Abstract
The authors report a case of an older gentleman with a history of metastatic prostate cancer who presented to the emergency department following 3 weeks of progressively intermittent and then continuous priapism. After an initial clinical workup, an MRI was performed of the pelvis for further evaluation of the patient's condition which demonstrated metastatic lesions within his corpora cavernosa. The patient underwent follow-up core-needle biopsy with pathologically proven metastasis.
Background
As one of several causes of painless priapism, malignant priapism is an exceedingly rare cause which is rarely seen in the emergency setting. Diagnostic imaging is an important part of the standard work-up of a patient presenting with this condition, and both MRI and ultrasound are tools which are readily available in the emergency department setting for further evaluation.
Case presentation
Our patient, an older man with a greater than 20-year history of Gleason 4+5 prostate cancer, with known osseous and liver metastasis, contacted his urologist complaining of ‘paroxysmal’ episodes of erections for the prior 3 weeks that had progressed into one continuous and unrelenting erection over the preceding week. The patient had experienced no haematuria, voiding difficulties or other constitutional symptoms. Because the patient contacted his urologist after hours, he was instructed to present to the Emergency Department for immediate evaluation by the on-call urology resident to which he agreed.
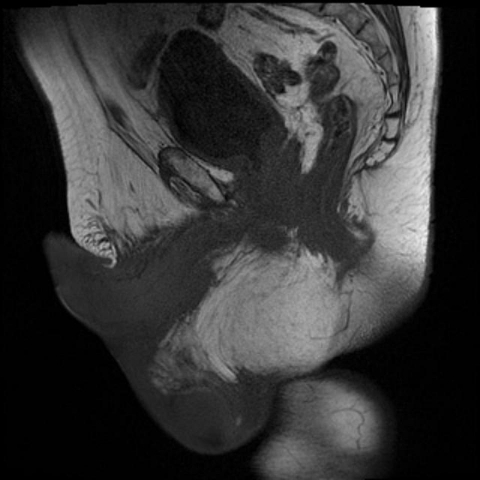
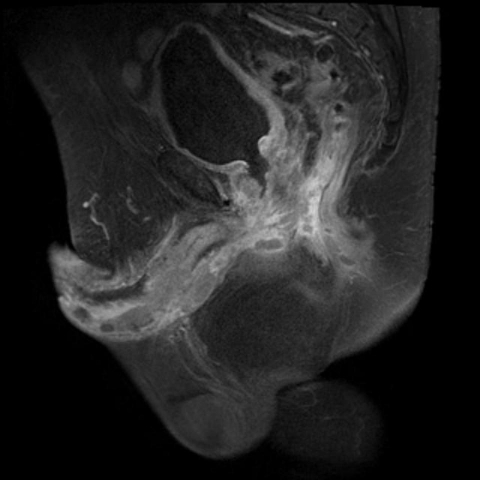
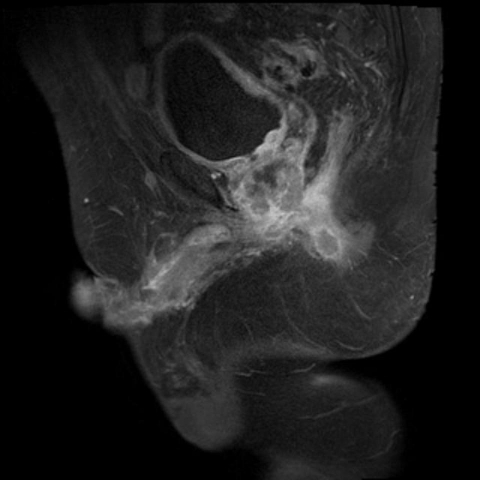
In the emergency room, the patient was found to have a non-tender, fibrous priapism with mild-to-moderate, non-pitting scrotal edema and adjacent groin edema. No penile discharge was noted. Prostate examination revealed a firm, non-tender gland without nodules. An MRI was performed by request of the urology department using a Siemens 3.0 Tesla MR magnet (Megnetom Trio; Siemens AG, Erlangen Germany) to acquire images of the lower pelvis and penis with axial, sagittal and coronal multi-planar fields of view in standard T1, T2 and postcontrast T1 fat-suppressed sequences. Multiple nodular lesions within both corpora cavernosum showed isointensity to the surrounding vascular structures on T2, with enhancement of the lesions following gadolinium administration on the postcontrast fat-suppressed T1 weighted sequence (figure 1). The patient's primary prostatic adenocarcinoma was also visualised invading the inferior aspect of the bladder, with associated irregularity of the bladder wall which enhanced following contrast administration. In addition, several peripherally enhancing nodules were identified within the right ischiorectal fossa compatible with necrotic lymphatic metastasis (figure 2). After acquiring the MRI, a phenylepherine injection of the penis was performed in an attempt to treat the patient's priapism. This therapeutic attempt was unsuccessful, and the patient was subsequently discharged home with a painless erection and no demonstrable voiding difficulties. A follow-up CT and biopsy were scheduled for the next morning with Urology.
