Abstract
Published rates of comorbidity between pediatric bipolar disorder (PBD) and attention-deficit/hyperactivity disorder (ADHD) have been higher than would be expected if they were independent conditions, but also dramatically different across different studies. This review examines processes that could artificially create the appearance of comorbidity or substantially bias estimates of the ADHD-BPD comorbidity rate, including: categorization of dimensional constructs, overlap among diagnostic criteria, over-splitting, developmental sequencing, and referral or surveillance biases. Evidence also suggests some mechanisms for “true” BPD-ADHD comorbidity, including shared risk factors, distinct subtypes, and weak causal relationships. Keys to differential diagnosis include focusing on episodic presentation and non-overlapping symptoms unique to mania.
Bipolar and ADHD Comorbidity: Both Artifact and Outgrowth of Shared Mechanisms
“Comorbidity,” meeting criteria for more than one psychiatric disorder, is the rule--not the exception--in both clinical and research samples. Although comorbidity is a general phenomenon extensively reviewed (e.g., Angold, Costello, & Erkanli, 1999; Caron & Rutter, 1991; Youngstrom, Findling, & Calabrese, 2003), the observed comorbidity of pediatric bipolar disorder (PBD) and attention-deficit/hyperactivity disorder (ADHD) is a recent, fascinating example that has prompted intense debate (e.g., Biederman, Klein, Pine, & Klein, 1998; Klein, Pine, & Klein, 1998). This article uses BPD-ADHD comorbidity to illustrate established mechanisms that could lead to co-occurrence of symptoms or entire syndromes. After documenting the extent of comorbidity, we discuss mechanisms for “false” or artificial comorbidity, their relevance to the BPD-ADHD axis, and some processes that could account for “true” comorbidity between the two disorders. Our review closes with guidance about how to decide which disorder is “primary” if enough symptoms for both are present.
How Often Are ADHD and Bipolar Disorder Comorbid with Each Other?
The bipolar spectrum, which includes bipolar I, bipolar II, cyclothymic disorder, and bipolar NOS, affects between 0 and 6% of youths in epidemiological samples around the world, averaging 1.8% (Van Meter et al., under review). ADHD is far more common, with estimated prevalences from 5 to 10% (Smith, Barkley, & Shapiro, 2007). If BPD and ADHD were completely independent, then the only ~2% of cases with ADHD would be expected to have BPD. Conversely, only ~8% of cases with BPD would be expected to have ADHD as well, and only 3 youths out of every 2000 in the community would be unfortunate enough to have both conditions. However, a recent review of six non-referred samples found that the rates of comorbidity tended to be elevated well above chance levels (Galanter & Leibenluft, 2008).
The rates of comorbidity in clinical samples should be higher than found in unfiltered community samples: Because youths with both disorders would be more impaired, they would be more likely to seek services (“Berkson's bias”; Berkson, 1946). Thus comorbid cases would be over-represented in clinical samples. Published estimates from clinical samples run the full gamut from 0% (Hurtig et al., 2007) to 98% (Wozniak et al., 1995), with a meta-analysis of seven BPD studies finding an average rate of 62% also meeting criteria for ADHD (Kowatch, Youngstrom, Danielyan, & Findling, 2005). Two things are clear: (a) BPD-ADHD comorbidity is too common to be a chance co-occurrence of independent phenomena, and (b) the tremendous variability of rates deserves explanation.
Is It All a Mistake? “False” Comorbidity as a Potential Explanation
Caron & Rutter (1991) delineated several mechanisms that could result in “artifactual” and “true” comorbidity, all of which potentially contribute to some degree to the apparent ADHD-BPD comorbidity. Possible sources of artifactual comorbidity include:
(1) Using categorical labels where dimensions might be more appropriate
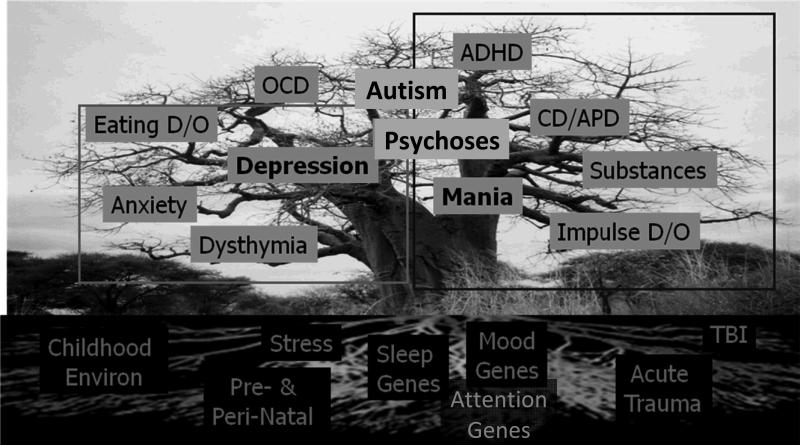
There is no hard edge separating normal development and the pathological mood states of bipolar disorder. Nor are there clear quantitative or qualitative boundaries between disorders within the bipolar spectrum, or between bipolar versus unipolar depression (Youngstrom, 2009). Formal statistical evaluations can find no distinct category underlying ADHD, whether by rating scales or neuropsychological instruments (Frazier, Youngstrom, & Naugle, 2007; Haslam et al., 2006). There is no firm boundary between the irritability or inattention associated with bipolar disorder and the same symptoms resulting from other syndromes. The apparent “comorbidity” appearing between BPD and ADHD could be an artifact of drawing categorical “boxes” over what actually is a seamless spectrum of symptoms flowing from the same developmental pathological process (see Figure 1, where the metaphorical “tree” branches into different symptom clusters defining different disorders).
