Abstract
Context
Efforts to improve care for nursing home residents stand to be enhanced by measures to assess the degree to which staff provide palliative care. As the incidence of death in nursing homes increases with the aging population, the gap in measurement must be addressed. To that end, we report the development and psychometric testing of a nursing home palliative care survey.
Objectives
The purpose of this study was to evaluate the psychometric properties of the Palliative Care Survey for use in nursing homes.
Methods
Psychometric evaluation of the instrument was completed in two phases. Phase 1 focused on individual item analyses and subsequent revision or deletion of items, and Phase 2 evaluated evidence for reliability and validity. Phase 1 included 26 nursing homes and staff (n = 717) and Phase 2 included 85 nursing homes and staff (n = 2779). Data were analyzed using item-total correlations, Cronbach’s alpha, confirmatory factor analysis, and analysis of variance (ANOVA).
Results
Support was obtained for a 51-item Palliative Care Survey (PCS) made up of two constructs Palliative Care Practice and Palliative Care Knowledge.
Conclusion
The PCS measures the extent to which nursing home staff engage in palliative care practices and have knowledge consistent with good end-of-life care. Both practice and knowledge are an essential foundation to providing good end-of-life care to nursing home residents. Efforts to improve care for the dying in nursing homes have been slowed by an absence of measurement tools that capture care processes; a gap, which the Palliative Care Survey reported here, helps fill.
Keywords: Palliative care, nursing homes
Introduction
As the American population ages, nursing homes are increasingly a setting for end-of-life care. More than 1,000 people a day die in long-term care settings nationally and in some states, as many as one in three older adults die in nursing homes. 1, 2 By the year 2020, 40% of those over 65 will die in nursing homes. 3 Too often, nursing home residents die in pain with unrelieved physical and psychosocial suffering. 4-7 While death is inevitable for permanently placed residents, undue suffering is not.
Long-standing concerns exist about the quality of care in nursing homes. Evidence indicates that quality has improved; however, serious problems continue in areas that commonly affect end of life such as use of feeding tubes, transfer to hospital, and symptom management for dyspnea and pain. 5, 8-12 These findings indicate that incorporating palliative care practices, such as advance care planning, pain management, and bereavement care for family and staff, is central to improving end-of-life experiences for residents.
The World Health Organization 15 defines palliative care as an approach to care:
…that improves the quality of life of patients and their families facing the problems associated with life-threatening illness, through the prevention and relief of suffering by means of early identification and impeccable assessment and treatment of pain and other problems, physical, psychosocial, and spiritual (http://www.who.int/cancer/palliative/definition/en/).
Palliative care is both a philosophy and a care delivery approach. For nursing homes, palliative care includes a resident/family centered focus, enhances residents’ quality of life, and complements traditional restorative interventions. 16, 17 In nursing homes that have a palliative care focus, 4, 5, 18 staff embrace death as a normal and inevitable outcome for permanently placed residents. Further, staff: a) engage in advance care planning, i.e., to talk openly about dying and to elicit residents’ personal preferences regarding end-of-life care upon admission, at care plan meetings, and whenever a resident’s condition changes; b) are knowledgeable about and engage in active symptom management; c) integrate palliative planning and interventions demonstrated by fewer unnecessary hospitalizations and feeding tubes, and more hospice referrals; d) provide psychosocial support for dying residents and their family members; e) employ bereavement interventions, such as memorial services, for staff, other residents, and family members; and f) provide staff continuing education regarding palliative care. 4, 5, 13, 16, 19
Although palliative care guidelines exist 16 and small scale palliative care models have been developed, tested, and found beneficial, 20-22 the widespread adoption of these guidelines and/or the diffusion of innovative models has not occurred. 19 Nursing homes that regularly refer residents to hospice provide a stronger palliative care focus and demonstrate positive outcomes such as fewer hospitalizations, lower feeding tube rates, and better pain management. Hospice may have a positive impact on resident care, but only 6% of nursing home residents nationally receive the hospice benefit. 23 Additional studies are needed that evaluate and link the processes of care provided by nursing home staff to resident outcomes at the end of life.
