Abstract
We present a case of optic neuritis and myelo-radiculopathy as a late association following Chlamydia psittaci infection. A 45-year-old female patient with a prior history of C psittaci pneumonia and subsequent reactive arthritis presented to the neurology unit with severe headache, constitutional symptoms and monocular disturbance in vision. Clinical examination revealed focal signs with brisk upper limb reflexes compared to lower limbs and mild left-sided pyramidal signs. Systemic inflammatory markers were raised and serological studies showed no evidence of re-infection. MRI showed multiple high signal foci within the brain parenchyma and pachymeningeal thickening and enhancement. There was marked clinical and haematological improvement with high dose corticosteroids.
Background
We report a case of a delayed neurological syndrome in association with prior Chlamydia psittaci infection in a patient with a definite but remote history of C psittaci pneumonia and subsequent reactive arthritis. Other causes of myelo-radiculopathy with meningoencephalopathy and optic neuritis were excluded and the patient was effectively treated with immunosuppression. The case additionally demonstrates the relevance of previous infective history and the potential para-immune complications that may result.
Case presentation
A 45-year-old woman presented to our neurology unit via her general practitioner in January 2009. She complained of an 8-day history of a severe bi-frontal and occipital headache. She described it as constant with occasional sharp jabs of pain. The onset was associated with constitutional symptoms of generalised malaise and arthralgia affecting all her joints including her neck, shoulders and jaw. She went on to develop night sweats even though within 4 days the arthralgia had settled spontaneously. Four days into her illness she woke with impaired vision in her right eye. She reported a greying of her central vision with ‘washing out’ of colours. She denied ocular or orbital pain, and reported no jaw claudication or scalp tenderness. Due to the persistent nature of the headache and the appearance of visual symptoms she attended her general practitioner 7 days into her illness and was started on oral steroids as there was concern regarding the possibility of temporal arteritis. She reported rapid improvement in her headache 24 h after starting steroids although the visual symptoms persisted.
She reported a previous medical history of C psittaci pneumonia diagnosed in 2003 with other known contacts from the same source, pneumonic chest x-ray changes and a fourfold elevation in C psittaci titres. She was treated at the time with two courses of antibiotics over a period of 4 months as she failed to respond after the first. Two years following this she developed an inflammatory arthritis that was suspected to represent a post infectious reactive arthopathy and demonstrated a negative autoimmune screen including rheumatoid factor at that time. She was treated with oral steroids and sulphasalazine for 18 months before complete resolution of symptoms. There was a family history of rheumatoid arthritis from her mother and her daughter had Crohn's disease.
General physical examination was unremarkable with normal respiratory examination and normal cardiovascular examination. She was apyrexial. Visual acuity in the right eye (OD) was 6/12, not corrected with pin-hole examination, and in the left eye (OS) 6/6. Visual fields were preserved but she reported red colour desaturation. There was a mild right afferent pupillary defect. Fundoscopy was normal. The remainder of the cranial nerve examination was normal. There was a mild spastic increase in tone in the left upper limb and both lower limbs, with some accentuation to the left. Reflexes were brisk in both upper limbs but relatively suppressed in the lower limbs. There was no evidence of sensory impairment.
Investigations
Investigations revealed markers of systemic illness with an elevated erythrocyte sedimentation rate (ESR) of 122 and a C reactive protein of 208 (figure 1). Urea and electrolytes, liver function, bone profile and serum B12 and folate were all normal. Full blood count revealed a lymphopaenia of 0.5×109/l. Extensive immunological testing revealed negative antibodies for antinuclear antibodies, antineutrophil cytoplasmic antibodies, RhF and cryoglobulins. Complement levels were mildly elevated in keeping with systemic response. Serum and cerebrospinal fluid (CSF) angiotensin converting enzyme was normal. Lumbar puncture was performed revealing a normal white cell count of 1 and an elevated CSF protein of 0.58 g/dl. CSF glucose was normal but plasma glucose was elevated at 8.8 mmol. Oligoclonal bands were not detected in the CSF. Other serological investigations including HIV, treponema and borrelia were normal. Serum was sent for atypical pneumonia screen and there was no elevation in titres.
Figure 1.
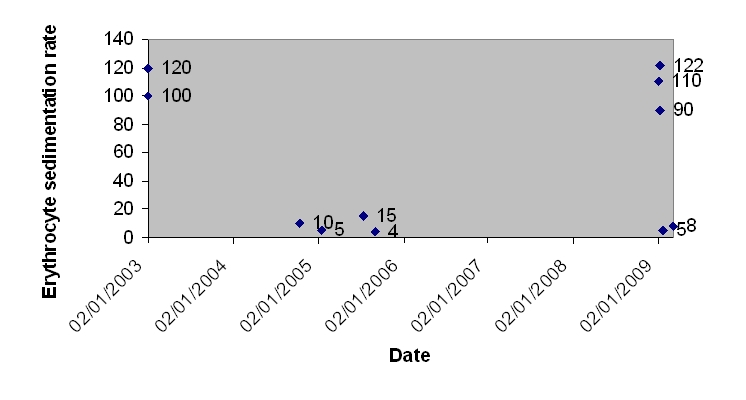
Erythrocyte sedimentation rate trend from 2003 to current presentation.
