Abstract
Pulmonary artery sarcomas (PAS) are rare and probably incurable tumours. The clinical manifestations are non-specific and very similar to that of patients with thromboembolic disease, resulting in delay of the correct diagnosis and proper treatment. We report the case of a 66-year-old woman with PAS diagnosed by computed tomography guided biopsy. Chemotherapy treatment was initiated but the patient died 11 months after diagnosis.
Background
Pulmonary artery sarcomas (PAS) are exceedingly rare and the prognosis is very poor regardless of treatment. The clinical presentation and physical examination are non-specific and frequently patients are misdiagnosed as having chronic thromboembolic disease. Anderson et al1 reported a series of six cases and all of them were initially investigated for chronic thromboembolism. Parish et al2 evaluated nine patients in a 30 year period; seven were originally treated as pulmonary thromboembolism. Huo et al3 reviewed reports of seven cases, of which five were thought to have chronic thromboembolism.
Case presentation
The patient was a 66-year-old woman without any previous relevant medical history. She presented with a 2 month history of shortness of breath on exertion. She was diagnosed with asthma and treated with inhaled glucocorticosteroids. There was no improvement of the dyspnoea and she developed a continuous non-pleuritic chest pain. Echocardiography revealed pulmonary hypertension that was presumed to be secondary to left ventricular dysfunction and she was treated with furosemide, digoxin and spironolactone. Because there was no improvement, she was referred to our service. At this point, the patient presented with mild exertional dyspnoea, worsening of chest pain, and reported two episodes of loss of consciousness. The cardiovascular examination revealed a prominent pulmonary component of the second heart sound. Examination of the lungs was normal.
Investigations
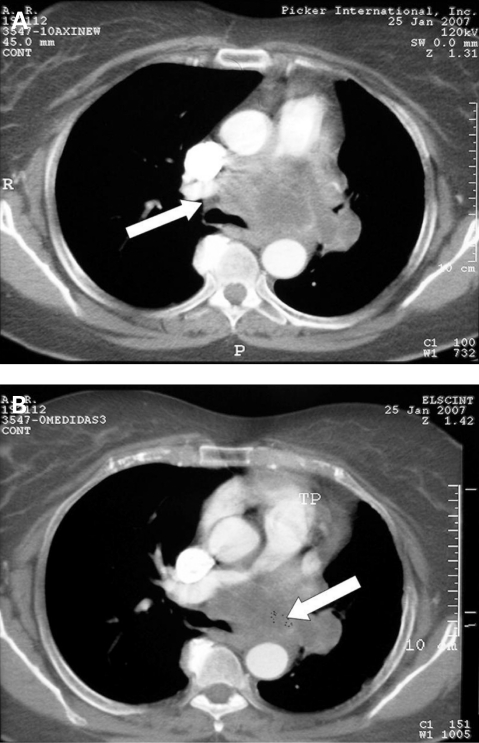
Chest x-ray showed an enlargement of the left pulmonary artery, and transthoracic echocardiography revealed right ventricular dilatation, tricuspid regurgitation and absence of blood flow into the left pulmonary artery. Computed tomography (CT) scan showed an intraluminal mass, maximal diameter 7.5 cm, obstructing the pulmonary trunk and main pulmonary branches and involving the aortic arch and descending aorta, extending to the mediastinum and involving the oesophagus (fig 1). A percutaneous CT guided biopsy of mediastinal mass was performed. Histologically, the tumour consisted of an intermediary degree spindle cell sarcoma.
Figure 1.
Computed tomography axial scans showing the pulmonary trunk lumen obliterated by a solid mass (A, white arrow); the mass extended to the entire left pulmonary artery as well as to the adjacent mediastinal fat (B, white arrow).
Treatment
Chemotherapy was initiated with paclitaxel and gemcitabine because the tumour was considered unresectable by the surgical team.
Outcome and follow-up
There was no response to chemotherapy and the patient died 11 months after diagnosis.
