Abstract
Lightning strike is the most common environmental cause of sudden cardiac death, but it may also be associated with a myriad of injuries to various organ systems. Direct myocardial injury may be manifest as electrocardiographic alterations or elevation in cardiac-specific isoenzymes; however, significant electrical cardiac trauma appears uncommon. A case is presented of severe acute cardiomyopathy in a “Takotsubo” distribution causing cardiogenic shock following lightning strike in a previously healthy 37-year-old woman. Although rarely identified in this context, Takotsubo cardiomyopathy (also known as “transient left ventricular apical ballooning syndrome”) is characterised by transient cardiac dysfunction, electrocardiographic changes that may mimic acute myocardial infarction and minimal release of cardiac-specific enzymes in the absence of obstructive coronary artery disease. The condition is associated with a substantial female bias (up to 90% of cases) in reported series, and despite occasionally dramatic presentations recovery of left ventricular function is almost universal over days to weeks. In rare instances, however, the syndrome has been associated with more catastrophic complications such as papillary muscle or cardiac free wall rupture, necessitating emergency surgical intervention to preserve life. In clinical practice, non-lethal lightning strike-induced cardiac injury is frequently associated with small elevations of cardiac isoenzymes without overt clinical sequelae; however, the incidence of silent myocardial mechanical dysfunction remains unknown. Cases such as the one presented highlight the potential for serious, albeit usually transient, cardiac sequelae from lightning strike injury and remind us that our mothers’ advice to remain indoors during thunderstorms is probably worth heeding.
BACKGROUND
Lightning strike is the most common environmental cause of sudden cardiac death, but it may also be associated with a myriad of injuries to various organ systems.1 Direct myocardial injury may be manifest as electrocardiographic alterations or elevation in cardiac-specific isoenzymes; however significant electrical cardiac trauma appears uncommon. We report a case of lightning strike-induced cardiomyopathy causing cardiogenic shock.
CASE PRESENTATION
A 37-year-old woman, with no significant past medical history, was struck by lightning while running from the beach to avoid an approaching electrical storm. She suffered a cardiac arrest, with immediate cardiopulmonary resuscitation commenced by nearby friends and rapid spontaneous recovery. On arrival at hospital, she exhibited fluctuating mental state, facial and limb paraesthesia and shoulder and back pain. Circumferential neck burns were apparent, associated with a metallic necklace she had been wearing at the time of the attack, and punctate burns were noted at her waist, related to metallic jean studs. Her thorax, abdomen and lower limbs were remarkable for the striking cutaneous “ferning” (Lichtenberg figures) of electrical injury. No obvious exit wounds were apparent. Otherwise there was no evidence of head trauma and cardiovascular examination was initially unremarkable. Admission ECG revealed sinus rhythm at 100 beats/min with widespread minor ST elevation and normal QTc interval.
Soon after initial hospital assessment, she rapidly developed respiratory distress with radiographic evidence of pulmonary oedema. Subsequent biochemistry revealed marked elevation of predominantly skeletal muscle creatine kinase (3154 U/l, myocardial creatine kinase 29.3 µg/l; 0.9%) and an associated elevation in cardiac troponin T (0.83 µg/l). Transthoracic echocardiography was performed to differentiate cardiac failure from direct electrical pulmonary injury as a cause of her deterioration. This revealed left ventricular apical akinesis and associated moderate–severe left ventricular systolic impairment despite basal preservation of contractile function; changes consistent with a “Takotsubo” cardiomyopathy.
INVESTIGATIONS
Initial ECG revealed sinus tachycardia with widespread minor ST elevation. Chest x ray revealed widespread alveolar opacities consistent with pulmonary oedema, with associated prominence of the pulmonary veins and upper lobe venous diversion. Cardiac silhouette appeared normal.
Biochemistry: creatine kinase (3154 U/l, myocardial creatine kinase 29.3 µg/l; 0.9%), elevation in cardiac troponin T (0.83 µg/l). Otherwise nothing abnormal detected (initially).
Transthoracic echocardiography was performed to differentiate cardiac failure from direct electrical pulmonary injury as a cause of her deterioration: The echocardiogram showed moderate–severe global left ventricular systolic dysfunction with mid-apical segment akinesis but sparing/hyperkinesis of myocardial basal segments; features consistent with a Takotsubo cardiomyopathy.
Subsequent coronary angiography revealed normal coronary arteries.
DIFFERENTIAL DIAGNOSIS
Direct electrical cardiac injury – cardiac isoenzyme release inconsistent with the degree of cardiac systolic dysfunction.
Direct cardiac trauma related to cardiopulmonary resuscitation (CPR) – minimal CPR performed with “spontaneous” return of circulation. Dysfunction inconsistent with mechanical myocardial contusion.
Hypoxic myocardial injury – period of cardiac arrest (less than 1 min) would appear insufficient to cause myocardial dysfunction of such severity in an otherwise healthy individual.
Bystander myocarditis – no clinical features pre-lightning strike to suggest a coincidental inflammatory carditis.