Figure 1.
The Tree Metaphor for Bipolar Disorder Pathology, Etiologies, and Possibly Related Disorders: Equipotentiality of roots, multifinality of clinical course and presentations.
Note: Eating D/O = Eating Disorder; OCD = Obsessive/Compulsive Disorder; ADHD = Attention-Deficit/Hyperactivity Disorder; CD/APD = Conduct Disorder/Antisocial Personality Disorder; Impulse D/O = Impulse control Disorder; TBI = Traumatic Brain Injury
(2) Overlap in Diagnostic Criteria
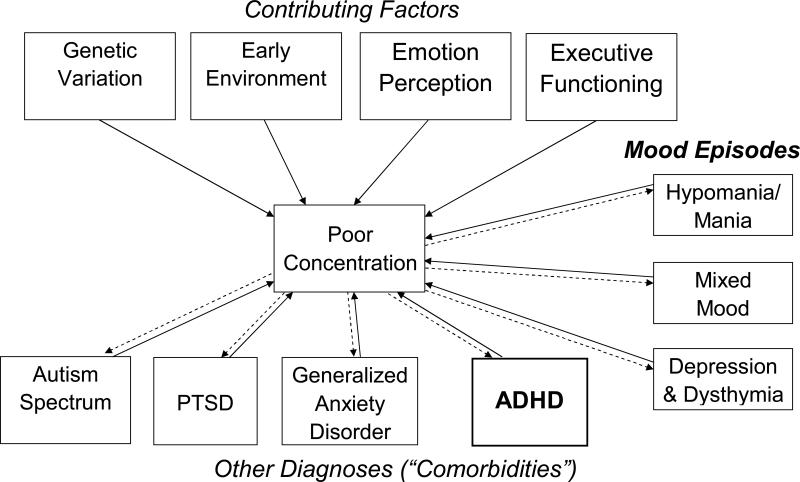
There has been much debate about symptom overlap between ADHD and BPD (Biederman, et al., 1998; Klein, et al., 1998). Data indicate that BPD is a distinct entity, even when eliminating the overlapping items (Kim & Miklowitz, 2002). On the other hand, if the overlapping symptoms of inattention, hyperactivity, impulsiveness, and irritability are eliminated from ADHD, the disorder disappears! This suggests that in a symptom Venn diagram, ADHD could fit entirely within BPD--rather ironic given that ADHD is the more common disorder. The nonspecificity of irritable mood, poor concentration, and high motor activity is notorious: Not only are these symptoms common features of mania and ADHD, but they are also diagnostic symptoms of unipolar depression, generalized anxiety disorder, post-traumatic stress disorder, and oppositional defiant disorder (American Psychiatric Association, 2001); and they are common features of yet more pediatric diagnoses. Figure 2 illustrate this issue using poor concentration as an example. Similarly, impulsiveness, another symptom ADHD and BPD share, is found in numerous other disorders. When a symptom is counted towards more than one diagnosis, it lowers the number of additional symptoms required to pass threshold for the additional diagnosis. Nonspecific symptoms are like “wild cards” that can be used to construct multiple hands, inflating comorbidity if each hand is treated as a separate condition (Youngstrom, 2010). Because it is possible to interpret 4 wild cards as 4 aces, 4 kings, or 4 queens at will, there is some concern that “comorbidity” may just be an overplayed hand. How many true aces are needed to be confident that this hand should be treated as 4 aces rather than 4 queens?
Figure 2.
Interplay between contributing factors, mood states, and other diagnoses in equifinality of “poor concentration.” Dashed lines indicate that poor concentration is part of the diagnostic criteria for the disorder or a common associated symptom. Solid lines indicate probable causal relationships.
(3) Over-Splitting: Artificial Subdivision of Syndromes
There is a long and fruitful debate between “lumpers” who favor diagnostic parsimony versus “splitters” who prefer carefully nuanced clinical description. Over-splitting would create a falsely inflated rate of comorbidity by treating multiple components of the same larger diagnostic entity as separate conditions that frequently co-occur. High rates of comorbidity thus invite questions about whether a nosological system is over-splitting.
Further, a single form of pathology can influence multiple areas of functioning, generating “comorbidities” that are manifestations of a single problem. Diagnosing BPD and ADHD could create artifactual comorbidity if the symptoms actually are expressions of a single underlying process. DSM sometimes provides guidance about this. For example, anxiety disorders should not be diagnosed as “comorbid” with mood disorders unless the anxiety symptoms also occur outside the mood episode. However, the only direction DSM offers for ADHD and mood disorder is criterion E, which states that ADHD should not be diagnosed if the symptoms are better explained by another disorder. Criterion E is often neglected in practice and even in some epidemiological studies, which tend to overdiagnose ADHD. The notion of over-splitting is further reinforced by recent genetic studies identifying relationships between the same single nucleotide polymorphism (e.g., SLC6A3 and SLC6A4; Anderson et al., 2009; Cho et al., 2005; Devlin et al., 2005; Mick et al., 2008; Retz, Thome, Blocher, Baader, & Rosler, 2002; Swanson et al., 2007) or copy number variation (Bijlsma et al., 2009) and different neuropsychiatric conditions or even typical functioning.
