Abstract
The unusual case of a 31-year-old woman who developed tricuspid valve endocarditis with positive blood cultures for Escherichia coli is presented. The patient had no underlying cardiac disease or predisposing conditions that could have made her susceptible to the native valve infection. Despite a lengthy course of intravenous antibiotics only a partial response was achieved. The patient underwent cardiac surgery and had a good postoperative recovery.
Background
Infective endocarditis is an important differential diagnosis for any patient presenting with pyrexia of unknown origin. This report serves as an example of the principle that even in young, previously healthy and normal subjects a presentation of persistent fever should among others prompt investigation of endocarditis. A detailed history is essential and may uncover constitutional symptoms that should not be underestimated and are often key in leading to a diagnosis of subacute bacterial endocarditis.
This case highlights for clinicians that the diverse nature and evolving epidemiological profile of infective endocarditis ensures that it remains a diagnostic challenge. We must be aware that the prevalence of tricuspid valve endocarditis (TVE) in non-intravenous drug users (non-IVDUs) is rising,1 therefore a high index of suspicion and low threshold for investigation to exclude infective endocarditis should not just be applicable to high-risk groups (for example, intravenous drug users) but anyone who presents with a pyrexia of unknown origin.
The case also is a reminder of the role of the modified Duke criteria. It remains the leading assessment criteria, as recommended in the European Society of Cardiology (ESC) guidelines, however it must be remembered that it is useful for the classification of infective endocarditis but it should not replace clinical judgement.
Case presentation
A 31-year-old woman with no significant medical history presented with pyrexia, lower abdominal and pelvic pain in mid July 2009. She was found to have thrombocytopoenia with a platelet level of 15 x 109/L (normal range 150–400), haemoglobin (Hb) 10.7 g/dl (normal range 12.0–16.0 g/dl), white cell count (WCC) 7.23 109/L (normal range 4.2–10.8), C reactive protein level of 192 mg/L (normal range 0–10), mildly elevated liver function tests (conjugated bilirubin 50 μmol/L (normal range 0–5)) and normal urea and electrolytes. This was initially thought to be secondary to a viral infection. A set of blood cultures taken on admission were positive for Escherichia coli. CT of the abdomen and pelvis, a chest x-ray, transvaginal scan, midstream urine (MSU) test, sexually transmitted disease screening and viral serology including HIV revealed no clear infective source. She received intravenous meropenam and metronidazole. She was discharged 2 weeks later with a 5-day course of amoxicillin.
The patient then re-presented in mid August with ongoing lower abdominal tenderness, non-specific malaise and night sweats. A further set of blood cultures was still positive for E coli, repeat imaging (CT of the abdomen and pelvis and chest x-ray) and tests again found no source for her illness. Her blood tests showed ongoing anaemia (Hb 11.8 g/dl), elevated C reactive protein (60 mg/L) and a normal WCC. Due to her persistent pyrexia a transthoracic echocardiogram (TTE) was performed on 27 August. This revealed a large mobile vegetation on her tricuspid valve with moderate tricuspid regurgitation.
Investigations
Once diagnosed as having TVE, the following tests were completed to try and explain how this previously fit and well woman had developed tricuspid valve disease. Blood cultures: these were repeated with each spike in temperature; 24 readings taken in total. Microbiology: tests were performed for hepatitis B+C, HIV, autoimmune profile, cat scratch disease, Borrelia burgdorferi and chlamydia serology. ‘HACEK’ group tests for influenza A+B, Coxiella burnetti, RSV, Mycoplasma pneumoniae and adenovirus were also performed. Urine tests: 5-hydroxyindoleacetic acid (5-HIAA; to exclude carcinoid syndrome), MSU (multiple) and a urine drug screen were performed. High vaginal swabs: swabs for chlamydia and gonorrhoea were taken. Sputum cultures: these were also taken. The above tests were all negative.
Reviews by ear, nose and throat, gastroenterology, gynaecology, respiratory and maxillofacial teams shed no further light on the possible source. Two decaying wisdom teeth were extracted to remove a potential source of infection.
TTEs and a transoesophageal echocardiography were completed during this admission. A TTE on 1 October showed an increase in the size of tricuspid vegetation (figure 1). There was a large mobile mass attached to the anterior leaflet (118 mm2) with a smaller mass at the base of the posterior leaflet (45 mm2).
Figure 1.
