Abstract
Emphysematous pyelonephritis (EPN) is a rare but life-threatening acute suppurative infection of the kidney, characterised by production of gas within the renal parenchyma, collecting system or perirenal tissue. It has a high mortality rate (70% to 90%), and the majority of patients have diabetes mellitus. The left kidney is most common involved and Escherichia coli is the most common pathogen. EPN complicated with pneumomediastinum (PM) has been reported in only four cases previously. Here, a case of PM as first manifestation of EPN in a non-diabetic 81-year-old man is reported. He had experienced back pain and abdominal fullness for 1 week. A plain radiograph, CT aortography and MRI confirmed the diagnosis of EPN complicated with PM. The patient died on the 22nd day of treatment with antibiotics of cefmetazole, gentamycin and metronidazole.
BACKGROUND
Pneumomediastinum (PM), a collection of mediastinal air, often results from the rupture of intrathoracic structures. Emphysematous pyelonephritis (EPN) is a rare but life-threatening acute suppurative infection of the kidney characterised by production of gas within the renal parenchyma, collecting system or perirenal tissue. Anatomically, the retroperitoneum, mediastinum, back and neck are linked by fascial planes, allowing air migration by pressure gradient. PM as a presentation in retroperitoneal infection has been reported in only four cases previously. We report a case of PM as the first manifestation of EPN in a non-diabetic 81-year-old man.
CASE PRESENTATION
An 81-year-old man with a history of hypertension and coronary artery disease, receiving angioplasty under regular medication, presented to our institution having experienced back pain and abdominal fullness for 1 week. Physical examination was unremarkable. Laboratory test evaluation revealed white blood cell counts of 22 200 cells/mm3 with 91.3% segmented neutrophils, haemoglobin 9.4 g/dl, platelet counts 110×103/mm3, blood urea nitrogen 78 mg/dl, creatinine 3.4 mg/dl, glucose 93 mg/dl, lactate 15.7 mg/dl (normal <12), albumin 1.9 g/dl (normal range 3.5–5.0 g/dl), total protein 4.9 g/dl (normal range 6.0–8.0 g/dl), C-reactive protein 36.6 mg/dl (normal level <0.4 g/dl) and lactate dehydrogenase 382 U/litre (normal range 120–240 U/litre). Plain radiographs of thoracic and lumbar spines revealed PM and air along the abdominal aorta over the prevertebral regions (fig 1). CT aortography with intravenous contrast media displayed multifoci of air bubbles within the parenchyma of non-enhanced left kidney, extending to the hilum and abdominal aorta, and ascending to the thoracic aorta and distal aortic arch (fig 2). MRI of thoracic and lumbar spines showed multifoci of air bubbles along the thoracic and abdominal aorta in T1-weighted and T2-weighted images, and periaortic regions (fig 3). Radiological pictures were compatible with EPN complicated with PM. A consulted urologist suggested surgical intervention, but the patient’s family did not consent to the procedure due to the patient’s age and the high risk from surgery. Intravenous antibiotics with cefmetazole, gentamycin and metronidazole were prescribed for infection control, but the patient died on the 22nd day.
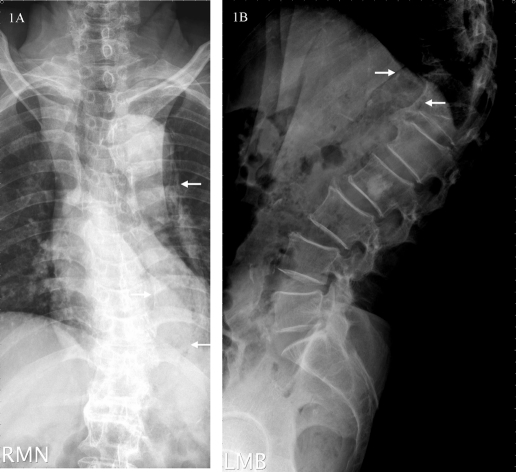
Figure 1.
Plain radiographs of thoracic and lumbar spines demonstrating pneumomediastinum (arrow in (A)) and air along the abdominal aorta over prevertebral regions (arrow in (B)).
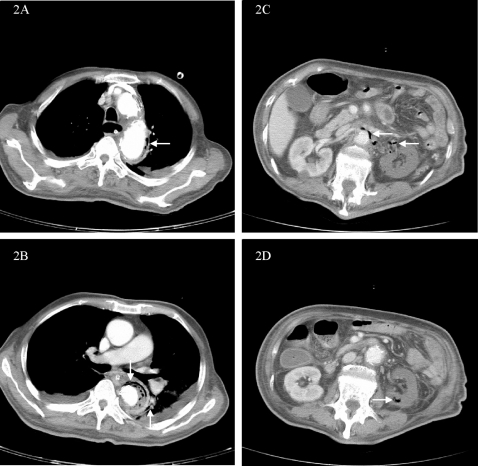
Figure 2.
CT scan of the aorta with intravenous contrast showing multifoci of air bubbles surrounding the distal aortic arch (arrow in (A)), thoracic aorta and mediastinum (arrow in (B)) and abdominal aorta (arrow in (C)), extending from the left renal hilum (arrow in (C)) and air bubbles within the parenchyma of non-enhanced left kidney (arrow in (D)).