Figure 1.
Sagittal T1 (upper left), T2 (upper right) and postcontrast fat suppressed T1 (lower left) images through the midline of the pelvis demonstrate nodular metastasis and engorgement of the corpora cavernosa. Also note the irregularity of the prostate and thickening of the inferior bladder wall secondary to invasion by the primary adenocarcinoma of the prostate.
Figure 2.
Sagittal postcontrast fat suppressed T1 weighted image through the right lower pelvis demonstrates a peripherally enhancing nodule within the right ischiorectal fossa compatible with necrotic metastatic lymph nodes. Again seen is the irregularly enhancing primary prostatic mass with extension to the inferior bladder wall.
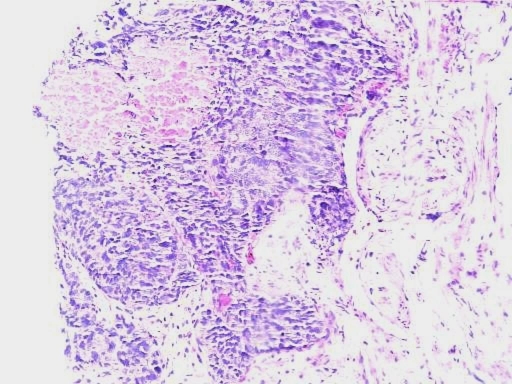
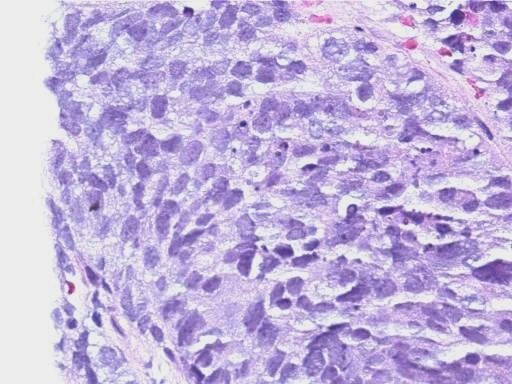
The next day the patient underwent multiple core-needle biopsies of both the proximal and distal portions of the left corpora cavernosum within the urology department. Pap stain-2, Diff Quik-1 and Hemotoxylin and Eosin stains revealed poorly differentiated adenocarcinoma consistent with metastatic adenocarcinoma of the prostate (figure 3). In addition, lymphovascular invasion was identified.
Figure 3.
(A) Medium and (B) high magnification H&E stains from corporal penile aspiration show solid sheets of neoplastic epithelial cells with areas of central necrosis are visualised, compatible with the patient's prior Gleason 5 prostate carcinoma.
Differential diagnosis
Given the patient's history of malignancy, metastatic cancer would be a primary consideration, with the most common sources including urothelial (transitional cell carcinoma), prostate, renal, gastrointestinal (colon and oesophageal) and melanoma. Additional considerations would include extension of primary squamous-cell carcinoma or basal-cell carcinoma of the penis into the corpora. Final malignant considerations would include primary or metastatic sarcoma to the corpora cavernosa; however, this is exceedingly rare. Additionally, high- and low-flow states of priapism would be a consideration, with high-flow states caused by conditions such as traumatic penile injuries, cavernosal arterial injuries, arteriosinusoidal fisula's and cocaine use. Low-flow states of priapism are most commonly due to venooclusive or ischemic changes secondary to conditions such as hypercoaguable states (lupus, malignancy, protein C deficiency), dialysis, vasculitis, medications (trazodone, riperidol, hydralazine, prazosin), alcohol and spinal-cord impingement.