From our previous work, largely qualitative, factors such as staffing levels, staff communication and teamwork, and the provision of palliative care interventions significantly impacted care decisions, such as the use of hospice and hospitalization, and resident outcomes, such as the degree of physical and psychosocial suffering. 4, 5, 18, 24-26 Nursing homes whose staff demonstrated stronger communication and teamwork practices had a stronger foundation for the delivery of palliative care 5, 18, 26 but communication and teamwork are not sufficient for the delivery of palliative care. For example, staff may work well in teams, but if staff lacked sufficient clinical knowledge about pain management or did not engage in advance care planning, the provision of optimal palliative interventions did not occur. Further, if nursing home administrators did not support a positive philosophical orientation toward death and dying through activities such as bereavement support for staff and family or hospice referrals, the delivery of palliative care also was impeded. 5, 13
Efforts to improve care for residents stand to be enhanced by measures to assess the degree to which nursing home staff provides palliative care. Many measures capture variables related to good end-of-life outcomes such as satisfaction with care, pain management, and honoring of preferences. 14, 27 As the incidence of death in nursing homes increases with the aging population, the gap in measurement regarding care processes must be addressed. Illuminating the relationship between care processes, i.e, what staff do for residents and resident outcomes (e.g., satisfaction with care or quality of life), will provide a more comprehensive evaluation of nursing home care and offer opportunities to develop targeted interventions to enhance care. Given the increasing importance of helping nursing homes achieve the best environment for optimal end-of-life care, an assessment method that captures the various components of palliative care processes is needed. To that end, we report the development and psychometric testing of a nursing home palliative care survey.
Methods
Instrument Development
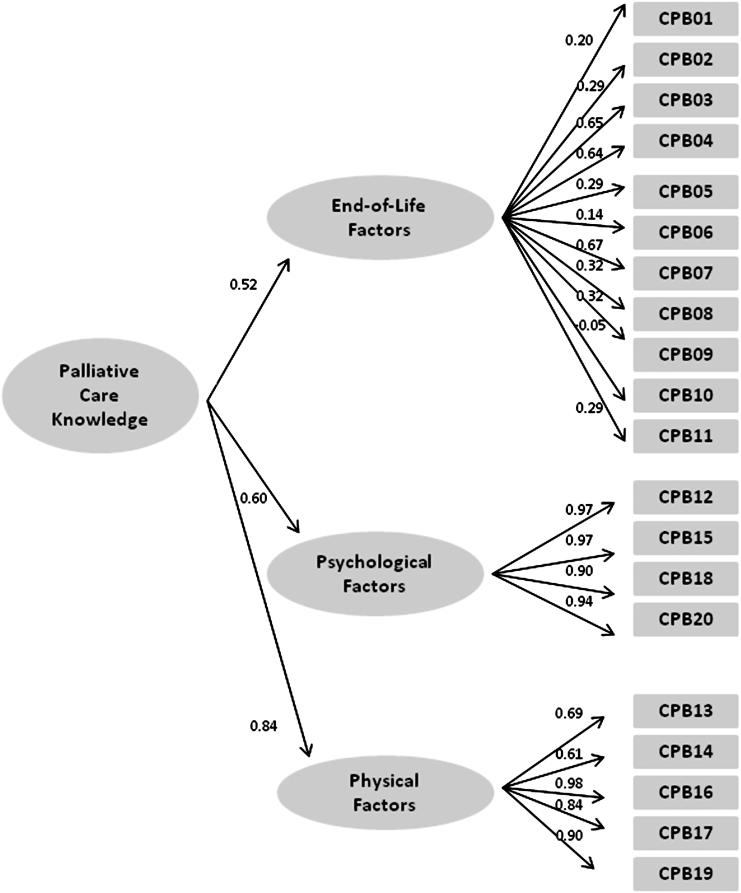
Following a review of the literature and the first author’s qualitative data from nursing homes, 4, 5, 18, 24-26, 28 palliative care, for the survey, was proposed as an overarching latent construct composed of two constructs, each reflecting different elements of palliative care. The Palliative Care Survey (PCS) encompasses: Palliative Care Practice and Palliative Care Knowledge. Palliative Care Practice reflects what nursing home staff do, their actions or interventions that demonstrate a palliative approach to care and Palliative Care Knowledge reflects basic knowledge that underpins care planning and decision making (see Table 1). Palliative Care Practice comprises four subconstructs: bereavement, planning/intervention, communication with family, and provider coordination. Bereavement items reflect attention to the grieving process such as emotional support for family, staff, and residents and activities such as memorial services. Planning and intervention reflects the timing of care planning decisions including orders for do-not-resuscitate, hospice referrals, and the use of feeding tubes. Communication with family addresses provider/staff and family understanding regarding the plan of care. Provider coordination reflects nursing home staff and provider coordination of palliative interventions such as pain management and hospice referrals. Palliative Care Knowledge comprises three subconstructs: psychological, physical, and end-of-life factors. Psychological and physical items reflect knowledge regarding palliative practices to manage pain and symptoms. Items, for example, focus on when to administer pain medication and factors that influence physical discomfort. The end-of-life factors subconstruct reflects knowledge surrounding common end-of-life issues such as the management of weight loss.
Table 1.