(4) Developmental Sequencing
Another possibility is that one disorder may be a developmental precursor of another. This could be considered an example of “heterotypic continuity,” where the same developmental process presents differently at changing ages or social contexts, or requires time and environmental inputs to grow into a fully elaborated form. Cyclothymic disorder and bipolar NOS are logical potential prodromes for bipolar II and bipolar I disorder, as they already involve mood dysregulation. Roughly a third of cases who start with these conditions “progress” to bipolar I or II within three years (Angst et al., 2003; Birmaher et al., 2009; Lewinsohn, Klein, & Seeley, 2000). Others do not show a manic episode, but often have a major depression (Shankman et al., 2009), leaving it uncertain whether the illness is a bipolar depression. Roughly a third of cases also appear to change to a different, nonbipolar diagnosis (Birmaher, et al., 2009; Shankman, et al., 2009). Conversely, cases with other kinds of affective dysregulation that fit less clearly on the bipolar spectrum –such as elevated profiles on the Child Behavior Checklist or having chronic “Severe Mood Dysregulation”--, although highly impaired at follow-up, are unlikely to develop BPD (Brotman et al., 2006; Meyer et al., 2009). This is an artificial form of comorbidity if multiple names are being applied to what is actually a single developmental process.
Some have speculated that ADHD might be a prodrome for bipolar disorder (Tillman & Geller, 2006). Certainly, ADHD symptoms of are also common symptoms of PBD. Epidemiological studies indicate a much earlier age of onset for ADHD, consistent with the possibility of it being a precursor for bipolar disorder. However, longitudinal studies of cohorts with ADHD have found that few cases actually develop bipolar disorder (Galanter et al., 2003; Hazell, Carr, Lewin, & Sly, 2003). Further, many adults with bipolar disorder never had diagnosed ADHD (Galanter & Leibenluft, 2008). Clearly ADHD and PBD are not always different labels for the same condition at varying ages.
(5) Referral or Surveillance Biases
Referral or surveillance biases have had substantial impact on some published findings with regard to PBD. One group's early studies of PBD ascertained cases from an ADHD clinic, with the result that almost 100% of cases with bipolar disorder also met criteria for ADHD (Wozniak, et al., 1995). Subsequent publications have all found lower rates of ADHD in cohorts with PBD (although still quite high), making clear that the high estimate was a consequence of the recruitment pattern, not a product of PBD itself (Kowatch, et al., 2005). There is not strong evidence that rates of “comorbid” ADHD in PBD cases exceed rates of ADHD in nonbipolar cases drawn from the same clinical settings.
Clinical samples also have other potential confounds that could distort our understanding of comorbidity. Clinical samples often underestimate the rate of hypomania, for example, because hypomania does not create enough impairment to motivate treatment seeking. Research with college student samples finds people with recurrent hypomanias but no lifetime history of depression or mania (Alloy et al., 2008; Depue, Krauss, Spoont, & Arbisi, 1989). In fact, it is questionable whether recurrent hypomania without impairment is a disorder, although it might share some of the processes.
Surveillance biases are a major issue in studying PBD. Older research systematically underestimated the rates of hypomania, mania, and mixed episodes in youth, especially when prevailing theory held that these would only begin to manifest in adolescence, much as was the belief with unipolar depression in previous decades (Kovacs, 1989). Conversely, studies of adults with bipolar disorder often failed to formally assess for ADHD because it was assumed to be a pediatric illness (cf. Kessler, Berglund, Demler, Jin, & Walters, 2005; Nierenberg et al., 2005) despite an adult case report as early as 1972 (Arnold, Strobl, & Weisenberg, 1972). Unfortunately, semi-structured and structured interviews provide imperfect insurance against surveillance effects, due to differences in training and conceptualization: Disagreements about mania are high even when clinicians are presented with identical vignettes (Dubicka, Carlson, Vail, & Harrington, 2008) or videotaped interviews (Mackin, Targum, Kalali, Rom, & Young, 2006).
Surveillance bias could also work in the opposite direction, leading to inflated estimates of comorbidity. If clinicians are concerned about the possibility of PBD in cases with ADHD, then better monitoring may contribute to perception of an association between PBD and ADHD. The literature about medication-induced mania may provide the strongest example of this: Elevated rates of mania are found in open studies (where the observer and family know that they are receiving active medication) but not in double-blind studies (Carlson, 2003; Joseph, Youngstrom, & Soares, 2009; Licht, Gijsman, Nolen, & Angst, 2008; Scheffer, Kowatch, Carmody, & Rush, 2005).
Potential “True Comorbidity” Between BPD and ADHD
It also is possible to have “true comorbidity.” Possible mechanisms include (1) overlapping risk factors or common underlying dimensions of cognitive, behavioral, or affective dysfunction, (2) comorbidity creating a distinct, meaningful syndrome, and (3) one disorder increasing risk for the other (Caron & Rutter, 1991). All three probably contribute to the comorbidity between ADHD and PBD.
(1) Overlapping Risk Factors
To date, identified risk factors for bipolar disorder are all non-specific (Tsuchiya, Byrne, & Mortensen, 2003). Several candidate genes for bipolar disorder have been implicated in ADHD, unipolar depression, and schizophrenia, among other conditions (Faraone, Glatt, & Tsuang, 2003). Not surprisingly there is substantial neurocognitive overlap between BPD and ADHD, including deficits in response inhibition, working memory, and other executive functions. Low birth weight, pre- and peri-natal insult, and abuse and trauma all are associated with both mood and attention problems (Hack et al., 2004). Even family history of BPD is not specifically limited to risk of developing PBD: Offspring of a parent with BPD have increased risk of many different poor outcomes, including ADHD (Hodgins, Faucher, Zarac, & Ellenbogen, 2002). The correlation between BPD and ADHD may be the product of each being independently associated with the same underlying third variable – the shared risk factor.