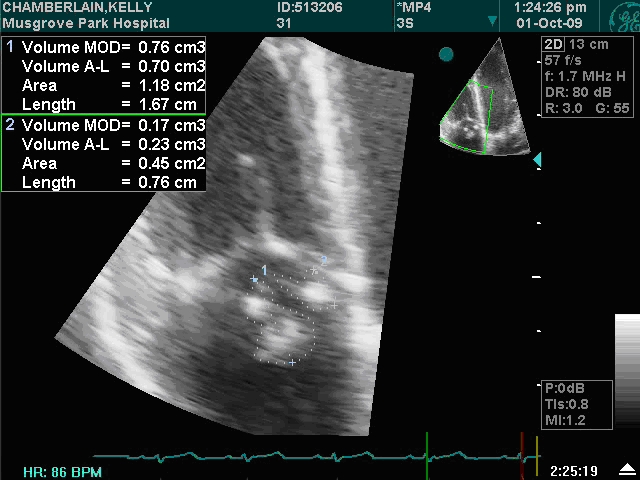
A transthoracic echo taken on 1 October 2009, showing large mobile vegetations on the anterior and posterior leaflets of the tricuspid valve.
Treatment
Imipenem and gentamicin were given following microbiological advice. Despite this she had persistent pyrexia. Her inflammatory markers initially decreased to a C reactive protein level as low as 21 in response to antibiotics, but on two occasions the C reactive protein level increased to over 300, which correlated with septic emboli to the lung. On both these occasions the patient had pleuritic pain, which led to two CT pulmonary angiographies being performed (28 August 2009 and 5 October 2009).
After a 6-week course of intravenous antibiotics with continued pyrexia and a C reactive protein level of approximately 100, surgery was considered as indicated by the ESC guidelines. The patient underwent a valvectomy on 14 October 2009.
Outcome and follow-up
Samples of the vegetation from surgery underwent further analysis. Histology was consistent with chronic vegetation; special stains demonstrated no bacteria or fungi. Scrapings from the valve were culture negative. The patient completed a further 2 weeks of meropenem, as advised by microbiologists, during which she remained apyrexial with a normal C reactive protein level of 1. Her final TTE showed the repaired tricuspid valve leaflets functioning well with only a trace of regurgitation. She was then discharged with no further complications.
Discussion
Infective endocarditis caused by Gram-negative bacilli is rare and commonly considered to be primarily a disease of IVDUs2 Staphylococcus aureus is the organism most frequently isolated (60% to 90%)3 in cases of TVE as it naturally colonises the skin and is commonly introduced by IVDUs. Other causative organisms of TVE include Candida species, especially Candida glabrata, Streptococcus bovis, Gemella morbillorum and Pseudomonas aeruginosa.4
Most bacteria can of course cause native valve endocarditis (NVE), however it is rare to contract E coli NVE, with only 36 cases being reported between 1902 and 2002.3 Micol et al5 reported that the majority of cases were in older (>70 years) women, with the urinary tract being the most common portal of entry. Of the 36 cases reviewed, 20 involved the mitral valve with no specific number documented for tricuspid valve involvement. A literature search found only one case report, by Magalhaes et al,6 of TVE due to E coli in a 16-year-old boy with no predisposing risk factors for endocarditis.
As reported by Jauréguy et al,7 bacteraemia from E coli is one of the most common bloodstream isolates, for which it is associated with a high rate of morbidity and mortality. Although the extraintestinal pathogenic E coli strains are rarely responsible for endocarditis, clinicians will frequently encounter E coli bacteraemia with some reports suggesting that it accounts for approximately 20% of all clinically significant bloodstream isolates. Therefore the differential diagnosis of endocarditis is important and should never be discounted when faced with E coli bacteraemia.
This case was not atypical of infective endocarditis, with the patient having subacute pyrexia of unknown origin. The patient's history and clinical presentation fulfilled both major criteria of the modified Duke's criteria.8 There were two separate occasions in which blood cultures grew E coli. Unfortunately, despite extensive investigations and reviewing the chronology of the patient's history the portal of entry of the micro-organism was never found. We can only propose that we were unlucky in missing the portal of entry or that the true causative organism was never cultured. It was disappointing but not unexpected that cultures of the valve scrapings were negative due to the long course of intravenous antibiotics that the patient had received prior to surgery. This case highlights that TVE is rarely considered in the differential diagnosis of a patient who is febrile who does not use intravenous drugs, however it is an important differential diagnosis that must never be forgotten, especially as this is not an exceptional case but rather emphasises, as reported by Heydari et al,4 that isolated TVE continues to occur, eluding diagnosis and sometimes only discovered at autopsy.
Throughout this patient's admission expert microbiological advice was sought. Her antibiotic treatment was felt sufficient to cover E coli as well as other Gram-negative bacilli. It was unusual to see only a partial response after 6 weeks of a therapeutic regime.