Palliative Care Survey Example Items
| Palliative Care Practice | Example Items |
|---|---|
| Bereavement | When a resident dies, I follow up with his/her roommate to provide emotional support. |
| We have memorials for residents who die. | |
| Provider Coordination | When residents are at the end of life, the primary care provider:
|
| Communication with Family | When a resident approaches death, how often do family members:
|
| Planning/interventions | When would a hospice referral be made for Mrs. Davis?a
|
| Palliative Care Knowledge | |
| Psychological | Anxiety contributes to physical pain |
| Physical | Residents can sleep when they have physical pain. |
| End-of-life factors | Feeding tubes prevent aspiration. |
Item is based on a resident case vignette,
Initially, care planning and intervention items were developed in two formats to compare what format elicited greater variability in responses. For example, some of the planning/intervention items were embedded within an unfolding, resident-centered case vignette where respondents were provided a story about a resident on admission followed by a three-month update where the resident had declined. Questions were based on the admission status as well as the resident’s three-month declining status. The same questions, without a case vignette, were placed elsewhere in the survey.
The initial draft of the PCS included 94 items. Following the initial item development, a debriefing process, similar to cognitive interviewing, was conducted to establish developmental validity. 29, 30 Participants (n = 16) from two nursing homes known to have palliative care programs included a nurse practitioner, a director of nursing, a palliative care nurse, social workers, registered nurses (RNs), licensed practical nurses (LPNs), and certified nurse assistants (CNAs). Each staff participant completed the survey and then participated in a face-to-face discussion with an interviewer to give his/her interpretation of the items including the case vignette, difficulties completing items, rationale for responses to items, and overall comments regarding the relevance of the items to palliative care and the nursing home environment. Clarifying information was elicited about the appropriate wording of items. Items were revised or deleted based on staff comments leaving a total of 70 items for further testing.
Psychometric evaluation of the instrument was completed in two phases. Phase 1 focused on individual item analyses and subsequent revision or deletion of items. Phase 2 gathered evidence for reliability and validity. Each phase received Institutional Review Board approval. Table 2 displays the job characteristics of study participants in the two phases.
Table 2.
Job Title Characteristics of Study Personnel
| Job title | Phase 1 n = 717 n (%) |
Phase 2 n = 2779 n (%) |
|---|---|---|
| Certified nurse assistant |
360 (50) | 1424 (51) |
| Licensed practical nurse |
76 (11) | 472 (17) |
| Registered nurse | 58 (8) | 362 (13) |
| Restorative | 23 (3) | 126 (5) |
| Activities | 12 (2) | 156 (6) |
| Social Services | 16 (2) | 104 (4) |
| Unknown | 172 (24) | 135 (5) |
Phase 1
Sample and Setting
For the initial testing of the 70-item survey, a list of nursing homes within one hour of a Midwestern metropolitan area (n = 99) was generated and randomly sorted. Based on the order of the sorting, the first 26 nursing homes were invited to participate with 77% (n=20) of the homes agreeing. In addition, four homes were purposefully selected and added because of their established palliative care programs. Of the participating homes (n = 24), 11 homes (46%) were non-profit; two homes were Medicaid only, while the remaining 22 homes were dually Medicare-Medicaid certified. Nursing home bed size ranged from 60 to 300 (M = 126). Direct care staff (n=717), including nursing, social service, activities, and restorative personnel, completed the surveys.
Data Analysis
Dimensionality was explored using principal components exploratory factor analysis with Varimax rotation. Items with < 0.30 factor loadings were deleted. Initial factors were examined based on eigenvalues greater than one, the scree plot, and conceptual congruence, that supported the four hypothesized subconstructs: bereavement, planning/intervention, family communication, and provider coordination.
Results
Descriptive statistics and central tendency were examined for each item, deleting those that were skewed and lacked variability (14 items deleted). Generally, planning and intervention items, which were not embedded within a vignette, lacked variability. For example, when staff was asked to indicate when discussions regarding preferences for resuscitation occurred, they overwhelmingly selected on admission, thus eliciting little variability. When this question was posed as part of an unfolding, resident case vignette, the same question elicited greater variability and staff selected other options such as “at the next care plan meeting” or “when the provider orders it.” Therefore, the items associated with the case vignette were retained for further testing.
Item-to-total correlations ranged from 0.40 to 0.90 for all but three items, which were revised for additional testing. Because the Knowledge construct contains dichotomous items, it was analyzed separately and the three subconstructs remained: psychological, physical, and end-of-life factors.