Alternatively, there is evidence of some specificity in risk factors for BPD and ADHD. For example, polymorphisms in genes important for calcium channel function (ex. CACNA1C) have been associated with bipolar disorder (Sklar et al., 2008), but have not yet been implicated in ADHD. Deletions or mutations in CACNA1C may result in episodic neural dysfunction (Gargus, 2009) and provide a molecular basis for the episodic vs. chronic distinction between BPD and ADHD. These possibilities for shared or differentiated genetic mechanisms remain tentative, given the frequent failures to replicate findings in the early stages of development of genetic research in this area. Another limitation of the extant literature is that studies almost always examine cases versus unaffected controls, which cannot identify whether genes are specific to ADHD or bipolar, versus being a shared mechanism.
Additionally, a meta-analysis of neurocognitive functioning in pediatric bipolar disorder identified substantial declines in verbal learning and long-term memory with intact intellectual abilities (Joseph, Frazier, Youngstrom, & Soares, 2008). In contrast, individuals with ADHD show little, if any, verbal memory dysfunction but moderate to large (~9 point) IQ reduction relative to healthy controls. This suggests that the substantial, but incomplete, BPD-ADHD comorbidity may be due to a combination of shared and specific risk factors.
(2) Comorbidity as Distinct Subtype
Comorbidity may also indicate a distinct, meaningful subtype. Some argue that comorbid ADHD may be a characteristic of a pediatric-onset variant of bipolar disorder (Faraone, Biederman, Mennin, Wozniak, & Spencer, 1997). The “comorbid ADHD and bipolar” subtype might be a version that has more chronic course and impairment. However, the symptoms of comorbid ADHD often persist even after mood symptoms have responded to intervention, and then respond well to adjunctive treatment with stimulants (Findling et al., 2005; Scheffer, et al., 2005). The treatment response findings challenge the model that these symptoms are all part of a unitary pediatric subtype and suggest that it might be a “true comorbidity” involving two distinct conditions. Alternatively, differential treatment response may simply reflect targeting different branches on the same tree (Figure 1).
(3) Causal Relationships (Prodrome & Risk Factors)
The third possibility, that ADHD or BPD might create an increased risk of the other condition, is also plausible, although it has yet to be demonstrated in prospective longitudinal studies (cf. Kim-Cohen et al., 2003). Given the typical ages of onset, it is more likely that ADHD might be a risk factor for PBD than the other way around. PBD also may lead to enough behavior problems to technically satisfy criteria for a second disorder, but in this instance the behaviors would be a bipolar-induced “phenocopy” of the other condition. All of the symptoms of ADHD could be observed as part of a hypomanic or manic episode. Figure 2 illustrates how the symptom of poor concentration can be the product of multiple different factors, and how it can be associated with multiple diagnoses. If the only sample of behavior is taken from a manic episode, it would be impossible to tell whether the ADHD symptoms were completely attributable to the mania versus a separate condition. It is unknown whether the mechanisms producing the inattention, hyperactivity, and impulsiveness in mania are identical to the mechanisms underlying ADHD, but the overlap in risk factors and some aspects of neurocognitive functioning (Joseph, Frazier, Youngstrom, & Soares, 2008) could be consistent with shared processes. ADHD also could lead to greater family conflict, increased stress through disrupted peer and academic functioning, and increased substance use, with each factor mediating the increased risk for development of BPD.
Deciding Which Is “Primary”
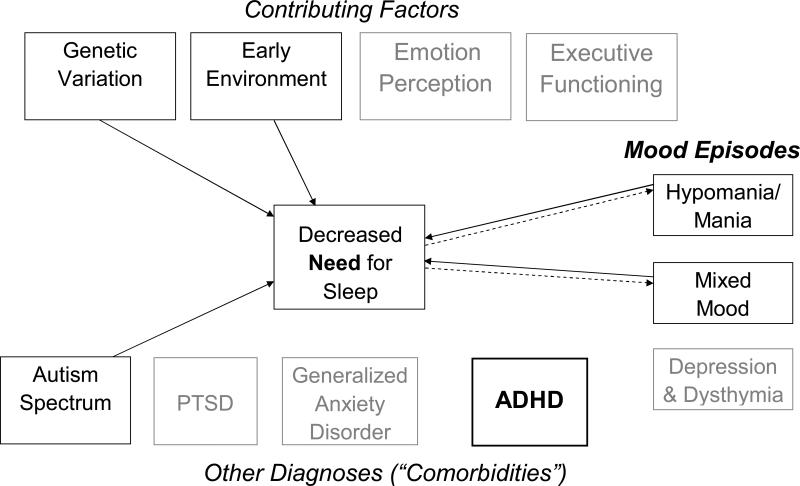
Because there are no symptoms unique to ADHD, there are two main strategies to disentangle the diagnoses. One is to focus on symptoms that are more specific to mania, such as elated mood, grandiosity and unstable self esteem, or decreased need for sleep (as distinct from restless sleep or insomnia; see Figure 3) and possibly including neurocognitive deficits that are more specific to bipolar disorder, such as verbal learning and memory (Joseph, et al., 2008; Kaplan, Dewey, Crawford, & Fisher, 1998). The other strategy is to assess the course of the symptoms: A more episodic presentation is suggestive of a mood disorder, and a more chronically persistent presentation suggests ADHD. Putting these strategies together, chronically persistent inattention, distractibility, hyperactivity, and impulsiveness without high-specificity, non-overlapping symptoms of mania or episodic exacerbations is “pure” ADHD, whereas episodic symptoms that include high-specificity symptoms constitute mania. Chronic hyperactivity, impulsiveness, and attention problems with episodic exacerbation would be consistent with comorbid PBD superimposed on ADHD (Youngstrom, Birmaher, & Findling, 2008).