The ESC guidelines3 recommend that surgical treatment should be considered, as follows, in cases of treatment resistant right-sided infective endocarditis.
Micro-organisms difficult to eradicate or bacteraemia >7 days despite adequate antimicrobial treatment, or
Persistent tricuspid valve vegetation (>20 mm) after recurrent pulmonary emboli with or without concomitant right heart failure.
The guidelines advocate valvectomy without prosthetic replacement, which is what our patient underwent.
Although the ESC guidelines provide specific parameters this report highlights a common problem faced by clinicians, as was found in this case, in terms of optimal timing for tricuspid valve surgery. There appears to be no universal agreement. A study by Sung et al9 found that earlier operative timings may improve early outcomes, however these favourable results could not be satisfactorily explained. The general consensus is that it would be unwise to delay surgery because of the potentially high operative mortality.
Sung et al9 suggest that tricuspid tissue valve repair can nowadays be performed with low operative mortality achieved through optimal perioperative management. A study by Bleiweis et al10 was unable to isolate any significant pre/intraoperative risk factors for operative death, however both studies9 10 recognise that certain strategies, such as improved myocardial protection, optimal perioperative care and modified ultrafiltration, play an important role in lowering operative mortalities.
In conclusion, our patient was fortunate to have made such a successful full recovery from TVE and surgery. The case presented with atypical bacteria, she had no evidence of intravenous drug use, she was not infected with HIV or hepatitis and she herself vehemently denied any intravenous drug use. We have no reason to suspect otherwise, and for that very reason we were lost without Occam's razor.
Learning points.
There should always be a high index of suspicion for infective endocarditis in patients who present with a clinical picture of persistent fever (>38 °C) of unknown origin, even in young, normal subjects.
Clinicians should be aware that the prevalence of tricuspid valve endocarditis (TVE) in non-intravenous drug users (non-IVDUs) is rising.1
In accordance with the European Society of Cardiology (ESC) guidelines there is no rationale for delaying blood culture sampling to coincide with peaks of fever.3
Footnotes
Competing interests None.
Patient consent Obtained.
References
- 1.Castillo JC, Anguita MP, Torres F, et al. Comparison of features of active infective endocarditis involving native cardiac valves in nonintravenous drug users with and without predisposing cardiac disease. Am J Cardiol 2002;90:1266–9 [DOI] [PubMed] [Google Scholar]
- 2.Morpeth S, Murdoch D, Cabell CH, et al. ; International Collaboration on Endocarditis Prospective Cohort Study (ICE-PCS) Investigators Non-HACEK Gram-negative bacillus endocarditis. Ann Intern Med 2007;147:829–35 [DOI] [PubMed] [Google Scholar]
- 3.Habib G, Hoen B, Tornos P, et al. Guidelines on the prevention, diagnosis, and treatment of infective endocarditis (new version 2009): the Task Force on the Prevention, Diagnosis, and Treatment of Infective Endocarditis of the European Society of Cardiology (ESC). Eur Heart J 2009;30:2380, 2402–3 [DOI] [PubMed] [Google Scholar]
- 4.Heydari AA, Safari H, Sarvghad MR. Isolated tricuspid valve endocarditis. Int J Infect Dis 2009;13:e109–11 [DOI] [PubMed] [Google Scholar]
- 5.Micol R, Lortholary O, Jaureguy F, et al. Escherichia coli native valve endocarditis. Clin Microbiol Infect 2006;12:401–3 [DOI] [PubMed] [Google Scholar]
- 6.Magalhaes V, Markman Filho B, Lucena V, et al. Tricuspid valve endocarditis due to Escherchia coli: a case report. Rev Bras Med 1995;52:231–2 [Google Scholar]
- 7.Jauréguy F, Carbonnelle E, Bonacorsi S, et al. Host and bacterial determinants of initial severity and outcome of Escherichia coli sepsis. Clin Microbiol Infect 2007;13:854–62 [DOI] [PubMed] [Google Scholar]
- 8.Modified Duke criteria for the diagnosis of infective endocarditis, 2009:2382, table 11. http://www.escardio.org/guidelines-surveys/esc-guidelines/GuidelinesDocuments/guidelines-IE-FT.pdf [Google Scholar]
- 9.Sung K, Park PW, Park KH, et al. Is tricuspid valve replacement a catastrophic operation? Eur J Cardiothorac Surg 2009;36:825–9 [DOI] [PubMed] [Google Scholar]
- 10.Bleiweis MS, deVirgilio C, Milliken JC, et al. Tricuspid valve surgery: 15-year experience. J Natl Med Assoc 1996;88:645–8 [PMC free article] [PubMed] [Google Scholar]