The initial testing of the Palliative Care Survey (PCS) provided encouraging results. Fifty-six items were retained for additional testing: 36 items for Palliative Care Practice (bereavement, 8 items; planning/intervention, 20 items; communication with family, 3 items; provider coordination, 5 items) and 20 items for Palliative Care Knowledge (psychological, 4 items; physical, 5 items; and end-of-life factors, 11 items).
Phase 2
Setting and Sample
Phase 2 was completed as part of a larger, ongoing study that is assessing the relationship of staff communication, teamwork, and palliative care practices to end-of-life outcomes for nursing home residents and their family members. 31 One hundred randomly selected nursing homes in two Midwestern states were recruited to participate. The parent study had a 39% refusal rate. From the initial sample of 100 nursing homes, 15 homes were removed from the parent study due to missing data. Thus, data from 85 nursing homes comprised the sample for Phase 2 and were used to psychometrically evaluate the Palliative Care Survey (PCS). To assess factorial validity, the resulting model from Phase 1 was evaluated using confirmatory factor analyses to fit the hypothesized model to the data in Phase 2.
Based on the authors’ preliminary studies, 4, 5, 18, 26 the following hypotheses were generated to evaluate construct validity: 1) nursing home staff communication and teamwork will be positively related to the survey subconstructs of Palliative Care Practice (bereavement, planning/intervention, family communication, and provider coordination); and 2) licensed staff (registered nurses, licensed practical nurses) will have higher scores on the Palliative Care Knowledge construct than unlicensed staff (certified nurse aides).
Procedures
Nursing home administrators were invited to participate and gave informed consent prior to approaching direct care staff for data collection. Staff were provided written and verbal information about the study and provided their agreement for participation. Research personnel gave an inservice presentation, unrelated to palliative care, as an incentive for nursing home and staff participation. Following the inservice, staff completed both the Palliative Care Survey (PCS) and Shortell’s Organization and Management Survey in 20 to 30 minutes.
Measures
Palliative Care Practice. Four subconstructs comprised the palliative care practice model: bereavement (8 items), planning/intervention (20 items), family communication (3 items), and provider coordination (5 items). Responses are rated on a 4-point Likert-type scale ranging from never to always. The planning/intervention items are summed to create four weighted scores for analysis procedures. Summation criteria were determined based on expert opinion and evidence-based practice in palliative care.
Palliative Care Knowledge. Three subconstructs comprised the palliative care knowledge model. They included factors that influence pain: psychological (4 items) and physical (5 items), and end-of-life factors (11 items). Items are dichotomous.
Communication and Teamwork. Staff communication and teamwork were measured using Shortell’s Organization and Management Survey. This survey has established reliability and validity in the hospital setting 32, 33 and has been adapted to reflect the language of the nursing home setting. 34, 35 Communication has five dimensions with a total of 18 items: openness (4 items), accuracy (4 items), timeliness (4 items), effectiveness (2 items) and understanding (4 items). Teamwork has three dimensions with a total of 12 items: cohesion (6 items), meeting effectiveness (2 items), and unit relations (4 items). Responses are rated on a 5-point Likert-type scale ranging from strongly disagree to strongly agree. On both measures, teamwork and communication, all items are summed and the mean score was used for analysis. In nursing homes, Cronbach’s alphas have ranged from 0.83 to 0.90. Construct validity has been supported by hypothesis testing with divergent groups. 34, 35
Data Analysis
Item statistics were generated to evaluate variability, central tendency, missing data, and distribution characteristics. Internal consistency reliability was examined using Cronbach’s alpha, evaluating the inter-item correlations (acceptable range = 0.30 - 0.70), corrected item-to-total correlation (≥ 0.30), and alpha-if-item deleted (increase of ≤ 0.01). Cronbach’s alphas were calculated using Tetrachoric correlations36 among the items for all constructs (α ≥ 0.70).37 Evidence for construct validity was evaluated using M-Plus software systems to conduct the confirmatory factor analysis (structural equation modeling) and for the hypothesis testing. For the confirmatory factor analysis, goodness-of-fit indices were generated including the comparative fit index (CFI) and the room mean square error of approximation (RMSEA). 38, 39 Desirable indices include a CFI greater than 0.90 or a RMSEA less than 0.08. 38 For construct validity, the first hypothesis was evaluated using Pearson’s correlation between Palliative Care Practice subconstructs with communication and teamwork as well as the second hypothesis using ANOVA of Palliative Care Knowledge across staff type.
Results
Of the 85 homes that comprised the sample, 52 were in rural locations and 33 were urban, while 45 were for-profit and 40 were not-for-profit. Nursing home bed size ranged from 60 to 193 (M = 89). Description of nursing home staff positions are presented in Table 2. Staff demographics are presented in Table 3.
Table 3.