Figure 3.
Interplay between contributing factors, mood states, and other diagnoses in equifinality of “decreased need for sleep.” Decreased need for sleep, with high levels of energy, is distinct from difficulty falling asleep or insomnia – which would not be specific to bipolar disorder and which would show relationship with all of the disorders listed below. Dashed lines indicate that decreased need for sleep is part of the diagnostic criteria for the disorder. Solid lines indicate probable causal relationships.
How do clinicians or researchers decide which diagnosis is “primary” when both could be coded as present? The term “primary” can connote which came first developmentally, which is worst in terms of severity, which causes the other (as in the third model of true comorbidity, above), or which brings the youngster to clinical attention. In most cases of true comorbidity, classifying the BPD as primary is consistent with the usual comparative severity, alerts the clinician and family to be vigilant for episodes, and expedites the treatment plan (and with some insurance plans, may facilitate coverage).
Implications for Research and Practice
Because all ADHD symptoms can also be BPD symptoms, both investigators and clinicians need to pay great attention to ADHD Criterion E, the exclusionary criterion, that the symptoms are not better accounted for by another disorder. A convenient rule of thumb is that the symptoms do not exclusively occur during another disorder, such as during manic episodes –the chronic vs. episodic rule. Implementation of criterion E requires a complete psychiatric history and mental status exam, which may uncover non-overlapping symptoms as well as delineate the time course of the common symptoms. Paradoxically, a mental status exam cannot be used to diagnose ADHD because of most children's lack of insight about their own inattentiveness/distractibility/impulsivity/hyperactivity and the fact that they may not show it in a novel 1:1 situation; but ADHD can often be excluded by mental status exam. This issue needs more investigation by primary medical practitioners and probably in epidemiologic studies.
When both ADHD and BPD are diagnosed together, it is usually clinically useful to consider the BPD the initial and primary target of treatment even if the ADHD came first chronologically for two reasons: (a) the greater severity and more sinister prognosis of BPD; and (b) the risk that medications for ADHD may exacerbate bipolar symptoms if the patient is not first “covered” by a mood stabilizer. In some cases there may be only symptoms of ADHD with no non-overlapping symptoms, but the symptoms are of such intensity that the clinician suspects they may constitute a prodrome of BPD, especially with a family history of BPD. In that case, it is acceptable to first treat the ADHD (possibly considering a nonstimulant medicaton rather than stimulant), but inform the family, monitor very closely for breakthrough of mania, and be prepared to institute a mood stabilizer emergently. The MTA results suggest that most such cases do not have an adverse reaction to ADHD medication (Galanter, et al., 2003). In such cases behavioral treatment will be especially important both for containing behavioral symptoms and for reducing the dose of ADHD medication needed for optimal results (MTA Cooperative Group, 1999).
References
- Alloy LB, Abramson LY, Walshaw PD, Cogswell A, Grandin LD, Hughes ME, et al. Behavioral approach system and behavioral inhibition system sensitivities and bipolar spectrum disorders: Prospective prediction of bipolar mood episodes. Bipolar Disorders. 2008;10:310–322. doi: 10.1111/j.1399-5618.2007.00547.x. [DOI] [PubMed] [Google Scholar]
- American Psychiatric Association . Diagnostic and statistical manual of mental disorders. 4th--Text Revision ed. Author; Washington, DC: 2001. [Google Scholar]
- Anderson BM, Schnetz-Boutaud NC, Bartlett J, Wotawa AM, Wright HH, Abramson RK, et al. Examination of association of genes in the serotonin system to autism. Neurogenetics. 2009 doi: 10.1007/s10048-009-0171-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Angold A, Costello EJ, Erkanli A. Comorbidity. Journal of Child Psychology and Psychiatry. 1999;40:57–87. [PubMed] [Google Scholar]
- Angst J, Gamma A, Benazzi F, Ajdacic V, Eich D, Rossler W. Toward a re-definition of subthreshold bipolarity: epidemiology and proposed criteria for bipolar-II, minor bipolar disorders and hypomania. Journal of Affective Disorders. 2003;73:133–146. doi: 10.1016/s0165-0327(02)00322-1. [DOI] [PubMed] [Google Scholar]
- Arnold LE, Strobl D, Weisenberg A. Hyperkinetic adult. Study of the “paradoxical” amphetamine response. JAMA. 1972;222:693–694. doi: 10.1001/jama.222.6.693. [DOI] [PubMed] [Google Scholar]
- Berkson J. Limitations of the application of fourfold tables to hospital data. Biometrics Bulletin. 1946;2:47–53. [PubMed] [Google Scholar]
