clavicle fracture, sternoclavicular joint subluxation, and long thoracic nerve injury: an unusual constellation of injuries sustained during wrestling. Am J Sports Med. 2000;28:904–8. doi: 10.1177/03635465000280062301. [DOI] [PubMed] [Google Scholar]
- 19.Plaga BR, Looby P, Feldhaus SJ, et al. Axillary artery injury secondary to inferior shoulder dislocation. J Emerg Med. doi: 10.1016/j.jemermed.2008.01.018. [DOI] [PubMed] [Google Scholar]
- 20.Sikka RS, Neault M, Guanche CA. An avulsion of the subscapularis in a skeletally immature patient. Am J Sports Med. 2004;32:246–9. doi: 10.1177/0363546503258906. [DOI] [PubMed] [Google Scholar]
- 21.Oppliger RA, Landry GL, Foster SW, et al. Wisconsin minimum weight program reduces weight-cutting practices of high school wrestlers. Clin J Sport Med. 1998;8:26–31. doi: 10.1097/00042752-199801000-00007. [DOI] [PubMed] [Google Scholar]
- 22.Tipton CM, Tcheng TK, Zambraski EJ. Iowa wrestling study: weight classification systems. Med Sci Sports. 1976;8:101–4. [PubMed] [Google Scholar]
- 23.Newton R, Doan B, Meese M, et al. Interaction of wrestling shoe and competition surface: effects on coefficient of friction with implications for injury. Sports Biomech. 2002;1:157–66. doi: 10.1080/14763140208522794. [DOI] [PubMed] [Google Scholar]
- 24.Grindstaff T, Potach D. Prevention of Common Wrestling Injuries. Strength and Conditioning Journal. 2006;28:20–8. [Google Scholar]
- 25.Hergenroeder AC. Prevention of sports injuries. Pediatrics. 1998;101:1057–63. doi: 10.1542/peds.101.6.1057. [DOI] [PubMed] [Google Scholar]
- 26.Best TM. Muscle-tendon injuries in young athletes. Clin Sports Med. 1995;14:669–86. [PubMed] [Google Scholar]
- 27.Adirim TA, Cheng TL. Overview of injuries in the young athlete. Sports Med. 2003;33:75–81. doi: 10.2165/00007256-200333010-00006. [DOI] [PubMed] [Google Scholar]
- 28.Xiang H, Sinclair SA, Yu S, et al. Case ascertainment in pediatric traumatic brain injury: challenges in using the NEISS. Brain Inj. 2007;21:293–9. doi: 10.1080/02699050701311034. [DOI] [PubMed] [Google Scholar]
- 29.US Dept of Health and Human Services, Centers for Disease Control and Prevention, National Center for Injury Prevention and Control, et al. NATIONAL ELECTRONIC INJURY SURVEILLANCE SYSTEM ALL INJURY PROGRAM, 2004. [Computer file]. ICPSR version: ICPSR04598-v1. Atlanta, GA: U.S. Dept. of Health and Human Services, Centers for Disease Control and Prevention, National Center for Injury Prevention and Control [producer]; 2006. [Google Scholar]; Ann Arbor MI: Inter-university Consortium for Political and Social Research [distributor]; 2006-11-21. [Google Scholar]
- 30.Yard EE, Collins CL, Dick RW, et al. An epidemiologic comparison of high school and college wrestling injuries. Am J Sports Med. 2008;36:57–64. doi: 10.1177/0363546507307507. [DOI] [PubMed] [Google Scholar]
- 31.Strauss RH, Lanese RR. Injuries among wrestlers in school and college tournaments. JAMA 22. 1982;248:2016–9. [PubMed] [Google Scholar]
- 32.Lorish TR, Rizzo TD, Jr, Ilstrup DM, et al. Injuries in adolescent and preadolescent boys at two large wrestling tournaments. Am J Sports Med. 1992;20:199–202. doi: 10.1177/036354659202000218. [DOI] [PubMed] [Google Scholar]
- 33.Pasque CB, Hewett TE. A prospective study of high school wrestling injuries. Am J Sports Med. 2000;28:509–15. doi: 10.1177/03635465000280041101. [DOI] [PubMed] [Google Scholar]
- 34.Agel J, Ransone J, Dick R, et al. Descriptive epidemiology of collegiate men’s wrestling injuries: National Collegiate Athletic Association Injury Surveillance System, 1988–1989 through 2003–2004. J Athl Train. 2007;42:303–10. [PMC free article] [PubMed] [Google Scholar]
- 35.Yard EE, Comstock RD. A comparison of pediatric freestyle and Greco-Roman wrestling injuries sustained during a 2006 US national tournament. Scand J Med Sci Sports. 2008;18:491–497. doi: 10.1111/j.1600-0838.2007.00716.x. [DOI] [PubMed] [Google Scholar]
- 36.Mello MJ, Myers R, Christian JB, et al. Injuries in youth football: national emergency department visits during 2001–2005 for young and adolescent players. Acad Emerg Med. 2009;16:243–248. doi: 10.1111/j.1553-2712.2009.00357.x. [DOI] [PubMed] [Google Scholar]
- 37.McLain LG, Reynolds S. Sports injuries in a high school. Pediatrics. 1989;84:446–50. [PubMed] [Google Scholar]
- 38.Rechel JA, Yard EE, Comstock RD. An epidemiologic comparison of high school sports injuries sustained in practice and competition. J Athl Train. 2008;43:197–204. doi: 10.4085/1062-6050-43.2.197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Borowski LA, Yard EE, Fields SK, et al. The epidemiology of US high. school basketball injuries, 2005–2007. Am J Sports Med. 2008;36:2328–35. doi: 10.1177/0363546508322893. [DOI] [PubMed] [Google Scholar]
- 40.Yard EE, Schroeder MJ, Fields SK, Collins CL, Comstock RD. The epidemiology of United States high school soccer injuries, 2005–2007. Am J Sports Med. 2008;36:1930–1937. doi: 10.1177/0363546508318047. [DOI] [PubMed] [Google Scholar]
- 41.Wroble RR, Albright JP. Neck and low back injuries in wrestling. Clin Sports Med. 1986;5:295–325. [PubMed] [Google Scholar]