Phase 2 Staff Demographics
| Frequency (%)a | ||
|---|---|---|
| Number of years employed at this nursing home |
Less than one year | 582 (21) |
| 1-5 years | 942 (34) | |
| 6-10 years | 377 (14) | |
| 11-15 years | 224 (8) | |
| 16-20 years | 146 (5) | |
| More than 20 | 226 (8) | |
| Missing | 282 (10) | |
| Education level | Less than high school | 92 (3) |
| High school or GED | 1378 (50) | |
| Associate’s degree | 839 (30) | |
| Bachelor’s degree | 308 (11) | |
| Masters degree | 69 (2) | |
| Missing | 93 (3) | |
| Ethnicity | African American | 75 (3) |
| Asian American | 40 (1) | |
| Multi-racial | 33 (1) | |
| Caucasian | 2175 (78) | |
| Hispanic American | 81 (3) | |
| Native American | 142 (5) | |
| Other | 149 (5) | |
| Missing | 84 (3) | |
| Gender | Male | 151 (5) |
| Female | 2430 (87) | |
| Missing | 198 (7) | |
| Age | Less and 24 years | 424 (15) |
| 25-34 years | 583 (21) | |
| 35-44 years | 518 (18) | |
| 45-54 years | 675 (24) | |
| 55 – 64 years | 408 ((15) | |
| 65 or greater | 121 (4.3) | |
| Missing | 50 (2) |
Note: percentage (%) based on all data including missing.
Missing data varied per demographic item.
Item Analysis. All items on the Palliative Care Practice subconstructs exhibited variability across all response options with item means ranging from 1.84 to 3.63 (range 1 to 4). For Palliative Care Knowledge all items exhibited variability with the mean proportion correct ranging from 0.27 to 0.99 (range 0.00 to 1.00).
Confirmatory Factor Analysis. Separate second order factor analytic modeling procedures were conducted for the hypothesized structures for the Palliative Care Practice (Fig. 1) and Palliative Care Knowledge (Fig. 2) constructs. The hypothesized (H) model for the Palliative Care Practice had adequate fit of the model to the data (Table 4). Upon review, however, five of the measured items did not load on their corresponding subconstruct; three items on bereavement, one item on family communication, and one item on provider coordination. With these five items removed the final model exhibited a better fit to the data (CFI = 0.94; RMSEA = 0.04). Thus a parsimonious Palliative Care Practice model contained 31 items. The correlations of the second order factor, Palliative Care Practice, with the four subconstructs were bereavement (r =0.68, P <0.001); planning and interventions (r =0.44, P <0.001); family communication (r =0.24, P <0.001); and provider coordination (r =0.70 P <0.001).
Table 4.
Fit Indices for the Measurement Models of Palliative Care Practice and Knowledge
| Fit Indices Measurement Model |
Χ 2 | df | Χ(0) 2 | df(0) | CFI |
RMSEA
(90% CI) |
|---|---|---|---|---|---|---|
| PCS (H) | 689.75 | 162 | 0.92 | 0.05 (0.04, 0.05) |
||
| PCS (F) | 338.31 | 86 | 4011.59 | 105 | 0.94 | 0.04 (0.04, 0.05) |
| Knowledge (H/F) | 240.63 | 88 | 10674.09 | 79 | 0.99 | 0.03 |
H = Hypothesized model; F = Final model; Χ2= Chi2 Model Fit; df=Degrees of Freedom Model Fit; Χ(0)2=Chi2 Baseline Model Fit; df(0) =Degrees of Freedom Baseline Model Fit
AU: SHOULD CHI2 BE CHI2?
The hypothesized model for Palliative Care Knowledge had excellent fit to the data (Table 4). One variable measured (feeding tubes prolong life) did not have a significant loading on the subconstruct, end-of-life factors. Because of the importance of this information in providing end-of-life care, a decision was made to retain this item in the model. The correlations of the three subconstructs with the second order Palliative Care Knowledge factor were psychological (r =0.84, P <0.001), physical (r =0.52, P <0.001), and end-of-life factors (r =0.60, P <.001).
Reliability. Following the final delineation of both the Palliative Care Practice and Knowledge constructs, Cronbach’s alpha were above the ≥ 0.70 for Palliative Care Practice (α = 0.75) and for Palliative Care Knowledge ( α = 0.81). Two of the four subconstructs for Palliative Care Practice met the minimum requirement with family communication, provider coordination, bereavement, and planning/intervention subconstructs having α = 0.77, 0.79, 0.62, 0.69; respectively. For the Palliative Care Knowledge construct, the Cronbach’s alphas for the three subconstructs were psychological (0.97), physical (0.90), and end-of-life factors (0.60). Removal of any of the items on the subconstructs did not improve alpha; thus, all items were retained.
