Abstract
A 65-year-old woman from a rural area presented to the surgical service with a very large abdominal lump that the patient had first noticed 8 years previously. The lump had steadily increased in size over time, and the patient had dysuria, weakness and dyspnoea on exertion. On examination she was grossly anaemic with a large retroperitoneal lump that occupied the whole right side of abdomen; the lump was soft to firm in consistency and non-tender. She had no lymphoedema or other palpable lymph nodes. Ultrasound revealed a large retroperitoneal tumour with fatty elements, arising from the right kidney. There was no involvement of the intestines. Findings of the computed tomography scan were typical for renal angiomyolipoma. The patient underwent surgery and the tumour was excised. Four units of blood were transfused preoperatively and in addition two units were given postoperatively. The patient was given thromboprophylaxis perioperatively and in the postoperative period because she was bedridden and could not ambulate. She made an uneventful recovery.
Background
Angiomyolipoma (AML) is an uncommon soft tissue tumour involving the kidney, liver and other visceral organs. It is composed of smooth muscle cells, adipocytes and small to medium sized hyalinised vessels. Clinically renal and hepatic AML are usually associated with tuberous sclerosis complex and are more common in females. The tumour is diagnosed by ultrasound, computed tomography (CT) scan, magnetic resonance imaging (MRI), histology, and immunohistochemistry
A case of benign giant renal AML is presented here because of its uncommon occurrence. Presentation of the tumour, the diagnostic modalities employed, and its treatment are discussed
Case presentation
A 65-year-old woman presented with a very large lump in abdomen. She noticed the lump 8 years previously, but did not consult a physician as it did not cause her any problems. For the last 3 years it had started gradually increasing in size and occupied nearly the whole of the abdomen. Of late she had felt general weakness, breathlessness on exertion, and dysuria.
On examination the patient was severely anaemic and had a huge abdominal lump occupying the right side of her abdomen, crossing the midline and extending to most of the left side. The lump was soft to firm, and non-tender. There were no significant lymph nodes.
Investigations
Haemoglobin: 6 g/dl (microcytic hypochromic anaemia)
Chest x-ray: did not reveal any secondary spread and was unremarkable
Ultrasound: right renal tumour, abundant fatty element, no involvement of intestines
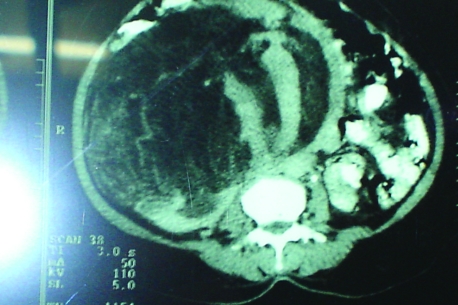
CT scan: suggestive of renal AML (fig 1).
Figure 1.
Computed tomography scan suggesting renal angiomyolipoma.
Differential diagnosis
Renal AML has to be differentiated from liposarcoma; in addition, renal epithelioid AML closely mimics renal cell carcinoma.
Differentiated by:
Fine needle aspiration cytology (FNAC)—CT/ultrasound guided
Histopathology
Immunohistochemistry
HMB-45 immunoreactivity.
Treatment
Excision done through a transperitoneal midline incision. The tumour, which occupied most of the abdomen, was highly vascular. All feeders to the tumour and also the draining veins were controlled.
