Abstract
Xeroderma pigmentosum is a rare autosomal recessive disease characterised by hypersensitivity to sunlight, and is associated with a high incidence of skin cancer. We report a case of xeroderma pigmentosum with malignant neurilemoma in a 46-year-old woman which is unique due to its presentation, which was confirmed histopathologically.
Trial registration number:
31095
BACKGROUND
Xeroderma pigmentosum (XP) is a rare autosomal recessive disease characterised by hypersensitivity to sunlight and is associated with a high incidence of skin cancer; some groups of patients exhibit variable neurological abnormalities. Squamous cell carcinomas, basal cell carcinomas and malignant melanomas appear at an early age in patients with XP.1 We report a case of XP with malignant neurilemoma in a 46-year-old woman. The case report has been prepared in compliance with Beijing Tongren Hospital Ethics Committee guidelines.
CASE PRESENTATION
A 46-year-old woman presented with a decrease in vision, photophobia, blepharospasm and lacrimation of the left eye 2 months earlier, for which topical eye drugs were not helpful. The left eye was enucleated and the orbit implanted with hydroxyapatite for keratohelcosis. There were multiple hyperpigmented lesions all over her body except in the armpit, which had been present since she was 3 years old, and she had simultaneously developed photophobia and corneal dryness. The pigmented lesion was raised 4–6 mm from the surface. It was nodular, soft and immovable in places. On ocular examination, in the left eye a large orbital firm mass with an irregular outer surface of 2.0 cm × 2.5 cm was present, which was attached to the palpebral conjunctiva and the eyelids and could move with hydroxyapatite (fig 1). The right upper lid and lower lid showed hyperpigmented and hypopigmented maculas similar to the rest of the body, and corneal opacity involving the entire cornea. The patient had no other contributory non-ocular findings.
Figure 1.

The patient with a mass in the left orbit preoperatively. The pigmented lesion was raised 4–6 mm from the surface. She developed a firm mass in the interpalpebral zone of the left eye measuring 2.0×2.5 cm, which was attached to the palpebral conjunctiva and the eyelids.
INVESTIGATIONS
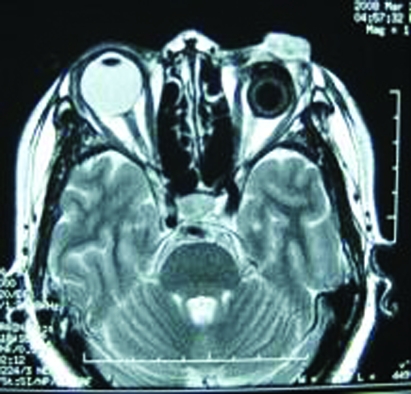
On magnetic resonance imaging (MRI) scanning, the mass appeared undefined, solitary and anterior of the hydroxyapatite. The mass was isointense with respect to the extraocular muscles and brain on T1 weighted images, and hyperintense on T2 weighted images with contrast enhancement, asymmetrical signals. MRI disclosed a heterogeneous signal intensity on T2 weighted images (fig 2). On contrast enhanced computed tomography (CT) scanning, the mass was enhanced heterogeneously, showing patchy unenhanced areas. The patient was assessed for evidence of metastasis in the lung or the liver by chest x ray and abdominal sonar. Bleeding and coagulation profiles, ECG, liver and kidney functions tests were routinely performed before surgery.
Figure 2.
Magnetic resonance image disclosing a heterogeneous signal intensity on T2 weighted images.
The presumptive diagnosis of XP and orbital tumour was made, and orbital exenteration was carried out. Biopsy revealed a malignant schwannoma. Histologically, mitotic figures were easily found. Immunohistochemically, the tumour cells were positive for NSE vimentin, CK, partly positive for S-100, EMA, desmin and negative for GFAP, Syn, HMB45, HHF35, and CD34 (figs 3 and 4).
Figure 3.
Histological examination revealed a typical pattern of schwannoma consisting of Antoni type B. Histopathologically, the tumour tissue consists of so-called Antoni A and B type cells. Type A tissue shows densely packed, elongated spindle cells, while type B tissue has a more myxoid consistency. Haematoxylin and eosin; original magnification ×20.
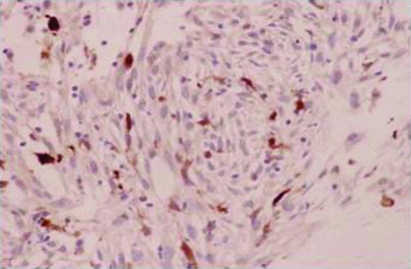
Figure 4.
S-100 protein is positive in immunochemistry staining. Immunohistochemically, the tumour cells were partly positive for S-100. Original magnification ×200.
TREATMENT
Based on the above mentioned findings, a diagnosis of XP with malignant neurilemoma of the orbit was confirmed. After surgery, antibiotics were given to prevent infections and general management of the patient included protection from ultraviolet radiation and the administration of steroid drops to the right orbit.
