Abstract
A 19-year-old woman presented with a left upper abdominal mass. Computed tomography of the abdomen showed a solitary cystic lesion in the splenic hilum, approximately 20×16 cm in size, demonstrating almost total displacement of the remaining splenic parenchyma. She had high serum concentrations of carbohydrate antigen 19-9 and cancer antigen 125. A splenectomy was performed. Immunohistochemical study confirmed the existence of an epithelial cyst. Following surgery, the serum concentrations of the tumour markers decreased gradually. True splenic cysts are rare and their origin is controversial. In splenic cysts with high serum concentrations of tumour markers, such as occurred in our patient, cystectomy or splenectomy were preferred to remove tumour marker-producing epithelium and to prevent recurrence after treatment. If the epithelial lining of the cyst cannot be detected under light microscopy, immunohistochemical study should be performed.
BACKGROUND
Although splenic cysts are unusual in everyday surgical practice, the number of cases of splenic cysts being detected is increasing with advances in diagnostic modalities. Most cysts are asymptomatic and do not require treatment. On the other hand, giant cysts are very rare, but they often become symptomatic and critical due to enlargement, infection, and rupture. Cysts >15 cm in size are considered giant.1
Splenic cysts were classified by Martin into two major categories: primary or true cysts with epithelial lining of the cystic wall that may be parasitic or non-parasitic; and secondary or pseudocysts without true epithelial lining. True non-parasitic splenic cysts are rare.2
Although carbohydrate antigen 19-9 (CA 19-9) is a well known marker for pancreatic adenocarcinoma, high concentrations of CA 19-9 may be seen in patients with benign gastrointestinal and hepatobiliary diseases. Moreover, elevated CA 19-9 serum concentrations have been rarely reported in patients with splenic cysts.3–8
We report a rare case of giant true splenic cyst with high serum values of CA 19-9 and cancer antigen 125 (CA 125), and discuss the possible origin of the epithelial splenic cysts and the treatment strategies employed.
CASE REPORT
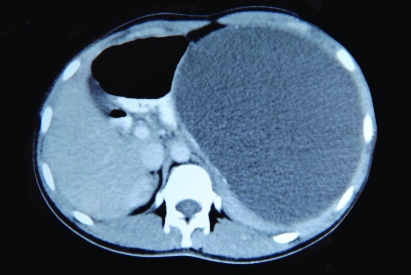
A 19-year-old woman, with no significant past medical or surgical history, presented with a 6 month history of left upper abdominal pain and a mass. On abdominal examination, an elastic-hard mass in the left upper abdomen and epigastrium was palpable and tender. Ultrasonography detected a giant cyst with septum within spleen. Computed tomography (CT) scan of the abdomen showed a solitary cystic lesion in the splenic hilum, approximately 20×16 cm in size, demonstrating almost total displacement of the remaining splenic parenchyma (fig 1). No other intra-abdominal abnormality was found. The patient had no history of previous abdominal or back trauma. A gynaecological examination, CT scan and ultrasound did not reveal any gynaecological diseases, including ovarian lesions and endometriosis. The indirect haemagglutination test and the enzyme linked immunosorbent assay (ELISA) for Echinococcus were negative. Serum concentrations of the tumour markers (normal values) were as follows: CA 19-9, 349 U/ml (normal ⩽35 U/ml); CA 125, 50 U/ml (normal ⩽35 U/ml); CA 15-3, 10 U/ml (normal ⩽31.3 U/ml); carcinoembryonic antigen (CEA), 1.34 ng/ml (normal ⩽3 ng/ml). Other laboratory tests were normal.
Figure 1.
Abdominal computed tomography scan showing a solitary cystic lesion in the splenic hilum, approximately 20×16 cm in size, demonstrating almost total displacement of the remaining splenic parenchyma.
The patient underwent laparotomy by means of a midline incision. The large cyst adhered to the stomach and abdominal surface of left diaphragm. Because the lesion was situated near the hilum, and organ preserving surgery was not possible, after complete mobilisation the intact cyst was removed together with the spleen (fig 2). Exploration of the entire abdomen was negative for further disease. Her postoperative course was uneventful, and she was discharged on day 6 after surgery.
Figure 2.
Macroscopic view of the splenic cyst.
Pathological findings
The resected spleen weighed 3500 g and measured 25×18×15 cm. The cyst contained pale brownish proteinous fluid and measured 19×16 cm. The inner surface of the cyst was brownish and rough, like granulation tissue (fig 3). The material was fixed in 10% buffered formalin, and sections for microscopy were stained with haematoxylin and eosin (H&E). The immunohistochemical study was done using the avidin-biodin complex method. Histologically, the wall of the cyst was composed of dense hyalinofibrous tissue. The lining attenuated and atrophic epithelium was indistinct in H&E section. There was haemorrhage with haemosiderin laden cells. With immunohistochemical study the epithelial lining cells were positive for cytokeratins (CK7, AE1/AE3) (fig 4), epithelial membrane antigen, and CA 19-9. In addition, the epithelial lining cells were weakly positive for CA 125. Calretinin, HBME-1 and CEA were absent in the lining cells of the cyst. According to the microscopic, macroscopic and immunohistochemical findings, a diagnosis of splenic epithelial cyst was made.
