Abstract
The case of a 58-year-old man with a large midthoracic oesophageal diverticulum and a left diaphragmatic relaxation who presented with night regurgitations, abdominal bloating, epigastric burning and a sensation of fullness after meals is reported. The patient underwent a successful thoracotomic diverticulectomy with left diaphragmatic plicature. The postoperative course was uneventful. To our knowledge this is the first reported case of an association between midthoracic oesophageal diverticulum and left diaphragmatic relaxation. Moreover, we hypothesised that the diverticulum was caused by a pulsion mechanism due to obstruction of the distal oesophagus secondary to diaphragmatic relaxation.
Background
Midthoracic diverticulum is a rare disease (15% of all oesophageal diverticula), most commonly secondary to tracheobronchial lymph nodes affected by inflammatory processes. A midthoracic diverticulum is usually a traction diverticulum, produced by continued peristalsis of the oesophagus against a fixed oesophageal adhesion. The majority of these diverticula are the result of oesophageal motility disorders, due to a lack of coordination between the distal oesophagus and lower oesophageal sphincter (LES).1 The symptoms of midthoracic oesophageal diverticulum vary widely, ranging from primary symptoms, such as dysphagia and regurgitation, to oesophagitis, bleeding and chest pain.2 3 Many patients with small diverticula are asymptomatic, and therefore surgical management is usually reserved for patients with larger symptomatic diverticula.4 In most published series, oesophageal diverticulectomy has been performed via thoracotomic or thoracoscopic approaches.5
Diaphragmatic relaxation is a pathology rarely observed because it generally has few symptoms. Its causes include trauma, neuromuscular disorders, iatrogenic disease (especially cardiac or mediastinal surgery), cervical spondylosis and infection.6 7 We report the first case of an association between midthoracic oesophageal diverticulum and diaphragmatic relaxation, probably due to abnormal rise of the emidiaphragm.
Case presentation
A 58-year-old man was referred to our institute in November 2007, with severe night regurgitations, abdominal bloating, epigastric burning and a sensation of fullness after meals.
Investigations
Oesophagogastroduodenoscopy and oesophageal barium radiography showed a giant midthoracic oesophageal diverticulum and chest x-ray showed left diaphragmatic relaxation.
A spiral CT confirmed a giant diverticulum in the right side of the middle third of the oesophagus. The diverticulum pulled up the gastro-oesophageal junction but was not associated with hiatus hernia. The CT also showed an important left diaphragmatic rise (figure 1A,B).
Figure 1.
Spiral CT scan. (A) Transverse scan. (B) Coronal scan showing in the right side of the middle third of the oesophagus, a giant diverticulum pulling up the gastro-oesophageal junction and an important left diaphragmatic rise.
Surprisingly, oesophageal manometry showed normal pressure of the LES.
Treatment
The patient (figure 2) underwent a left posterolateral thoracotomy. After division of the triangular ligament, the oesophagus was mobilised (figure 2A) and a giant midthoracic diverticulum was found strictly adherent to the superior vena cava, aorta and right mediastinic pleura. The diverticulum was mobilised from adjacent tissues and the point of origin from the oesophageal muscle was identified. After mobilisation of the neck of the diverticulum, it was excised using a TA55 roticulator (figure 2B). The oesophageal muscle layers over the stump of the diverticular neck were approximated using 3-0 polydioxanone interrupted sutures (figure 2C). Finally, a diaphragmatic plicature using an interrupted non-absorbable suture was performed (figure 2D).
Figure 2.
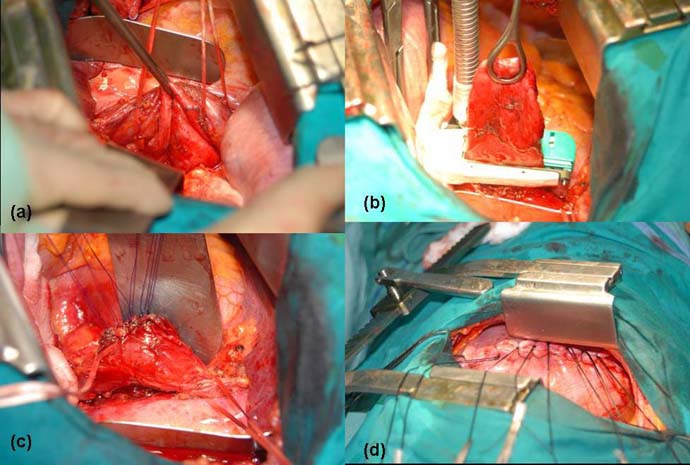
Photographs of the operation. (A) The oesophagus mobilised from adjacent structures. (B) The diverticulum being excised. (C) Oesophageal muscle layers being approximated using 3-0 polydioxanone interrupted sutures. (D) The diaphragmatic plicature.