OUTCOME AND FOLLOW-UP
The patient was followed up for 2 weeks postoperatively. The wound healed satisfactorily and the proptosis was reduced (fig 5).
Figure 5.

The mass in the left orbit was dissected 2 weeks postoperatively.
DISCUSSION
XP was first described in 1874 by Hebra.2 It is characterised by photosensitivity, pigmentary changes, photophobia, and propensity for early development of malignancy after sunlight exposure that causes mucocutaneous and neurological abnormalities. Among the ocular tissues, the lids, conjunctiva and cornea are predominantly affected because they are exposed to ultraviolet radiation from sunlight. Ocular surface neoplasms, including squamous cell carcinoma and basal cell carcinoma, occur with a predilection for the limbal area. Basal cell carcinoma and squamous cell carcinoma of the lids and cornea (limbus) occur frequently.3 The case reported here is a type of neurilemoma, and is extremely rare. Yamashiro et al4 and Nakamura et al5 have reported similar cases.
Neurilemomas are uncommon orbital tumours that arise from the Schwann cell sheaths of peripheral nerves. About 2% of space occupying orbital lesions have been reported to be peripheral nerve tumours, with approximately 1% neurilemomas.6 Neurilemoma extends from the glial–schwannian junction in the cranial nerves and spinal roots to the termination of the nerve fibres in its end organ receptor, and includes the posterior root ganglia. Neurilemomas may affect any location throughout the peripheral nervous system. They arise within a nerve consisting of a single fascicle. The tumours are composed entirely of the supporting Schwann cells and peripherally displaced nerve fibres, resulting in a globoid eccentric tumour mass. In the early intrafascicular growth phase, small neurilemomas displace nerve fibres without forming a capsule. The larger tumours increase the size of the parent nerve and become separated from surrounding fascicles by a capsule derived from the perineurium and epineurium.
Neurilemoma is also very useful in evaluating intracranial extension; it usually has an intermediate intensity on T1 weighted images, and the T2 weighted signal varies from intermediate to high, depending on the cellularity of the lesion and the cystic characteristics of the lesion (fig 2). With the enhancement pattern, you can see the mottling of the lesion and the heterogenous appearance; post-contrast, it is a lot cleaner and enhancing more evenly across the field.
The histopathology shows a biphasic pattern of Antoni A and Antoni B areas (fig 3). The Antoni A areas comprise compact cells with twisted nuclei and occasionally intranuclear vacuoles. Antoni B areas are the degenerative areas composed of spindle cell shapes running in a haphazard manner. The entire tumour may be composed of either area. They are commonly intermixed. Immunohistochemical staining using anti–S-100 protein antibody demonstrates uniformly and intensely positive staining of Schwann cells in the tumour (fig 4). Since the clinical manifestations and image findings are usually non-specific, histopathological examination is the main method to make a definite diagnosis.
The management of this patient involved measures to avoid exposure to the harmful effects of ultraviolet rays of the sun and fluorescent lamps (tube light), which may emit ultraviolet rays, and the application of sunscreens to the skin.
LEARNING POINTS
Xeroderma pigmentosum is a rare autosomal recessive disease characterised by hypersensitivity to sunlight.
Ocular surface neoplasms, including squamous cell carcinoma and basal cell carcinoma, can occur with a predilection for the limbal area.
The case reported here is a type of neurilemoma, and is extremely rare.
Footnotes
Competing interests: none.
Patient consent: Patient/guardian consent was obtained for publication
REFERENCES
- 1.Norgauer J, Idzko M, Panther E, et al. Xeroderma pigmentosum. Eur J Dermatol 2003; 13: 4–9 [PubMed] [Google Scholar]
- 2.Hebra F, Kaposi M. On diseases of the skin including exanthemata. New Sydenham Soc 1874; 61: 252–8 [Google Scholar]
- 3.Mseddi M, Sellami D, Elloumi Y, et al. Ophthalmologic manifestations of the xeroderma pigmentosum. Tunis Med 2006; 84: 542–4 [PubMed] [Google Scholar]
- 4.Yamashiro S, Nagahiro S, Mimata C, et al. Malignant trigeminal schwannoma associated with xeroderma pigmentosum—case report. Neurol Med Chir (Tokyo) 1994; 34: 817–20 [DOI] [PubMed] [Google Scholar]
- 5.Nakamura T, Ono T, Yoshimura K, et al. Malignant schwannoma associated with xeroderma pigmentosum in a patient belonging to complementation group D. J Am Acad Dermatol 1991; 25(2pt 2): 349–53 [DOI] [PubMed] [Google Scholar]
- 6.Shields JA, Shields CL, Scartozzi R. Survey of 1264 patients with orbital tumors and simulating lesions: the 2002 Montgomery lecture, part 1. Ophthalmology 2004; 111: 997–1008 [DOI] [PubMed] [Google Scholar]