Abstract
The authors describe two cases that developed organizing pneumonia (OP) associated with novel influenza A(H1N1) virus. These patients were admitted to intensive care unit (ICU) because of severe respiratory failure. After initial clinical improvement, both patients worsened their condition during their second week of ICU stay, presenting fever, increasing in inflammatory parameters and worsening in oxygen exchange and respiratory mechanics. Chest x-rays and computed tomographies showed an increment on lung infiltrates, given by areas of consolidation and ground glass opacification. Although broad-spectrum antibiotics were administered, patients showed no improvement. All cultures, including bronchoalveolar lavage samples, were negative. In both cases, an open lung biopsy was performed, and histopathological examination of the specimen was compatible with OP. Both patients were successfully treated with high-dose corticoids. The aim of this report is to alert about the possibility of OP associated with novel influenza virus in patients with severe respiratory failure.
Background
These two cases provide clinical insight into lung involvement due to novel influenza. In our series, we confirmed 19 patients with this new virus in the intensive care unit (ICU) setting. The development of OP in two of them (more than 10%), excess by far the usual incidence of this rare disease. That is the reason why we present this case report, because we believe that OP should be considered on the differential diagnosis of patients with severe novel influenza who present fever and air space consolidation, without demonstrated infection, during in-hospital stay, mainly because is a scenario where steroids might be useful.
Case presentation
Case 1
A 52-year-old woman, smoker (15 packages/year), obese (BWI 34 kg/m2), with osteoarthritis and chronic use of glucosamine, acetaminophen and zopiclone, was admitted to emergency department, with history of 3 days dry cough, high fever, headache, myalgias, odynophagia, arthralgias, pleuritic pain and dyspnoea. Chest x-ray and CT showed show diffuse ground glass opacities with areas of peripheral and peribronchovascular lobular consolidation (figure 1). Arterial blood gases (ABG) analysis revealed severe hypoxemia (PaO2:FiO2 ratio 48), being transferred to ICU for MV. Most relevant laboratory findings at admission were WBC 4100 per mm3 with 10% of bands, platelets 113,000 per mm3, CRP 328 mg/l, Procalcitonin 2.35 ng/ml and LDH 2053 U/l. Ceftriaxone, Levofloxacin and Oseltamivir were initiated, and hydrocortisone was added, according to the local recommendations for A(H1N1) virus pandemic management. Panel viral was positive for influenza virus and specific rRT-PCR confirmed novel influenza A(H1N1) virus. Prolonged prone ventilation (PPV) was applied. All cultures, including LBA samples were negative, thus antibiotics were suspended. The patient improved progressively, and was returned to supine. However, 5 days later, her oxygen exchange deteriorated again to a PaO2:FiO2 ratio 66. Chest x-ray revealed new infiltrates. In addition, high fever and increasing inflammatory parameters (WBC, CRP, PCT) were observed. Broad-spectrum antibiotics were administered and a second period of PPV was applied. The patient was carried in prone position to a new chest CT which showed foci of ground glass had evolved to bilateral consolidations, with predominant subpleural peripheral distribution (figure 1). Having a mono-organic failure, without infection demonstrated, a pulmonary inflammatory process like organizing pneumonia (OP) was suspected. A chest surgeon performed an open lung biopsy (OLB) through minithoracotomy with the patient still in PPV. Findings confirmed an OP (figure 2) associated to novel influenza A(H1N1) virus; other causes had been excluded. Patient received a steroid pulse therapy with methylprednisolone (500 mg per day during 3 days) and significant improvement was observed. She was successfully weaned of MV and later discharged from ICU in good conditions.
Figure 1.
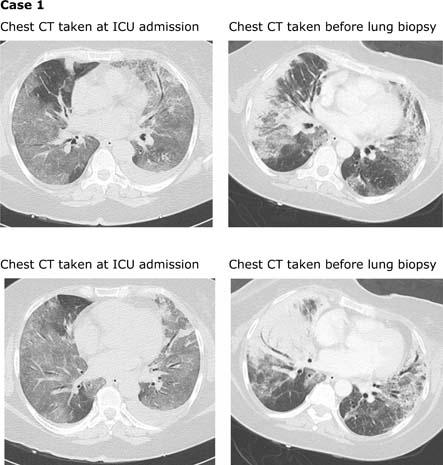
Chest CT taken at ICU admission show diffuse ground glass opacities with some peripheral and peribronchovascular lobular consolidation. Chest CT taken before lung biopsy show foci of ground glass have evolved to bilateral consolidations, predominantly in a subpleural peripheral distribution. Areas of ground glass opacities have appeared in both upper lobes (not shown in these pictures). In left lower lobe, ground glass opacities has been replaced by fine reticular intralobular opacities with traction bronchioloectasis (suggesting initial fibrosis).