Outcome and follow-up
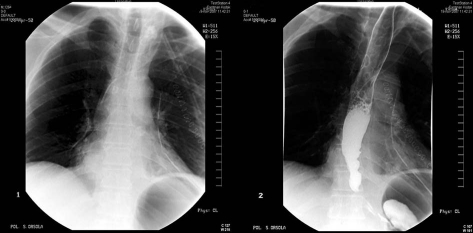
There were no intraoperative complications and the postoperative course was uneventful. A gastrographin swallow did not show any sign of leakage, and chest x-ray showed the left side of the diaphragm had returned to its normal site (figure 3A,B). The patient was discharged in the 11th postoperative day; after 1 year the patient is asymptomatic and has gained 5 kg in weight.
Figure 3.
(A) Postoperative chest x-ray showing a normal diaphragmatic profile. (B) An oesophageal radiograph with water-soluble contrast medium (CM) showing a normal oesophagus after diverticulectomy.
Discussion
Midthoracic oesophageal diverticula represent 15% of all oesophageal diverticula. Most previous studies highlight the importance of a traction mechanism in the pathogenesis of oesophageal diverticula, especially in the middle third of the oesophagus because of its proximity to the tracheobronchial lymph nodes affected by inflammatory processes. The aetiology of diverticula has been clarified recently, and the association between midthoracic oesophageal diverticula and motor disorders, secondary to increased intraluminal pressure, has been stressed.
In the present case we hypothesise that the oesophageal diverticulum was related to relaxation of the diaphragm. The rise of the left hemidiaphragm would cause lack of space and consequently increased pressure in the left hemithorax. This would create a siphon-shaped angle at the gastro-oeosphageal junction, causing an increase in intraluminal oesophageal pressure. The subsequent disturbance in the movement of the oesophagus would induce the oesophageal diverticulum through a pulsion mechanism, on the right side because the left hemidiaphragm is affected. Due to the pathogenesis of the diverticulum, we did not perform anti-reflux surgery. We chose a left thoracotomic approach, even though the diverticulum was on the right side of the oesophagus, because we also had to perform the left diaphragmatic plicature.
This report demonstrates an association between left diaphragmatic relaxation and a midthoracic oesophageal diverticulum, not previously described in the literature, due not to specific motor disorders but to obstruction of the distal oesophagus as a result of diaphragmatic relaxation causing a siphon-shaped angle at the gastro-oesophageal junction. The particular ethiopathogenesis with a pulsion mechanism in this case shows that the relaxation is the main cause of this condition.
Plication is a valuable treatment for unilateral diaphragmatic paralysis, which improves patients’ dyspnoea and work ability. Because of the risk of aspiration and potential life-threatening pulmonary complications in some patients, surgery should be undertaken in all patients with thoracic oesophageal diverticula regardless of the presence or absence of symptoms. We did not perform a fundoplication or a myotomy but rather treated the diaphragmatic relaxation with plication because the relaxation was the first cause of the diverticulum and accompanying symptoms.
Learning points.
-
▶
Some midthoracic oesophageal diverticula are congenital in origin, others are caused by traction from contiguous mediastinal inflammation and adenopathy, while others, as in our case, have a different aetiology.
-
▶
Aspiration pneumonia may accompany large symptomatic diverticula, so surgery should be undertaken in all patients with thoracic oesophageal diverticula regardless of the presence or absence of symptoms.
-
▶
Surgical options usually include diverticulectomy with myotomy.
-
▶
In our case we did not perform a fundoplication or a myotomy but instead treated the diaphragmatic relaxation with plication because it was the first cause of the diverticulum and accompanying symptoms.
Footnotes
Competing interests None.
Patient consent Obtained.
References
- 1.Orringer MB. Epiphrenic diverticula: facts and fable. Ann Thorac Surg 1993;55:1109–13 [DOI] [PubMed] [Google Scholar]
- 2.Debas HT, Payne WS, Cameron AJ, et al. Physiopathology of lower esophageal diverticulum and its implications for treatment. Surg Gynecol Obstet 1980;151:593–600 [PubMed] [Google Scholar]
- 3.Benacci JC, Deschamps C, Trastek VF, et al. Epiphrenic diverticulum: results of surgical treatment. Ann Thorac Surg 1993;55:1109–13 [DOI] [PubMed] [Google Scholar]
- 4.Varghese TK, Jr, Marshall B, Chang AC, et al. Surgical treatment of epiphrenic diverticula: a 30-year experience. Ann Thorac Surg 2007;84:1801–9 [DOI] [PubMed] [Google Scholar]
- 5.Rosati R, Fumagalli U, Bona S, et al. Diverticulectomy, myotomy and fundoplication through laparoscopy: a new optino to treat epiphrenic diverticela? Ann Surg 1998;227:174–8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Higgs SM, Hussain A, Jackson M, et al. Long term results of diaphragmatic plication for unilateral diaphragm paralysis. Eur J Cardiothorac Surg 2002;21:294–7 [DOI] [PubMed] [Google Scholar]
- 7.Altorki NK, Sunagawa M, Skinner DB. Thoracic esophageal diverticula. Why is operation necessary? J Thorac Cardiovasc Surg 1993;105:260–4 [PubMed] [Google Scholar]