Treatment
Prior to presentation, the patient was taking an oral regimen of 50 mg of bicalutamide daily and 10.8 mg of goserelin via injection every 3 months for treatment of his metastatic disease. Following his episode of malignant priapism, the patient was treated palliatively with external beam radiation, as it was felt that with his associated co-morbidities he would not do well surgically. In addition, the patient's bicalutamide dose was increased to 150 mg PO daily. He continued with his prescribed dose of 10.8 mg of goserelin every 3 months. In addition, he underwent chemo-embolisation of his hepatic metastasis approximately 2 months following his episode of priapism.
Outcome and follow-up
The patient was regularly followed by his urologist, with subsequent palliative radiation as his primary therapy. He received 4000 cGy of radiation to his prostate, base of his bladder and to his penis. In addition, his bicalutamide was increased to 150 mg following his presentation. Following his change in medical therapy and radiation, the patient's priapism slowly resolved over the following several weeks. Over the next several months, the patient's overall condition continued to decline, and he eventually succumbed to his disease.
Discussion
Priapism is defined as a sustained, undesirable erection lasting greater than 4 h which is not associated with stimulation or sexual interest. Generally, the aetiology of priapism is due to either high-flow or low-flow states, with idiopathic or pharmacologic causes as the most common cause in adults. High-flow priapism is generally secondary to traumatic injury to the pelvis, with increased arterial flow to the penis causing a sustained erection. Low-flow causes are many, to include haemoglobinopathies, pharmacologic, neoplastic and neurologic causes. Priapism is subsequently classified into either ischemic or non-ischemic causes, with ischemic causes generally secondary to low-flow states with resultant decreased overall blood flow throughout the penis. Ischemic priapism is a medical emergency, with treatment indicated within 24–48 h due to risks of tissue loss and necrosis. Other potential consequences of priapism include severe patient discomfort and pain, risk of urinary retention, as well as potential vascular compromise (if traumatic in origin). This spectrum of pathologic aetiologies renders evaluation of priapism as a medical emergency, as the source is often immediately unknown prompting urgent initiation of the patient's diagnostic work-up.1
Ultrasound is the most common primary imaging modality to visualise the penis, with MRI used as an adjunct to ultrasound for problem solving when the clinical and sonographic features remain non-diagnostic. Ultrasound is readily accepted for initial screening due to its high availability, low cost and real-time capabilities. High-frequency, 7.5–12 MHz, linear transducers are used because they yield images with better resolution, compared to lower-frequency transducers. Transverse and longitudinal grayscale images of the corpora spongiosum and both cavernosa are captured along with Doppler images of the both cavernosal arteries in order to document flow characteristics.2 Subsequently, lesions which are identified with US are further characterised in multiple planes with grayscale and focal Doppler interrogation. Metastatic disease usually appears as either a single focal hypoechoic lesion or multiple hyperechoic structures, both of which demonstrate hypervascularity.3
With its excellent soft-tissue contrast, multi-planar capabilities and excellent spatial resolution, MRI can also confidently be used to identify and characterise primary and metastatic penile neoplasms. MRI distinguishes between corpora cavernosa and spongiosum depending upon the rate of blood flow through them at the time of imaging. Most commonly, the cavernous spaces are intermediate signal on T1 and high signal on T2 sequences. The corpora cavernosa demonstrate the same signal because they share common blood flow via interconnecting fenestrations. The spongiosum, however, is isolated from the cavernosa, and its signal varies slightly from them. The cavernosal bodies are surrounded by an inner and outer fibrous layer, the tunica albuginea and Buck's fascia, respectively; which are low in signal intensity on both T1 and T2 weighted images. Cavernosal arteries are seen on coronal T2 images as a hypointense foci within the medial aspect of the corpora cavernosa. T1, T2 and postcontrast fast suppressed T1 images are routinely regarded as the most useful sequences to obtain when evaluating for malignancy of the penis.4