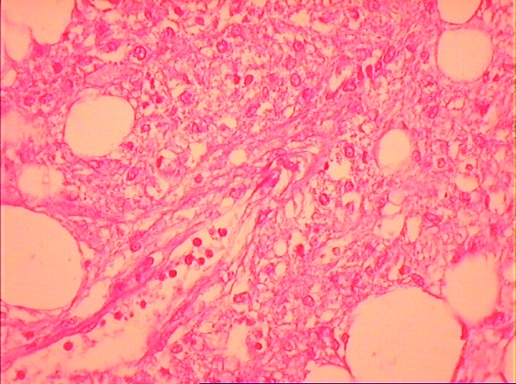
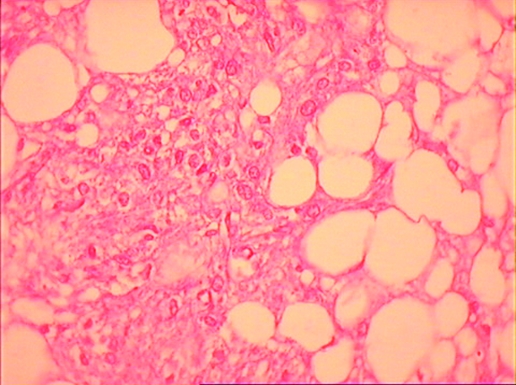
The tumour was excised intact. Its weight was 1350 g (fig 2). A nephrectomy was done due to the inability to differentiate it from renal cell carcinoma, and the non-availability of intraoperative frozen section reporting. Histology of the excised tumour showed mature adipocytes, smooth muscles and blood vessels (figs 3 and 4). There was no evidence of malignant change.
Figure 2.
Specimen showing renal angiomyolipoma.
Figure 3.
Histopathology: angiomyolipoma 1.
Figure 4.
Histopathology: angiomyolipoma 2.
Outcome and follow-up
Two closed tube drains—one in the right renal area and another in the pelvis—were used
Two units of red blood cells (packed cells) were transfused
Thromboprophylaxis (enoxaparin 4 ml) was given perioperatively and for 5 days postoperatively as the patient was bedridden and could not ambulate
Chest physiotherapy was started from the second postoperative day
The patient tolerated oral feeds from the fourth day. Stitches were removed on the 10th postoperative day and the patient was discharged from hospital in stable condition.
The patient has been free of symptoms for the last 21 months.
Discussion
Renal AML is an uncommon tumour, benign in nature and sometimes associated with tuberous sclerosis complex. Due to the benign nature of the tumour it can be managed with surveillance alone. Treatment is required once it becomes symptomatic. Presently there are various treatment options in the management of symptomatic renal AML. These include selective arterial embolisation, nephron sparing surgery, cryoablation of the tumour, and radiofrequency ablation of the tumour; however, few cases require nephrectomy, and few malignant cases have been reported. The decision to operate depends on the symptoms caused to the patient due to its size.1 In a study of 46 cases of AML, 35 were followed up; one died of malignant spread of AML.2 In a case of malignant epithelioid AML of the kidney, the patient had liver metastasis that responded to doxorubicin.3 A case of retroperitoneal extra-renal AML (positive for HMB 45 and smooth muscle actin) was reported that resembled liposarcoma.4 AML of epithelioid subtype with tumour necrosis may suggest malignant change.5 Long believed to be a hamartoma, AML is now considered a neoplasm that arises from the perivascular epithelioid cells.6
Typical AML can be diagnosed by ultrasound and CT in up to 95% of cases.7 On FNAC it can be erroneously diagnosed as renal cell carcinoma or sarcoma. An extensive sampling and HMB 45 and CD-68 positivity combined with cytokeratin negativity are of paramount importance for correct diagnosis.8,9 Bilateral AML should not be treated unless it has life threatening problems.10 In case of renal rupture if the radiological diagnosis is ambiguous, renal exposure is indicated both from a diagnostic and therapeutic standpoint.11 Renal AML may be associated with pulmonary lymphangiomyomatosis.12 Two cases of tuberous sclerosis complex with giant AML were managed conservatively for more than 20 years.13
Presently in the management of renal AML selective artery embolisation has been successfully done and reported by various authors14–20; however, recently in a retrospective study of 102 cases of renal AML, Sooriakumaran et al30 found it to be effective in controlling haemorrhage in the acute setting but encountered complications. Nephron sparing surgery is an acceptable alternate to selective arterial embolisation and has been done by various authors.19–28 Laparoscopic cryoablation has also been reported as minimal invasive procedure to treat renal AML29
Learning points
Renal angiomyolipoma (AML) is an uncommon soft tissue tumour which is mostly benign in nature, and occurs more commonly in females. Mostly these tumours can managed with surveillance only.