Visual evoked potential provided paraclinical evidence of right optic nerve demyelination. Nerve conduction studies showed no electrophysiological evidence of a radiculopathy. MRI of the brain and spine was reviewed with our neuroradiology colleagues and showed several high signal foci in the white matter and grey–white matter interface with some pachymeningeal enhancement in the brain on contrast administration (figure 2A–C). Spine MRI was unremarkable. CT angiogram was performed and was not indicative of a vasculitic process. Due to the clinical presentation we also performed CT of the thorax and gallium scan to exclude the possibility of sarcoidosis. Both scans proved normal.
Figure 2.
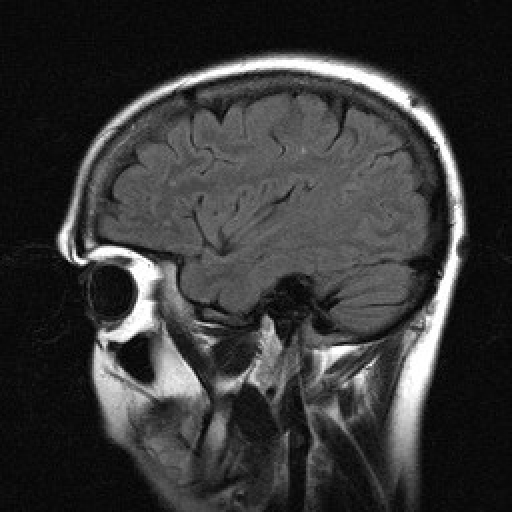
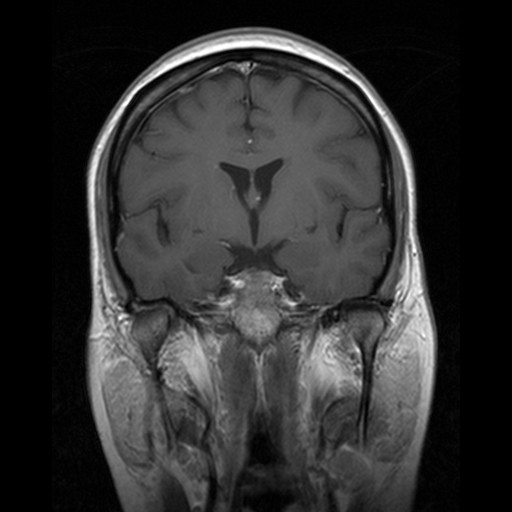
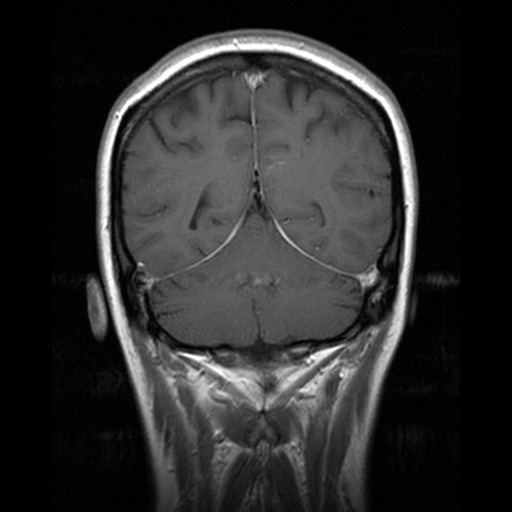
MRI appearances of parenchymal and pachymeningeal enhancement. (A) MRI sagittal T2 image showing few high signal foci within brain parenchyma. (B) MRI coronal T1+C image showing pachymeningeal enhancement over the right parietal cortex. (C) MRI coronal T1+C image showing diffuse tentorial pachymeningeal enhancement.
Differential diagnosis
The clinical presentation was of a myelo-radiculopathy with meningoencephalopathy and optic neuritis. The differential diagnosis included neuroinflammatory disorders such as sarcoidosis, an autoimmune process, a neoplastic or paraneoplastic illness, or an infectious or parainfectious mediated illness, and is summarised in table 1.
Table 1.
Differential diagnoses of myelo-radiculopathy with optic neuritis
| Infective | Lyme disease | Tuberculosis | HIV | Atypical pneumonia | Treponema |
| Immune | Systemic lupus erythematosis/other vasculitides | Sarcoidosis | Behcet's disease | ||
| Other | Postinfective | Lymphoma | Pareneoplastic |
Treatment
The patient was initially treated by her general practitioner with 60 mg of oral prednisolone and had received two doses. We elected to treat her more aggressively with 1 g per day of methylprednisolone for 3 days with a slowly tapering course of oral prednisolone over 3 months.