Figure 2.
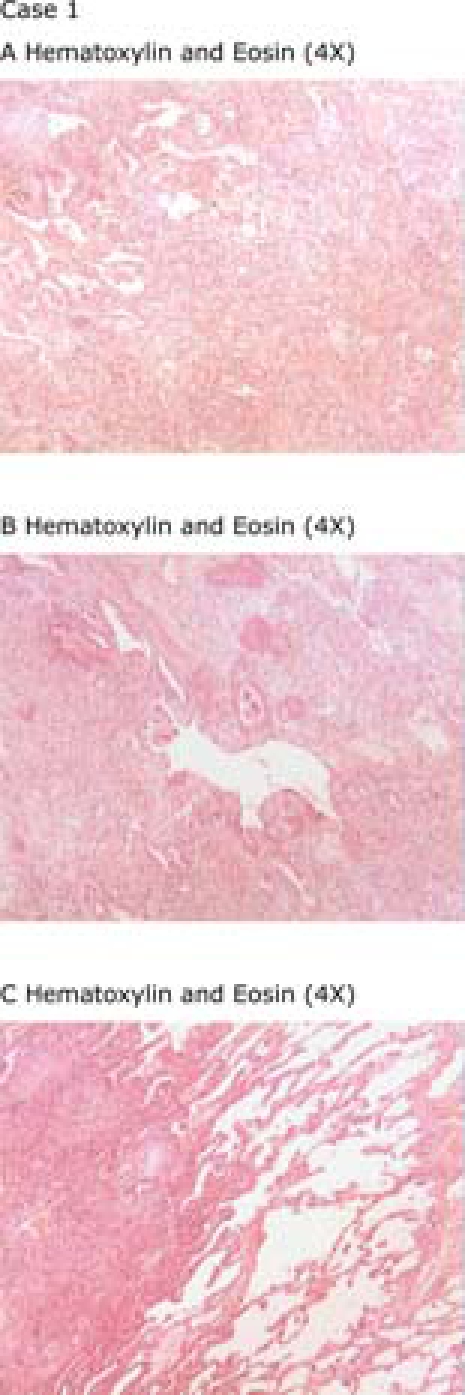
Histopathological findings in Case 1(A) Sparse intraalveolar areas of fibrin accumulation (Masson bodies) and organizing pneumonia. (B) Solid area with bronchiolar necrosis and reparative changes, squamous metaplasia and type II alveolar hyperplasia. (C) Organizing pneumonia involving 75% of the alveolar spaces in the lung parenchyma.
Case 2
A 36-year-old man, diabetic, BWI 27.8 kg/m2 was admitted to ICU because of 7 days with influenza-like illness and dyspnoea, whose ABG analysis revealed severe hypoxemia (PaO2:FiO2 ratio 131) and MV was initiated. Chest x-ray and CT showed extensive areas of ground glass opacities and air space consolidation (figure 3). Most relevant laboratory findings at ICU admission were WBC 2500 per mm3, platelets 88,000 per mm3, CRP 153 mg/l, Procalcitonin 0.54 ng/ml, CK 1046 U/l and LDH 1250 U/l. Ceftriaxone, Cotrimoxazole, Levofloxacin, Oseltamivir and hydrocortisone (300 mg per day) were administered, and PPV was applied. All cultures and serologic studies were negative, with exception of rRT-PCR for novel influenza A (H1N1) virus. Hence, only Oseltamivir was maintained. After 4 days on PPV, patient showed clinical and radiological improvement and was turned back to supine. However, 10 days later, he developed high fever, increased his inflammatory parameters (WBC 10,100 per mm3, and CRP 190 mg/l; but PCT was only 0.18 ng/ml), and worsened his oxygen exchange to PaO2:FiO2 ratio 185. CT revealed new areas of consolidation (figure 3). Second-line antibiotics were administered, but all cultures, including bronchoalveolar lavage (BAL) samples, resulted negative. The patient underwent OLB via minithoracotomy at the lower and upper left lobes. Histology confirmed the diagnosis of OP associated with novel influenza virus (figure 4). Methylprednisolone was administered using the same dose and duration described in case 1. Symptoms and radiographic findings improved rapidly, but the patient developed hyperactive delirium and critical illness neuromuscular abnormalities, both of which delayed his weaning from MV and prolonged the length of ICU stay. However, he was discharged from hospital in good conditions 40 days after admission.
