Abstract
A 48-year-old woman presented with a 2-week history of diarrhoea and abdominal pain. No overt gastrointestinal bleeding was reported and there was no history of loss of weight or loss of appetite. General and abdominal examination was unremarkable except for subconjunctival pallor. The haemoglobin was 7.1 g/dl at presentation with the peripheral blood film indicating iron deficiency anaemia. An urgent colonoscopy revealed two strictures within a 5 cm segment of transverse colon. The distal stricture showed significant ulceration and inflammation, while the proximal one showed an impassable “diaphragm-like” stricture. Biopsies from both of the strictures showed chronic inflammatory infiltrate with numerous eosinophils and no evidence of malignancy. The patient had been taking enteric-coated diclofenac tablets 50 mg three times daily over the past 10 years for chronic backache. Her bowel symptoms resolved significantly within 4 weeks of stopping diclofenac and she continued to remain relatively asymptomatic at 3 months follow-up.
BACKGROUND
Non-steroidal anti-inflammatory drug (NSAID) prescriptions have increased over the last decade. Colonic strictures associated with their usage have been reported, but is rare. There needs to be increased awareness about this distinct entity, which may present with symptoms of malignancy or with features of bowel obstruction or perforation. Endoscopists need to be aware of the findings of this condition and the importance of careful history taking, so as to allow timely diagnosis.
CASE PRESENTATION
A 48-year-old woman presented with 2-week history of diarrhoea and abdominal pain. There was no history of any change in bowel habits prior to this, or any per-rectal bleeding or maelena. She did not complain of any history of loss of weight or loss of appetite. On examination, subconjunctival pallor was noted. The rest of the examination, including abdominal examination, was unremarkable. Her past medical history included lumbar discectomy in 2002 and chronic lower backache. She did not smoke and took alcohol rarely. There was no family history of bowel or other malignancy.
INVESTIGATIONS
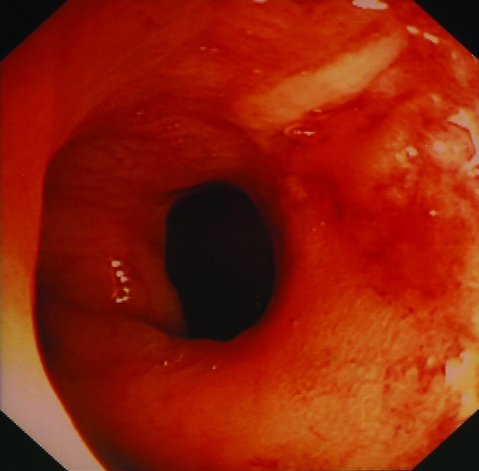
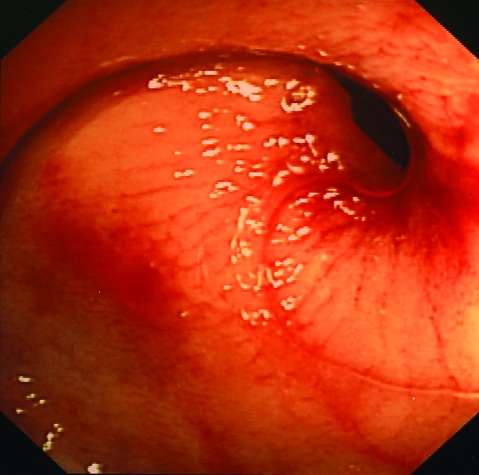
The haemoglobin was 7.1 g/dl at presentation with the peripheral blood film indicating iron deficiency anaemia. An urgent colonoscopy revealed two strictures within a 5 cm segment of transverse colon. The distal stricture showed significant ulceration and inflammation (fig 1), while the proximal stricture showed an impassable “diaphragm-like” stricture (fig 2). Biopsies from both of the strictures showed a chronic inflammatory infiltrate with numerous eosinophils and no evidence of malignancy. A barium enema demonstrated a tight stricture at the level of hepatic flexure, holding the contrast from passing proximally. CT colonography demonstrated three relatively tight strictures within the mid ascending to proximal transverse colon. No other intrinsic abnormality was demonstrated within the rest of the colon.
Figure 1.
Distal stricture showing diaphragm-like stricture, ulceration and inflammation.
Figure 2.
Proximal stricture showing classic diaphragm-like appearance.
DIFFERENTIAL DIAGNOSIS
The differential diagnosis included malignant stricture, diverticular stricture or stricture secondary to Crohn disease.
TREATMENT
Retrospective questioning confirmed that the patient had been taking enteric-coated diclofenac tablets 50 mg three times daily over the past 10 years for chronic backache. Her bowel symptoms resolved significantly within 4 weeks of stopping diclofenac.