Metastasis to the penis is relatively rare, despite its rich blood supply.4–6 However, despite its rarity, penile metastasis generally portends an advanced stage and a poor prognosis.4 5 Penile metastasis usually arises secondary to a surrounding primary genitourinary organ malignancy in 70–75% of cases,4–6 with rectosigmoid colon primaries accounting for another 13%.6 The most frequent primary cancer to metastasise to the penis is cancer of the bladder (27%) followed by primary prostatic cancer (generally adenocarcinoma from the glandular portion of the organ).4 5 7 Eberth is credited for documenting the first case of penile metastasis in 1870, and since that time, there have been about 460 additional cases reported in the literature worldwide.6 8
Retrograde venous flow via communications between the dorsal venous system of the penis and venous plexuses draining the pelvic viscera is believed to be the primary route of malignant spread to the penis.5 6 Other routes of malignant spread to the penis include retrograde lymphatic flow, arterial spread, direct extension from aggressive low-lying rectal cancers and implantation secondary to surgical instrumentation.6 9 The corpora cavernosa are the most frequently reported sites of penile metastasis.5
Penile metastasis most commonly presents as multiple infiltrative lesions, indurated nodules (60%) or in episodes of priapism (40%).4–6 9An even rarer presentation is the distinct entity known as ‘malignant priapism’ which was first described in 1938 by Peacock. Malignant priapism is defined as the invasion of malignant cells into the cavernous sinuses and draining veins without affecting the arterial supply. The blockage of venous drainage leads to an erection from inability of the patent, distended cavernous sinuses to drain.4 Another mechanism which may contribute to malignant priapism includes irritation of the neural pathways of erection by local tumour infiltration. Both high- and low-flow states of priapism occur and high-flow priapism (high-flow in the cavernosal arteries with reversal of flow in diastole) is believed to be more common.4 6 Regardless of exact mechanism, vascular invasion of the penis likely portends a poorer outcome in metastatic disease when it originates from urothelial carcinomas and adenocarcinoma of the prostate.7
Biopsy or corporeal aspirations are the most common procedures to yield a histopathalogical diagnosis.6 Imaging remains the most sensitive method for determining cavernosal metastasis and is also extremely useful in preoperative staging.9 On MRI, penile metastasis usually has a low signal intensity on T1 which is isointense to the adjacent corpora cavernosa. The metastatic focus is heterogeneously hypo- to iso-intense and clearly contrasted against the hyperintense signal of the cavernosal bodies on T2 weighted imaging. Metastatic foci commonly enhance on postcontrast T1 images more than the adjacent cavernosum. In addition, MRI is quite useful for evaluating the primary malignancy if confined to the genitourinary tract, prostate or rectosigmoid colon secondary to their inclusion within the typical field of view. Metastatic lymph node involvement may additionally be noted and can assist with surgical staging.6 9
Management of metastatic lesion in the corpora cavernosa includes local excision, partial or total penectomy, radiation, and/or chemotherapy. The average prognosis is 1 year (range of 47 weeks to 7 years) from the time cavernous metastasis is first discovered.5
Learning points.
-
▶
Malignant Priapism is an uncommon cause of painless priapism which may be seen in older individuals.
-
▶
MRI and Ultrasound can be readily used to elucidate the cause of painless priapism.
-
▶
Imaging is helpful in staging the patient's disease as well as identifying additional silent disease within the region of interest.
Footnotes
Competing interests None.
References
- Burnett A, Bivalacqua T. Priapism: current principles and practice. Urol Clin North Am 2007;34:631–42 [DOI] [PubMed] [Google Scholar]
- 2.Sadeghi-Nejad H, Dogra V, Seftel AD, et al. Priapism. Radiol Clin North Am 2004;42:427–43 [DOI] [PubMed] [Google Scholar]
- 3.Guvel S, Kilinc F, Torun D, et al. Malignant priapism secondary to bladder cancer. J Androl 2003;24:499–500 [DOI] [PubMed] [Google Scholar]
- 4.Pretorius ES, Siegelman ES, Ramchandani P, et al. MR imaging of the penis. Radiographics 2001;21:S283–98; discussion S298–9 [DOI] [PubMed] [Google Scholar]
- 5.Dubocq FM, Tefilli MV, Grignon DJ, et al. High flow malignant priapism with isolated metastasis to the corpora cavernosa. Urology 1998;51:324–6 [DOI] [PubMed] [Google Scholar]
- 6.Cherian J, Rajan S, Thwaini A, et al. MR imaging of the penis. Radiographics 2001;21:S283–99 [DOI] [PubMed] [Google Scholar]
- 7.Savion M, Livne PM, Mor C, et al. Mixed carcinoma of the prostate with penile metastases and priapism. Eur Urol 1987;13:351–2 [DOI] [PubMed] [Google Scholar]
- 8.Chan PT, Bégin LR, Arnold D, et al. Priapism secondary to penile metastasis: a report of two cases and a review of the literature. J Surg Oncol 1998:68:51–9 [DOI] [PubMed] [Google Scholar]
- 9.Schroeder-Printzen I, Vosshenrich R, Weidner W, et al. Malignant priapism in a patient with metastatic prostate adenocarcinoma. Urol Int 1994;52:52–4 [DOI] [PubMed] [Google Scholar]