Patients present because of the tumour size and in some cases because of the symptoms associated with the intra-tumoral haemorrhage.
Typical AML can be diagnosed by a combination of ultrasound and CT scan in 95% cases; HMB 45 reactivity is positive in all cases.
Symptomatic cases require treatment in the form of selective arterial embolisation, nephron sparing surgery, or cryoablation of the tumour.
Nephrectomy has a limited but important role in acute/semi-elective settings for haemorrhage associated with AML, where selective arterial embolisation has failed, and also where there is uncertainty as to the benign nature of the tumour.
Footnotes
Competing interests: none.
Patient consent: Patient/guardian consent was obtained for publication
REFERENCES
- 1.De la Cruz Ruiz M, Rivero Martinez MD, Fernandez Dominguez L, et al. Giant renal angiomyolipoma. Arch Esp Urol 1999; 52: 381–5 [PubMed] [Google Scholar]
- 2.L’Hostis H, Deminiere C, Ferriere JM, et al. Renal angiomyolipoma: a clinicopathologic, immunohistochemical, and follow-up study of 46 cases. Am J Pathol 1999; 23: 1011–20 [DOI] [PubMed] [Google Scholar]
- 3.Cibas ES, Goss GA, Kulke MH, et al. Malignant epithelioid angiomyolipoma (‘sarcoma ex angiomyolipoma’) of the kidney: a case report and review of the literature. Am J Pathol 2001; 25: 121–6 [DOI] [PubMed] [Google Scholar]
- 4.Cavazza A, Giunta A, Pedrazzoli C, et al. Extra renal retroperitoneal angiomyolipoma: description of a case and review of the literature. Pathologica 2001; 93: 44–9 [PubMed] [Google Scholar]
- 5.Lin WC, Wang JH, Wei CJ, et al. Malignant renal epithelioid angiomyolipoma with aggressive behaviour and distant metastasis. J Chin Medical Assoc 2003; 66: 303. [PubMed] [Google Scholar]
- 6.Leclere JC, Marchal F, Stines J, et al. Epithelioid renal angiomyolipoma: benign or malignant tumour? J Radiol 2003; 84: 851–4 [PubMed] [Google Scholar]
- 7.Lin WY, Chuang CK, Ng KF, et al. Renal angiomyolipoma with lymph node involvement: a case report and literature. Review Chang Gung Med J 2003; 26: 607–10 [PubMed] [Google Scholar]
- 8.Svec A, Velenska Z. Renal epithelioid angiomyolipoma – a close mimic of renal cell carcinoma. Report of A case and review of the literature. Pathol Res Pract 2005; 200: 851–6 [DOI] [PubMed] [Google Scholar]
- 9.Kulkarni B, Desai SB, Dave B, et al. Renal angiomyolipomas – a study of 18 cases. Indian J Pathol Microbiol 2005; 48: 459–63 [PubMed] [Google Scholar]
- 10.Mantas D, Papachristodoulou A. Bilateral renal angiomyolipoma. Acta Chir Belg 2006; 106: 707–9 [DOI] [PubMed] [Google Scholar]
- 11.Kosciesza S, Mohring C, Kirchner J, et al. Spontaneous renal angiomyolipoma rupture. Rare differential diagnosis of renal ruptures. Urologe A 2007; 46: 92. [DOI] [PubMed] [Google Scholar]
- 12.Nimi A, Kume H, Kumano S, et al. Giant renal angiomyolipoma in a case with pulmonary lymphangiomyomatosis. Nippon Hinyokika Gakkai Zasshi 2007; 98: 713–7 [DOI] [PubMed] [Google Scholar]
- 13.Danforth TL, Lane BR, Novick AC. Conservative management of giant symptomatic angiomyolipomas in patients with the tuberous sclerosis complex. BJU Int 2007; 100: 794–7 [DOI] [PubMed] [Google Scholar]
