Background
Bowel obstruction is a common surgical emergency. If a patient fails to settle with conservative management or demonstrates signs of peritonitis an operation is indicated.1 As part of the assessment, radiological investigation, as well as history and examination, can be paramount in identifying the cause. We describe a rare and previously unreported aetiology for small bowel obstruction due to fistulation of a spinal implant into the bowel lumen.
Case presentation
A 72-year-old woman with a past history of ulcerative colitis and long-term steroid therapy underwent subtotal colectomy and end ileostomy 11 years previously. Over the preceding 12 months she had experienced multiple episodes of subacute bowel obstruction and abdominal pain. Investigations with plain radiographs and CT had failed to identify a cause, although adhesions were suspected as the most likely cause. The patient presented with a 4-day history of abdominal distension, nausea and vomiting, with decreased output from her ileostomy. Past surgical history consisted of multiple spinal operations, including an L1-4 spinal fusion 9 years earlier followed by an L5/S1 decompression 2 years ago. This second spinal operation was complicated by methicillin-resistant Staphylococcus aureus (MRSA) sepsis and chronic osteomyelitis of the lumbosacral spine. She was obese, type II diabetic and with poor mobility. On initial assessment she was septic, in atrial fibrillation and had a positive urine dipstick for blood, leucocytes and nitrites. The diagnosis of urinary sepsis and ileus was made. She was treated conservatively with nasogastric tube, intravenous fluids and antibiotics. Her stoma output increased and she improved clinically. On day 9 of the admission, she complained of increased abdominal distension and pain, and again the stoma stopped working. She was tachycardic, with a low-grade temperature and raised WCC (25). Abdominal x-ray showed small bowel obstruction, thought to be adhesional (figure 1). A CT scan was performed which demonstrated the presence of a foreign body causing obstruction just proximal to ileostomy (figure 2).
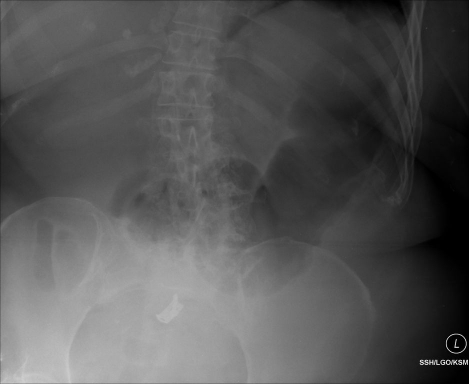
Figure 1.
Plain abdominal taken on admission showing distended small bowel but no evidence of the radio-opaque spinal disc spacer.
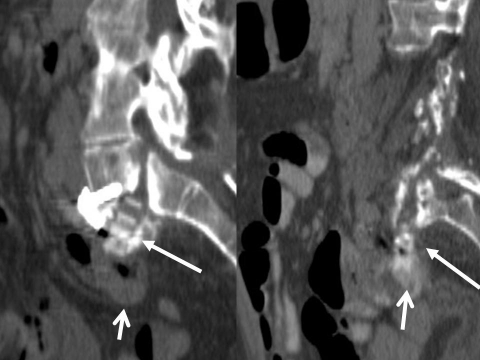
Figure 2.
Sagittal reformatted (left) and axial (right) CT images demonstrating the L5/S1 disc spacer (block arrow) within the dilated prestomal small bowel (stoma – open arrow). Note the CT attenuation characteristics of the spacer, lower than adjacent cortical bone, making it difficult to visualise on plain radiography.
The patient absolutely denied passing anything per stoma. A laparotomy with on table ileoscopy via the stoma was performed. Endoscopy was unhelpful and failed to identify the obstruction. At laparotomy adhesions were divided and the point of obstruction with collapsed distal small bowel identified. Enterotomy identified a cage implant used in the L5/S1 spinal fusion, to be the cause of obstruction (figure 3).2 3 Following removal, she settled without further complication.
Figure 3.
Cage implant used in the L5/S1 spinal fusion, removed from the small bowel.
Discussion
Following extensive literature review, no cases of small bowel obstruction due to spinal implants have been reported. Abdominal complications following spinal instrumentation have been seen, but appear to be exceptionally rare. A first report of bowel perforation from a spinal rod in a paediatric patient was reported in 20054, and a gastrointestinal bleed has also been reported.5 This case raises a number of issues. The patient had had previous episodes of small bowel obstruction presumed secondary to adhesions. Abdominal radiographs at the time had not been able to identify the radiolucent spinal cage implant made from a carbon-fibre composite. Although non-metalic implants are not visible on plain radiographs (figure 1), with an index of suspicion it is possible to identify them with CT. More recent implants have radio-opaque tracers which help accurate alignment in surgery and would be clearly identifiable on plain film. Had the implant been seen on previous imaging, intervention may have been planned at an earlier stage. Retrospective review of her CT scans does show the spinal implant apparently fistulating into the small bowel 4 months prior to this admission, most visible on multiplanar reformats (figure 4). This patient's history of multiple spinal instrumentation with long-term steroids and MRSA osteomyelitis would place her at risk of small bowel fistulation. At operation small bowel endoscopy was attempted but, as is often the case, this was unsuccessful. The patient was better served by laparotomy, in view of her deteriorating clinical picture and the need to find the definitive cause of obstruction. If clinical findings mandate laparotomy this should not be delayed. This case is a first report in the literature of small bowel obstruction due to fistulation of a spinal implant directly into the bowel lumen.
Figure 4.
Sagittal reformats of the lumbar spine. Eighteen months pre-episode (left) – subluxation of the disc spacer (block arrow) associated, but not fistulating into small bowel loops antero-inferiorly (open arrow). Four months pre-episode (right) – disc spacer (block arrow) apparently fistulating into oral-contrast-filled small bowel (open arrow). Interestingly, no gas is seen tracking back into the disc space.
Footnotes
Competing interests None.
Patient consent Obtained.
References
- 1.Coleman MG, Moran BJ. Small bowel obstruction. In: Johnson CD, Taylor I, eds. Recent advances in surgery 22. Edinburgh: Churchill Livingstone, 1999:87–98 [Google Scholar]
- 2.PEEK Becoming an Alternative to Titanium Spinal Fusion Cages. Technology Spotlight. http://www.medcompare.com (accessed 15 July 2010)
- 3.Kurtz SM, Devine JN. PEEK biomaterials in trauma, orthopedic, and spinal implants. Biomaterials 2007;28:4845–69 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Nguyen H, Tomita S, Gillingham B. Small bowel perforation from unit rod posterior spinal fusion. J Pediatr Surg 2005;40:e7–8 [DOI] [PubMed] [Google Scholar]
- 5.Al-Binali AM, Sigalet D, Goldstein S, et al. Acute lower gastrointestinal bleeding as a late complication of spinal instrumentation. J Pediatr Surg 2001;36:498–500 [DOI] [PubMed] [Google Scholar]