Figure 3.
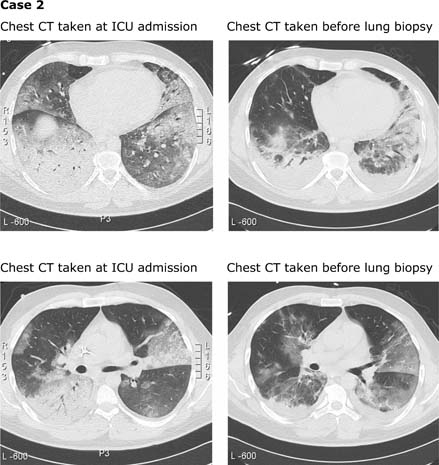
Chest CT taken at ICU admission show extensive areas of ground glass opacities and air space consolidation. Chest CT taken before lung biopsy show decrease of ground glass opacities in middle right lobe, and progression of consolidation in left lower and lingule. In addition, loss of global lung volume is observed.
Figure 4.
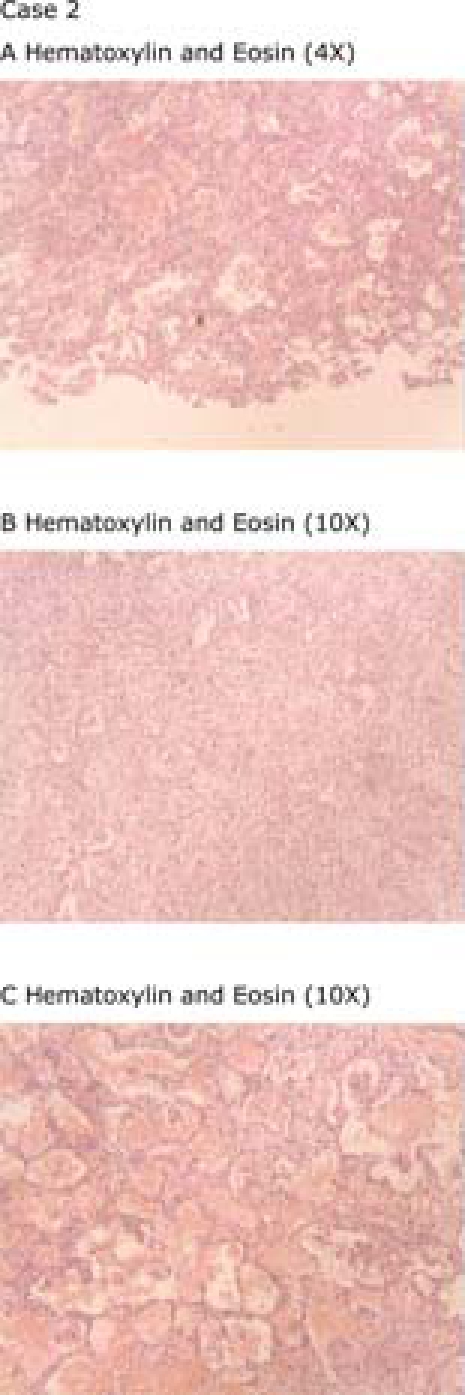
Histopathological findings in Case 2.(A) Mild interstitial inflammatory lymphoplasmacytic cell infiltrate and sparse fibrin accumulation intraalveolar. (B) Solid area of prominent organizing pneumonia and athelectasia. (C) Intraalveolar oedema and haemorrhage admixed with macrophages and Masson bodies.
Outcome and follow-up
Both patients were successfully treated and discharged from Hospital. Eight months after, they remain in good conditions, and their chest CT control significantly improved.
Discussion
Bronchiolitis obliterans OP (BOOP), which has recently been called OP, is an unusual lung disease, which is histopathologically defined by the presence of granulation tissue (inflammatory cells, fibroblasts and loose connective tissue) in the lumen of the distal pulmonary airspaces (alveoli and alveolar ducts), and in the bronchiolar lumen (Bronchiolitis obliterans), which lead to plugging of the bronchiolar and alveolar lumen.1 OP is considered a nonspecific response to many types of lung injury, including medications, toxins, radiation, connective tissue diseases, cancers, lung and bone marrow transplantation, chronic thyroiditis, alcoholic cirrhosis, inflammatory bowel disease and bacterial or virus infection.1 It is defined as idiopathic OP or cryptogenic OP (COP) when no underlying cause is present or identifiable.2
OP related to influenza viral infection only has been characterised in a few case reports, in immunocompetent and immunocompromised patients.3–6 The clinical behaviour observed in these patients does not seem to differ from OP due to other causes. However, to our knowledge, the radiographic and histological findings of OP associated to the novel pandemic influenza A (H1N1) virus have not been previously described. In our case series of 19 critical ill patients admitted to ICU because of respiratory failure and MV requirement due to severe novel A (H1N1) virus infection, 2 out of 19 developed OP. In order to establish novel influenza as the probable cause of OP in these two cases, other potential causes, including drugs, toxins and other infections, were considered, explored and excluded, leaving novel influenza as the most likely contributor.