Hypotheses Testing. For the first hypothesis, there were strong correlations between Palliative Care Practice and communication (r = 0.72, P < 0.001) and teamwork (r = 0.74, P < 0.001). There were weak to moderate correlations between communication and teamwork with bereavement (r = 0.51, P < 0.001 and 0.58, P < 0.001, respectively); with planning/intervention (r = 0.23, P < 0.001 and 0.26, P < 0.001, respectively); with family communication (r = 0.32, P < 0.001 and 0.35, P < 0.001, respectively), and with provider coordination (r = 0.48, P < 0.001 and 0.43, P < .001, respectively). Thus, the first hypothesis was supported, lending evidence of construct validity.
For the second hypothesis, there was a significant difference between licensed staff (RNs and LPNs) and unlicensed staff on the Palliative Care Knowledge [F(3) = 131.78, P < 0.001] and the three subconstructs: psychological [F(3) = 50.26, P < 0.001], physical [F(3) = 17.47, P < 0.001], and end-of-life factors [F(3) = 97.82, P < 0.001]. On Palliative Care Knowledge, RNs (M = 0.812) scored significantly (P < 0.001) higher than LPNs (M = 0.76) or CNA/CMAs (M = 0.64). Although the differences were not as large, the same pattern existed among the three levels of staff for the Palliative Care Knowledge. This support for the second hypothesis provided evidence of construct validity for the knowledge items.
Discussion
The 51-item Palliative Care Survey (PCS) made up of Palliative Care Practice and Knowledge measures the extent to which nursing home staff engage in palliative care practices and have knowledge consistent with good end-of-life care. Both practice and knowledge are an essential foundation to providing good end-of-life care to nursing home residents.
There is strong empirical and psychometric support for the PCS and evidence of adequate validity and reliability. It is psychometrically challenging to design items that capture what staff actually do as opposed to what they think they do or think they are supposed to do. For example, staff typically are aware of federal regulations requiring discussion of advance directives on admission, and they answered such direct questions accordingly. On the other hand, planning/intervention items based in vignettes that ask staff what typically is done in their nursing home elicit greater variability and less missing data than questions posed directly. In addition, response patterns from the vignette-based questions were more consistent with data from our qualitative studies. For example, both qualitative data and data from the PCS indicate that most discussions about dying are triggered by an event such as weight loss or hospitalization as opposed to ongoing planning initiated at admission or shortly thereafter. The PCS was developed to cover a range of practices and levels of knowledge of licensed and unlicensed nursing personnel. This study shows the PCS captured variation in the staff behavior and knowledge.
As empirical evidence emerges and standards for practice change, additional sub-scales may be added to the Palliative Care Survey. For example, although the PCS captures key aspects of end-of-life care, such as bereavement care, it does not assess staff members’ attention to the spiritual needs of residents or family. As practices develop to address additional aspects of palliative care, users of the PCS may wish to augment it with other appropriate measures of those concepts. Also, the PCS covers a range of practices and levels of knowledge of licensed and unlicensed staff. It is possible that separate versions tailored to the roles and desired knowledge levels of different levels of staff may be warranted in some investigations. Further, the PCS has been developed and evaluated in the Midwest. Additional testing across a wider geographic area is warranted.
Nursing homes are complex organizations with multiple interacting structures and processes that influence resident outcomes. Investigators have examined structural characteristics such as staffing levels or skill mix and related these to resident outcomes. 5 However, efforts to improve care and quality of life for residents would be incomplete without considering palliative care as an essential clinical process for all permanently placed residents. Many nursing homes in the United States struggle to provide even basic attention to palliative care at the end of life. 40 Given the rapid increase of dying in nursing homes in light of the aging population, there is urgent need for empirical research and sound psychometric measures of salient variables in the provision of palliative care. Efforts to improve care for the dying in nursing homes have been slowed by an absence of measurement tools for research; 1 a gap, which the Palliative Care Survey reported here, helps fill.
Acknowledgments
Disclosures and Acknowledgments This study was partially funded by NINR 5RO1NR009547.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
The authors declare no conflicts of interest.
References
- 1.Munn JC, Zimmerman S, Hanson LC, et al. Measuring the quality of dying in long-term care. J Am Geriatr Soc. 2007;55:1371–1379. doi: 10.1111/j.1532-5415.2007.01293.x. [DOI] [PubMed] [Google Scholar]
- 2.Teno JM. Brown Atlas of dying. [Accessed October 11, 2008]. Available at: http://www.chcr.brown.edu/dying/brownatlas.htm.
