Abstract
A 15-year-old girl presented with a chief complaint of bleeding from her nose. She had noticed worms emerging from her right nostril. She had a continuous dull ache on the right side of her nose, spreading over the maxillary sinus area, and on the infra-orbital margin on the same side. She complained of difficulty breathing through her right nostril and a foul smell, which was associated with orbital oedema. Intra-oral examination revealed erythema of the soft palate on the same side, which was tender on palpation. Her condition was diagnosed as nasal myiasis with orbital and palatal extension. Nasal myiasis was treated by surgical removal of the maggots and with Ivermectin and local application of turpentine. The symptoms resolved and the dangers of orbital complications and penetration into the intracranial cavity were averted. The serious short-term complications of nasal myiasis were prevented by prompt treatment.
Background
Nasal myiasis is relatively rare in developed nations but is not uncommon in India as it is a tropical country. However, extension of nasal myiasis into the orbit and palate is relatively rare. Physicians in developed countries may be unfamiliar with this parasitic infection and thus misdiagnose it and initiate inappropriate treatment. Lesions can be mistaken for allergic rhinitis, cellulitis, insect bites, subcutaneous cysts or even malignancy. Treating physicians should be aware of this condition as early diagnosis with adequate and careful surgical exploration of the lesion forestall extensive tissue damage and morbidity.
Case presentation
A 15-year-old girl with low socioeconomic status presented with a 4-day history of continuous bleeding from the right nostril. The bleeding had started as drops. A constant dull aching pain was present on the right side of the nose, spreading over the maxillary sinus area, and on the infra-orbital margin on the same side. The patient had difficulty breathing through the right nostril and complained of a foul smell. A day after the discomfort had started she had felt movement within her nasal cavity and later noticed a few worms emerging from her right nostril on sneezing. Her medical history and the family history were non-contributory. General examination revealed that the patient was conscious and co-operative, with a normal IQ. Extra-oral examination revealed a diffuse swelling of middle third of the face on the right side (figure 1), bleeding from the right nostril and blood clots in both nostrils, partial closure of the right eyelid and slightly disturbed vision. The lateral aspects of the nose, maxillary sinus area and infra-orbital margin were tender on the right side. No lymphadenopathy was noted.
Figure 1.

Orbital oedema on the right side.
Intra-oral examination revealed diffuse erythema of the soft palate and the central area of the lesion appeared granular (figure 2). The area was tender on palpation. No other significant finding in the oral cavity was noted.
Figure 2.

Intra-oral palatal erythema.
A provisional diagnosis of nasal myiasis with orbital and palatal extension was made and the patient was hospitalised.
Investigations
The paranasal sinus view showed opacification of the right maxillary sinus (figure 3). Axial and coronal CT sections showed marked soft tissue thickening in the region of the soft palate, right nasal cavity and nasal septum, thinning of the soft tissue cartilaginous part of the nasal septum and erosion of the bony nasal septum, hard palate and intercellular septae of ethmoid air cells. The posterior nasopharyngeal space was partially obliterated due to marked soft palate swelling (figure 4 and 5). The maggots were reported to be Chrysomia bezziana by a zoologist at the Department of Parasitology, Indian Veterinary Research Institute, Izathnagar.
Figure 3.

CT scan showing haziness within the right maxillary sinus.
Figure 4.
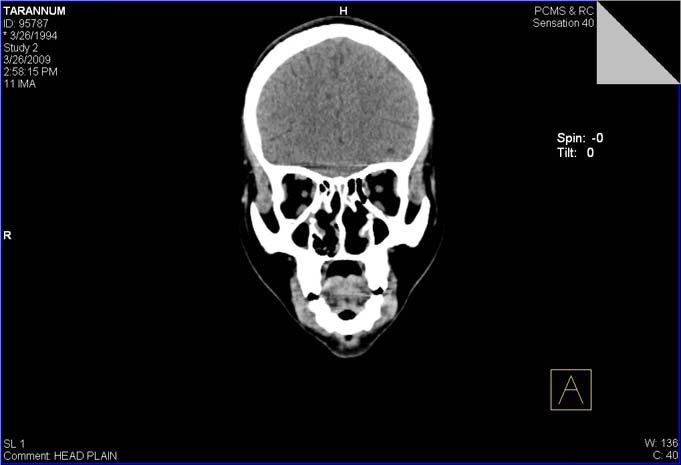
CT scan showing thickening of the soft palate, right nasal cavity and nasal septum with associated thinning of the cartilaginous part of the nasal septum.
Figure 5.