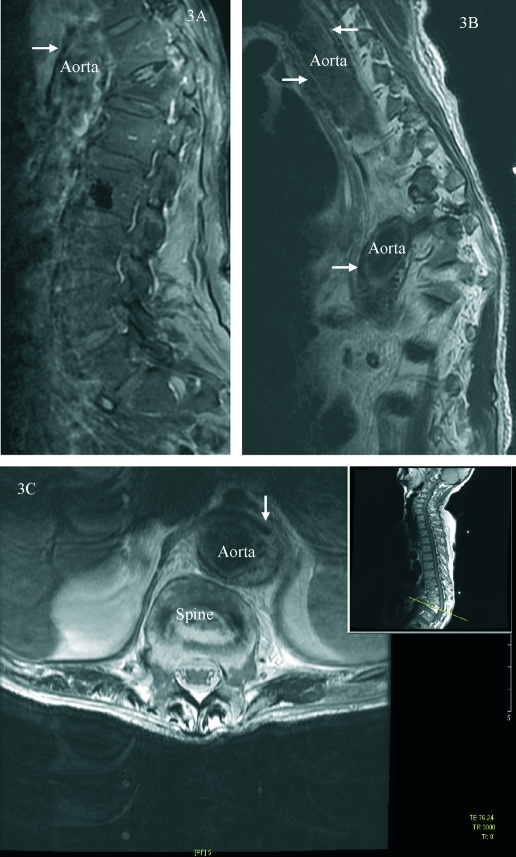
Figure 3.
MRI of thoracic and lumbar spines showing multifoci of air bubbles along the thoracic and abdominal aorta in T1-weighted and T2-weighted images (arrows in (A) and (B)) and periaortic regions (arrow in (C)).
INVESTIGATIONS
Radiological pictures, including plain radiographs, CT aortography and MRI of thoracic and lumbar spines revealed multifoci of air bubbles within the parenchyma of non-enhanced left kidney extending to the hilum and abdominal aorta, and ascending to the thoracic aorta and distal aortic arch, which were compatible with EPN complicated with PM.
DIFFERENTIAL DIAGNOSIS
The presence of PM implicates the possibility of life-threatening underlying illnesses, including a variety of severe iatrogenic injuries, blunt oral, cervical or chest trauma, obstructive lung diseases, intoxication, severe pulmonary infection and retroperitoneal infection, such as in the present case with EPN. Retroperitoneal air can migrate into the thoracic cavity with nuchal subcutaneous tissues in some instances. We recommend that the differential diagnosis of PM or nuchal subcutaneous emphysema should also include retroperitoneal infection, such as EPN.
TREATMENT
A consulted urologist suggested surgical intervention, but the patient’s family did not consent to the procedure due to the patient’s age and the high risk from surgery. Intravenous antibiotics with cefmetazole, gentamycin and metronidazole were prescribed.
OUTCOME AND FOLLOW-UP
EPN is a rare but life-threatening infection with a high mortality rate (70% to 90%), and the majority of patients have diabetes mellitus. Our patient died on the 22nd day without surgical intervention.
DISCUSSION
EPN is a rare but life-threatening acute suppurative infection of kidney characterised by production of gas within the renal parenchyma, collecting system, or perirenal tissue, with a high mortality rate (70% to 90%). The majority of patients have diabetes mellitus and the left kidney is most commonly involved. Escherichia coli is the most common pathogen.1–5 EPN complicated with PM has been reported in only four cases previously.1–4 The pathogenesis of PM from intra-abdominal origin involves the escape of gas from the abdomen and its diffusion superiorly through the paravertebral retroperitoneal tissues, diaphragmatic hiatus or along the great vessels into the mediastinum by pressure gradient.1,3,5 The frequency of EPN complicated with PM is very low. MRI is the most sensitive radiological technique and CT is 100% diagnostic in the presence of suspicious chest and abdominal films.1 History taking, physical examination and image study are needed to administer immediate treatment. EPN should be initially treated according to the recommendations of Huang and Tseng.5 Once EPN is cured PM can be controlled.1 We recommend that the differential diagnosis of PM should include retroperitoneal infections, such as EPN.3
LEARNING POINTS
Pneumomediastinum (PM) may be a first manifestation of emphysematous pyelonephritis (EPN).
Radiological mandatory studies should include CT and even MRI, especially in the presence of suspicious chest and abdominal films.
Adequate intravenous fluid resuscitation with empiric antibiotics and surgical debridement and/or drainage are recommended in these life-threatening conditions.
Footnotes
Competing interests: None.
Patient consent: Patient/guardian consent was obtained for publication.
REFERENCES
- 1.Ting KH, Lin KH, Chang CC. Emphysematous pyelonephritis: presenting with pneumomediastinum. Am J Emerg Med 2006; 24: 350–2 [DOI] [PubMed] [Google Scholar]
- 2.Park SH, Hong HP, Kim MC, et al. Emphysematous pyelonephritis associated with pneumoperitoneum and pneumomediastinum: a case report. J Korean Soc Emerg Med 2005; 16: 398–402 [Google Scholar]
- 3.Wang YC, Wang JM, Chow YC, et al. Pneumomediastinum and subcutaneous emphysema as the manifestation of emphysematous pyelonephritis. Int J Urol 2004; 11: 909–11 [DOI] [PubMed] [Google Scholar]
- 4.Menif E, Nouira K, Baccar S, et al. Emphysematous pyelonephritis: report of 3 cases. Ann Urol (Paris) 2001; 35: 97–100 [DOI] [PubMed] [Google Scholar]
- 5.Huang JJ, Tseng CC. Emphysematous pyelonephritis: clinicoradiological classification, management, prognosis, and pathogenesis. Arch Intern Med 2000; 160: 797–805 [DOI] [PubMed] [Google Scholar]