OUTCOME AND FOLLOW-UP
Follow-up in the clinic 3 months after presentation showed significant improvement in bowel symptoms. We have planned to repeat imaging or endoscopy based on assessment at next clinic visit.
DISCUSSION
Colonic diaphragm-like strictures result from chronic use of sustained-release NSAIDs.1 NSAID-induced strictures were first described in 1989.2 These have been reported in at least 50 cases over the last 10 years because of increased use of NSAIDs worldwide. These strictures are predominantly seen in proximal ascending colon, but can occur anywhere along the length of small or large bowel.3 These patients present with either symptoms of malignancy or may present acutely with perforation.4 NSAID intake to stricture formation duration can be as short as 18 months.5
The exact pathophysiology of NSAID-induced colonic strictures is not clear. One theory postulates local toxic effects of a sustained-release NSAID preparation on mucosal integrity because of inhibition of protective prostaglandins, through a mechanism involving cyclo-oxygenase (COX).6 Other mechanisms by which NSAIDs can damage local mucosa include increasing intestinal permeability, uncoupling of mitochondrial oxidative phosphorylation or modulating COX-independent signal transduction pathways.7 A systemic effect of NSAIDs causing bowel strictures has been recorded previously.8 The diaphragms are characterised histologically by submucosal fibrosis and a chaotic arrangement of smooth muscle fibres, and vascular and neural elements, resembling hamartomas.9
In the majority of cases, discontinuation of the offending drug results in symptom resolution.10 Severe stenotic stricture may require surgical resection. Endoscopic pneumatic dilatation may be an alternative to surgery.7
LEARNING POINTS
Colonic strictures induced by non-steroidal anti-inflammatory drugs (NSAIDs) are also called “diaphragm disease of colon”, as they produce diaphragm-like strictures.
They are increasing in incidence due to the popularity of NSAIDs.
Endoscopists need to be aware of this condition and the triad of diaphragm-like stricture, ulceration and inflammation.
They are common in ascending colon, but can occur anywhere along the length of small and large bowel.
In the majority of cases, discontinuation of the offending drug results in symptom resolution.
Footnotes
Competing interests: none.
Patient consent: Patient/guardian consent was obtained for publication.
REFERENCES
- 1.Stolte M, Karimi D, Vieth M, et al. Strictures, diaphragms, erosions or ulcerations of ischaemic type in colon should always prompt consideration of nonsteroidal anti-inflammatory drug-induced lesions. World J Gastroenterol 2005; 11: 5828–33 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Sheers R, Williams WR. NSAIDs and gut damage [letter]. Lancet 1989; 2: 1154. [DOI] [PubMed] [Google Scholar]
- 3.Thiéfin G, Beaugerie L. Toxic effects of nonsteroidal antiinflammatory drugs on the small bowel, colon, and rectum. Joint Bone Spine 2005; 72: 286–94 [DOI] [PubMed] [Google Scholar]
- 4.Aloysius MM, Kaye PV, Lobo DN. Non-steroidal anti-inflammatory drug (NSAID)-induced colonic strictures and perforation: a case report. Dig Liver Dis 2006; 38: 276–8 [DOI] [PubMed] [Google Scholar]
- 5.Hjartarson HF, Cariglia N, Bjœrnsson J. NSAIDs-induced colopathy with diaphragm-like strictures – Case report. Laeknabladid 2004; 90: 133–5 [PubMed] [Google Scholar]
- 6.Cipolla G, Crema F, Scco S, et al. Nonsteroidal anti-inflammatory drugs and inflammatory bowel disease: current perspectives. Pharmacol Res 2002; 46: 1–6 [DOI] [PubMed] [Google Scholar]
- 7.Smith JA, Pineau BC. Endoscopic therapy of NSAID-induced colonic diaphragm disease: two cases and a review of published reports. Gastrointest Endosc 2000; 52: 120–5 [DOI] [PubMed] [Google Scholar]
- 8.Whittle BJR. COX-1 and COX-2 products in the gut: therapeutic impact of COX-2 inhibitors. Gut 2000; 47: 320–5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kelly ME, McMahon LE, Jaroszewski DE, et al. Small-bowel diaphragm disease: seven surgical cases. Arch Surg 2005; 140: 1162–6 [DOI] [PubMed] [Google Scholar]
- 10.Mulcahy HE, O’Donoghue D. Nonsteroidal anti-inflammatory drugs and their colonic effects: more interesting than irritating? Eur J Gastroenterol Hepatol 2002; 14: 1177–8 [DOI] [PubMed] [Google Scholar]