- Biederman J, Klein RG, Pine DS, Klein DF. Resolved: Mania is mistaken for ADHD in prepubertal children. Journal of the American Academy of Child & Adolescent Psychiatry. 1998;37:1091–1093. doi: 10.1097/00004583-199810000-00020. [DOI] [PubMed] [Google Scholar]
- Bijlsma EK, Gijsbers AC, Schuurs-Hoeijmakers JH, van Haeringen A, Fransen van de Putte DE, Anderlid BM, et al. Extending the phenotype of recurrent rearrangements of 16p11.2: deletions in mentally retarded patients without autism and in normal individuals. Eur J Med Genet. 2009;52:77–87. doi: 10.1016/j.ejmg.2009.03.006. [DOI] [PubMed] [Google Scholar]
- Birmaher B, Axelson D, Goldstein B, Strober M, Gill MK, Hunt J, et al. Four-Year Longitudinal Course of Children and Adolescents With Bipolar Spectrum Disorders: The Course and Outcome of Bipolar Youth (COBY) Study. American Journal of Psychiatry. 2009 doi: 10.1176/appi.ajp.2009.08101569. appi.ajp.2009.08101569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brotman MA, Schmajuk M, Rich BA, Dickstein DP, Guyer AE, Costello EJ, et al. Prevalence, Clinical Correlates, and Longitudinal Course of Severe Mood Dysregulation in Children. Biological Psychiatry. 2006;60:991–997. doi: 10.1016/j.biopsych.2006.08.042. [DOI] [PubMed] [Google Scholar]
- Carlson GA. The bottom line. Journal of Child and Adolescent Psychopharmacology. 2003;13:115–118. doi: 10.1089/104454603322163826. [DOI] [PubMed] [Google Scholar]
- Caron C, Rutter M. Comorbidity in child psychopathology: Concepts, issues and research strategies. Journal of Child Psychology and Psychiatry. 1991;32:1063–1080. doi: 10.1111/j.1469-7610.1991.tb00350.x. [DOI] [PubMed] [Google Scholar]
- Cho HJ, Meira-Lima I, Cordeiro Q, Michelon L, Sham P, Vallada H, et al. Population-based and family-based studies on the serotonin transporter gene polymorphisms and bipolar disorder: a systematic review and meta-analysis. Molecular Psychiatry. 2005;10(8):771–781. doi: 10.1038/sj.mp.4001663. [DOI] [PubMed] [Google Scholar]
- Depue RA, Krauss S, Spoont MR, Arbisi P. General Behavior Inventory identification of unipolar and bipolar affective conditions in a nonclinical university population. Journal of Abnormal Psychology. 1989;98(2):117–126. doi: 10.1037//0021-843x.98.2.117. [DOI] [PubMed] [Google Scholar]
- Devlin B, Cook EH, Jr., Coon H, Dawson G, Grigorenko EL, McMahon W, et al. Autism and the serotonin transporter: the long and short of it. Molecular Psychiatry. 2005;10(12):1110–1116. doi: 10.1038/sj.mp.4001724. [DOI] [PubMed] [Google Scholar]
- Dubicka B, Carlson GA, Vail A, Harrington R. Prepubertal mania: diagnostic differences between US and UK clinicians. European child & adolescent psychiatry. 2008;17(3):153–161. doi: 10.1007/s00787-007-0649-5. [DOI] [PubMed] [Google Scholar]
- Faraone SV, Biederman J, Mennin D, Wozniak J, Spencer T. Attention-deficit hyperactivity disorder with bipolar disorder: A familial subtype? Journal of the American Academy of Child & Adolescent Psychiatry. 1997;36:1378–1387. doi: 10.1097/00004583-199710000-00020. [DOI] [PubMed] [Google Scholar]
- Faraone SV, Glatt SJ, Tsuang MT. The genetics of pediatric-onset bipolar disorder. Biological Psychiatry. 2003;53:970–977. doi: 10.1016/s0006-3223(02)01893-0. [DOI] [PubMed] [Google Scholar]
- Findling RL, McNamara NK, Stansbrey RJ, Gracious BL, Whipkey RE, Demeter CA, et al. Combination lithium and divalproex sodium in pediatric bipolar symptom re-stabilization. Journal of the American Academy of Child & Adolescent Psychiatry. 2005 doi: 10.1097/01.chi.0000189135.05060.8a. [DOI] [PubMed] [Google Scholar]
- Frazier TW, Youngstrom EA, Naugle RI. The Latent Structure of Attention-Deficit/Hyperactivity Disorder in a Clinic-Referred Sample. Neuropsychology. 2007;21:45–64. doi: 10.1037/0894-4105.21.1.45. [DOI] [PubMed] [Google Scholar]
- Galanter C, Carlson G, Jensen P, Greenhill L, Davies M, Li W, et al. Response to Methylphenidate in children with Attention Deficit Hyperactivity Disorder and Manic Symptoms in the Multimodal Treatment Study of children with Attention Deficit Hyperactivity Disorder Titration Trial. Journal of Child and Adolescent Psychopharmacology. 2003;13:123–136. doi: 10.1089/104454603322163844. [DOI] [PubMed] [Google Scholar]
- Galanter CA, Leibenluft E. Frontiers between attention deficit hyperactivity disorder and bipolar disorder. Child and adolescent psychiatric clinics of North America. 2008;17:325–346. doi: 10.1016/j.chc.2007.11.001. [DOI] [PubMed] [Google Scholar]
- Gargus JJ. Genetic calcium signaling abnormalities in the central nervous system: seizures, migraine, and autism. Annals of the New York Academy of Sciences. 2009;1151:133–156. doi: 10.1111/j.1749-6632.2008.03572.x. [DOI] [PubMed] [Google Scholar]
