Abstract
The present report highlights the possible adverse effects of doxylamine, a common over the counter sleep aid. Doxylamine is an antihistamine that at toxic doses can cause anticholinergic effects, including seizures, rhabdomyolysis and death. The following case describes a patient with doxylamine toxicity who presented with seizure and confusion. Our patient was managed symptomatically, and remained otherwise stable throughout his hospitalisation. This case is atypical in terms of a delayed rhabdomyolysis and a false positive urine drug screen test for methadone. There is evidence that doxylamine at toxic levels can lead to false positives for methadone and phencyclidine testing using immunoassay-based urine drug screen kits. Urine drug screen testing on patients who are hospitalised is typically performed using immunoassays. However, in certain cases confirmatory secondary testing may be required. Doxylamine is prone to abuse and knowledge of the clinical presentation of its toxicity and the management of acute overdose can be life-saving.
BACKGROUND
The present report describes a case of doxylamine (Unisom) toxicity as part of a suicide attempt. We describe here the toxicities involved due to doxylamine overdose. In particular we highlight that a delayed rhabdomyloysis can occur in such patients and that false positive testing for methadone can occur using immunoassay urine drug screen testing. The intention is to remind clinicians of the potential toxicities ascribed to what may often be considered a benign over the counter drug and that confirmatory testing is warranted in light of positive urine drug screen testing.
CASE PRESENTATION
In July 2008, a healthy 36-year-old Portuguese man presented to our emergency department (ED) 45 min after consuming 96 25 mg tablets of doxylamine as part of a suicide attempt. On presentation, he was diaphoretic, warm to touch with a reduced level of consciousness. His general physical examination was otherwise normal with no significant neurological deficits except for an initial Glasgow Coma Scale (GCS) score of 9. While in the ED he suffered a brief grand mal seizure, which terminated spontaneously. Thereafter he became tachycardic (120 beats/min) and somewhat agitated. CT scan of the head, chest radiographs and ECG were all unremarkable. The patient was treated with gastric lavage, activated charcoal and supportive care. His urine drug screen was positive for methadone. The remainder of his laboratory studies were unremarkable. Initial serum creatine phosphokinase (CPK) was 153 U/litre (38–174 U/litre), with a myoglobin of 23.3 mg/dl (17.4–105 ng/ml). However, after 24 h CPK levels began rising sharply (3917 U/litre) reaching a peak of 9432 U/litre by the fourth day. Serum myoglobin rose to 500.3 ng/ml and serum aldolase to 92.3 U/litre on the second and fourth day, respectively. Additionally, testing for HIV, hepatitis, thyroid dysfunction, autoimmune and inflammatory disorders were all negative. An EEG was also unremarkable. During his entire hospital course the patient showed no signs or symptoms of muscle weakness, tenderness or rashes and his renal function remained normal throughout. Upon further questioning the patient vehemently denied any alcohol or other illicit drug abuse. The patient was aggressively hydrated and after the fifth hospital day his CPK level started returning to normal, whereupon he was transferred to a psychiatric unit for inpatient management of severe depression with suicidal ideations.
DISCUSSION
Doxylamine is a member of the ethanolaime class of antihistamines, available as an over the counter sleep aid. Doxylamine has a half life of roughly 10 h and is metabolised by the liver into N-demethyl doxylamine and N,N-didemethyl doxylamine.1,2 While considered benign, drug overdose can lead to toxicity with antihistaminergic/anticholenergic effects. Doxylamine, like other antihistamines, competitively inhibits histamine at the H1 receptor and also has anticholinergic effects. There have reports of doxylamine toxicity causing seizures, rhabdomyolysis and anticholinergic effects, including tachycardia, flushing, mydriasis, confusion and hypertension.3–5 There appears to be no correlation between the plasma level of doxylamine and its toxic clinical sequelae.4 The majority of patients with doxylamine toxicity who present with anticholinergic symptoms also have acutely elevated CPK levels.3–5 Here we present a case of delayed elevation of CPK levels with a false positive urine methadone drug screen.