- 14.Kothary N, Soulen MC, Clark TW, et al. Renal angiomyolipoma: long- term results after arterial embolization. J Vasc Interv Radiol 2005; 16: 45–50 [DOI] [PubMed] [Google Scholar]
- 15.Vallejo BJ, Herrera TE, Domenech CA, et al. Renal angiomyolipoma: presentation, treatment and results of 20 cases. Actas Urol Esp 2008; 32: 307–15 [DOI] [PubMed] [Google Scholar]
- 16.Hadley DA, Bryant LJ, Ruckle HC. Conservative treatment of renal angiomyolipomas in patients with tuberous sclerosis. Clin Nephrol 2006; 65: 22–7 [DOI] [PubMed] [Google Scholar]
- 17.Seyam RM, Bissada NK, Kattan SA, et al. Changing trends in presentation, diagnosis and management of renal anagiomyolipoma: comparison of sporadic and tuberous sclerosis complex-associated forms. Urology 2008; 72: 1077–82 [DOI] [PubMed] [Google Scholar]
- 18.Ramon J, Rimon U, Garniek A, et al. Renal angiomyolipoma: long term results following selective arterial embolization. Eur Urol 2008 Apr 23. (Epub ahead of print). [DOI] [PubMed] [Google Scholar]
- 19.Khaitan A, Hemal AK, Seth A, et al. Management of renal angiomyolipoma in complex clinical situations. Urol Int 2001; 67: 28–33 [DOI] [PubMed] [Google Scholar]
- 20.Tsai HN, Chou YH, Shen JT, et al. The management strategy of renal angiomyolipoma. Kaohsiung J Med Sci. 2002; 18: 340–6 [PubMed] [Google Scholar]
- 21.Mullerad M, Hidas G, Kastin A, et al. Nephron sparing surgery as a treatment modality for renal angiomyolipoma. Harefuah 2005; 144: 619–21, 678, 677 [PubMed] [Google Scholar]
- 22.Fazeli-Matin S, Novick AC. Nephron-sparing surgery for renal angiomyolipoma. Urology 1998; 52: 577–83 [DOI] [PubMed] [Google Scholar]
- 23.Heidenreich A, Hegele A, Varga Z, et al. Nephron sparing surgery for renal angiomyolipoma. Eur Urol 2002; 41: 267–73 [DOI] [PubMed] [Google Scholar]
- 24.Chen SS, Lin AT, Chen KK, et al. Renal angiomyolipoma – experience of 20 years in Taiwan. Eur Urol 1997; 32: 175–8 [PubMed] [Google Scholar]
- 25.Boorjian SA, Frank I, Inman B, et al. The role of partial nephrectomy for the management of sporadic renal angiomyolipoma. Urology 2007; 70: 1064–8 [DOI] [PubMed] [Google Scholar]
- 26.Yip SK, Tan PH, Cheng WS, et al. Surgical management of angiomyolipoma: nephron –sparing surgery for symptomatic tomour. Scand J Urol Nephrol 2000; 34: 32–5 [DOI] [PubMed] [Google Scholar]
- 27.Hsu TH, O’Hara J, Mehta A, et al. Nephron- sparing nephrectomy for giant renal angiomyolipoma associated with lymphangioleiomyomatosis. Urology 2002; 59: 138. [DOI] [PubMed] [Google Scholar]
- 28.Minervini A, Giubilei G, Masieri L, et al. Simple enucleation for the treatment of renal angiomyolipoma. BJU Int 2007; 99: 887–91 [DOI] [PubMed] [Google Scholar]
- 29.Byrd GF, Lawatsch EJ, Mesrobian HG, et al. Laparoscopic cryoablation of renal angiomyolipoma. J Urol 2006; 176: 1512–6; discussion 1516 [DOI] [PubMed] [Google Scholar]
- 30.Sooriakumaran P, Gibbs P, Coghlin G, et al. Angiomyolipomata: challenges, solutions and future prospects based on over 100 cases treated. BJU Int 2009 Jun 2. (Epub ahead of print). [DOI] [PubMed] [Google Scholar]