TREATMENT
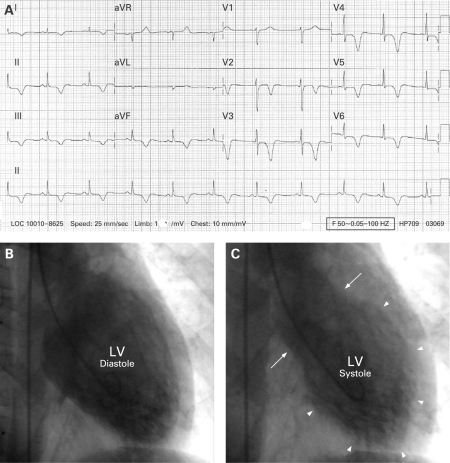
Supportive measures were successfully employed with diuresis and cardiac monitoring. Subsequent ECGs revealed striking anterolateral and inferior T wave inversion suggestive of widespread cardiac ischaemia (fig 1A). Coronary angiography was performed 7 days later, confirming normal coronary arteries with moderate–severe cardiomyopathy in a “Takotsubo” distribution (fig 1B, C). As demonstrated by transthoracic echocardiography, proximal systolic contraction was preserved (arrows) with severe hypokinesis of the mid-distal segments (arrowheads).
Figure 1.
(A) 12-Lead electrocardiogram performed on the day following lightning strike, revealing deep inferior and anterolateral T wave inversion, more often consistent with widespread myocardial ischaemia. (B, C) Left ventriculogram performed 7 days after lightning strike, demonstrating preserved contractility/hypercontractility in the basal segments (arrows) and severe hypokinesis in the mid-distal segments (arrowheads), consistent with a “Takotsubo” cardiomyopathy. LV, left ventricle.
OUTCOME AND FOLLOW-UP
Cardiac function returned to normal over the subsequent 6 weeks with supportive medical care.
DISCUSSION
Takotsubo cardiomyopathy (also known as “transient left ventricular apical ballooning syndrome”) is characterised by transient cardiac dysfunction, ECG changes that may mimic acute myocardial infarction and minimal release of cardiac-specific enzymes in the absence of obstructive coronary artery disease.2 First described in Japan in 1991,3 the syndrome was named “Takotsubo” cardiomyopathy after the round-bottomed, narrow-necked pots (“tako-tsubo”) still used to trap octopus in that country. Traditionally associated with episodes of extreme emotional stress, the function of the distal myocardial segments is depressed, with compensatory hyperkinesis of the basal regions, producing the appearance of systolic apical ballooning, as in this case. Best described in the Japanese population, case series have been reported in white populations in Europe and North America more recently with a substantial female bias (up to 90% of cases).2 The pathogenesis of the condition remains uncertain but is believed to relate either to direct catecholamine-mediated cardiotoxicity, or to transient global myocardial ischaemia resulting from coronary spasm or widespread microvascular dysfunction.2 Despite occasionally dramatic presentations, recovery of left ventricular function is almost universal over days to weeks. In rare instances, however, the syndrome has been associated with more catastrophic complications such as papillary muscle or cardiac free wall rupture, necessitating emergency surgical intervention to preserve life.
This case report describes the development of acute cardiogenic shock in a young woman following lightning strike, with echocardiographic and angiographic evidence of a severe cardiomyopathy in a “Takotsubo” distribution. Although the exact pathogenesis of cardiomyopathy in this woman is uncertain, the brief duration (<20 s) of cardiac arrest and resuscitation suggest that hypoxia and mechanical trauma related to chest compression would be unlikely causes. Whether related to direct electrical injury causing myocardial infarction or stunning, or to an adrenergic surge in the context of lightning strike and cardiac arrest, is uncertain; however, the rapidly improving clinical course strongly favours the Takotsubo syndrome.
In clinical practice, lightning-strike-induced cardiac injury is frequently associated with small elevations of cardiac isoenzymes without overt clinical sequelae; however, the incidence of silent myocardial mechanical dysfunction remains unknown. Such cases highlight the potential for serious, albeit usually transient, cardiac sequelae from lightning strike injury and remind us that our mothers’ advice to remain indoors during thunderstorms is probably worth heeding.
LEARNING POINTS
Lightning strike is the most common environmental cause of sudden cardiac death.
Silent myocardial dysfunction following electrical injury may be more common than suspected based on routine clinical assessment.
Takotsubo cardiomyopathy is characterised by transient cardiac dysfunction, ECG changes that may mimic acute infarction and normal coronary arteries.
More common in women, Takotsubo cardiomyopathy invariably follows some form of major emotional or physical precipitant, and recovery over days to weeks is usual.
We describe a case of Takotsubo cardiomyopathy associated with lightning strike.
Acknowledgments
This article has been adapted with permission from Dundon BK, Puri R, Leong DP, Worthley MI. Takotsubo cardiomyopathy following lightning strike. Emerg Med J 2008; 25: 460–1.
Footnotes
Competing interests: none.
REFERENCES
- 1.Whitcomb D, Martinez JA, Daberkow D. Lightning injuries. South Med J 2002; 95: 1331–4 [PubMed] [Google Scholar]
- 2.Gianni M, Dentali F, Grandi AM, et al. Apical ballooning syndrome or takotsubo cardiomyopathy: a systematic review. Eur Heart J 2006; 27: 1523–9 [DOI] [PubMed] [Google Scholar]
- 3.Dote K, Sato H, Tateishi H, et al. Myocardial stunning due to simultaneous multivessel coronary spasms: a review of 5 cases. (In Japanese).J Cardiol 1991; 21: 203–14 [PubMed] [Google Scholar]