It has been suggested that antihistamines cause a direct toxic effect on striated muscle by injuring the sarcolemma, thereby causing an influx of sodium. A higher intracellular sodium concentration activates Na/K ATPase, thereby depleting cellular ATP. Increased intracellular sodium also leads to higher intracellular calcium levels which can then activate proteolytic enzymes.6 The combined depletion of ATP and activated intracellular enzymes leads to myocyte injury, rhabdomyolysis and release of muscle enzymes such as CPK and myoglobin.6 Treatment involves aggressive hydration with monitoring of serum electrolytes and renal function. Seizures due to anticholinergic effects can be treated with diazepam, followed by phenytoin and phenobarbital, as needed.4 The cautious use of physostigmine, the acetylcholinesterase inhibitor, has been suggested for severe refractory delirium unresponsive to high doses of benzodiazepines, resistant seizures and haemodynamically unstable and resistant narrow complex supraventricular arrhythmias.7 Our patient’s acute symptoms may have been due to an initial peak of doxylamine in the plasma (2.4 h) while the delayed rise in CPK may be explained by the drug’s prolonged elimination half life (10.1 h).1 However, daily monitoring of doxylamine and its metabolites in the plasma would be needed to support such a hypothesis. Nonetheless, delayed muscle toxicity has been reported after overdose with other drugs (eg, venlafaxine and olanzapine).8,9
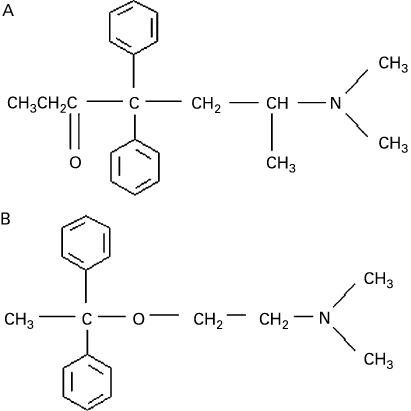
Drug screening on patients who are hospitalised is typically performed on urine specimens using immunoassays. Confirmatory testing usually involves either gas chromatography or mass spectrometry.10 Assays for methadone are specific and detect the parent compound as only about a third of the drug is excreted unchanged.10 Furthermore, doxylamine is excreted as the unchanged drug and two N-demethylated products (N-demethyl doxylamine and N,N-didemethyl doxylamine).2 There is evidence that doxylamine at toxic levels can lead to false positive methadone2,11 and phencyclidine12 results using immunoassay-based urine drug screen kits. It seems likely that our patient’s doxylamine level was elevated enough to give such a false positive result, which may be attributed to the similarity between parent compounds (fig 1).
Figure 1.
Chemical structure of methadone (A) and doxylamine (B).
Doxylamine, like other drugs available over the counter, is prone to abuse and is often employed during suicide attempts. Knowledge of the clinical presentation of doxylamine toxicity and the management of acute overdose can aid the clinician in terms of treatment. Knowing that doxylamine at toxic levels can give false positive results on routine urine drug screening and that confirmatory testing may be in required can also be of clinical value.
LEARNING POINTS
Doxylamine is an over the counter sleep aid with anticholinergic side effects when taken at toxic doses that can lead to seizures, rhabdomylosis, including a delayed rhabdomyloysis, and potentially death.
Doxylamine-induced seizures can be treated with benzodiazepines and rhabdomylosis treated with aggressive hydration.
Urine drug screen testing using immunoassay kits can give false positive methadone and phencyclidine tests in patients with doxylamine toxicity. In certain clinical settings positive drug screen testing should be confirmed using either gas chromatography or mass spectrometry confirmatory tests.
Footnotes
Competing interests: None.
Patient consent: Patient/guardian consent was obtained for publication.
REFERENCES
- 1.Friedman H, Greenblatt DJ. The pharmacokinetics of doxylamine: use of automated gas chromatography with nitrogen-phosphorus. J Clin Pharmacol 1985; 25: 448–51 [DOI] [PubMed] [Google Scholar]
- 2.Gielsdorf W, Schubert K. Biotransformation of doxylamine: isolation, identification and synthesis of some metabolites. J Clin Chem Clin Biochem 1981; 19: 485–90 [PubMed] [Google Scholar]
- 3.Soto LF, Miller CH, Ognibere AJ. Severe rhabdomyolysis after doxylamine overdose. Postgrad Med 1993; 93: 227–9 [DOI] [PubMed] [Google Scholar]
- 4.Köppel C, Tenczer J, Ibe K. Poisoning with over-the-counter doxylamine preparations: an evaluation of 109 cases. Hum Toxicol 1987; 6: 355–9 [DOI] [PubMed] [Google Scholar]
- 5.Khosla U, Ruel KS, Hunt DP. Antihistamine-induced rhabdomyolysis. South Med J 2003; 96: 1023–6 [DOI] [PubMed] [Google Scholar]
- 6.Larbi EB. Drug induced rhabdomyolysis. Ann Saudi Med 1998; 18: 525–30 [DOI] [PubMed] [Google Scholar]
- 7.McCann DJ, Roth B. Toxicity, antihistamine. eMed J. http://www.emedicine.com/EMERG/topic38.htm (accessed 26 July 2008) [Google Scholar]
- 8.Wilson AD, Howell C, Waring WS. Venlafaxine ingestion is associated with rhabdomyolysis in adults: a case series. J Toxicol Sci 2007; 32: 97–101 [DOI] [PubMed] [Google Scholar]
- 9.Waring WS, Wrate J, Bateman DN. Olanzapine overdose is associated with acute muscle toxicity. Hum Exp Toxicol 2006; 25: 735–40 [DOI] [PubMed] [Google Scholar]
- 10.Moeller KE, Lee KC, Kissack JC. Urine drug screening: practical guide for clinicians (review). Mayo Clin Proc 2008; 83: 66–76 [DOI] [PubMed] [Google Scholar]
- 11.Hausmann E, Kohl B, von Boehmer H, et al. False-positive EMIT indication of opiates and methadone in a doxylamine intoxication. J Clin Chem Clin Biochem 1983; 21: 599–600 [PubMed] [Google Scholar]
- 12.Levine BS, Smith ML.Effects of diphenhydramine on immunoassays of phencyclidine in urine. Clin Chem 1990; 36:1258. [PubMed] [Google Scholar]