Figure 3.
Cut section of the cyst, showing a granular appearance.
Figure 4.
In the immunohistochemical study, the lining attenuated and atrophic epithelium of true splenic cyst were positive for cytokeratin (AE1/AE3).
The concentrations of CA 19-9 and CA 125 in the cyst fluid were 48 217 U/ml and 1162 U/ml, respectively.
Two months after the surgery, the serum concentrations of the tumour markers were 46 U/ml for CA 19-9, 20 U/ml for CA 125, 12 U/ml for CA 15-3, and 0.87 ng/ml for CEA. Three months later, the values of CA 19-9 and the other tumour markers were normal.
DISCUSSION
Although the number of cases of splenic cysts is increasing with advances in diagnostic modalities, true cysts of the spleen are still rare.1 Depending on the cellular lining of the cystic wall, true splenic cysts are divided into epithelial or mesothelial. The origin of epithelial cysts is controversial. Their histogenesis has been attributed to the embryonic inclusion of epithelial tissue from adjacent organs, and to post-traumatic invagination of mesothelial cells.3 There is also evidence that the epithelial lining of the cyst wall could be a result of squamous metaplasia of the mesothelial lining.4 Thus, all true splenic cysts should be considered to be of mesothelial origin. However, in the present case, the epithelial origin of the true splenic cyst was assessed by immunohistochemical analysis, showing strong positivity of cellular lining for epithelial antigens (epithelial membrane antigen, AE1/AE3, CK 7) but not for mesothelial antigens (calretinin, HBME-1). Lieto et al3 also showed that true epithelial cysts originated from epithelial cells, such as our case.
Some true cysts with completely atrophied or desquamation cellular lining may be assumed to be pseudocysts. The exact diagnosis can be established, when pathologic examination of the entire cyst wall can be performed.5 In the present case, epithelial lining of the entire cyst wall was not seen with microscopic examination. Even though it was thought to be a pseudocyst, according to the light microscopy findings, because of the lack of history of trauma and high CA 19-9 and CA-125 serum concentrations, immunohistochemical study was performed whether it was a true splenic cyst or not. Thus, the lining attenuated and atrophic epithelium cells were detected with immunohistochemical study and the diagnosis of true splenic cyst was confirmed.
CA 19-9 is a well known marker for diagnosing and managing patients with pancreatic adenocarcinoma. However, its usefulness is rather limited because elevated serum values of CA 19-9 may be encountered in patients with other gastrointestinal adenocarcinomas or even benign disorders, with a sensitivity and specificity of 77% and 88%, respectively.3 The first case of a splenic cyst with elevated serum CA 19-9 was reported by Terada et al6 in 1994. Since then, elevated CA 19-9 serum values have been reported in approximately 30 cases of splenic cysts, most of epithelial origin.7 However, in a few cases with elevated CA19-9 serum concentrations, concurrent high values of the other cancer antigens such as CEA and CA 125 have been reported. In previous cases, the splenic cyst contents also showed an abnormally high concentration of the tumour markers, and they were localised in the lining of the epithelial cells, as in the present case.3,8 Our patient also had elevated preoperative CA 19-9 and CA125 serum values, which decreased to within normal limits following splenectomy. Therefore, the elevation is most likely due to production of the tumour markers in the splenic cysts, and the decrease in their serum concentrations following surgery supports this notion.
The optimal treatment strategy for patients with non-parasitic splenic cysts remains controversial. Published patient series are usually small and follow-up evaluation often incomplete.1 Cysts >5 cm are susceptible to haemorrhage, rupture, and infection and should be managed surgically, even when asymptomatic.1,5,9 Conservative options such as percutaneous aspiration and sclerosis of cysts are reported to be ineffective.9 Various surgical procedures have been described based on the patient’s age and the size, location, and nature of the cyst. Earlier, the classic approach to splenic cysts was laparotomy and complete splenectomy. However, there was a trend toward more conservative surgery after the 1970s, because of the appearance of overwhelming life threatening septicaemia, especially in children who underwent splenectomy. Indeed, the spleen has an important role in haematopoiesis, immune function, and protection against infections and malignancies. Today, the optimal treatment options are partial splenectomy (preserving >25%), total cystectomy, marsupialisation or cyst decapsulation (unroofing), with access by open laparotomy or laparoscopy.1,10 The recurrence of splenic cysts occurs usually in cases where the primary splenic cyst was incompletely removed. Because malignant degeneration of primary splenic cysts is generally not expected, and to prevent recurrence after treatment of primary splenic cysts, partial splenectomy can be performed.9 However, any type of conservative procedure is difficult to perform if the cyst is very large, is located in the splenic hilum, is covered completely by the splenic parenchyma (intrasplenic cyst), or if there are multiple cysts (polycystic). Complete splenectomy is indicated in these cases, using either the open or the laparoscopic approach because of the risk of intractable bleeding from the spleen.1,9,10
In the preoperative setting, it is hard to distinguish between primary and secondary splenic cysts. Patient history (age, gender, and history of trauma) is not very reliable. Ultrasound and CT scan do not help in determining the cyst type. The epithelium lining some true splenic cysts may produce tumour markers such as CA 19-9, CA 125, CA 50, and CEA.9 Intraoperatively, the gross appearance of the cyst and cyst fluid can be assessed, and a frozen section of the cyst wall can be performed. In intraoperative frozen section, the presence or absence of an epithelial lining is not always completely reliable. If a lining epithelium is present, a primary cyst is suspected, and a partial splenic resection or cystectomy can be performed.7,9 If no lining epithelium is present, a secondary cyst is suspected, and a decapsulation or marsupialisation should be performed, despite the possible microscopic pitfalls.9 The exact diagnosis can only be established postoperatively, when pathologic examination of the cyst wall can be performed.1,9
In our case the cyst was of a significant size. We had to treat the large cyst located in the hilum, whereas the splenic parenchyma consisting of a rim of tissue was pushed to the periphery. Therefore, both indications for splenectomy were met—location and dimension. Because laparoscopic splenectomy is not performed routinely in our centre and the cyst was very large, we performed an open complete splenectomy. The cyst was proven to be a true epithelial cyst.