Outcome and follow-up
The patient's headache rapidly improved on oral prednisolone and there was further marked improvement in both headache and vision with the administration of methylprednisolone. Concurrently there was rapid and substantial improvement in her haematological markers of inflammation with a reduction in ESR first to 90 by the following day and to 5 within 14 days. At 3-month follow-up her symptoms had entirely resolved although there were similar neurological findings in the limbs on examination. Visual acuity had improved to 6/5 OD and 6/4 OS. She remained on 5 mg per day of oral prednisolone to be reduced by 1 mg every 2 weeks.
Discussion
Acute C psittaci infection gives rise to the clinical picture of psittacosis, an ornithosis. A respiratory syndrome predominates as the presenting feature, as for other atypical pneumonias, although cases may present with neurological, gastrointestinal, cardiological, haematological or other systemic features.1 A neurological syndrome during the acute illness may range from headache to meningo-encephalitis to other rarer syndromes including cerebellar syndromes, transverse myelitis, cranial neuropathies and status epilepticus. Headache in acute infection occurs in 38–87% of cases.2 Other neurological syndromes are much rarer.
The diagnosis of psittacosis is usually confirmed by serological testing with either complement fixation or microimmunofluorescent (MIF) antibody (Ab) testing. Confirmation requires a compatible clinical illness together with either culture of C psittaci, a fourfold or greater change in Ab titre to at least 1:32 between acute and convalescent sampling, or MIF immunoglobulin M titre of at least 1:16. Cross reactivity with other Chlamydia species can occur. Our patient originally presented with acute pneumonia in 2003 and a fourfold change in titres was documented (figure 3). Further supportive evidence for this acute illness was of numerous contact infections from the same source.
Figure 3.
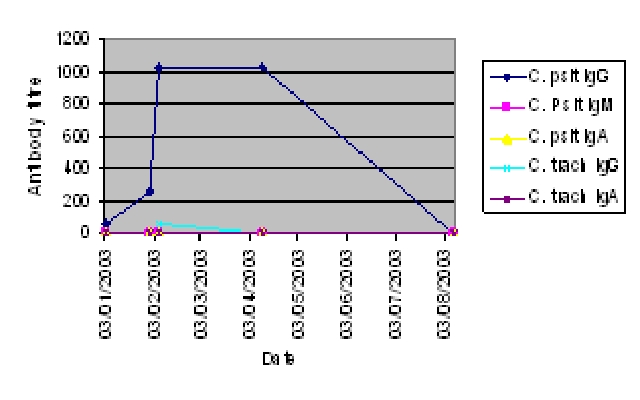
Diagnostic Chlamydia spp. titres during atypical pneumonia, 2003.
Reactive arthritis remote to incident infection has been reported in Chlamydia species infection3 and chronic or relapsing arthritis is associated with Chlamydia infection.4 The pathogenesis of reactive arthritis as a sequelae of Chlamydia infections remains under debate. There is evidence to suggest that chronic synovial infection may contribute. Host–antigen interaction seems to play a role in those with human leucocyte antigen B27, thought to alter the T cell response. Antigen induced immune complex formation and deposition may alternatively be invoked. To our knowledge delayed neurological manifestations have not been reported.
We propose that our patient, who had a clinically definite C psittaci infection with subsequent limited reactive arthritis, developed a late neurological manifestation of C psittaci infection. Haematological markers confirm a systemic inflammatory response (figure 1), but serological testing excluded recurrent active infection. Tests for other causes of optic neuritis and myelo-radiculopathy failed to reveal an alternative diagnosis in our patient, however we acknowledge that such a causal relationship to this association is speculative and we have not demonstrated a definitive pathophysiological mechanism.
Learning points.
-
▶
Chlamydia psittaci infection can present with neurological syndromes and should be tested for, in addition to other atypical pneumonias, in patients presenting with meningo-encephalitis or other neurological syndromes, who have respiratory or constitutional symptoms and signs.
-
▶
Delayed, immune mediated complications may occur from previous infections and should be considered even in remote infective histories after thorough investigations of alternative causes.
-
▶
In patients suspected of late manifestations of infectious processes or parainfectious processes steroids should be considered to moderate the immune processes involved.
Acknowledgments
The authors gratefully acknowledge input from Dr A Parry-Jones, specialist registrar in neurology and Dr J Hoyle, consultant physician.
Footnotes
Competing interests None.
Patient consent Obtained.
References
- 1.Crosse BA. Psittacosis: a clinical review. J Infect 1990;21:251–9 [DOI] [PubMed] [Google Scholar]
- 2.Hughes P, Chidley K, Cowie J. Neurological complications in psittacosis: a case report and literature review. Respir Med 1995;89:637–8 [DOI] [PubMed] [Google Scholar]
- 3.Koga T, Miyashita T, Watanabe T, et al. Reactive arthritis which occurred one year after acute chlamydial urethritis. Intern Med 2008;47:663–6 [DOI] [PubMed] [Google Scholar]
- 4.Inman RD, Whittum-Hudson JA, Schumacher HR, et al. Chlamydia and associated arthritis. Curr Opin Rheumatol 2000;12:254–62 [DOI] [PubMed] [Google Scholar]