- 3.Brock DB, Foley DJ. Demography and epidemiology of dying in the U.S. with emphasis on deaths of older persons… A good dying: Shaping health care for the last months of life… the Corcoran symposium. Hosp J. 1998;13:49–60. doi: 10.1080/0742-969x.1998.11882887. [DOI] [PubMed] [Google Scholar]
- 4.Forbes S. This is heaven’s waiting room: End of life in one nursing home. J Gerontol Nurs. 2001;27:37–45. doi: 10.3928/0098-9134-20011101-10. [DOI] [PubMed] [Google Scholar]
- 5.Forbes-Thompson S, Gessert CE. End of life in nursing homes: connections between structure, process, and outcomes. J Palliat Med. 2005;8:545–555. doi: 10.1089/jpm.2005.8.545. [DOI] [PubMed] [Google Scholar]
- 6.Kayser-Jones J. The experience of dying: an ethnographic nursing home study. Gerontologist. 2002;42(Spec No 3):11–19. doi: 10.1093/geront/42.suppl_3.11. [DOI] [PubMed] [Google Scholar]
- 7.Kayser-Jones J, Schell E, Lyons W, et al. Factors that influence end-of-life care in nursing homes: The physical environment, inadequate staffing, and lack of supervision. Gerontologist. 2003;43(Spec No 2):76–84. doi: 10.1093/geront/43.suppl_2.76. [DOI] [PubMed] [Google Scholar]
- 8.Hanson LC, Eckert JK, Dobbs D, et al. Symptom experience of dying long-term care residents. J Am Geriatr Soc. 2008;56:91–98. doi: 10.1111/j.1532-5415.2007.01388.x. [DOI] [PubMed] [Google Scholar]
- 9.Hodgson NA, Lehning AJ. Palliative care in nursing homes: a comparison of high- and low-level providers. Int J Palliat Nurs. 2008;14:38–44. doi: 10.12968/ijpn.2008.14.1.28152. [DOI] [PubMed] [Google Scholar]
- 10.Johnson VM, Teno JM, Bourbonniere M, Mor V. Palliative care needs of cancer patients in U.S. nursing homes. J Palliat Med. 2005;8:273–279. doi: 10.1089/jpm.2005.8.273. [DOI] [PubMed] [Google Scholar]
- 11.Oliver DP, Porock D, Zweig S. End-of-life care in U.S. nursing homes: a review of the evidence. J Am Med Dir Assoc. 2004;5:147–155. doi: 10.1097/01.JAM.0000123063.79715.8E. [DOI] [PubMed] [Google Scholar]
- 12.Wunderlich GS, Kohler PO, editors. Improving the quality of long-term care. National Academies Press; Washington, DC: 2001. [PubMed] [Google Scholar]
- 13.Forbes-Thompson S, Gajewski B, Scott-Cawiezell J, Dunton N. An exploration of nursing home organizational processes. West J Nurs Res. 2006;28:935–954. doi: 10.1177/0193945906287053. [DOI] [PubMed] [Google Scholar]
- 14.Teno JM. TIME: Toolkit of instruments to measure end-of-life care. [Accessed January 15, 2009]. Available at: http://www.chcr.brown.edu/pcoc/toolkit.htm.
- 15.World Health Organization WHO definition of palliative care. [Accessed January 16, 2009]. Available at: http://www.who.int/cancer/palliative/definition/en/
- 16.National Consensus Project for Quality Palliative Care Clinical practice guidelines for quality palliative care. [Accessed March 10, 2010]. Available at: http://www.nationalconsensusproject.org.