In conclusion, when a splenic cyst is diagnosed, serum values of the tumour markers should be measured. In splenic cysts with high serum concentrations of tumour markers, such as in our patient, a cystectomy or splenectomy are preferred to rule out malignant lesions, to remove tumour marker-producing epithelium, and to prevent recurrence after treatment. Those splenic cysts with high serum concentrations of tumour markers, that do not have evidence of any trauma, should undergo immunohistochemical study for true splenic cyst, if the epithelial lining of the cyst cannot be discovered under light microscopy. The lining attenuated and atrophic epithelium of a true splenic cyst can be demonstrated by immunohistochemical study.
LEARNING POINTS
Benign true spleen cysts are uncommon and rarely associated with elevated serum and intracystic tumour markers CA 19-9 and CA125.
In splenic cysts with high serum concentrations of tumour markers, cystectomy or splenectomy are preferred to rule out malignant lesions, to remove tumour marker-producing epithelium, and to prevent recurrence after treatment.
In splenic cysts with high serum concentrations of tumour markers that do not have evidence of any trauma, immunohistochemical study for true splenic cyst should be undertaken if the epithelial lining of the cyst cannot be demonstrated under light microscopy.
The lining attenuated and atrophic epithelium of a true splenic cyst can be demonstrated by immunohistochemical study.
Footnotes
Competing interests: none.
Patient consent: Patient/guardian consent was obtained for publication
REFERENCES
- 1.Palanivelu C, Rangarajan M, Madankumar MV, et al. Laparoscopic internal marsupializaton for large nonparasitic splenic cysts: effective organ-preserving technique. World J Surg 2008; 32: 20–5 [DOI] [PubMed] [Google Scholar]
- 2.Martin JW. Congenital splenic cysts. Am J Surg 1958; 96: 302–8 [DOI] [PubMed] [Google Scholar]
- 3.Lieto E, Castellano P, Ferraraccio F, et al. Normal interleukin-10 serum level opposed to high serum levels of carbohydrate antigen 19-9 and cancer antigens 125 and 50 in a case of true splenic cyst. Arch Med Res 2003; 34: 145–8 [DOI] [PubMed] [Google Scholar]
- 4.Trompetas V, Panagopoulos E, Priovolou-Papaevangelou M, et al. Giant benign true cyst of the spleen with high serum level of CA 19-9. Eur J Gastroenterol Hepatol 2002; 14: 85–8 [DOI] [PubMed] [Google Scholar]
- 5.Morgenstern L. Nonparasitic splenic cysts: pathogenesis, classification, and treatment. J Am Coll Surg 2002; 194: 306–14 [DOI] [PubMed] [Google Scholar]
- 6.Terada T, Yasoshima M, Yoshimitsu Y, et al. Carbohydrate antigen 19-9 producing giant epithelial cyst of the spleen in a young woman. J Clin Gastroenterol 1994; 18: 57–61 [DOI] [PubMed] [Google Scholar]
- 7.Paksoy M, Karabicak I, Kusaslan R, et al. Laparoscopic splenic total cystectomy in a patient with elevated CA 19-9. JSLS 2006; 10: 507–10 [PMC free article] [PubMed] [Google Scholar]
- 8.Hashimoto T, Sugino T, Fukuda T, et al. Multiple epithelial cysts of the spleen and on the splenic capsule, and high serum levels of CA19-9, CA125 and soluble IL-2 receptor. Pathol Int 2004; 54: 349–54 [DOI] [PubMed] [Google Scholar]
- 9.Mertens J, Penninckx F, DeWever I, et al. Long-term outcome after surgical treatment of nonparasitic splenic cysts. Surg Endosc 2007; 21: 206–8 [DOI] [PubMed] [Google Scholar]
- 10.Macheras A, Misiakos EP, Liakakos T, et al. Non-parasitic splenic cysts: a report of three cases. World J Gastroenterol 2005; 11: 6884–7 [DOI] [PMC free article] [PubMed] [Google Scholar]