OP remains a diagnosis of exclusion. Hence, once other most common diagnoses have been ruled out, interventional examinations should be conducted, if the patient's condition allows it, to make an early histological diagnosis and start proper treatment. BAL results are usually nonspecific, thus it is not considered of diagnostic value.7 Therefore, considering transbronchial biopsy permits accurate diagnosis only in a minority of the patients, an OLB is the evaluation of choice in order to ensure OP diagnosis.8 Interestingly, one of our patients was subjected to a CT as well as to an OLB while still being in prone position due to severe respiratory failure and no complication was observed.
The role of corticosteroids in the management of severely ill patients with novel influenza A (H1N1) virus infection is unclear and controversial. However, moderate-dose corticoids do not seem to increase the risks,9 and might be helpful in the most severe cases. Therefore, driven by some clinical similarities with SARS, and severe community-acquired pneumonia,10 11 we decided to treat all our severe patients with hydrocortisone from the ICU admission during a 7 days period. Whether this therapy was an actual contribution and in which amount, should be further evaluated in larger series.
Regarding OP treatment, it mainly consists in the administration of systemic corticosteroids, which induce frequently a rapid clinical improvement. Epler et al1 suggested an initial dose of 1 mg/kg prednisone, but there are also data showing good results using only 0.5 mg/kg.12 In our two cases, steroid therapy was very effective, too. However, we preferred a high-dose corticoid to ensure the clinical response of these two patients, because in both cases hydrocortisone treatment had been finished only recently when OP was diagnosed, and the severity of the first case required a rapid and intensive intervention. Given the evident improvement we observed in the first case with a steroid pulse therapy, we decided the second case should receive the same treatment. We cannot discard that a lower corticoids dose could have been equally effective in our patients.
When managing OP cases, it is generally suggested to continue therapy with corticosteroids for at least 6 months reducing the dose, but a common problem is relapse of disease when corticosteroids dosage is tapered off.13 After 8 months, our two of patients are in good condition without relapsing, despite they finished prednisone at 6 months.
Different clinical types of pneumonia associated with influenza virus infection have been reported: influenza complicated by secondary bacterial pneumonia, primary influenza virus pneumonia and combined influenza virus and bacterial pneumonia.14 Nevertheless, these cases suggest that OP should be kept in mind as other possible type of associated pneumonia, when treating patients who present this clinical behaviour following influenza-like illness by novel A (H1N1) virus infection.
The pathologic features of pulmonary influenza virus infection that have been described are as follows: necrotizing tracheobronchitis, enlargement and vacuolisation of respiratory epithelial cells, fibrinous pneumonia (diffuse alveolar damage), secondary bacterial pneumonia (especially pneumococcal) and Bronchiolitis obliterans with OP.15–19
These two cases provide clinical insight into lung involvement due to novel influenza. Although 19 confirmed patients with this new virus in the ICU setting may appear as a limited series, the development of OP in more than 10% of these patients excess by far the usual incidence of this rare disease, and suggests OP should be considered on the differential diagnosis of patients with severe novel influenza who present high fever and air space consolidation, without demonstrated infection, during in-hospital stay.
Learning points
OP should be considered on the differential diagnosis of patients with severe novel influenza who present high fever and air space consolidation, without demonstrated infection, during in-hospital stay.
OP remains a diagnosis of exclusion. Hence, once other most common diagnoses have been ruled out, interventional examinations should be conducted, if the patient's condition allows it, to make an early histological diagnosis and start proper treatment.
Open lung biopsy is the evaluation of choice in order to ensure OP diagnosis. Inclusive in those patients with severe respiratory failure is feasible and relatively safe.
Footnotes
Competing interests None.
Patient consent Obtained.