CT scan showing mild erosion of the bony nasal septum, hard palate and intercellular septae of ethmoid air cells.
Treatment
The patient was immediately hospitalised. Oral therapy of Ivermectin 6 mg daily was continued for 1 week. A cotton bud impregnated with turpentine was placed in the right nostril for approximately 10 min and 20 maggots were manually removed (figure 6). The same procedure was repeated for two more days. Surgical exploration of the site and local debridement was carried out after removal of all the maggots. Bleeding through the nose was controlled by the application of cotton buds. The patient was advised on personal hygiene and oral hygiene instructions were given.
Figure 6.

Removed maggots.
Outcome and follow-up
Ivermectin therapy and cotton buds with turpentine encouraged the maggots to emerge. Surgical exploration of the site and removal of maggots relieved the discomfort. Bleeding through the nose was controlled by the application of pressure with sterile cotton buds. Follow-up on further visit showed reduced swelling of the face, orbital cellulitis and erythema of the soft palate (figure 7 and 8).
Figure 7.

The postoperative appearance of the patient after 8 days, with no peri-orbital oedema.
Figure 8.

Postoperative reduced palatal erythema.
Discussion
Infestation of the nose can be extremely dangerous because of the possibility of penetration into the intracranial cavity. The maggots may spread laterally and posteriorly to the orbit and paranasal sinuses and in a few instances may spread inferiorly and perforate the palate.
Myiasis in the nose can cause orbital complications. There are specific areas of weakness in the lamina papyracea, and similarly the infra-orbital canal is a weak area in the orbital floor. Local spread due to associated thrombophlebitis, particularly through the diploic veins of the frontal bone, or from the sphenoid, can affect the bone itself and spread into adjacent cranial fossa. Significantly, the venous connections between sinuses and the orbit have no valves allowing free communication of infection.1
Myiasis affects individuals at any age but is more common in middle-aged and older patients; both sexes are equally affected.2 The larvae tunnel deep into soft tissue, separating the epithelium and mucoperiosteum from bone and obtaining their nutrition from surrounding tissues.
The larvae are more readily visible in wounds. A definitive diagnosis of the exact species of fly responsible cannot be made on the basis of the fly's larval stage. Larvae obtained from a patient must be reared on meat or a synthetic medium until they pupate and eventually emerge as adult flies.
Myiasis is usually initiated when flies are attracted by a wound and lay their eggs in necrotic, haemorrhagic or pus-filled lesions.3 Secondary bacterial infections are common. All conditions compromising bodily integrity predispose to infestation.4
The parasites are quite mobile and their clinical signs and symptoms always appear suddenly. The main symptoms are a foreign-body sensation and itching in the throat, followed by cough and other respiratory and nasal manifestations such as nasal discharge, sneezing, laryngospasm, dyspnoea and stridor.5 The patient in the present case showed most of the clinical signs and symptoms.
The larvae release toxins to destroy the host tissue.6 The continuous nasal bleeding and intense halitosis seen in the present case are suggestive of the destruction caused by toxins released by the larvae. Progressive destruction and cavitations occur as the larvae grow in body tissue. The host also responds by creating a fibrous capsule to which the larvae can become tightly attached.7
