Abstract
A woman in her 40s originally from Zimbabwe presented to our accident department in the UK with a 4 day history of menorrhagia and exertional chest pain. Her clinical examination was unremarkable. Routine blood tests revealed a haemoglobin value of 6.8 g/dl and a platelet count of 15×109/l, with normal renal function and coagulation profile. Blood film showed microangiopathic haemolytic anaemia and thrombocytopenia. On direct questioning, she admitted to being HIV positive, and receiving antiviral therapy at another hospital. A diagnosis of HIV associated thrombotic thrombocytopenic purpura (TTP) was made. The patient was transferred to a tertiary centre for urgent plasma exchange. She required 8 days of 1.5 litre exchanges with solvent detergent fresh frozen plasma (FFP) and high dose steroids. She responded within 24 h with increasing haemoglobin and platelet counts, and at discharge her haemoglobin was 10.7 g/dl and platelet count 253×109/l.
BACKGROUND
This case highlights the need to consider thrombotic thrombocytopenic purpura (TTP) as a possible diagnosis in any patient presenting with a microangiopathic haemolytic anaemia blood picture and a low platelet count—especially when the coagulation screen is normal.
CASE PRESENTATION
A patient in her 40s, originally from Zimbabwe, presented with a 4 day history of pronounced menorrhagia and exertional chest pain. The patient was currently under investigation for anaemia, having had a negative colonoscopy and oesophagogastroduodenoscopy (OGD). Her initial medical history was of pulmonary tuberculosis in 2005 and a perforated duodenal ulcer treated in Zimbabwe in 1992. Clinical examination was entirely unremarkable except for pallor.
INVESTIGATIONS
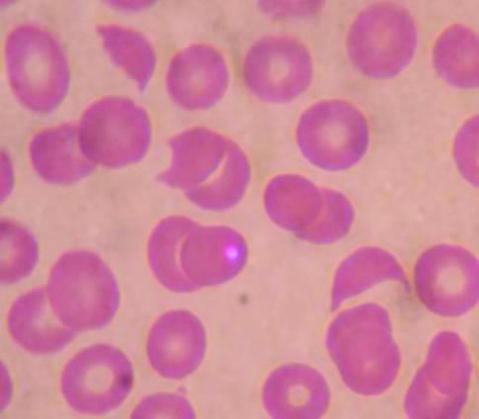
Routine initial blood tests showed a haemoglobin value of 6.8 g/dl, white cell count (WCC) of 8.5×109/l, and a platelet count of 15×109/l. Liver function tests showed an albumin value of 34 g/l, bilirubin 23 μmol/l, alanine aminotransferase (ALT) 43 IU/l, and alkaline phosphatase (ALP) 34 IU/l. Renal function was normal. Blood film showed a microangiopathic haemolytic anaemia with 5% schistocytes (fig 1). Coagulation screen was normal.
Figure 1.
Blood film showing three schistocytes (fragmented red cells), a spherocyte and thrombocytopenia.
DIFFERENTIAL DIAGNOSIS
Thrombotic thrombocytopenic purpura
Haemolytic uraemic syndrome
Immune thrombocytopenia and bleeding.
TREATMENT
Discovery of schistocytosis prompted urgent retrieval of the patient’s notes which revealed the patient was HIV positive, diagnosed in 2005, and was currently stable on an anti-retroviral regimen of Kaletra (lopinavir + ritonavir) and efavirenz, which was being monitored at another hospital. Once the diagnosis of TTP was established the patient was transferred the same day to a tertiary centre for urgent plasma exchange.
OUTCOME AND FOLLOW-UP
Testing on arrival at the tertiary centre revealed a lactate dehydrogenase (LDH) value of 1182 U/l, ADAMTS-13 activity <5%, and the presence of an IgG inhibitory antibody to ADAMTS-13.
Central venous access was established and she required 8 days of plasma exchange with solvent detergent treated fresh frozen plasma (FFP) and high dose steroids. She responded within 24 h. Her recovery was complicated by an episode of line sepsis which was treated with antibiotics and removal of the central line. She was discharged with a haemoglobin value of 10.7 g/dl and platelet count of 253×109/l.
DISCUSSION
TTP is a rare haematological disorder (incidence <1:100 000 per annum) characterised by an otherwise unexplained thrombocytopenia and microangiopathic haemolytic anaemia. It may furthermore present with renal failure, neuropathy and/or fever. Histologically, platelet thrombi form around damaged endothelium in affected tissues. Episodes are triggered by an accumulation of ultra-large high molecular weight von Willebrand’s Factor—which arise due to a constitutional or acquired deficiency of the cleaving protease, ADAMTS-13.1 TTP is a recognised complication of HIV.2 Some patients present with normal CD4 counts and an ADAMTS-13 inhibitor, similar to HIV negative patients. Other patients present with advanced HIV, low CD4 counts and no evidence of an ADAMTS-13 inhibitor.2
LEARNING POINTS
Rapid decline of platelet count and schistocytes >1.5% warrants an urgent coagulation screen. A normal coagulation screen is highly suggestive of thrombotic thrombocytopenic purpura (TTP). An abnormal coagulation screen usually indicates disseminated intravascular coagulopathy.
TTP carries a 90% mortality if untreated; this declines to 10% with plasma exchange.3 Therefore early diagnosis is lifesaving in most cases.
The diagnosis of TTP should prompt consideration of a number of risk factors including HIV, pancreatitis, pregnancy, underlying malignancy and certain medications—for example, cyclosporine, post-infective, autoimmune diseases.
HIV should be routinely considered in high risk groups; many patients may not inform the admitting medical team of their diagnosis.
Footnotes
Competing interests: none.
Patient consent: Patient/guardian consent was obtained for publication
REFERENCES
- 1.Furlan M, Lämmle B. Aetiology and pathogenesis of thrombotic thrombocytopenic purpura and haemolytic uraemic syndrome: the role of von Willebrand factor-cleaving protease. Best Practice & Research: Clinical Haematology 2001; 14: 437–54 [DOI] [PubMed] [Google Scholar]
- 2.Miller RF, Scully M, Cohen H, et al. Thrombotic thrombocytopenic purpura in HIV-infected patients. Int J STD AIDS 2005; 16: 538–42 [DOI] [PubMed] [Google Scholar]
- 3.Rock GA, Shumak KH, Buskard NA, et al. Comparison of plasma exchange with plasma infusion in the treatment of thrombotic thrombocytopenic purpura. Canadian Apheresis Study Group. N Engl J Med 1991; 325: 393–9 [DOI] [PubMed] [Google Scholar]