Discussion
Angiosarcoma is one of the rarest types of sarcoma of the thorax. The true incidence is unknown because only a hundred or so cases have been reported.1,3–5 Studies have shown a slight female preponderance and the tumour typically occurs in the sixth decade.4 The aetiology of PAS is obscure. It has been suggested to be a neoplastic transformation of primitive mesenchymal cells present in the intima of the pulmonary arteries.1,3
Diagnosis is difficult and often delayed because symptoms are insidious and nonspecific. The common symptoms are dyspnoea, cough and chest pain, with or without right ventricular dysfunction. These symptoms mimic thromboembolic disease and the patients can be easily misdiagnosed. Signs such as weight loss, fever or anaemia could also be present.1,4
Chest x-ray generally shows large masses in the anterior mediastinum and hilar enlargement. Findings on the CT scan are similar in PAS and thromboembolic disease and are characterised by filling defects at different levels in the pulmonary vasculature. Gadolinium magnetic resonance imaging (MRI) with enhancement of the lesion is indicative of the tumour. This enhancement gives MRI an advantage in the differential diagnoses because a non-vascularised intraluminal thrombus should not enhance after injection of gadolinium. Information about the enhancement on sarcoid infiltration of the pulmonary artery was not found in the literature; however, 80% of patients with infiltrative lung disease presented positive results on MRI when the disease was active.6 Surgical or percutaneous biopsy confirms the diagnosis of PAS.3 For vascular tumours there is a risk when performing CT guided biopsy, mainly haemorrhagic complications. In this case, although the mediastinal mass showed a relationship with the pulmonary trunk and main pulmonary branches, the tumour was solid and large. In addition, the surgical staff is well trained and defined that the biopsy would not be harmful to the patient. Indeed, the CT guided biopsy was performed and the patient had no complications.
Because clinical findings usually cannot distinguish between PAS and acute or chronic embolic disease, patients are initially treated with anticoagulants or even with thrombolysis. There are no studies evaluating long term anticoagulation to determine if this treatment would improve outcome. In fact, many case reports suggest that the failure of anticoagulation to improve a patient’s condition should raise the suspicion of PAS.2 This patient was referred with such advanced disease that the initial diagnosis was lung cancer, so we did not prescribe anticoagulation. Because these tumours are rare, data from large randomised trials are not available and the best treatment for primary PAS is still unknown. Case reports suggest that surgical resection is the treatment of choice for PAS, and is thought to produce the best survival rates in the earliest stages of disease. However, even after the surgery, the mean survival period is 12 months. Palliative chemotherapy is the usual treatment in advanced disease, with response rates of approximately 50%.4
Learning points
Although rare, pulmonary artery sarcoma is a differential diagnosis for pulmonary embolism.
Pulmonary angiosarcomas are difficult to diagnose and a high suspicion is needed.
Early diagnosis is associated with better prognosis.
Footnotes
Competing interests: None.
Patient consent: Patient/guardian consent was obtained for publication.
REFERENCES
- 1.Anderson BM, Kriett MJ, Kapelanski PD, et al. Primary pulmonary artery sarcoma: a report of six cases. Ann Thorac Surg 1995; 59: 1487–90 [DOI] [PubMed] [Google Scholar]
- 2.Parish JM, Rosenow III EC, Swensen SJ, et al. Pulmonary artery sarcoma: clinical features. Chest 1996; 110: 1480–8 [DOI] [PubMed] [Google Scholar]
- 3.Huo L, Lai S, Gladish G, et al. Pulmonary artery angiosarcoma: a clinicopathologic and radiological correlation. Ann Diagn Pathol 2005; 9: 209–14 [DOI] [PubMed] [Google Scholar]
- 4.Miura S, Meirmanov S, Nakashima M, et al. Intimal sarcoma of the pulmonary artery: Report of an autopsy case. Pathol Res Pract 2005; 201: 469–74 [DOI] [PubMed] [Google Scholar]
- 5.Maruo A, Okita Y, Okada K, et al. Surgical experience for the pulmonary artery sarcoma. Ann Thorac Surg 2006; 82: 2014–16 [DOI] [PubMed] [Google Scholar]
- 6.Gaeta M, Blandino A, Scribano E, et al. Chronic infiltrative lung diseases. Value of gadolinium-enhanced MRI in the evaluation of disease activity – early report. Chest 2000; 117: 1173–8 [DOI] [PubMed] [Google Scholar]