References
- 1.Epler GR, Colby TV, McLoud TC, et al. Bronchiolitis obliterans organizing pneumonia. N Engl J Med 1985;312:152–8 [DOI] [PubMed] [Google Scholar]
- 2.Lohr RH, Boland BJ, Douglas WW, et al. Organizing pneumonia. Features and prognosis of cryptogenic, secondary, and focal variants. Arch Intern Med 1997;157:1323–9 [DOI] [PubMed] [Google Scholar]
- 3.Staud R, Ramos LG. Influenza A-associated bronchiolitis obliterans organizing pneumonia mimicking Wegener's granulomatosis. Rheumatol Int 2001;20:125–8 [DOI] [PubMed] [Google Scholar]
- 4.Case records of the Massachusetts General Hospital. Weekly clinicopathological exercises. Case 36–2001. Acute febrile respiratory illness in a 57-year-old man with recurrent pulmonary disorders. N Engl J Med 2001;345:1558–65 [DOI] [PubMed] [Google Scholar]
- 5.Murata Y, Walsh EE, Falsey AR. Pulmonary complications of interpandemic influenza A in hospitalized adults. J Infect Dis 2007;195:1029–37 [DOI] [PubMed] [Google Scholar]
- 6.Fujita J, Bandoh S, Yamaguchi M, et al. Chest CT findings of influenza virus-associated pneumonia in 12 adult patients. Influenza Other Respi Viruses 2007;1:183–7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Nagai S, Aung H, Tanaka S, et al. Bronchoalveolar lavage cell findings in patients with BOOP and related diseases. Chest 1992;102(1 Suppl):32–7S [DOI] [PubMed] [Google Scholar]
- 8.Alasaly K, Muller N, Ostrow DN, et al. Cryptogenic organizing pneumonia. A report of 25 cases and a review of the literature. Medicine 1995;74:201–11 [DOI] [PubMed] [Google Scholar]
- 9.Salluh JI, Póvoa P, Soares M, et al. The role of corticosteroids in severe community-acquired pneumonia: a systematic review. Crit Care 2008;12:R76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Montón C, Ewig S, Torres A, et al. Role of glucocorticoids on inflammatory response in nonimmunosuppressed patients with pneumonia: a pilot study. Eur Respir J 1999;14:218–20 [DOI] [PubMed] [Google Scholar]
- 11.Meduri GU, Tolley EA, Chrousos GP, et al. Prolonged methylprednisolone treatment suppresses systemic inflammation in patients with unresolving acute respiratory distress syndrome: evidence for inadequate endogenous glucocorticoid secretion and inflammation-induced immune cell resistance to glucocorticoids. Am J Respir Crit Care Med 2002;165:983–91 [DOI] [PubMed] [Google Scholar]
- 12.Flowers JR, Clunie G, Burke M, et al. Bronchiolitis obliterans organizing pneumonia: the clinical and radiological features of seven cases and a review of the literature. Clin Radiol 1992;45:371–7 [DOI] [PubMed] [Google Scholar]
- 13.Lazor R, Vandevenne A, Pelletier A, et al. Cryptogenic organizing pneumonia. Characteristics of relapses in a series of 48 patients. The Groupe d'Etudes et de Recherche sur les Maladles “Orphelines” Pulmonaires (GERM”O”P). Am J Respir Crit Care Med 2000;162(2 Pt 1):571–7 [DOI] [PubMed] [Google Scholar]
- 14.Louria DB, Blumenfeld HL, Ellis JT, et al. Studies on influenza in the pandemic of 1957-1958. II. Pulmonary complications of influenza. J Clin Invest 1959;38(1 Part 2):213–65 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Lucksch F. Pathologic anatomy of influenza: a review based chiefly on German sources. Arch Pathol 1928;5:448–91 [Google Scholar]
- 16.Winterbauer RH, Ludwig WR, Hammar SP. Clinical course, management, and long-term sequelae of respiratory failure due to influenza viral pneumonia. Johns Hopkins Med J 1977;141:148–55 [PubMed] [Google Scholar]
- 17.Laraya-Cuasay LR, DeForest A, Huff D, et al. Chronic pulmonary complications of early influenza virus infection in children. Am Rev Respir Dis 1977;116:617–25 [DOI] [PubMed] [Google Scholar]
- 18.Yeldandi AV, Colby TV. Pathologic features of lung biopsy specimens from influenza pneumonia cases. Hum Pathol 1994;25:47–53 [DOI] [PubMed] [Google Scholar]
- 19.Guarner J, Shieh WJ, Dawson J, et al. Immunohistochemical and in situ hybridization studies of influenza A virus infection in human lungs. Am J Clin Pathol 2000;114:227–33 [DOI] [PubMed] [Google Scholar]


