Dear Editor,
Recently in your journal, Sud et al. [1] reported on a meta-analysis of randomized controlled trials of mechanical ventilation in the prone position. They found a 16% reduction in relative risk of mortality among patients with baseline PaO2/FiO2 <100 mmHg, which was consistent with their a priori hypothesis that improved oxygenation during prone ventilation would be clinically important in patients at high risk of death from profound hypoxemia. Furthermore, post hoc analysis showed that the statistically significant difference between the relative risks of mortality in the more severely hypoxemic patients versus the less severely hypoxemic patients was robust across several PaO2/FiO2 thresholds up to 140 mmHg. This meta-analysis could help bedside clinicians in their decisions to mechanically ventilate patients in the prone position, or not.
The investigators chose a threshold PaO2/FiO2 of 100 mmHg because this value was used to stratify patients in a recent randomized controlled trial of mechanical ventilation in prone position [2], and because bedside clinicians can readily determine whether a patient’s PaO2/FiO2 is above or below this threshold. However, a practical question facing bedside clinicians when deciding to use or forego mechanical ventilation in the prone position is interpretation of the effects of the level of positive end-expiratory pressure (PEEP). Higher levels of PEEP recruit collapsed alveoli, and as such improve oxygenation. Thus, higher levels of PEEP could erroneously give the impression that acute respiratory distress syndrome (ARDS) is not present or resolving, causing bedside clinicians to forego the use of mechanical ventilation in the prone position.
Of course, it should be noted that the investigators chose to use the baseline PaO2/FiO2 as a threshold in their analysis. Frequently the baseline PaO2/FiO2 is not greatly influenced by PEEP, since the level of PEEP usually is low at the moment it is calculated (i.e., directly after initiation of mechanical ventilation). However, this may not always be true, especially not in intensive care units familiar with use of higher levels of PEEP (i.e., where PEEP is titrated on peripheral oxygenation, frequently before any arterial blood sample is obtained). In addition, patients may develop ARDS during the course of mechanical ventilation [3]. In these patients, higher levels of PEEP are used even more regularly.
Probably it was not possible to obtain sufficient data to calculate the Lung Injury Score [4] or the Oxygenation Index [5] from the trials that were meta-analyzed. Both the Lung Injury Score and the Oxygenation Index take into account the level of PEEP (or mean airway pressure). It can be questioned, however, whether bedside clinicians can readily determine these scores, and thus adequately use them in their decisions to use or forego mechanical ventilation in the prone position.
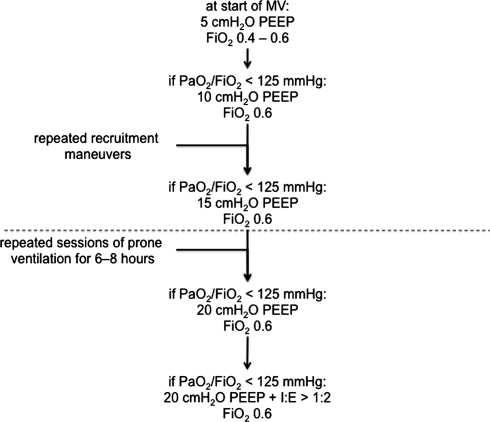
We developed a more practical approach in our intensive care unit (Fig. 1). In case of acute respiratory distress syndrome with profound hypoxemia (defined as PaO2/FiO2 <125 mmHg) we first raise the level of PEEP stepwise to 15 cmH2O. Each step may or may not be preceded by recruitment maneuvers by using sustained inflation. From then, the prone position is used, irrespective of PaO2/FiO2, with the knowledge that PaO2/FiO2 would decline if the level of PEEP would be reduced. Prone ventilation is continued as long as the level of PEEP to be used is ≥15 cmH2O. If PaO2/FiO2 remains <125 mmHg with prone ventilation, the level of PEEP is further increased and inversed ratio ventilation is used. This approach is not evidence based, though it is practical and in harmony with the findings of the meta-analysis by Sud et al. [1]. In our center, neither extracorporeal membrane oxygenation nor high-frequency oscillation nor ventilation with nitric oxide is used.
Fig. 1.
Schematic presentation of the local mechanical ventilation guideline; mechanical ventilation in the prone position is used when the level of PEEP is >15 cmH2O, aiming for PaO2/FiO2 >125 mmHg (below the dotted line); prone position is continued for 6–8 h, and is repeated until PaO2/FiO2 stays well above 125 mmHg; in addition, if PaO2/FiO2 remains <125 mmHg in prone position, the level of PEEP is further increased and inversed ratio ventilation is used
Open Access
This article is distributed under the terms of the Creative Commons Attribution Noncommercial License which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
References
- 1.Sud S, Friedrich JO, Taccone P, Polli F, Adhikari NK, Latini R, Pesenti A, Guerin C, Mancebo J, Curley MA, Fernandez R, Chan MC, Beuret P, Voggenreiter G, Sud M, Tognoni G, Gattinoni L. Prone ventilation reduces mortality in patients with acute respiratory failure and severe hypoxemia: systematic review and meta-analysis. Intensive Care Med. 2010;36:585–599. doi: 10.1007/s00134-009-1748-1. [DOI] [PubMed] [Google Scholar]
- 2.Taccone P, Pesenti A, Latini R, Polli F, Vagginelli F, Mietto C, Caspani L, Raimondi F, Bordone G, Iapichino G, Mancebo J, Guérin C, Ayzac L, Blanch L, Fumagalli R, Tognoni G, Gattinoni L, Prone-Supine II Study Group Prone positioning in patients with moderate and severe acute respiratory distress syndrome: a randomized controlled trial. JAMA. 2009;302:1977–1984. doi: 10.1001/jama.2009.1614. [DOI] [PubMed] [Google Scholar]
- 3.Gajic O, Frutos-Vivar F, Esteban A, Hubmayr RD, Anzueto A. Ventilator settings as a risk factor for acute respiratory distress syndrome in mechanically ventilated patients. Intensive Care Med. 2005;31:922–926. doi: 10.1007/s00134-005-2625-1. [DOI] [PubMed] [Google Scholar]
- 4.Murray JF, Matthay MA, Luce JM, Flick MR. An expanded definition of the adult respiratory distress syndrome. Am Rev Respir Dis. 1988;138:720–723. doi: 10.1164/ajrccm/138.3.720. [DOI] [PubMed] [Google Scholar]
- 5.Ortiz RM, Cilley RE, Bartlett RH. Extracorporeal membrane oxygenation in pediatric respiratory failure. Pediatr Clin North Am. 1987;34:39–46. doi: 10.1016/s0031-3955(16)36179-x. [DOI] [PubMed] [Google Scholar]