- Hack M, Youngstrom EA, Cartar L, Schluchter M, Gerry TH, Flannery D, et al. Behavioral outcomes and evidence of psychopathology among very low birth weight infants at age 20 years. Pediatrics. 2004;114:932–940. doi: 10.1542/peds.2003-1017-L. [DOI] [PubMed] [Google Scholar]
- Haslam N, Williams B, Prior M, Haslam R, Graetz B, Sawyer M. The latent structure of attention-deficit/hyperactivity disorder: a taxometric analysis. Australian and New Zealand, Journal of Psychiatry. 2006;40:639–647. doi: 10.1080/j.1440-1614.2006.01863.x. [DOI] [PubMed] [Google Scholar]
- Hazell PL, Carr V, Lewin TJ, Sly K. Manic symptoms in young males with ADHD predict functioning but not diagnosis after 6 years. Journal of the American Academy of Child & Adolescent Psychiatry. 2003;42(5):552–560. doi: 10.1097/01.CHI.0000046830.95464.33. [DOI] [PubMed] [Google Scholar]
- Hodgins S, Faucher B, Zarac A, Ellenbogen M. Children of parents with bipolar disorder. A population at high risk for major affective disorders. Child & Adolescent Psychiatric Clinics of North America. 2002;11(3):533–553. doi: 10.1016/s1056-4993(02)00002-0. [DOI] [PubMed] [Google Scholar]
- Hurtig T, Ebeling H, Taanila A, Miettunen J, Smalley S, McGough J, et al. ADHD and comorbid disorders in relation to family environment and symptom severity. Eur Child Adolesc Psychiatry. 2007;16(6):362–369. doi: 10.1007/s00787-007-0607-2. [DOI] [PubMed] [Google Scholar]
- Joseph M, Frazier TW, Youngstrom EA, Soares JC. A quantitative and qualitative review of neurocognitive performance in pediatric bipolar disorder. Journal of Child & Adolescent Psychopharmacology. 2008;18:595–605. doi: 10.1089/cap.2008.064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Joseph M, Youngstrom EA, Soares JC. Antidepressant-Coincident Mania in Children and Adolescents Treated with Selective Serotonin Reuptake Inhibitors. Future Neurology. 2009;4(1):87–102. doi: 10.2217/14796708.4.1.87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Joseph MF, Frazier TW, Youngstrom EA, Soares JC. A quantitative and qualitative review of neurocognitive performance in pediatric bipolar disorder. Journal of Child and Adolescent Psychopharmacology. 2008;18(6):595–605. doi: 10.1089/cap.2008.064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kaplan BJ, Dewey D, Crawford SG, Fisher GC. Deficits in long- term memory are not characteristic of ADHD. Journal of Clinical and Experimental Neuropsychology. 1998;20(4):518–528. doi: 10.1076/jcen.20.4.518.1477. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Berglund P, Demler O, Jin R, Walters EE. Lifetime Prevalence and Age-of-Onset Distributions of DSM-IV Disorders in the National Comorbidity Survey Replication. Archives of General Psychiatry. 2005;62:593–602. doi: 10.1001/archpsyc.62.6.593. [DOI] [PubMed] [Google Scholar]
- Kim-Cohen J, Caspi A, Moffitt TE, Harrington H, Milne BJ, Poulton R. Prior Juvenile Diagnoses in Adults With Mental Disorder: Developmental Follow-Back of a Prospective-Longitudinal Cohort. Archives of General Psychiatry. 2003;60:709–717. doi: 10.1001/archpsyc.60.7.709. [DOI] [PubMed] [Google Scholar]
- Kim EY, Miklowitz DJ. Childhood mania, attention deficit hyperactivity disorder and conduct disorder: a critical review of diagnostic dilemmas. Bipolar Disorders. 2002;4:215–225. doi: 10.1034/j.1399-5618.2002.01191.x. [DOI] [PubMed] [Google Scholar]
- Klein RG, Pine DS, Klein DF. Resolved: Mania is mistaken for ADHD in prepubertal children. Journal of the American Academy of Child & Adolescent Psychiatry. 1998;37:1093–1096. doi: 10.1097/00004583-199810000-00020. [DOI] [PubMed] [Google Scholar]
- Kovacs M. Affective disorders in children and adolescents. Special Issue: Children and their development: Knowledge base, research agenda, and social policy application. American Psychologist. 1989;44:209–215. [PubMed] [Google Scholar]
- Kowatch RA, Youngstrom EA, Danielyan A, Findling RL. Review and meta-analysis of the phenomenology and clinical characteristics of mania in children and adolescents. Bipolar Disorders. 2005;7:483–496. doi: 10.1111/j.1399-5618.2005.00261.x. [DOI] [PubMed] [Google Scholar]
- Lewinsohn PM, Klein DN, Seeley J. Bipolar disorder during adolescence and young adulthood in a community sample. Bipolar Disorders. 2000;2:281–293. doi: 10.1034/j.1399-5618.2000.20309.x. [DOI] [PubMed] [Google Scholar]
- Licht RW, Gijsman H, Nolen WA, Angst J. Are antidepressants safe in the treatment of bipolar depression? A critical evaluation of their potential risk to induce switch into mania or cycle acceleration. Acta Psychiatr Scand. 2008;118:337–346. doi: 10.1111/j.1600-0447.2008.01237.x. [DOI] [PubMed] [Google Scholar]
- Mackin P, Targum SD, Kalali A, Rom D, Young AH. Culture and assessment of manic symptoms. British Journal of Psychiatry. 2006;189:379–380. doi: 10.1192/bjp.bp.105.013920. [DOI] [PubMed] [Google Scholar]