When multiple maggots are detected, as in the present case, turpentine is used as it irritates and forces them out of hiding. Treatment consists of manual removal of maggots, broad-spectrum antibiotics and oral therapy with Ivermectin, a semi-synthetic macrolide antibiotic.8
A review of the literature yielded very few publications on this particular presentation of nasal myiasis, which to our knowledge is the first with orbital and palatal complications.
Manfrim et al reported the case of a 70-year-old woman with nasal obstruction, nose itching and nasal/palatal myiasis after she had undergone an operation for basal cell carcinoma of the nasolabial fold.9
Bapna et al described the case of 49-year-old man with worms emerging from his nostril, with maxillary sinusitis and sphenoiditis on the same side.10
Uriarte and Ell reported the case of a 64-year-old man who felt a sudden sensation in his nose leading to mild dyspnoea; two maggots were removed from his nose.11
Eyigör et al described a 33-year-old man who complained of a pronounced foreign body sensation, discharge from his nose, cough and a foreign body sensation in his right eye, which all occurred immediately after contact with sheep. He was diagnosed with and treated for naso-ophthalmic myiasis.2
Learning points.
-
▶
Nasal myiasis should be considered in the differential diagnosis of conditions exhibiting orbital and palatal erythema.
-
▶
Myiasis is diagnosed by observing the larvae as they periodically surface in the central punctum of the lesion.
-
▶
Rapid extension into surrounding tissues may occur and can cause tissue destruction and morbidity.
-
▶
Once the condition is diagnosed, immediate treatment with anthelmintic drugs and application of turpentine should be undertaken and followed by surgical debridement and follow-up.
Footnotes
Competing interests None.
Patient consent Obtained.
References
- 1.Lund VJ. The complications of sinusitis. Chapter 13. In: Kerr AG, Mackay IS, Bull TR, eds. Scott-Brown's Otolaryngology. Sixth edition Vol 4. Rhinology Mumbai, Maharashtra, India: KM Varghese Company; 1997:4/13/1 [Google Scholar]
- 2.Eyigör H, Dost T, Dayanir V, et al. A case of naso-ophthalmic myiasis. Kulak Burun Bogaz Ihtis Derg 2008;18:371–3 [PubMed] [Google Scholar]
- 3.Peters W. Infectious Diseases. First edition Philadelphia, PA, USA: Churchill Livingstone Elsevier; 1999:14.1–6 [Google Scholar]
- 4.Mallon PW, Evans M, Hall M, et al. “Something moving in my head”. Lancet 1999;354:1260. [DOI] [PubMed] [Google Scholar]
- 5.Aydin E, Uysal S, Akkuzu B, et al. Nasal myiasis by fruit fly larvae: a case report. Eur Arch Otorhinolaryngol 2006;263:1142–3 [DOI] [PubMed] [Google Scholar]
- 6.Sood VP, Kakar PK, Wattal BL. Myiasis in otorhinolaryngology with entomological aspects. J Laryngol Otol 1976;90:393–9 [DOI] [PubMed] [Google Scholar]
- 7.Tamizi M, Najafi MH, Sargolzaei N. Gingival Myiasis a case report. J Dent 2008;5:42–5 [Google Scholar]
- 8.Abdo EN, Sette-Dias AC, Comunian CR, et al. Oral myiasis: a case report. Med Oral Patol Oral Cir Bucal 2006;11:E130–1 [PubMed] [Google Scholar]
- 9.Manfrim AM, Cury A, Demeneghi P, et al. Nasal myiasis: case report and literature review. Arq Int Otorrinolaringol 2007;11:1–7 [Google Scholar]
- 10.Bapna S, Kothari S, Raju S, et al. A rare case of human nasal myiasis due to the larvae of Oestrus Ovis. J Parasit Dis 2006;30:184–6 [Google Scholar]
- 11.Uriarte FJ, Ell SR. Doctor, there are maggots in my nose. J R Soc Med 1997;90:634–5 [DOI] [PMC free article] [PubMed] [Google Scholar]