- 17.Thompson S, Church L. The structure and process of advanced chronic illness and palliative care in nursing homes. In: Bern-Klug M, editor. Transforming palliative care in nursing homes: The social work role. Columbia University Press; New York: 2010. pp. 31–58. [Google Scholar]
- 18.Forbes-Thompson S, Gessert CE. Nursing homes and suffering: part of the problem or part of the solution? J Appl Gerontol. 2006;25:234–251. [Google Scholar]
- 19.Hanson LC, Ersek M. Meeting palliative care needs in post-acute care settings: “to help them live until they die”. JAMA. 2006;295:681–686. doi: 10.1001/jama.295.6.681. [DOI] [PubMed] [Google Scholar]
- 20.Levy C, Morris M, Kramer A. Improving end-of-life outcomes in nursing homes by targeting residents at high-risk of mortality for palliative care: program description and evaluation. J Palliat Med. 2008;11:217–225. doi: 10.1089/jpm.2007.0147. [DOI] [PubMed] [Google Scholar]
- 21.Strumpf NE, Tuch H, Stillman D, Parrish P, Morrison N. Implementing palliative care in the nursing home. Ann Longterm Care. 2004;12:35–41. [Google Scholar]
- 22.Stillman D, Strumpf N, Capezuti E, Tuch H. Staff perceptions concerning barriers and facilitators to end-of-life care in the nursing home. Geriatr Nurs. 2005;26:259–264. doi: 10.1016/j.gerinurse.2005.06.002. [DOI] [PubMed] [Google Scholar]
- 23.Stevenson DG, Bramson JS. Hospice care in the nursing home setting: a review of the literature. J Pain Symptom Manage. 2009;38:440–451. doi: 10.1016/j.jpainsymman.2009.05.006. [DOI] [PubMed] [Google Scholar]
- 24.Forbes S, Bern-Klug M, Gessert C. End-of-life decision making for nursing home residents with dementia. J Nurs Scholarsh. 2000;32:251–258. doi: 10.1111/j.1547-5069.2000.00251.x. [DOI] [PubMed] [Google Scholar]
- 25.Bern-Klug M, Gessert C, Forbes S. The need to revise assumptions about the end of life: Implications for social work practice. Health Soc Work. 2001;26:38–48. doi: 10.1093/hsw/26.1.38. [DOI] [PubMed] [Google Scholar]
- 26.Forbes-Thompson S, Leiker T, Bleich MR. High-performing and low-performing nursing homes: a view from complexity science. Health Care Manage Rev. 2007;32:341–351. doi: 10.1097/01.HMR.0000296789.39128.f6. [DOI] [PubMed] [Google Scholar]
- 27.Kiely DK, Volicer L, Teno J, et al. The validity and reliability of scales for the evaluation of end-of-life care in advanced dementia. Alzheimer Dis Assoc Disord. 2006;20:176–181. doi: 10.1097/00002093-200607000-00009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Thompson S, Parker-Oliver D. A new model for long-term care: balancing palliative and restorative care delivery. J Hous Elderly. 2008;22:1–26. [Google Scholar]
- 29.Irwin DE, Varni JW, Yeatts K, DeWalt DA. Cognitive interviewing methodology in the development of a pediatric item bank: a patient reported outcomes measurement information system (PROMIS) study. Health Qual Life Outcomes. 2009;7:3. doi: 10.1186/1477-7525-7-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Woolley ME, Bowen GL, Bowen NK. Cognitive pretesting and the developmental validity of child self-report instruments: theory and applications. Res Soc Work Pract. 2004;14:191–200. doi: 10.1177/1049731503257882. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Forbes-Thompson SA. 5RO1NR009547-04. National Institute of Nursing Research; 2006. The impact of quality end-of-life care in nursing homes. [Google Scholar]
- 32.Shortell SM, Rousseau DM, Gillies RR, Devers KJ, Simons TL. Organizational assessment in intensive care units (ICUs): construct development, reliability, and validity of the ICU nurse-physician questionnaire. Med Care. 1991;29:709–726. doi: 10.1097/00005650-199108000-00004. [DOI] [PubMed] [Google Scholar]
- 33.Shortell SM, Zimmerman JE, Rousseau DM, et al. The performance of intensive care units: Does good management make a difference? Med Care. 1994;32:508–525. doi: 10.1097/00005650-199405000-00009. [DOI] [PubMed] [Google Scholar]
- 34.Scott J, Vojir C, Jones K, Moore L. Assessing nursing homes’ capacity to create and sustain improvement. J Nurs Care Qual. 2005;20:36–42. doi: 10.1097/00001786-200501000-00007. [DOI] [PubMed] [Google Scholar]
- 35.Scott-Cawiezell J, Schenkman M, Moore L, et al. Exploring nursing home staff’s perceptions of communication and leadership to facilitate quality improvement. J Nurs Care Qual. 2004;19:242–252. doi: 10.1097/00001786-200407000-00011. [DOI] [PubMed] [Google Scholar]
- 36.Gajewski BJ, Boyle DK, Thompson S. How a Bayesian might estimate the distribution of Cronbach’s alpha form ordinal-dynamic scaled data: a case study measuring nursing home residents quality of life. Methodology (Gott) in press. [Google Scholar]
- 37.Nunnally JC. Psychometric theory. McGraw-Hill; New York: 1978. [Google Scholar]
- 38.Brown TA. Confirmatory factor analysis for applied research. The Guilford Press; New York: 2006. [Google Scholar]
- 39.Kline RB. Principles and practice of structural equation modeling. The Guilford Press; New York: 1998. [Google Scholar]
- 40.Miller SC, Han B. End-of-life care in U.S. nursing homes: nursing homes with special programs and trained staff for hospice or palliative/end-of-life care. J Palliat Med. 2008;11:866–877. doi: 10.1089/jpm.2007.0278. [DOI] [PubMed] [Google Scholar]