- Meyer SE, Carlson GA, Youngstrom E, Ronsaville DS, Martinez PE, Gold PW, et al. Long-term outcomes of youth who manifested the CBCL-Pediatric Bipolar Disorder phenotype during childhood and/or adolescence. Journal of Affective Disorders. 2009;113:227–235. doi: 10.1016/j.jad.2008.05.024. [DOI] [PubMed] [Google Scholar]
- Mick E, Kim JW, Biederman J, Wozniak J, Wilens T, Spencer T, et al. Family based association study of pediatric bipolar disorder and the dopamine transporter gene (SLC6A3). Am J Med Genet B Neuropsychiatr Genet. 2008;147B:1182–1185. doi: 10.1002/ajmg.b.30745. [DOI] [PubMed] [Google Scholar]
- MTA Cooperative Group 14-Month randomized clinical trial of treatment strategies for attention-deficit/hyperactivity disorder. Archives of General Psychiatry. 1999 Dec;56:1073–1086. doi: 10.1001/archpsyc.56.12.1073. [DOI] [PubMed] [Google Scholar]
- Nierenberg AA, Miyahara S, Spencer T, Wisniewski SR, Otto MW, Simon N, et al. Clinical and diagnostic implications of lifetime attention-deficit/hyperactivity disorder comorbidity in adults with bipolar disorder: data from the first 1000 STEP-BD participants. Biological Psychiatry. 2005;57:1467–1473. doi: 10.1016/j.biopsych.2005.01.036. [DOI] [PubMed] [Google Scholar]
- Retz W, Thome J, Blocher D, Baader M, Rosler M. Association of attention deficit hyperactivity disorder-related psychopathology and personality traits with the serotonin transporter promoter region polymorphism. Neuroscience Letters. 2002;319(3):133–136. doi: 10.1016/s0304-3940(01)02575-7. [DOI] [PubMed] [Google Scholar]
- Scheffer RE, Kowatch RA, Carmody T, Rush AJ. Randomized, placebo-controlled trial of mixed amphetamine salts for symptoms of comorbid ADHD in pediatric bipolar disorder after mood stabilization with divalproex sodium. The American Journal of Psychiatry. 2005;162(1):58–64. doi: 10.1176/appi.ajp.162.1.58. [DOI] [PubMed] [Google Scholar]
- Shankman SA, Lewinsohn PM, Klein DN, Small JW, Seeley JR, Altman SE. Subthreshold conditions as precursors for full syndrome disorders: a 15-year longitudinal study of multiple diagnostic classes. Journal of child psychology and psychiatry, and allied disciplines. 2009 doi: 10.1111/j.1469-7610.2009.02117.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sklar P, Smoller JW, Fan J, Ferreira MA, Perlis RH, Chambert K, et al. Whole-genome association study of bipolar disorder. Molecular Psychiatry. 2008;13(6):558–569. doi: 10.1038/sj.mp.4002151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith BH, Barkley RA, Shapiro CJ. Attention-Deficit/Hyperactivity Disorder. In: Mash EJ, Barkley RA, editors. Assessment of Childhood Disorders. 4 ed. Guilford Press; New York: 2007. pp. 53–131. [Google Scholar]
- Swanson JM, Kinsbourne M, Nigg J, Lanphear B, Stefanatos GA, Volkow N, et al. Etiologic subtypes of attention-deficit/hyperactivity disorder: brain imaging, molecular genetic and environmental factors and the dopamine hypothesis. Neuropsychology Review. 2007;17(1):39–59. doi: 10.1007/s11065-007-9019-9. [DOI] [PubMed] [Google Scholar]
- Tillman R, Geller B. Controlled study of switching from attention-deficit/hyperactivity disorder to a prepubertal and early adolescent bipolar I disorder phenotype during 6-year prospective follow-up: Rate, risk, and predictors. Development and Psychopathology. 2006;18(04):1037–1053. doi: 10.1017/S0954579406060512. [DOI] [PubMed] [Google Scholar]
- Tsuchiya KJ, Byrne M, Mortensen PB. Risk factors in relation to an emergence of bipolar disorder: A systematic review. Bipolar Disorders. 2003;5(4):231–242. doi: 10.1034/j.1399-5618.2003.00038.x. [DOI] [PubMed] [Google Scholar]
- Wozniak J, Biederman J, Kiely K, Ablon JS, Faraone S, Mundy E, et al. Mania-like symptoms suggestive of childhood-onset bipolar disorder in clinically referred children. Journal of the American Academy of Child & Adolescent Psychiatry. 1995;34:867–876. doi: 10.1097/00004583-199507000-00010. [DOI] [PubMed] [Google Scholar]
- Youngstrom EA. Definitional issues in bipolar disorder across the life cycle. Clinical Psychology: Science & Practice. 2009;16:140–160. [Google Scholar]
- Youngstrom EA. A developmental psychopathology perspective on the assessment and diagnosis of bipolar disorder. In: Miklowitz D, Cicchetti D, editors. Bipolar Disorder: A Developmental Psychopathology Approach. Guilford Press; New York: 2010. [Google Scholar]
- Youngstrom EA, Birmaher B, Findling RL. Pediatric bipolar disorder: Validity, phenomenology, and recommendations for diagnosis. Bipolar Disorders. 2008;10:194–214. doi: 10.1111/j.1399-5618.2007.00563.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Youngstrom EA, Findling RL, Calabrese JR. Who are the comorbid adolescents? Agreement between psychiatric diagnosis, parent, teacher, and youth report. Journal of Abnormal Child Psychology, Special section on comorbidity. 2003;31:231–245. doi: 10.1023/a:1023244512119. [DOI] [PubMed] [Google Scholar]